Challenges of Testing COVID-19 Cases in Bangladesh
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Data and Analysis
2.2.1. COVID-19-Related Quantitative Data
2.2.2. Qualitative Information
2.2.3. GIS Data
3. Results
3.1. Dynamics of the COVID-19 Situation in Bangladesh
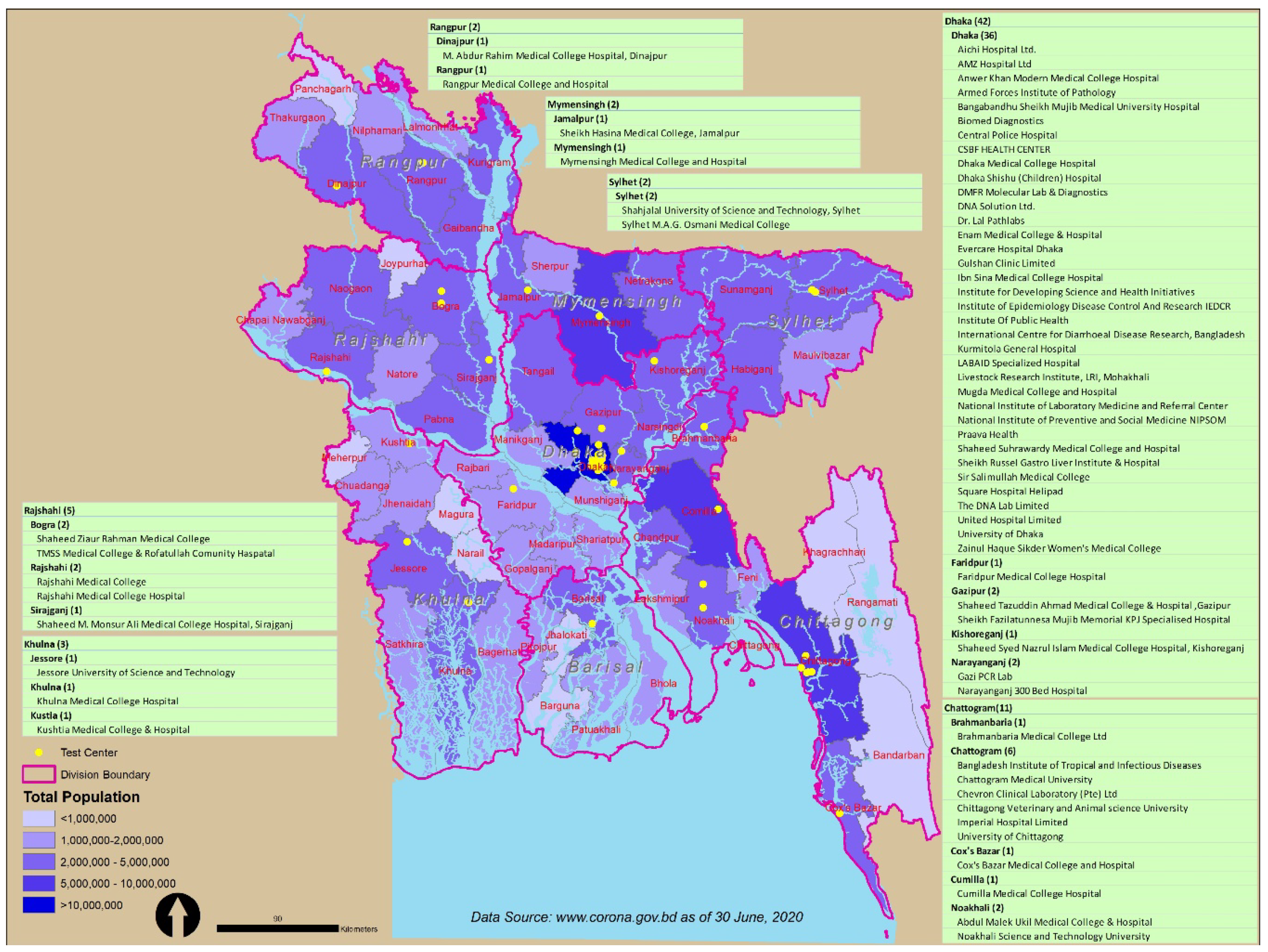
3.2. Available Facilities for Tackling COVID-19
3.3. Scarcity, Disparity, and Centrality of Testing Facilities
4. Discussion
4.1. Why Do We Need to Test Widely in Diverse Geographic Locations?
4.2. Recommendations for Prioritizing Spatial Decentralization of Testing Capabilities
- (i)
- Enhancing testing capacity at all geographic locations based on population density by removing regulatory and trading barriers;
- (ii)
- Stipulating hospital resources in the worst affected geographic locations so that people may receive necessary treatments immediately when required;
- (iii)
- Encouraging the decentralization of testing facilities into the more local area so that people do not need to travel to other cities, as this may spread the virus quickly in and out of the facility zones;
- (iv)
- Using cell phones to survey, inform, and pre-screen symptoms related to COVID-19 and advising citizens to attend nearby testing facilities where there are ample cases;
- (v)
- If there are shortages of a hospital, clinics, and testing facilities, the government may make a requisition of schools and similar buildings while repurposing them as testing and quarantine facilities throughout the country; the usages of primary schools as cyclone/emergency shelters during cyclone hazard in the coastal area of Bangladesh is likely [33].
- (vi)
- Rapidly scale up the production and distribution of masks at different geographic locations and inspire people to wear them in public places;
- (vii)
- Collaborate with and enhance networks among the testing facilities so that they can share their resources according to the needs of different geographic locations;
- (viii)
- Encourage volunteers to support local-level facilities in order to enhance testing capacity. However, necessary protective measures are highly recommended to the volunteers so that they may not work as an agent of community spread into their local neighborhoods;
- (ix)
- Update the database every day at all testing facilities. This will demonstrate the need for additional resources at different locations. Moreover, the local government may take additional regulatory measures (lockdown in any specific area for a few days) to contest community spread locally;
- (x)
- A critical recommendation is to introduce COVID-19 testing centers in each district geographically (i.e., at district headquarter) in order to increase testing capacities at the local level. This will ensure understanding of the worst-affected areas, and future strategies can be taken immediately upon data availability of infected patients.
- (xi)
- Providing relief aid for poor people where there are more COVID-19-infected people in order to maintain a home isolation period of 2 weeks.
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- John Hopkins University. Covid-19 Dashboard by the Center of System Sciences and Engineering at John Hopkins University [Internet]. 2020, Volume 2507, pp. 1–9. Available online: https://coronavirus.jhu.edu/map.html (accessed on 10 June 2020).
