Non-Communicable Diseases-Related Stigma: A Mixed-Methods Systematic Review
Abstract
:1. Introduction
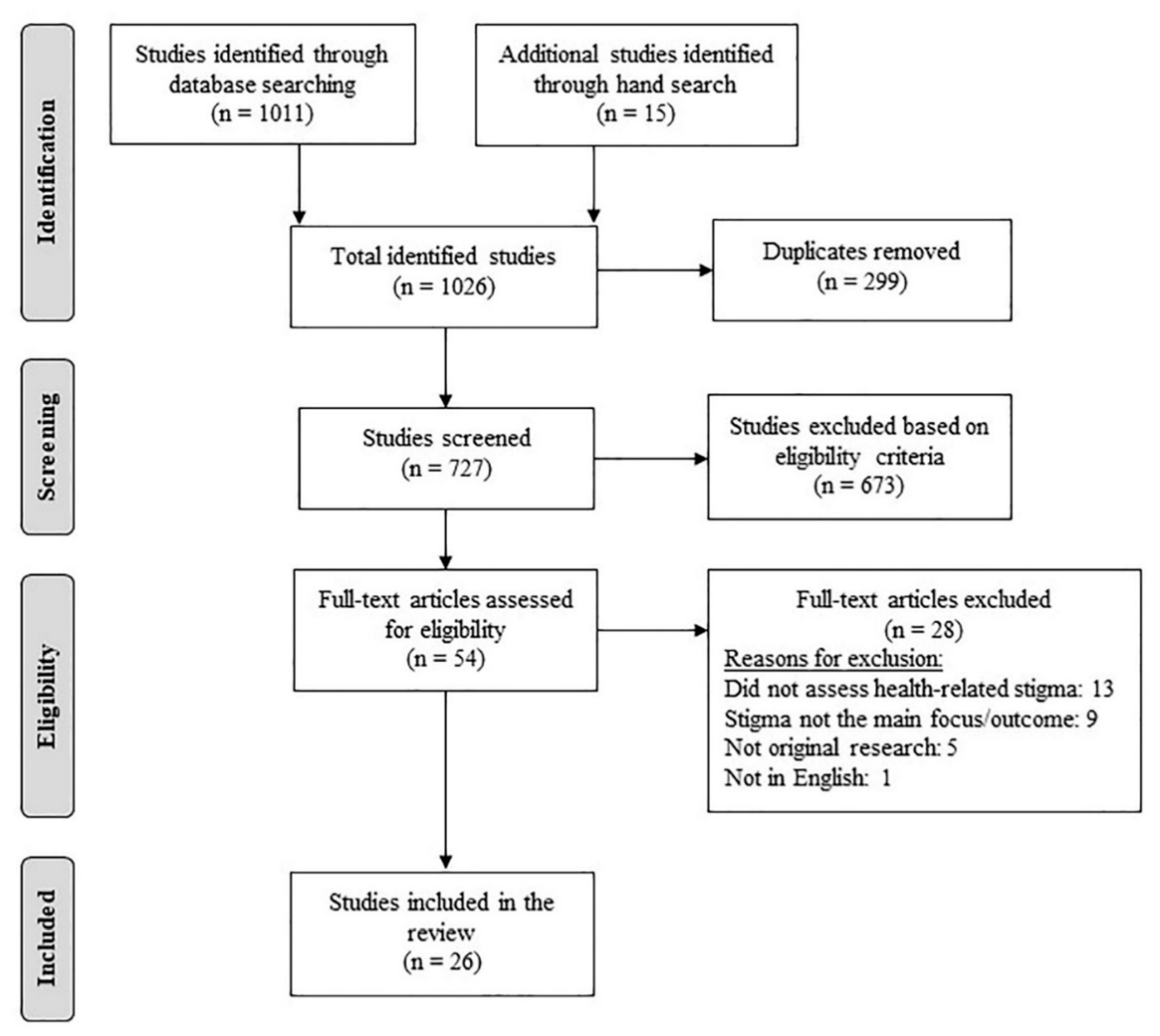
2. Methods
2.1. Search Strategy
2.2. Article Search
2.2.1. Inclusion Criteria
- Peer-reviewed articles in English;
- Studies on stigmatized persons living with one of the following four NCDs: cancers, CVDs, CRDs, and diabetes;
- Health-related stigma being the main focus of the study (qualitative) or the dependent variable (quantitative).
