Occupational Noise and Hypertension Risk: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
Aims and Objectives
2. Materials and Methods
2.1. Eligibility Criteria
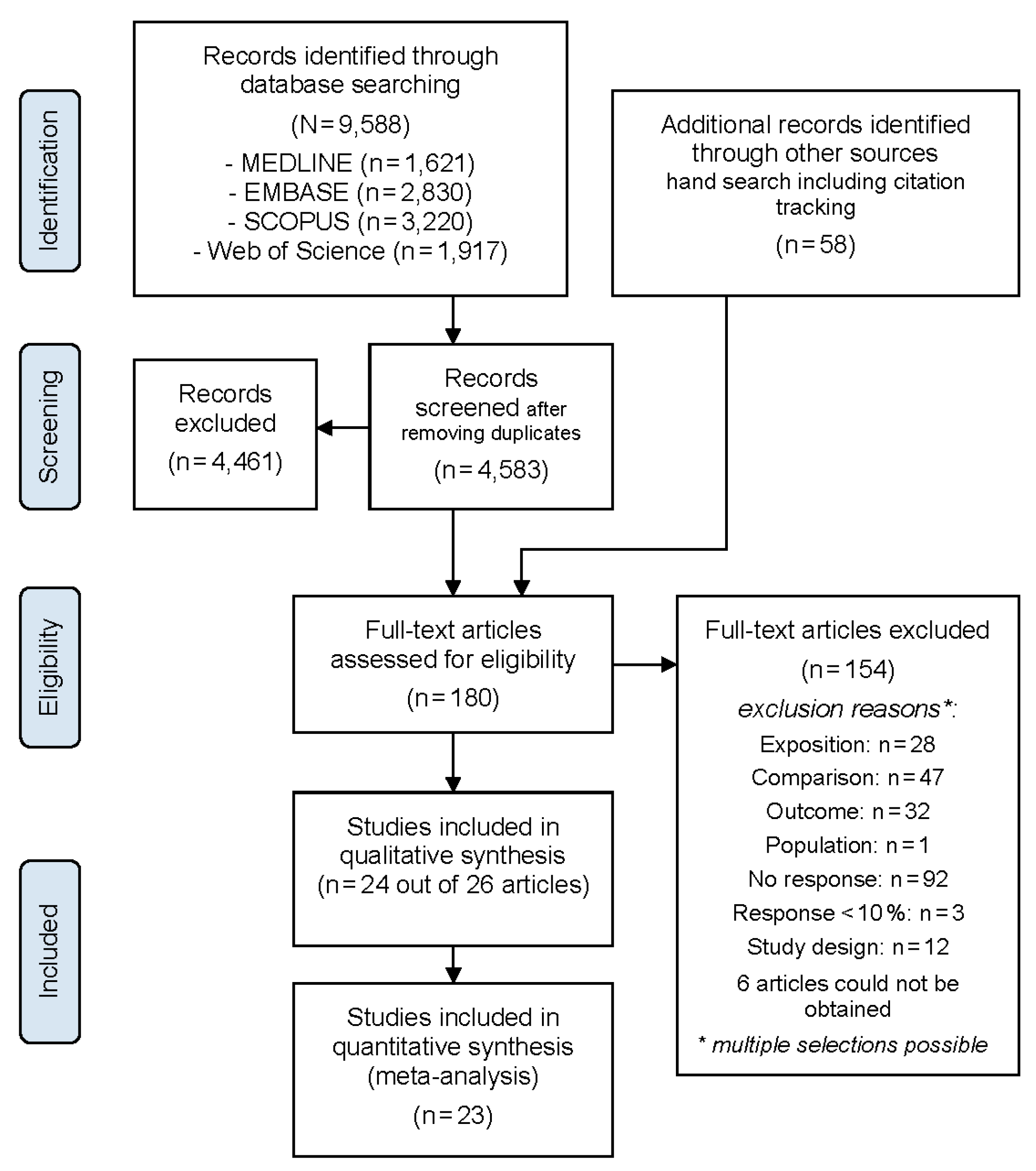
2.2. Study Selection
2.3. Data Extraction and Risk of Bias
2.4. Data Synthesis
2.5. Sensitivity Analysis
2.6. Assessment of Evidence
- study limitations (risk of bias);
- indirectness of evidence;