- Rodríguez-Morales, A.J.; Bonilla-Aldana, D.K.; Tiwari, R.; Sah, R.; Rabaan, A.A.; Dhama, K. COVID-19, an Emerging Coronavirus Infection: Current Scenario and Recent Developments—An Overview. J. Pure Appl. Microbiol. 2020, 14, 5–12. [Google Scholar] [CrossRef]
- Collins, A.E. Advancing the Disaster and Development Paradigm. Int. J. Disaster Risk Sci. 2018, 9, 486–495. [Google Scholar] [CrossRef]
- Kappes, M.S.; Papathoma-Köhle, M.; Keiler, M. Assessing physical vulnerability for multi-hazards using an indicator-based methodology. Appl. Geogr. 2012, 32, 577–590. [Google Scholar] [CrossRef]
- Yang, P.; Wang, X. COVID-19: A new challenge for human beings. Cell. Mol. Immunol. 2020, 17, 555–557. [Google Scholar] [CrossRef] [PubMed]
- Velavan, T.P.; Meyer, C.G. The COVID-19 epidemic. Trop. Med. Int. Health 2020, 25, 278–280. [Google Scholar] [CrossRef]
- Hsiang, S.; Allen, D.; Annan-Phan, S.; Bell, K.; Bolliger, I.; Chong, T.; Druckenmiller, H.; Huang, L.Y.; Hultgren, A.; Krasovich, E.; et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 2020, 584, 1–9. [Google Scholar] [CrossRef]
- Bedford, J.; Enria, D.; Giesecke, J.; Heymann, D.L.; Ihekweazu, C.; Kobinger, G.; Lane, H.C.; Memish, Z.; Oh, M.-D.; Sall, A.A.; et al. COVID-19: Towards controlling of a pandemic. Lancet 2020, 395, 1015–1018. [Google Scholar] [CrossRef]
- Watkins, J. Preventing a COVID-19 pandemic. BMJ 2020, 368, m810. [Google Scholar] [CrossRef]
- Nicola, M.; O’Neill, N.; Sohrabi, C.; Khan, M.; Agha, M.; Agha, R. Evidence based management guideline for the COVID-19 pandemic—Review article. Int. J. Surg. 2020, 77, 206–216. [Google Scholar] [CrossRef]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar]
- Islam, M.S.; Rahman, K.M.; Sun, Y.; Qureshi, M.O.; Abdi, I.; Chughtai, A.A.; Seale, H. Examining the current intelligence on COVID-19 and infection prevention and control strategies in health settings: A global analysis. Infect. Control Hosp. Epidemiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Krzysztofik, R.; Kantor-Pietraga, I.; Spórna, T. Spatial and functional dimensions of the COVID-19 epidemic in Poland. Eurasian Geogr. Econ. 2020, 1–14. [Google Scholar] [CrossRef]
- Huang, R.; Liu, M.; Ding, Y. Spatial-temporal distribution of COVID-19 in China and its prediction: A data-driven modeling analysis. J. Infect. Dev. Ctries. 2020, 14, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Li, Q.; Gao, S.; Kang, Y.; Shi, X. Mitigating COVID-19 outbreak via high testing capacity and strong transmission-intervention in the United States. MedRxiv 2020. [Google Scholar] [CrossRef]
- Chen, Y.; Jiao, J.; Bai, S.; Lindquist, J. Modeling the Spatial Factors of COVID-19 in New York City. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Algaissi, A.A.; Alharbi, N.K.; Hassanain, M.; Hashem, A.M. Preparedness and response to COVID-19 in Saudi Arabia: Building on MERS experience. J. Infect. Public Health 2020, 13, 834–838. [Google Scholar] [CrossRef]
- Ruktanonchai, A.N.W.; Floyd, J.R.; Lai, S.; Ruktanonchai, C.W. Assessing the impact of coordinated COVID-19 exit strategies across Europe Affiliations. Science 2020. [Google Scholar] [CrossRef]
- Raoofi, A.; Takian, A.; Sari, A.A.; Olyaeemanesh, A.; Haghighi, H.; Aarabi, M. COVID-19 Pandemic and Comparative Health Policy Learning in Iran. Arch. Iran. Med. 2020, 23, 220–234. [Google Scholar] [CrossRef]
- Ihekweazu, C.; Agogo, E. Africa’s response to COVID-19. BMC Med. 2020, 1, 8–20. [Google Scholar] [CrossRef]
- Pedrosa, N.L.; de Albuquerque, N.L.S. Spatial analysis of COVID-19 cases and intensive care beds in the state of Ceará, Brazil. Cienc Saude Coletiva 2020, 25, 2461–2468. [Google Scholar] [CrossRef]
- Fanelli, D.; Piazza, F. Analysis and forecast of COVID-19 spreading in China, Italy and France. Chaos Solitons Fractals 2020, 134, 109761. [Google Scholar] [CrossRef] [PubMed]
- Shim, E.; Tariq, A.; Choi, W.; Lee, Y.; Chowell, G. Transmission potential and severity of COVID-19 in South Korea. Int. J. Infect. Dis. 2020, 93, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.; Kupferschmidt, K. Countries test tactics in ‘war’ against COVID-19. Science 2020, 367, 1287–1288. [Google Scholar] [CrossRef] [PubMed]
- Desmet, K.; Wacziarg, R. Understanding Spatial Variation in Covid-19 across the United States [Internet]. NBER Working Paper. 2020, Volume 53, pp. 1–9. Available online: https://www.anderson.ucla.edu/faculty_pages/romain.wacziarg/downloads/2020_covid.pdf (accessed on 20 May 2020).