2.2.2. Exclusion Criteria
- Not original research (e.g., review, editorial, opinion pieces, commentary, protocol, etc.)
2.3. Data Extraction
2.4. Data Synthesis
2.4.1. Quantitative Synthesis
2.4.2. Qualitative Synthesis
- We used Pryor and Reeder’s [2] conceptual model of stigma to categorize the sources of stigma into two groups—structural and societal actors (public).
- We re-categorized the experiences/manifestations of stigma as per Scambler’s hidden distress model of stigma [20,26] into enacted stigma and felt stigma. We further extended the concept of felt stigma as per Weiss [53] and Tabah [54] into perceived stigma (perceptions about how societal actors negatively view and judge those with the health condition), internalized stigma (acceptance of stigmatizing social views and resultant feeling of shame for having the disease), and anticipated stigma (fear of encountering enacted stigma because of one’s health condition). In this review, perceived stigma and anticipated stigma are categorized as two distinct manifestations of felt stigma, the former arising from the awareness of stigma in society and the perception of stigmatization as a result of it, and the latter from anticipation and fear of discrimination [21,55]. Further, as per the conceptualization of stigma by Moore [55] and Weiss [53], in this study, internalized stigma is not confounded as self-stigma but as one of its components related to endorsement/acceptance of stereotypes and feelings of devaluation as a result of it. In this review, we will not specifically discuss self-stigma as a separate category, but reference it as a broader construct as described by Corrigan [17] that encompasses concepts of awareness of social norms and stereotypes, acceptance, endorsement, and application of those in one’s life, and the resultant consequences.
- Further, we expanded the consequences of stigma to include social, psychological, behavioral, and medical consequences.
- We also categorized the mitigating strategies into two distinct groups—coping strategies (internal/personal) and support/resources (external).
2.4.3. Integrative Synthesis
2.5. Quality Assessment
3. Results
3.1. Types of Stigma and Definitions
3.2. Stigma Prevalence/Level, Tools, and Observed Correlates
3.3. Sources of Stigma
3.4. Biopsychosocial Mechanisms Driving NCD-Related Stigma
3.5. Manifestations of NCD-Related Stigma
3.6. Consequences of NCD-Related Stigma
3.7. Mitigating Factors/Strategies for NCD-Related Stigma
3.8. Quality of Evidence
4. Discussion
4.1. Research Gaps and Suggestions for the Future
4.2. Limitations
4.3. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Global Health Observatory (GHO) Data: NCD Mortality and Morbility. Available online: http://www.who.int/gho/ncd/mortality_morbidity/en/ (accessed on 12 February 2020).