- inconsistency of evidence;
- imprecision;
- publication bias;
- 6.
- large magnitude of effect;
- 7.
- dose-response gradient; and,
- 8.
- residual confounding increases confidence.
3. Results
3.1. Risk of Bias
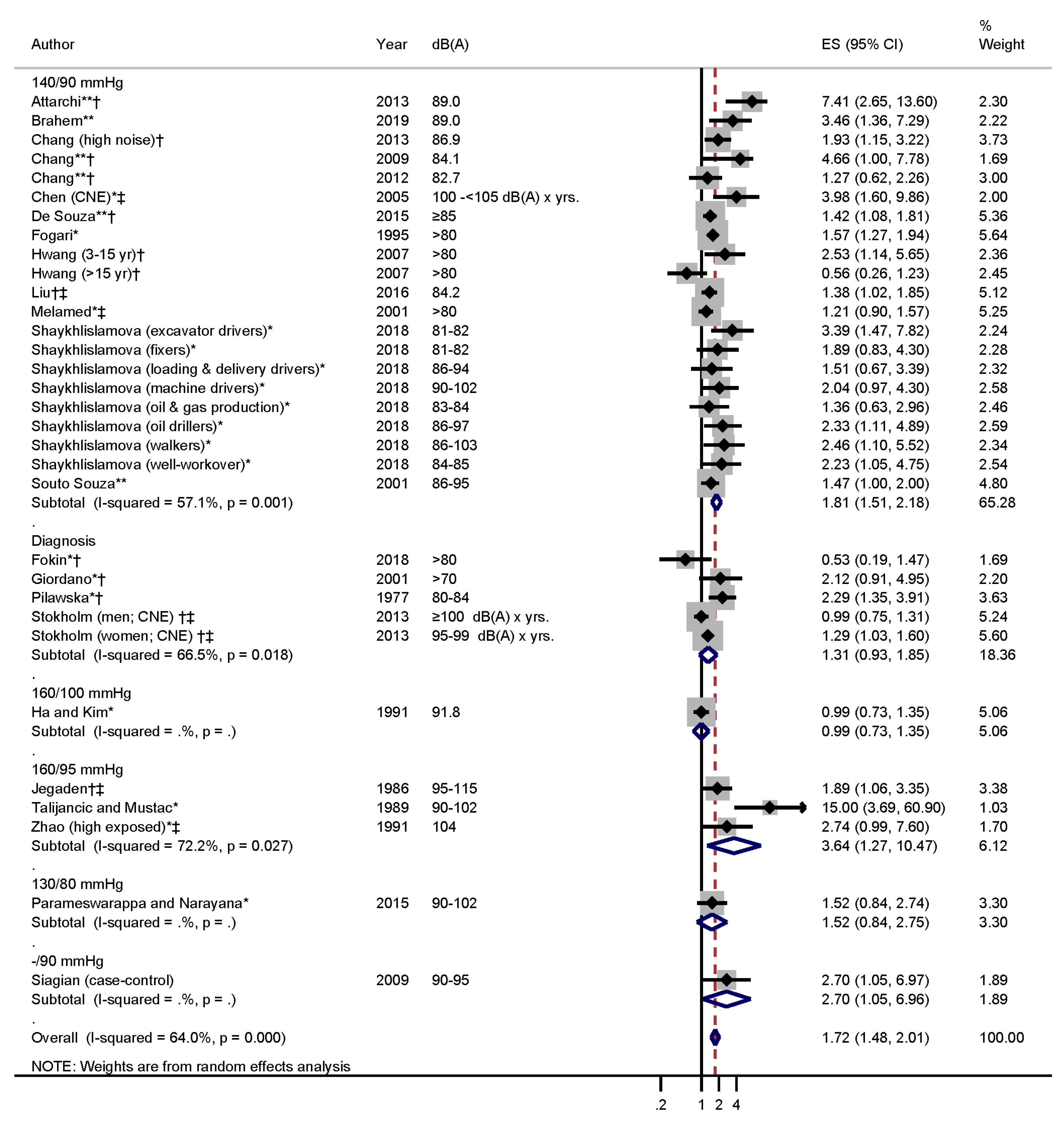
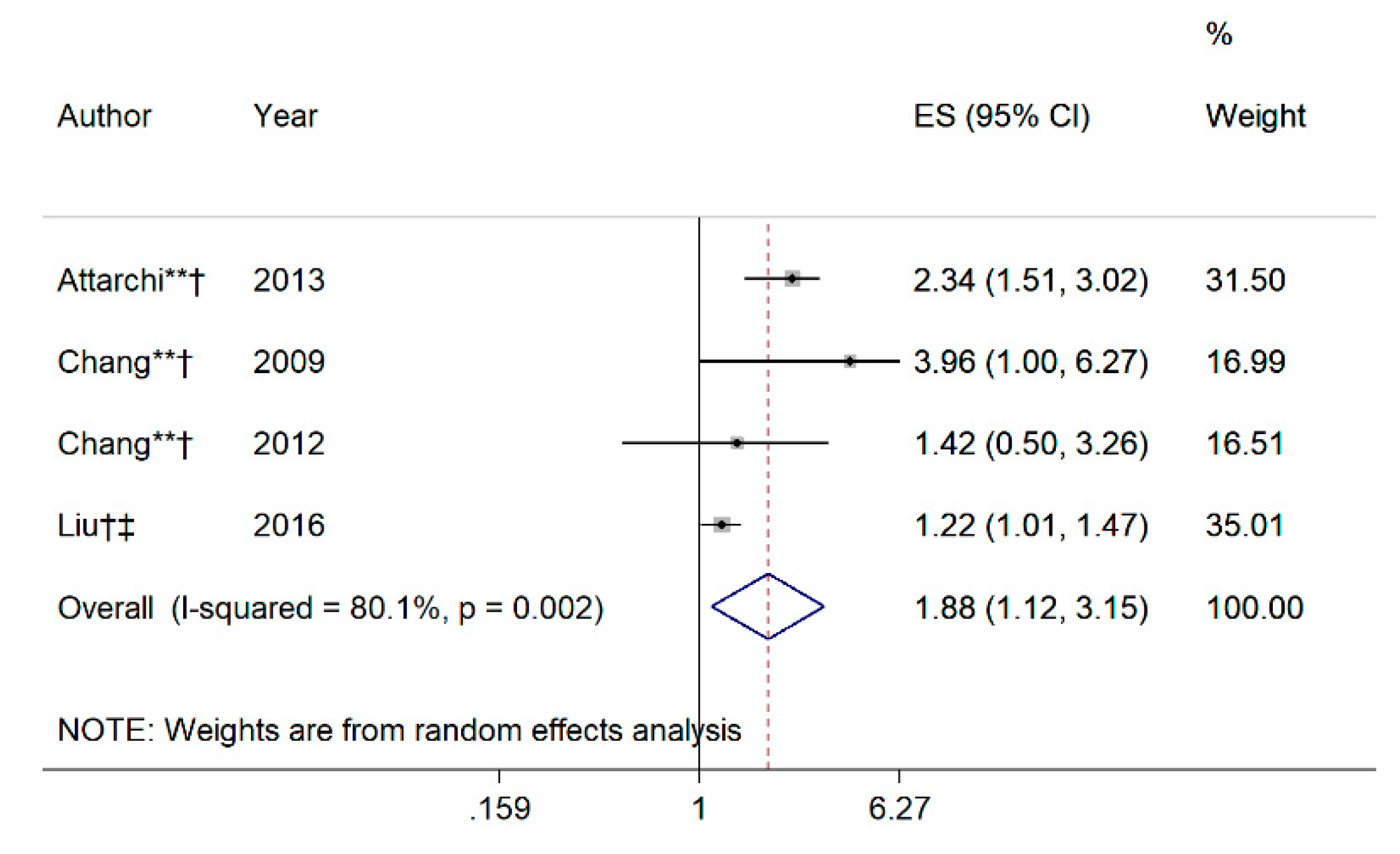
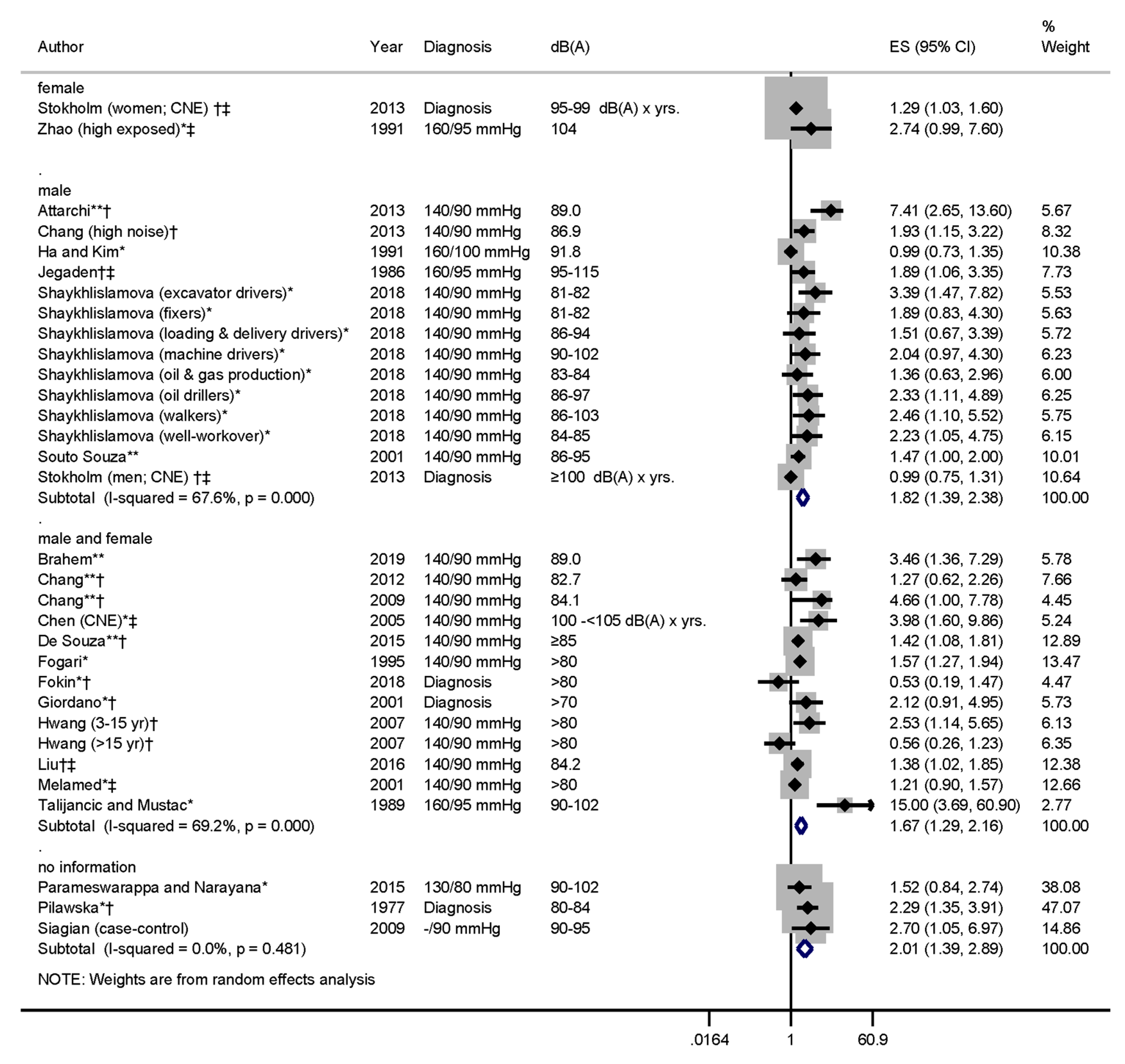
3.2. Meta-Analysis
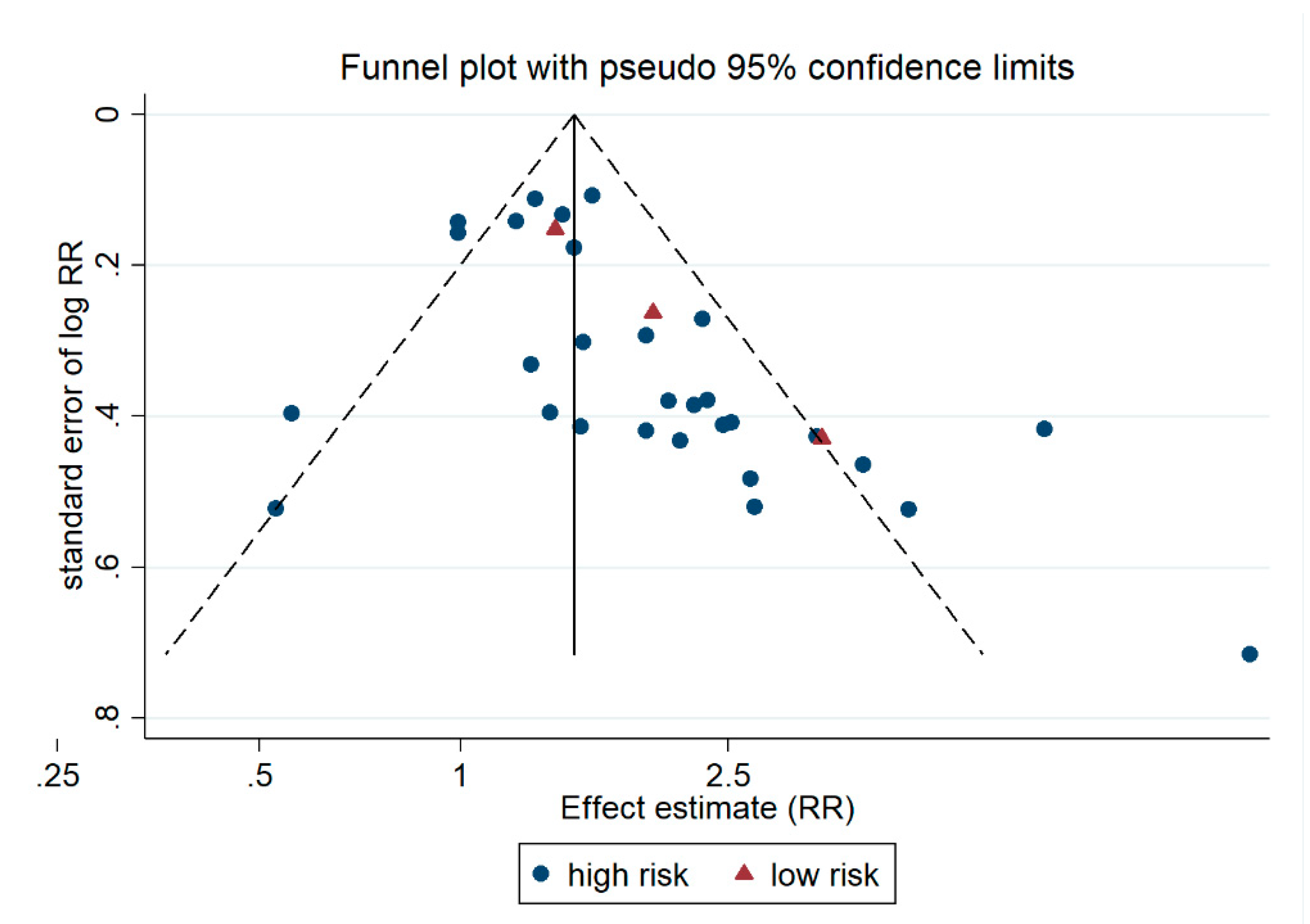
3.3. Publication Bias