- Karaye, I.M.; Horney, J.A. The Impact of Social Vulnerability on COVID-19 in the U.S.: An Analysis of Spatially Varying Relationships. Am. J. Prev. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, S.; Karim, T.; Alam, S. The Health Care System in Bangladesh: An Insight into Health Policy, Law and Governance Good Governance in Healthcare. Aust. J. Asian Law 2020, 20, 1–19. [Google Scholar]
- Mahmood, S.A.I. Health systems in Bangladesh. Health Syst. Policy Res. 2012, 1, 1–4. [Google Scholar] [CrossRef]
- Corburn, J.; Vlahov, D.; Mberu, B.; Riley, L.; Caiaffa, W.T.; Rashid, S.F.; Ko, A.I.; Patel, S.; Jukur, S.; Martínez-Herrera, E.; et al. Slum Health: Arresting COVID-19 and Improving Well-Being in Urban Informal Settlements. J. Urban Hered. 2020, 97, 348–357. [Google Scholar] [CrossRef] [PubMed]
- Truelove, S.; Abrahim, O.; Altare, C.; Lauer, S.A.; Grantz, K.H.; Azman, A.S.; Spiegel, P. The potential impact of COVID-19 in refugee camps in Bangladesh and beyond: A modeling study. PLoS Med. 2020, 17, e1003144. [Google Scholar] [CrossRef]
- Kumar, J.; Sahoo, S.; Bharti, B.; Walker, S. Spatial distribution and impact assessment of COVID-19 on human health using geospatial technologies in India Spatial distribution and impact assessment of COVID-19 on human health using geospatial technologies in India. Int. J. Multidiscip. Res. Dev. 2020, 7, 57–64. [Google Scholar]
- Chakraborty, I.; Maity, P. COVID-19 outbreak: Migration, effects on society, global environment and prevention. Sci. Total. Environ. 2020, 728, 138882. [Google Scholar] [CrossRef]
- Mallick, B. Cyclone shelters and their locational suitability: An empirical analysis from coastal Bangladesh. Disasters 2014, 38, 654–671. [Google Scholar] [CrossRef] [PubMed]
- Hamidi, S.; Sabouri, S.; Ewing, R. Does Density Aggravate the COVID-19 Pandemic? J. Am. Plan. Assoc. 2020, 1–15. [Google Scholar] [CrossRef]
- Binns, C.; Low, W.Y.; Kyung, L.M. The COVID-19 Pandemic: Public Health and Epidemiology. Asia-Pac. J. Public Health 2020. [Google Scholar] [CrossRef] [PubMed]
- Julka-Anderson, N. How COVID-19 is testing and evolving our communication skills. J. Med. Imaging Radiat. Sci. 2020. [Google Scholar] [CrossRef]
- World Health Organization. Preparedness, Prevention and Control of Coronavirus Disease (COVID-19) for Refugees and Migrants in Non-Camp Settings; WHO: Geneva, Switzerland, 2020; pp. 1–6. [Google Scholar]
- Hossain, M.; Hossain, S.; Uddin, M. Renewable energy: Prospects and trends in Bangladesh. Renew. Sustain. Energy Rev. 2017, 70, 44–49. [Google Scholar] [CrossRef]
- Timsina, J.; Wolf, J.; Guilpart, N.; van Bussel, L.G.; Grassini, P.; van Wart, J.; Hossain, A.; Rashid, H.; Islam, S.; van Ittersum, M. Can Bangladesh produce enough cereals to meet future demand? Agric. Syst. 2018, 163, 36–44. [Google Scholar] [CrossRef]
- United Nations. United Nations Department of Economic and Social Affairs [Internet]. World Population Prospects. 2015. Available online: http://esa.un.org/wpp/unpp/panel_population.htm (accessed on 23 May 2020).