- Pryor, J.B.; Reeder, G.D. Hiv-related stigma. In Hiv/Aids in the Post-Haart Era: Manifestations, Treatment, and Epidemiology; Hall, J.C., Hall, B.J., Cockerell, C.J., Eds.; PMPH USA: Shelton, CT, USA, 2011; pp. 790–806. [Google Scholar]
- Boutayeb, A.; Boutayeb, S.; Boutayeb, W. Multi-morbidity of non communicable diseases and equity in who eastern mediterranean countries. Int. J. Equity Health 2013, 12, 60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Engelgau, M.; Rosenhouse, S.; El-Saharty, S.; Mahal, A. The economic effect of noncommunicable diseases on households and nations: A review of existing evidence. J. Health Commun. 2011, 16 (Suppl. 2), 75–81. [Google Scholar] [CrossRef]
- Kien, V.D.; Minh, H.V.; Ngoc, N.B.; Phuong, T.B.; Ngan, T.T.; Quam, M.B. Inequalities in household catastrophic health expenditure and impoverishment associated with noncommunicable diseases in chi linh, hai duong, vietnam. Asia Pac. J. Public Health 2017, 29, 35S–44S. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- Van Brakel, W.H. Measuring health-related stigma—A literature review. Psychol. Health Med. 2006, 11, 307–334. [Google Scholar] [CrossRef] [PubMed]
- Berger, B.E.; Kapella, M.C.; Larson, J.L. The experience of stigma in chronic obstructive pulmonary disease. West J. Nurs. Res. 2011, 33, 916–932. [Google Scholar] [CrossRef] [PubMed]
- Browne, J.L.; Ventura, A.; Mosely, K.; Speight, J. ‘I call it the blame and shame disease’: A qualitative study about perceptions of social stigma surrounding type 2 diabetes. BMJ Open 2013, 3, e003384. [Google Scholar] [CrossRef] [Green Version]
- Cataldo, J.K.; Brodsky, J.L. Lung cancer stigma, anxiety, depression and symptom severity. Oncology 2013, 85, 33–40. [Google Scholar] [CrossRef] [Green Version]
- Nyblade, L.; Stockton, M.; Travasso, S.; Krishnan, S. A qualitative exploration of cervical and breast cancer stigma in karnataka, india. BMC Womens Health 2017, 17, 58. [Google Scholar] [CrossRef] [Green Version]
- Sarfo, F.S.; Nichols, M.; Qanungo, S.; Teklehaimanot, A.; Singh, A.; Mensah, N.; Saulson, R.; Gebregziabher, M.; Ezinne, U.; Owolabi, M.; et al. Stroke-related stigma among west africans: Patterns and predictors. J. Neurol. Sci. 2017, 375, 270–274. [Google Scholar] [CrossRef] [Green Version]
- Goffman, E. Stigma; Notes on the Management of Spoiled Identity; Prentice-Hall: Englewood Cliffs, NJ, USA, 1963. [Google Scholar]
- Link, B.G.; Phelan, J.C. Conceptualizing stigma. Annu. Rev. Sociol. 2001, 27, 363–385. [Google Scholar] [CrossRef]
- Weiss, M.G.; Ramakrishna, J.; Somma, D. Health-related stigma: Rethinking concepts and interventions. Psychol. Health Med. 2006, 11, 277–287. [Google Scholar] [CrossRef] [PubMed]
- Bos, A.E.R.; Pryor, J.B.; Reeder, G.D.; Stutterheim, S.E. Stigma: Advances in theory and research. Basic Appl. Soc. Psychol. 2013, 35, 1–9. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Larson, J.E.; Kuwabara, S.A. Social psychology of the stigma of mental illness: Public and self-stigma models. In Social Psychological Foundations of Clinical Psychology; The Guilford Press: New York, NY, USA, 2010; pp. 51–68. [Google Scholar]
- Parker, R.; Aggleton, P. Hiv and aids-related stigma and discrimination: A conceptual framework and implications for action. Soc. Sci. Med. 2003, 57, 13–24. [Google Scholar] [CrossRef]
- Rao, P.S. Study on differences and similarities in the concept and origin of leprosy stigma in relation to other health-related stigma. Indian J. Lepr. 2010, 82, 117–121. [Google Scholar] [PubMed]