3.4. Quality of Evidence Assessment
4. Discussions
4.1. Strengths and Limitations
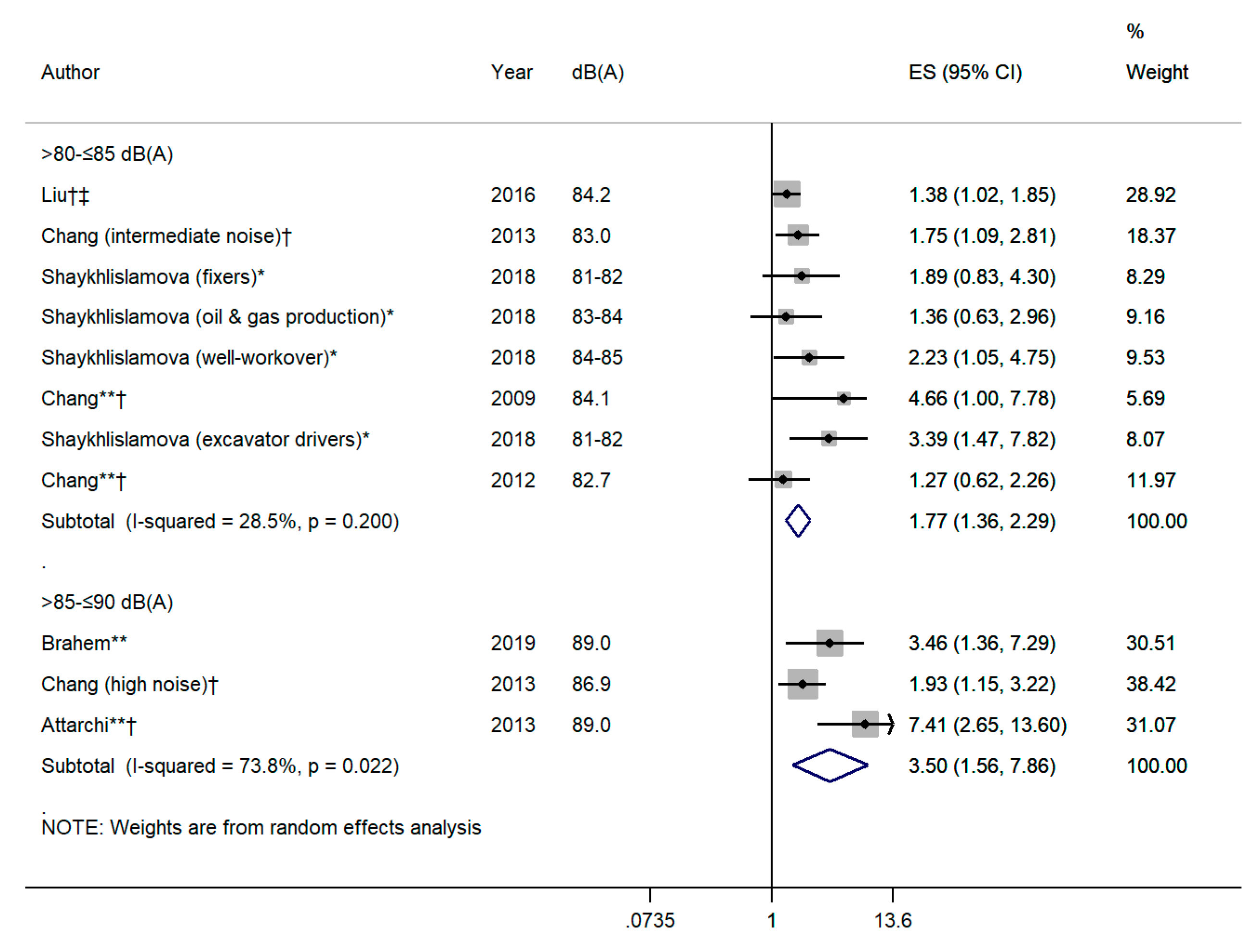
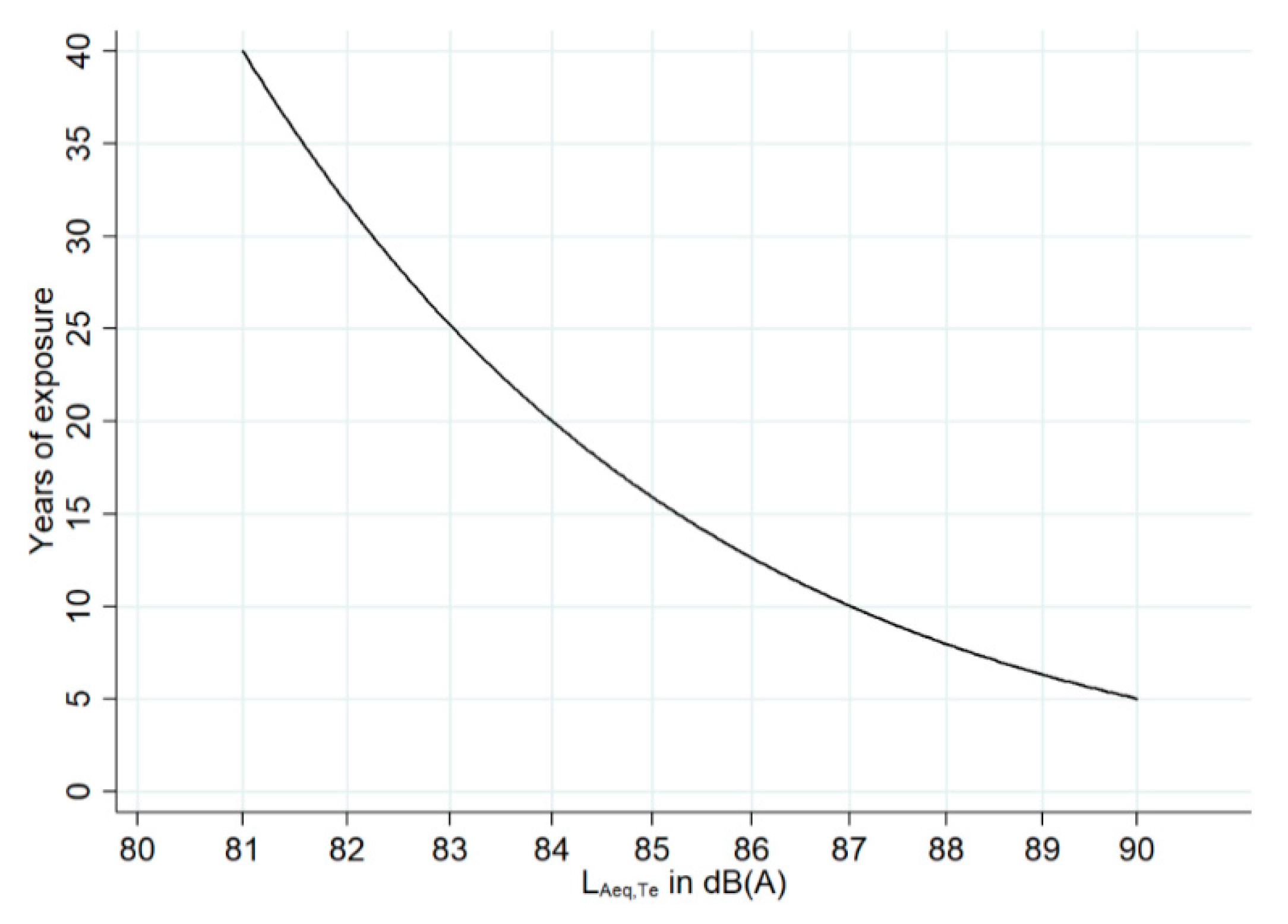
4.2. Dose-Response Relationship
4.3. Discussion of the Stokholm et al. 2013 Study
4.4. Evidence of Causality
- (a)
- (b)
- Further evidence of a dose-response relationship between the level of occupational noise exposure and risk of hypertension supports the association.
- (c)
- There is a strong association between the level of exposure to occupational noise and the risk of hypertension, which is more than three times higher for workers exposed to noise above 85 dB(A).
- (d)
- The relationship between occupational noise exposure and increased risk is consistent and it has been observed in a large number of epidemiological studies.