- Call, M.A.; Gray, C.; Yunus, M.; Emch, M. Disruption, not displacement: Environmental variability and temporary migration in Bangladesh. Glob. Environ. Chang. 2017, 46, 157–165. [Google Scholar] [CrossRef]
- National Food Policy Capacity Strengthening Programme. In Adapting Social Safety Net Programs to Climate Change Shocks: Issues and Options for Bangladesh; Ministry of Food and Disaster Management: Dhaka, Bangladesh, 2015; pp. 1–4.
- Anwar, B.; Xiao, Z.; Akter, S.; Rehman, R.U. Sustainable Urbanization and Development Goals Strategy through Public–Private Partnerships in a South-Asian Metropolis. Sustainability 2017, 9, 1940. [Google Scholar] [CrossRef]
- Domman, D.; Chowdhury, F.; Khan, A.I.; Dorman, M.J.; Mutreja, A.; Uddin, M.I.; Paul, A.; Begum, Y.A.; Charles, R.C.; Calderwood, S.B.; et al. Defining endemic cholera at three levels of spatiotemporal resolution within Bangladesh. Nat. Genet. 2018, 50, 951–955. [Google Scholar] [CrossRef]
- Nissan, H.; Burkart, K.; de Perez, E.C.; van Aalst, M.; Mason, S.J. Defining and Predicting Heat Waves in Bangladesh. J. Appl. Meteorol. Clim. 2017, 56, 2653–2670. [Google Scholar] [CrossRef]
- Parnini, S.N. Civil Society and Good Governance in Bangladesh. Asian J. Politi. Sci. 2006, 14, 189–211. [Google Scholar] [CrossRef]
- Doza, B.; Shammi, M.; Bahlman, L.; Islam, A.R.T.; Rahman, M. Psychosocial and Socio-Economic Crisis in Bangladesh Due to COVID-19 Pandemic: A Perception-Based Assessment. Front. Public Health 2020, 8, 341. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.D.-U.; Doza, B.; Khan, R.M.; Haque, A.; Mamun, M.A. Exploring COVID-19 stress and its factors in Bangladesh: A perception-based study. Heliyon 2020, 6. Available online: https://www.sciencedirect.com/science/article/pii/S2405844020312433 (accessed on 15 July 2020). [CrossRef] [PubMed]
- Monjur, M.R.; Hassan, Z. Early phases of COVID-19 management in a low-income country: Bangladesh. Infect. Control. Hosp. Epidemiol. 2020, 1. Available online: https://www.cambridge.org/core/journals/infection-control-and-hospital-epidemiology/article/early-phases-of-covid19-management-in-a-lowincome-country-bangladesh/41D2E52D802C3B7877A3512A071B0F3A (accessed on 1 July 2020). [CrossRef] [PubMed]
- Islam, S.; Ira, J.I.; Kabir, K.A.; Kamrujjaman, M. COVID-19 Epidemic Compartments Model and Bangladesh. Preprints 2020. [Google Scholar] [CrossRef]
- Ramachandran, S. The COVID-19 Catastrophe in Bangladesh, The Diplomat, April 29. Available online: https://thediplomat.com/2020/04/the-covid-19-catastrophe-in-bangladesh/ (accessed on 25 June 2020).