- Scambler, G. Re-framing stigma: Felt and enacted stigma and challenges to the sociology of chronic and disabling conditions. Soc. Theory Health 2004, 2, 29–46. [Google Scholar] [CrossRef]
- Stangl, A.L.; Earnshaw, V.A.; Logie, C.H.; van Brakel, W.; Simbayi, L.C.; Barre, I.; Dovidio, J.F. The health stigma and discrimination framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019, 17, 31. [Google Scholar] [CrossRef] [PubMed]
- Thornicroft, G. Stigma and discrimination limit access to mental health care. Epidemiol. Psichiatr. Soc. 2011, 17, 14–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scambler, G. Stigma and disease: Changing paradigms. Lancet 1998, 352, 1054–1055. [Google Scholar] [CrossRef]
- Earnshaw, V.A.; Bogart, L.M.; Dovidio, J.F.; Williams, D.R. Stigma and racial/ethnic hiv disparities moving toward resilience. Am. Psychol. 2013, 68, 225–236. [Google Scholar] [CrossRef]
- Jacoby, A. Felt versus enacted stigma—A concept revisited—Evidence from a study of people with epilepsy in remission. Soc. Sci. Med. 1994, 38, 269–274. [Google Scholar] [CrossRef]
- Scambler, G. Health-related stigma. Soc. Health Illn. 2009, 31, 441–455. [Google Scholar] [CrossRef] [PubMed]
- Nishio, I.; Chujo, M. Self-stigma of patients with type 1 diabetes and their coping strategies. Yonago Acta Med. 2017, 60, 167–173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Browne, J.L.; Ventura, A.; Mosely, K.; Speight, J. ‘I’m not a druggie, i’m just a diabetic’: A qualitative study of stigma from the perspective of adults with type 1 diabetes. BMJ Open 2014, 4, e005625. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meacham, E.; Orem, J.; Nakigudde, G.; Zujewski, J.A.; Rao, D. Exploring stigma as a barrier to cancer service engagement with breast cancer survivors in kampala, uganda. Psycho Oncol. 2016, 25, 1206–1211. [Google Scholar] [CrossRef]
- Park, J.H.; Park, J.H.; Kim, S.G.; Lee, K.S.; Hahm, M.I. Changes in employment status and experience of discrimination among cancer patients: Findings from a nationwide survey in korea. Psychooncology 2010, 19, 1303–1312. [Google Scholar] [CrossRef]
- Dyer, K.E. From cancer to sexually transmitted infection: Explorations of social stigma among cervical cancer survivors. Hum. Organ. 2010, 69, 321–330. [Google Scholar] [CrossRef]
- Gupta, A.; Dhillon, P.K.; Govil, J.; Bumb, D.; Dey, S.; Krishnan, S. Multiple stakeholder perspectives on cancer stigma in north india. Asian Pac. J. Cancer Prev. 2015, 16, 6141–6147. [Google Scholar] [CrossRef] [Green Version]
- Stergiou-Kita, M.; Pritlove, C.; Kirsh, B. The "big c"-stigma, cancer, and workplace discrimination. J. Cancer Surviv. 2016, 10, 1035–1050. [Google Scholar] [CrossRef]
- Halding, A.G.; Heggdal, K.; Wahl, A. Experiences of self-blame and stigmatisation for self-infliction among individuals living with copd. Scand J. Caring. Sci. 2011, 25, 100–107. [Google Scholar] [CrossRef]
- Suwankhong, D.; Liamputtong, P. Breast cancer treatment: Experiences of changes and social stigma among thai women in southern thailand. Cancer Nurs. 2016, 39, 213–220. [Google Scholar] [CrossRef]
- Trusson, D.; Pilnick, A. Between stigma and pink positivity: Women’s perceptions of social interactions during and after breast cancer treatment. Sociol. Health Illn. 2017, 39, 458–473. [Google Scholar] [CrossRef] [PubMed]
- Andrews, K.L.; Jones, S.C.; Mullan, J. Stigma: Still an important issue for adults with asthma. J. Asthma Allergy Educ. 2013, 4, 165–171. [Google Scholar] [CrossRef] [Green Version]