- (e)
- The temporal relationship between occupational noise exposure and hypertension has been established in several cohort studies.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Exposure in dB(A) | Years of Exposure | LEX,40y | RR LAeq(40y)-70 dBA (RR per 10dBA = 1.88) |
|---|---|---|---|
| 70 | 40 | 70.00 | 1.00 (Reference) |
| 80 | 5 | 70.97 | 1.06 |
| 80 | 10 | 73.98 | 1.29 |
| 80 | 15 | 75.74 | 1.44 |
| 80 | 20 | 76.99 | 1.55 |
| 80 | 30 | 78.75 | 1.74 |
| 80 | 40 | 80.00 | 1.88 |
| 81 | 5 | 71.97 | 1.13 |
| 81 | 10 | 74.98 | 1.37 |
| 81 | 15 | 76.74 | 1.53 |
| 81 | 20 | 77.99 | 1.66 |
| 81 | 30 | 79.75 | 1.85 |
| 81 | 40 | 81.00 | 2.00 |
| 82 | 5 | 72.97 | 1.21 |
| 82 | 10 | 75.98 | 1.46 |
| 82 | 15 | 77.74 | 1.63 |
| 82 | 20 | 78.99 | 1.76 |
| 82 | 30 | 80.75 | 1.97 |
| 82 | 40 | 82.00 | 2.13 |
| 83 | 5 | 73.97 | 1.28 |
| 83 | 10 | 76.98 | 1.55 |
| 83 | 15 | 78.74 | 1.74 |
| 83 | 20 | 79.99 | 1.88 |
| 83 | 30 | 81.75 | 2.10 |
| 83 | 40 | 83.00 | 2.27 |
| 84 | 5 | 74.97 | 1.37 |
| 84 | 10 | 77.98 | 1.65 |
| 84 | 15 | 79.74 | 1.85 |
| 84 | 20 | 80.99 | 2.00 |
| 84 | 30 | 82.75 | 2.24 |
| 84 | 40 | 84.00 | 2.42 |
| 85 | 5 | 75.97 | 1.46 |
| 85 | 10 | 78.98 | 1.76 |
| 85 | 15 | 80.74 | 1.97 |
| 85 | 20 | 81.99 | 2.13 |
| 85 | 30 | 83.75 | 2.38 |
| 85 | 40 | 85.00 | 2.58 |
| 86 | 5 | 76.97 | 1.55 |
| 86 | 10 | 79.98 | 1.88 |
| 86 | 15 | 81.74 | 2.10 |
| 86 | 20 | 82.99 | 2.27 |
| 86 | 30 | 84.75 | 2.54 |
| 86 | 40 | 86.00 | 2.75 |
| 87 | 5 | 77.97 | 1.65 |
| 87 | 10 | 80.98 | 2.00 |
| 87 | 15 | 82.74 | 2.24 |
| 87 | 20 | 83.99 | 2.42 |
| 87 | 30 | 85.75 | 2.70 |
| 87 | 40 | 87.00 | 2.92 |
| 88 | 5 | 78.97 | 1.76 |
| 88 | 10 | 81.98 | 2.13 |
| 88 | 15 | 83.74 | 2.38 |
| 88 | 20 | 84.99 | 2.58 |
| 88 | 30 | 86.75 | 2.88 |
| 88 | 40 | 88.00 | 3.12 |
| 89 | 5 | 79.97 | 1.88 |
| 89 | 10 | 82.98 | 2.27 |
| 89 | 15 | 84.74 | 2.54 |
| 89 | 20 | 85.99 | 2.74 |
| 89 | 30 | 87.75 | 3.07 |
| 89 | 40 | 89.00 | 3.32 |
| 90 | 5 | 80.97 | 2.00 |
| 90 | 10 | 83.98 | 2.42 |
| 90 | 15 | 85.74 | 2.70 |
| 90 | 20 | 86.99 | 2.92 |
| 90 | 30 | 88.75 | 3.27 |
| 90 | 40 | 90.00 | 3.53 |
References
- Lie, A.; Skogstad, M.; Johannessen, H.A.; Tynes, T.; Mehlum, I.S.; Nordby, K.C.; Engdahl, B.; Tambs, K. Occupational noise exposure and hearing: A systematic review. Int. Arch. Occup. Environ. Health 2016, 89, 351–372. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk, F.J. Non-auditory effects of noise in industry. Ii. A review of the literature. Int. Arch. Occup. Environ. Health 1986, 58, 325–332. [Google Scholar] [CrossRef]
- Kristensen, T.S. Cardiovascular diseases and the work environment. A critical review of the epidemiologic literature on nonchemical factors. Scand. J. Work Environ. Health 1989, 15, 165–179. [Google Scholar] [CrossRef] [PubMed]
- Van Kempen, E.E.; Kruize, H.; Boshuizen, H.C.; Ameling, C.B.; Staatsen, B.A.; de Hollander, A.E. The association between noise exposure and blood pressure and ischemic heart disease: A meta-analysis. Environ. Health Perspect. 2002, 110, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Penney, P.J.; Earl, C.E. Occupational noise and effects on blood pressure: Exploring the relationship of hypertension and noise exposure in workers. Aaohn J. 2004, 52, 476–480. [Google Scholar] [CrossRef]
- Kirby, D.A.; Herd, J.A.; Hartley, L.H.; Teller, D.D.; Rodger, R.F. Enhanced blood pressure responses to loud noise in offspring of monkeys with high blood pressure. Physiol. Behav. 1984, 32, 779–783. [Google Scholar] [CrossRef]
- Gamallo, A.; Alario, P.; Gonzalez-Abad, M.J.; Villanua, M.A. Acute noise stress, acth administration, and blood pressure alteration. Physiol. Behav. 1992, 51, 1201–1205. [Google Scholar] [CrossRef]
- Baudrie, V.; Tulen, J.H.; Blanc, J.; Elghozi, J.L. Autonomic components of the cardiovascular responses to an acoustic startle stimulus in rats. J. Auton. Pharmacol. 1997, 17, 303–309. [Google Scholar] [CrossRef]
- Engeland, W.C.; Miller, P.; Gann, D.S. Pituitary-adrenal and adrenomedullary responses to noise in awake dogs. Am. J. Physiol. 1990, 258, R672–R677. [Google Scholar] [CrossRef]
- Altura, B.M.; Altura, B.T.; Gebrewold, A.; Ising, H.; Gunther, T. Extraaural effects of chronic noise exposure on blood pressure, microcirculation and electrolytes in rats: Modulation by mg2+. Schr. Ver. Wasser Boden Lufthyg. 1993, 88, 65–90. [Google Scholar]
- Andriukin, A.A. Influence of sound stimulation on the development of hypertension. Clinical and experimental results. Cor Vasa 1961, 3, 285–293. [Google Scholar]
- Medoff, H.S.; Bongiovanni, A.M. Blood pressure in rats subjected to audiogenic stimulation. Am. J. Physiol. 1945, 143, 300–305. [Google Scholar] [CrossRef]
- Peterson, E.A.; Augenstein, J.S.; Tanis, D.C.; Augenstein, D.G. Noise raises blood pressure without impairing auditory sensitivity. Science 1981, 211, 1450–1452. [Google Scholar] [CrossRef] [PubMed]
- Rothlin, E.; Emmenegger, H.; Cerletti, A. Studies on production of audiogenic hypertension in rats. Helv. Physiol. Pharmacol. Acta 1953, 11, C25–C28. [Google Scholar] [PubMed]
- Smookler, H.H.; Goebel, K.H.; Siegel, M.I.; Clarke, D.E. Hypertensive effects of prolonged auditory, visual, and motion stimulation. Fed. Proc. 1973, 32, 2105–2110. [Google Scholar]
- Tucker, D.C.; Hunt, R.A. Effects of long-term air jet noise and dietary sodium chloride in borderline hypertensive rats. Hypertension 1993, 22, 527–534. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wu, C.C.; Chen, S.J.; Yen, M.H. Effects of noise on blood pressure and vascular reactivities. Clin. Exp. Pharmacol. Physiol. 1992, 19, 833–838. [Google Scholar] [CrossRef]