| Particulars | Details | Values |
|---|---|---|
| Centers and helplines | No. of testing centers | 68 |
| National call centers | 330 | |
| Health portal | 16263 | |
| National helpline | 109 | |
| Category of medical staff | Ayurvedic Medicine Centers (AMC) | 2 |
| Dental Surgeon | 6 | |
| Field Staff | 168 | |
| Medical Technologist | 208 | |
| Nurse | 824 | |
| Other (not elsewhere classified) | 260 | |
| Physician | 990 | |
| Support Staff | 566 | |
| Total number of facilities available up to 6 July 2020 | Apron/gown | 76,301 |
| Gloves—examination | 490,551 | |
| Gloves—surgical | 472,472 | |
| Head/face/eye shield | 1,234,726 | |
| Masks | 3,128,842 | |
| Personal Protective Equipment (PPE )kit | 1,169,728 | |
| Sanitizer | 190,755 | |
| Shoe protector | 66,809 |
| Division | Area | Population 2011 BBS | Density 2011 BBS | No. of Testing Facilities | People per Testing Center | Test on June 12 2020 | Total Test up to June 12 2020 | Tests in Million |
|---|---|---|---|---|---|---|---|---|
| Barisal | 13,225.2 | 8,325,666 | 613 | 1 | 8,325,666 | 234 | 10,900 | 1309 |
| Chattogram | 33,908.6 | 29,145,000 | 831 | 11 | 2,649,545 | 2917 | 84,281 | 2892 |
| Dhaka | 20,593.7 | 36,433,505 | 1751 | 42 | 867,464 | 11,850 | 531,488 | 14588 |
| Khulna | 22,284.2 | 15,687,759 | 699 | 3 | 5,229,253 | 735 | 29,781 | 1898 |
| Mymensingh | 10,584.1 | 11,370,000 | 1074 | 2 | 5,685,000 | 998 | 33,426 | 2940 |
| Rajshahi | 18,153.1 | 18,485,858 | 1007 | 5 | 3,697,172 | 846 | 31,694 | 1714 |
| Rangpur | 16,185.0 | 15,787,758 | 960 | 2 | 7,893,879 | 376 | 24,540 | 1554 |
| Sylhet | 12,635.2 | 9,807,000 | 779 | 2 | 4,903,500 | 470 | 20,350 | 2075 |
| Total | 147,569.1 | 145,042,546 | 983 | 68 | 2,132,979 | 18,426 | 766,460 | 5284 |
| Division | The Average Number of Days to Receive COVID-19 Test Results |
|---|---|
| Barisal | 8 days |
| Chattogram | 5 days |
| Dhaka | 5 days |
| Khulna | 10 days |
| Mymensingh | 6 days |
| Rajshahi | 6 days |
| Rangpur | 7 days |
| Sylhet | 5 days |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rahaman, K.R.; Mahmud, M.S.; Mallick, B. Challenges of Testing COVID-19 Cases in Bangladesh. Int. J. Environ. Res. Public Health 2020, 17, 6439. https://doi.org/10.3390/ijerph17186439
Rahaman KR, Mahmud MS, Mallick B. Challenges of Testing COVID-19 Cases in Bangladesh. International Journal of Environmental Research and Public Health. 2020; 17(18):6439. https://doi.org/10.3390/ijerph17186439
Chicago/Turabian StyleRahaman, Khan Rubayet, Md. Sultan Mahmud, and Bishawjit Mallick. 2020. "Challenges of Testing COVID-19 Cases in Bangladesh" International Journal of Environmental Research and Public Health 17, no. 18: 6439. https://doi.org/10.3390/ijerph17186439
APA StyleRahaman, K. R., Mahmud, M. S., & Mallick, B. (2020). Challenges of Testing COVID-19 Cases in Bangladesh. International Journal of Environmental Research and Public Health, 17(18), 6439. https://doi.org/10.3390/ijerph17186439