- Kato, A.; Fujimaki, Y.; Fujimori, S.; Isogawa, A.; Onishi, Y.; Suzuki, R.; Yamauchi, T.; Ueki, K.; Kadowaki, T.; Hashimoto, H. Psychological and behavioural patterns of stigma among patients with type 2 diabetes: A cross-sectional study. BMJ Open 2017, 7, e013425. [Google Scholar] [CrossRef] [Green Version]
- UN. Political Declaration of the High-Level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases; UN: New York, NY, USA, 2012. [Google Scholar]
- Alliance, N. Ncd Alliance Strategic Plan 2016–2020: From Global Commitments to National and Regional Action on ncd Prevention and Control; NCD Alliance: Geneva, Switzerland, 2016. [Google Scholar]
- Chambers, S.K.; Dunn, J.; Occhipinti, S.; Hughes, S.; Baade, P.; Sinclair, S.; Aitken, J.; Youl, P.; O’Connell, D.L. A systematic review of the impact of stigma and nihilism on lung cancer outcomes. BMC Cancer 2012, 12, 184. [Google Scholar] [CrossRef] [Green Version]
- Rose, S.; Paul, C.; Boyes, A.; Kelly, B.; Roach, D. Stigma-related experiences in non-communicable respiratory diseases: A systematic review. Chron. Respir. Dis. 2017, 14, 199–216. [Google Scholar] [CrossRef] [PubMed]
- Bulgin, D.; Tanabe, P.; Jenerette, C. Stigma of sickle cell disease: A systematic review. Issues Ment. Health Nurs. 2018, 39, 675–686. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, L.K.; Welter, E.; Leverenz, J.; Lerner, A.J.; Udelson, N.; Kanetsky, C.; Sajatovic, M. A systematic review of dementia-related stigma research: Can we move the stigma dial? Am. J. Geriatr. Psychiatry 2018, 26, 316–331. [Google Scholar] [CrossRef] [PubMed]
- Elliot, V.L.; Morgan, D.; Kosteniuk, J.; Froehlich Chow, A.; Bayly, M. Health-related stigma of noncommunicable neurological disease in rural adult populations: A scoping review. Health Soc. Care Community 2019, 27, e158–e188. [Google Scholar] [CrossRef]
- DeLuca, J.S. Conceptualizing adolescent mental illness stigma: Youth stigma development and stigma reduction programs. Adolesc. Res. Rev. 2020, 5, 153–171. [Google Scholar] [CrossRef]
- Overton, S.L.; Medina, S.L. The stigma of mental illness. J. Couns. Dev. 2008, 86, 143–151. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, J.; Harden, A.; Oakley, A.; Oliver, S.; Sutcliffe, K.; Rees, R.; Brunton, G.; Kavanagh, J. Integrating qualitative research with trials in systematic reviews. BMJ 2004, 328, 1010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect size estimates: Current use, calculations, and interpretation. J. Exp. Psychol. Gen. 2012, 141, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schabert, J.; Browne, J.L.; Mosely, K.; Speight, J. Social stigma in diabetes: A framework to understand a growing problem for an increasing epidemic. Patient 2013, 6, 1–10. [Google Scholar] [CrossRef]
- Engel, G.L. The clinical application of the biopsychosocial model. Am. J. Psychiatry 1980, 137, 535–544. [Google Scholar] [PubMed]
- Weiss, M.G. Stigma and the social burden of neglected tropical diseases. PLoS Negl. Trop Dis. 2008, 2, e237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tabah, E.N.; Yepnjio, F.; Njamnshi, A.K. Stigma in neurological diseases in the tropics. In Neglected Tropical Diseases and Conditions of the Nervous System; Bentivoglio, M., Cavalheiro, E.A., Kristensson, K., Patel, N.B., Eds.; Springer: New York, NY, USA, 2014; pp. 45–63. [Google Scholar]
- Moore, K.; Stuewig, J.; Tangney, J. Jail inmates’ perceived and anticipated stigma: Implications for post-release functioning. Self Identity 2013, 12, 527–547. [Google Scholar] [CrossRef] [Green Version]