- Yeakel, E.H.; Shenkin, H.A.; Rothballer, A.B.; McCann, S.M. Blood pressures of rats subjected to auditory stimulation. Am. J. Physiol. 1948, 155, 118–127. [Google Scholar] [CrossRef]
- Burwell, A.K.; Baldwin, A.L. Do audible and ultrasonic sounds of intensities common in animal facilities affect the autonomic nervous system of rodents? J. Appl. Anim. Welf. Sci. 2006, 9, 179–200. [Google Scholar] [CrossRef]
- Said, M.A.; El-Gohary, O.A. Effect of noise stress on cardiovascular system in adult male albino rat: Implication of stress hormones, endothelial dysfunction and oxidative stress. Gen. Physiol. Biophys. 2016, 35, 371–377. [Google Scholar] [CrossRef]
- Borg, E.; Moller, A.R. Noise and blood pressure: Effect of lifelong exposure in the rat. Acta Physiol. Scand. 1978, 103, 340–342. [Google Scholar] [CrossRef] [PubMed]
- Pillsbury, H.C. Hypertension, hyperlipoproteinemia, chronic noise exposure: Is there synergism in cochlear pathology? Laryngoscope 1986, 96, 1112–1138. [Google Scholar] [CrossRef] [PubMed]
- Munzel, T.; Daiber, A.; Steven, S.; Tran, L.P.; Ullmann, E.; Kossmann, S.; Schmidt, F.P.; Oelze, M.; Xia, N.; Li, H.; et al. Effects of noise on vascular function, oxidative stress, and inflammation: Mechanistic insight from studies in mice. Eur. Heart J. 2017, 38, 2838–2849. [Google Scholar] [CrossRef] [PubMed]
- Bao, G.; Metreveli, N.; Fletcher, E.C. Acute and chronic blood pressure response to recurrent acoustic arousal in rats. Am. J. Hypertens. 1999, 12, 504–510. [Google Scholar] [CrossRef]
- Eriksson, C.; Pershagen, G.; Nilsson, M. Biological Mechanisms Related to Cardiovascular and Metabolic Effects by Environmental Noise; WHO Regional Office for Europe: Copenhangen, Denmark, 2018. [Google Scholar]
- Babisch, W. Stress hormones in the research on cardiovascular effects of noise. Noise Health 2003, 5, 1–11. [Google Scholar]
- Maschke, C.; Rupp, T.; Hecht, K. The influence of stressors on biochemical reactions--a review of present scientific findings with noise. Int. J. Hyg. Environ. Health 2000, 203, 45–53. [Google Scholar] [CrossRef]
- Fu, W.; Wang, C.; Zou, L.; Liu, Q.; Gan, Y.; Yan, S.; Song, F.; Wang, Z.; Lu, Z.; Cao, S. Association between exposure to noise and risk of hypertension: A meta-analysis of observational epidemiological studies. J. Hypertens. 2017, 35, 2358–2366. [Google Scholar] [CrossRef]
- Skogstad, M.; Johannessen, H.A.; Tynes, T.; Mehlum, I.S.; Nordby, K.C.; Lie, A. Systematic review of the cardiovascular effects of occupational noise. Occup. Med. (Oxf. UK) 2016, 66, 10–16, Corrigendum: 2016, 66, 500. [Google Scholar] [CrossRef]
- Yang, Y.; Zhang, E.; Zhang, J.; Chen, S.; Yu, G.; Liu, X.; Peng, C.; Lavin, M.F.; Du, Z.; Shao, H. Relationship between occupational noise exposure and the risk factors of cardiovascular disease in china: A meta-analysis. Medicine 2018, 97, e11720. [Google Scholar] [CrossRef]
- Tomei, G.; Fioravanti, M.; Cerratti, D.; Sancini, A.; Tomao, E.; Rosati, M.V.; Vacca, D.; Palitti, T.; Di Famiani, M.; Giubilati, R.; et al. Occupational exposure to noise and the cardiovascular system: A meta-analysis. Sci. Total Environ. 2010, 408, 681–689. [Google Scholar] [CrossRef]
- Shea, B.J.; Grimshaw, J.M.; Wells, G.A.; Boers, M.; Andersson, N.; Hamel, C.; Porter, A.C.; Tugwell, P.; Moher, D.; Bouter, L.M. Development of amstar: A measurement tool to assess the methodological quality of systematic reviews. BMC Med. Res. Methodol. 2007, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Hamel, C.; Wells, G.A.; Bouter, L.M.; Kristjansson, E.; Grimshaw, J.; Henry, D.A.; Boers, M. Amstar is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J. Clin. Epidemiol. 2009, 62, 1013–1020. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. Amstar 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.J.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 acc/aha/aapa/abc/acpm/ags/apha/ash/aspc/nma/pcna guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. Circulation 2018, 138, e426–e483. [Google Scholar]
- World Health Organization (WHO). A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis: World Health Day 2013; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 esc/esh guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the european society of cardiology and the european society of hypertension: The task force for the management of arterial hypertension of the european society of cardiology and the european society of hypertension. J. Hypertens. 2018, 36, 1953–2041. [Google Scholar]
- Ijaz, S.; Verbeek, J.; Seidler, A.; Lindbohm, M.-L.; Ojajärvi, A.; Orsini, N.; Costa, G.; Neuvonen, K. Night-shift work and breast cancer—A systematic review and meta-analysis. Scand. J. Work Environ. Health 2013, 39, 431–447. [Google Scholar] [CrossRef]
- Romero Starke, K.; Kofahl, M.; Freiberg, A.; Schubert, M.; Gross, M.L.; Schmauder, S.; Hegewald, J.; Kampf, D.; Stranzinger, J.; Nienhaus, A.; et al. The risk of cytomegalovirus infection in daycare workers: A systematic review and meta-analysis. Int. Arch. Occup. Environ. Health 2020, 93, 11–28. [Google Scholar] [CrossRef]
- Zhang, J.; Yu, K.F. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 1998, 280, 1690–1691. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 14; StataCorp LLC: College Station, TX, USA, 2015. [Google Scholar]
- Harris, R.; Bradburn, M.; Deeks, J.; Harbord, R.; Altman, D.; Sterne, J. Metan: Fixed- and random-effects meta-analysis. Stata J. 2008, 8, 3–28. [Google Scholar] [CrossRef]
- Acoustique, I.T., Ed.; International Standard. ISO 1999: Acoustics—Estimation of Noise-Induced Hearing Loss, 3rd ed. ISO/TC 43 Akustik; ISO/TC 43 Acoustics. 2013. Available online: https://www.iso.org/standard/45103.html (accessed on 27 August 2020).