- Kmet, L.M.; Cook, L.S.; Lee, R.C. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields; Alberta Heritage Foundation for Medical Research: Edmonton, AB, Canada, 2004. [Google Scholar]
- Aantjes, C.J.; Gilmoor, A.; Syurina, E.V.; Crankshaw, T.L. The status of provision of post abortion care services for women and girls in eastern and southern africa: A systematic review. Contraception 2018, 98, 77–88. [Google Scholar] [CrossRef]
- Bonanno, A.; Esmaeli, B. Facial disfigurement, stigma, and cancer: Interaction between patients and members of secondary groups. Sociol. Spectr. 2012, 32, 138–156. [Google Scholar] [CrossRef]
- Brown, C.G.; Brodsky, J.; Cataldo, J.K. Lung cancer stigma, anxiety, depression and quality of life. J. Psychosoc. Oncol. 2014, 32, 59–73. [Google Scholar] [CrossRef] [Green Version]
- Cho, J.; Choi, E.K.; Kim, S.Y.; Shin, D.W.; Cho, B.L.; Kim, C.H.; Koh, D.H.; Guallar, E.; Bardwell, W.A.; Park, J.H. Association between cancer stigma and depression among cancer survivors: A nationwide survey in korea. Psychooncology 2013, 22, 2372–2378. [Google Scholar] [CrossRef] [PubMed]
- Gredig, D.; Bartelsen-Raemy, A. Diabetes-related stigma affects the quality of life of people living with diabetes mellitus in switzerland: Implications for healthcare providers. Health Soc. Care Community 2017, 25, 1620–1633. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Lim, L.C.; Koh, D. Stigma among workers attending a hospital specialist diabetes clinic. Occup. Med. Oxford 2015, 65, 67–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzalez, B.D.; Jacobsen, P.B. Depression in lung cancer patients: The role of perceived stigma. Psychooncology 2012, 21, 239–246. [Google Scholar] [CrossRef] [Green Version]
- Wood, A.W.; Barden, S.; Terk, M.; Cesaretti, J. The influence of stigma on the quality of life for prostate cancer survivors. J. Psychosoc. Oncol. 2017, 35, 451–467. [Google Scholar] [CrossRef]
- Chapple, A.; Ziebland, S.; McPherson, A. Stigma, shame, and blame experienced by patients with lung cancer: Qualitative study. BMJ 2004, 328, 1470. [Google Scholar] [CrossRef] [Green Version]
- Kato, A.; Fujimaki, Y.; Fujimori, S.; Izumida, Y.; Suzuki, R.; Ueki, K.; Kadowaki, T.; Hashimoto, H. A qualitative study on the impact of internalized stigma on type 2 diabetes self-management. Patient Educ. Couns. 2016, 99, 1233–1239. [Google Scholar] [CrossRef]
- Scambler, G. Sociology, social structure and health-related stigma. Psychol. Health Med. 2006, 11, 288–295. [Google Scholar] [CrossRef]
- Eisenberg, D.; Golberstein, E.; Gollust, S.E. Help-seeking and access to mental health care in a university student population. Med. Care 2007, 45, 594–601. [Google Scholar] [CrossRef]
- Campbell, D.G.; Bonner, L.M.; Bolkan, C.R.; Lanto, A.B.; Zivin, K.; Waltz, T.J.; Klap, R.; Rubenstein, L.V.; Chaney, E.F. Stigma predicts treatment preferences and care engagement among veterans affairs primary care patients with depression. Ann. Behav. Med. 2016, 50, 533–544. [Google Scholar] [CrossRef] [Green Version]
- Sirey, J.A.; Bruce, M.L.; Alexopoulos, G.S.; Perlick, D.A.; Raue, P.; Friedman, S.J.; Meyers, B.S. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. Am. J. Psychiatry 2001, 158, 479–481. [Google Scholar] [CrossRef] [PubMed]
- Samb, B.; Desai, N.; Nishtar, S.; Mendis, S.; Bekedam, H.; Wright, A.; Hsu, J.; Martiniuk, A.; Celletti, F.; Patel, K.; et al. Prevention and management of chronic disease: A litmus test for health-systems strengthening in low-income and middle-income countries. Lancet 2010, 376, 1785–1797. [Google Scholar] [CrossRef]