- Chang, T.Y.; Wang, V.S.; Hwang, B.F.; Yen, H.Y.; Lai, J.S.; Liu, C.S.; Lin, S.Y. Effects of co-exposure to noise and mixture of organic solvents on blood pressure. J. Occup. Health 2009, 51, 332–339. [Google Scholar] [CrossRef]
- Schünemann, H.; Brożek, J.; Guyatt, G.; Oxman, A. (Eds.) Grade handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group. 2013. Available online: Guidelinedevelopment.org/handbook (accessed on 28 August 2020).
- Teixeira, L.R.; Azevedo, T.M.; Bortkiewicz, A.; Correa da Silva, D.T.; de Abreu, W.; de Almeida, M.S.; de Araujo, M.A.N.; Gadzicka, E.; Ivanov, I.D.; Leppink, N.; et al. Who/ilo work-related burden of disease and injury: Protocol for systematic reviews of exposure to occupational noise and of the effect of exposure to occupational noise on cardiovascular disease. Environ. Int. 2019, 125, 567–578. [Google Scholar] [CrossRef] [PubMed]
- Woodruff, T.J.; Sutton, P. The navigation guide systematic review methodology: A rigorous and transparent method for translating environmental health science into better health outcomes. Environ. Health Perspect. 2014, 122, 1007–1014. [Google Scholar] [CrossRef]
- Attarchi, M.; Golabadi, M.; Labbafinejad, Y.; Mohammadi, S. Combined effects of exposure to occupational noise and mixed organic solvents on blood pressure in car manufacturing company workers. Am. J. Ind. Med. 2013, 56, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Brahem, A.; Riahi, S.; Chouchane, A.; Kacem, I.; Maalel, O.E.; Maoua, M.; Guedri, S.E.; Kalboussi, H.; Chatti, S.; Debbabi, F.; et al. Impact of occupational noise in the development of arterial hypertension: A survey carried out in a company of electricity production. Annales de Cardiologie et D’angeiologie 2019, 68, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.Y.; Liu, C.S.; Young, L.H.; Wang, V.S.; Jian, S.E.; Bao, B.Y. Noise frequency components and the prevalence of hypertension in workers. Sci. Total Environ. 2012, 416, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.Y.; Hwang, B.F.; Liu, C.S.; Chen, R.Y.; Wang, V.S.; Bao, B.Y.; Lai, J.S. Occupational noise exposure and incident hypertension in men: A prospective cohort study. Am. J. Epidemiol. 2013, 177, 818–825. [Google Scholar] [CrossRef]
- Chen, L.Z.; Pang, L.J.; Fu, B.Y. Epidemiological study on the occupational noise exposure and hypertension in mechanic factory workers. Zhonghua Liu Xing Bing Xue Za Zhi 2005, 26, 897–900. [Google Scholar] [PubMed]
- De Souza, T.C.; Perisse, A.R.; Moura, M. Noise exposure and hypertension: Investigation of a silent relationship. BMC Public Health 2015, 15, 328. [Google Scholar] [CrossRef]
- Fogari, R.; Zoppi, A.; Vanasia, A.; Marasi, G.; Villa, G. Occupational noise exposure and blood pressure. J. Hypertens. 1994, 12, 475–479. [Google Scholar] [CrossRef]
- Fogari, R.; Marasi, G.; Zoppi, A.; Malamani, G.D.; Vanasia, A.; Villa, G. Community control of hypertension at work-site: Epidemiological data of the agusta project. Eur. J. Epidemiol. 1995, 11, 591–595. [Google Scholar] [CrossRef]
- Fokin, V.A.; Shlyapnikov, D.M.; Red’ko, S.V. Risk assessment of occupational and occupationally conditioned diseases connection to noise when exceeding maximum permissible levels. Russ. J. Occup. Health Ind. Ecol. 2018, 2018, 17–19. [Google Scholar] [CrossRef]
- Giordano, C.; Conticello, S.; Beatrice, F.; Montemagno, A.; Boggero, R. Non-auditory effects of environmental noise: A study of metallurgical and mechanical workers. Acta Otorhinolaryngol. Ital. 2001, 21, 281–286. [Google Scholar] [PubMed]
- Ha, M.W.; Kim, D. Long term noise exposure of steel mill workers, hearing loss and blood pressure. Korean J. Prev. Med. 1991, 24, 496–506. [Google Scholar]
- Hwang, B.F.; Chang, T.Y.; Cheng, K.Y.; Liu, C.S. Gene-environment interaction between angiotensinogen and chronic exposure to occupational noise contribute to hypertension. Occup. Environ. Med. 2012, 69, 236–242. [Google Scholar] [CrossRef]
- Jégaden, D.; Le Pluart, C.; Marie, Y.; Piquemal, B. Contribution to the study noise-high blood pressure. Concerning 455 merchant sailors aged 40–55 years. Arch. Mal. Prof. 1986, 47, 15–20. [Google Scholar]
- Liu, C.S.; Young, L.H.; Yu, T.Y.; Bao, B.Y.; Chang, T.Y. Occupational noise frequencies and the incidence of hypertension in a retrospective cohort study. Am. J. Epidemiol. 2016, 184, 120–128. [Google Scholar] [CrossRef]
- Melamed, S.; Fried, Y.; Froom, P. The interactive effect of chronic exposure to noise and job complexity on changes in blood pressure and job satisfaction: A longitudinal study of industrial employees. J. Occup. Health Psychol. 2001, 6, 182–195. [Google Scholar] [CrossRef]
- Pang, L.J.; Chen, L.Z.; Fu, B.Y. Prevalence and influence factors of hypertension among mechanic factory workers. Zhong Nan Da Xue Xue Bao Yi Xue Ban J. Cent. South Univ. Med Sci. 2005, 30, 276–279. [Google Scholar]
- Parameswarappa, S.B.; Narayana, J. Impact of noise on hearing and hypertension among workers in steel industry. Int. J. Curr. Microbiol. App. Sci 2015, 4, 124–133. [Google Scholar]
- Pilawska, H.; Mikulski, T.; Rusin, J.; Soroka, M.; Wysocki, K. Effect of acoustic microclimate prevailing in shipyards on the health of workers. Med. Pr. 1977, 28, 441–447. [Google Scholar]
- Shaykhlislamova, E.R.; Volgareva, A.D.; Obukhova, M.P.; Gimranova, G.G.; Karimova, L.K.; Valeeva, E.T. Prevalence of blood circulation diseases among workers exposed to occupational noise in mineral extraction and their work-relatedness. Sib. Sci. Med. J. 2018, 38, 137–144. [Google Scholar]
- Siagian, M.; Basuki, B.; Kusmana, D. High intensity interior aircraft noise increases the risk of high diastolic blood pressure in indonesian air force pilots. Med. J. Indones 2009, 18, 276–282. [Google Scholar] [CrossRef][Green Version]
- Souto Souza, N.S.; Carvalho, F.M.; de Cassia Pereira Fernandes, R. Arterial hypertension among oil-drilling workers exposed to noise. Cadernos Saude Publica 2001, 17, 1481–1488. [Google Scholar]
- Stokholm, Z.A.; Bonde, J.P.; Christensen, K.L.; Hansen, A.M.; Kolstad, H.A. Occupational noise exposure and the risk of hypertension. Epidemiology (Camb. Mass) 2013, 24, 135–142. [Google Scholar] [CrossRef]
- Talijancic, A.; Mustac, M. Arterial hypertension in workers exposed to occupational noise. Arhiv za Higijenu Rada i Toksikologiju 1989, 40, 415–420. [Google Scholar]
- Zhao, Y.; Zhang, S.; Selvin, S.; Spear, R.C. A dose-response relationship for occupational noise-induced hypertension. Schr. Ver. Wasser Boden Lufthyg. 1993, 88, 189–207. [Google Scholar]
- Zhao, Y.M.; Zhang, S.Z.; Selvin, S.; Spear, R.C. A dose response relation for noise induced hypertension. Br. J. Ind. Med. 1991, 48, 179–184. [Google Scholar] [CrossRef][Green Version]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Van Kempen, E.; Casas, M.; Pershagen, G.; Foraster, M. Who environmental noise guidelines for the european region: A systematic review on environmental noise and cardiovascular and metabolic effects: A summary. Int. J. Environ. Res. Public Health 2018, 15, 379. [Google Scholar] [CrossRef]
- Fouriaud, C.; Jacquinet-Salord, M.C.; Degoulet, P.; Aime, F.; Lang, T.; Laprugne, J.; Main, J.; Oeconomos, J.; Phalente, J.; Prades, A. Influence of socioprofessional conditions on blood pressure levels and hypertension control. Epidemiologic study of 6665 subjects in the paris district. Am. J. Epidemiol. 1984, 120, 72–86. [Google Scholar] [CrossRef]
- Hill, A.B. The environment and disease: Association or causation? Proc. R. Soc. Med. 1965, 58, 295–300. [Google Scholar] [CrossRef] [PubMed]

| Inclusion | Exclusion | |
|---|---|---|
| Population (P) | General working population | Children and animals |
| Exposure (E) | Quantified occupational noise exposure in dB | No quantification of occupational noise exposure in dB |
| Comparison (C) | General working population or specific groups of workers with noise exposures LEX,8h ≤80 dB | No adequate comparison group |
| Outcome (O) | Primary arterial hypertension (ICD10 = I10) defined using at least one of the following criteria:
| No identification/diagnosis of hypertension using the definitions outlined in the inclusion criteria column |
| Study Design (S) | cohort, case-control, cross-sectional, case-cohort, nested-case-control studies with a response ≥10% | qualitative studies, case descriptions, ecological studies, experimental studies, letters to the editor, comments/editorials, congress abstracts/posters, reviews; epidemiological studies not reporting response or with response <10% |
| Study | Study Type | Major Domains | Minor Domains | OVERALL | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Recruitment & Follow-up (Cohort) | Exposure Definition & Measurement | Outcome Assessment & Validation | Con-Foun-Ding & Effect Modification | Analysis Method | Chronology | Assessor Blinding | Funding | Conflict of Interest | |||
| Attarchi 2013 [48] | CS |  |  |  |  |  |  |  |  |  |  |
| Brahem 2019 [49] | CS |  |  |  |  |  |  |  |  |  |  |
| Chang 2009 [44] | CS |  |  |  |  |  |  |  |  |  |  |
| Chang 2012 [50] | CS |  |  |  |  |  |  |  |  |  |  |
| Chang 2013 [51] | Co |  |  |  |  |  |  |  |  |  |  |
| Chen 2005 [52,63] | CS |  |  |  |  |  |  |  |  |  |  |
| De Souza 2015 [53] | CS |  |  |  |  |  |  |  |  |  |  |
| Fogari 1994 [54] § | CS |  |  |  |  |  |  |  |  |  |  |
| Fogari 1995 [55] | CS |  |  |  |  |  |  |  |  |  |  |
| Fokin 2018 [56] | Co |  |  |  |  |  |  |  |  |  |  |
| Giordano 2001 [57] | CS |  |  |  |  |  |  |  |  |  |  |
| Ha & Kim 1991 [58] | CS |  |  |  |  |  |  |  |  |  |  |
| Hwang 2012 [59] | Co |  |  |  |  |  |  |  |  |  |  |
| Jegaden 1986 [60] | CS |  |  |  |  |  |  |  |  |  |  |
| Liu 2016 [61] | Co |  |  |  |  |  |  |  |  |  |  |
| Melamed 2001 [62] | Co |  |  |  |  |  |  |  |  |  |  |
| Parameswarappa 2015 [64] | CS |  |  |  |  |  |  |  |  |  |  |
| Pilawska 1977 [65] | CS |  |  |  |  |  |  |  |  |  |  |
| Shaykhlislamova 2018 [66] | CS |  |  |  |  |  |  |  |  |  |  |
| Siagian 2009 [67] | Nested CC |  |  |  |  |  |  |  |  |  |  |
| Souto Souza 2001 [68] | CS |  |  |  |  |  |  |  |  |  |  |
| Stokholm 2013 [69] | Co |  |  |  |  |  |  |  |  |  |  |
| Talijancic 1989 [70] | CS |  |  |  |  |  |  |  |  |  |  |
| Zhao 1991 [71,72] | CS |  |  |  |  |  |  |  |  |  |  |
 Low Risk;
Low Risk;  Unclear Risk;
Unclear Risk;  High Risk; § not in meta-analysis.
High Risk; § not in meta-analysis.| Question: Are workers chronically exposed to noise at work with an exposure intensity of >80 dB(A) at an elevated risk for developing arterial hypertension? | ||||||||||
| № of Studies (Participants) | 1. Study limitations | 2. Indirectness | 3. Inconsistency | 4. Imprecision | 5. Publication Bias | 6. Effect size | 7. Dose-response Gradient | 8. Residual Confounding | Effect Size | Certainty |
| 23 observational studies (n = 171 985)1 | not serious2 | not serious | not serious3 | not serious | Detected4 ↓ | Detected5 ↑ | Detected6 ↑ | no | RR 1.72 (1.48 to 2.01) | ⨁⨁⨁ HIGH |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bolm-Audorff, U.; Hegewald, J.; Pretzsch, A.; Freiberg, A.; Nienhaus, A.; Seidler, A. Occupational Noise and Hypertension Risk: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6281. https://doi.org/10.3390/ijerph17176281
Bolm-Audorff U, Hegewald J, Pretzsch A, Freiberg A, Nienhaus A, Seidler A. Occupational Noise and Hypertension Risk: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2020; 17(17):6281. https://doi.org/10.3390/ijerph17176281
Chicago/Turabian StyleBolm-Audorff, Ulrich, Janice Hegewald, Anna Pretzsch, Alice Freiberg, Albert Nienhaus, and Andreas Seidler. 2020. "Occupational Noise and Hypertension Risk: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 17, no. 17: 6281. https://doi.org/10.3390/ijerph17176281
APA StyleBolm-Audorff, U., Hegewald, J., Pretzsch, A., Freiberg, A., Nienhaus, A., & Seidler, A. (2020). Occupational Noise and Hypertension Risk: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 17(17), 6281. https://doi.org/10.3390/ijerph17176281