- van Olmen, J.; Ku, G.M.; Bermejo, R.; Kegels, G.; Hermann, K.; Van Damme, W. The growing caseload of chronic life-long conditions calls for a move towards full self-management in low-income countries. Global. Health 2011, 7, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gausset, Q.; Mogensen, H.O.; Yameogo, W.M.; Berthe, A.; Konate, B. The ambivalence of stigma and the double-edged sword of hiv/aids intervention in burkina faso. Soc. Sci. Med. 2012, 74, 1037–1044. [Google Scholar] [CrossRef]
- Holzemer, W.L.; Uys, L.R. Managing aids stigma. Sahara J. 2004, 1, 165–174. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Wu, Z.; Wu, S.; Zhaoc, Y.; Jia, M.; Yan, Z. Hiv-related stigma in health care settings: A survey of service providers in china. AIDS Patient Care STDS 2007, 21, 753–762. [Google Scholar] [CrossRef] [PubMed]
- Takada, S.; Weiser, S.D.; Kumbakumba, E.; Muzoora, C.; Martin, J.N.; Hunt, P.W.; Haberer, J.E.; Kawuma, A.; Bangsberg, D.R.; Tsai, A.C. The dynamic relationship between social support and hiv-related stigma in rural uganda. Ann. Behav. Med. 2014, 48, 26–37. [Google Scholar] [CrossRef] [Green Version]
- Griffiths, K.M.; Crisp, D.A.; Barney, L.; Reid, R. Seeking help for depression from family and friends: A qualitative analysis of perceived advantages and disadvantages. BMC Psychiatry 2011, 11, 196. [Google Scholar] [CrossRef] [Green Version]
- Kemp, C.G.; Jarrett, B.A.; Kwon, C.S.; Song, L.; Jette, N.; Sapag, J.C.; Bass, J.; Murray, L.; Rao, D.; Baral, S. Implementation science and stigma reduction interventions in low- and middle-income countries: A systematic review. BMC Med. 2019, 17, 6. [Google Scholar] [CrossRef] [Green Version]
- Peters, R.M.; Dadun; Lusli, M.; Miranda-Galarza, B.; van Brakel, W.H.; Zweekhorst, M.B.; Damayanti, R.; Seda, F.S.; Bunders, J.F.; Irwanto. The meaning of leprosy and everyday experiences: An exploration in cirebon, indonesia. J. Trop Med. 2013, 2013, 507034. [Google Scholar] [CrossRef] [Green Version]
- Bekalu, M.A.; Eggermont, S.; Ramanadhan, S.; Viswanath, K. Effect of media use on hiv-related stigma in sub-saharan africa: A cross-sectional study. PLoS ONE 2014, 9, e100467. [Google Scholar] [CrossRef] [Green Version]
- Niederkrotenthaler, T.; Reidenberg, D.J.; Till, B.; Gould, M.S. Increasing help-seeking and referrals for individuals at risk for suicide by decreasing stigma: The role of mass media. Am. J. Prev. Med. 2014, 47, S235–S243. [Google Scholar] [CrossRef]
- Thornicroft, G.; Alem, A.; Antunes Dos Santos, R.; Barley, E.; Drake, R.E.; Gregorio, G.; Hanlon, C.; Ito, H.; Latimer, E.; Law, A.; et al. Wpa guidance on steps, obstacles and mistakes to avoid in the implementation of community mental health care. World Psychiatry 2010, 9, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Crocker, J. Social stigma and self-esteem: Situational construction of self-worth. J. Exp. Soc. Psychol. 1999, 35, 89–107. [Google Scholar] [CrossRef]
- Scambler, G.; Heijnders, M.; van Brakel, W.H.; Icraas. Understanding and tackling health-related stigma. Psychol. Health Med. 2006, 11, 269–270. [Google Scholar]
- Pearson, A.; White, H.; Bath-Hextall, F.; Salmond, S.; Apostolo, J.; Kirkpatrick, P. A mixed-methods approach to systematic reviews. Int. J. Evid. Based Healthc. 2015, 13, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Tran, B.X.; Phan, H.T.; Latkin, C.A.; Nguyen, H.L.T.; Hoang, C.L.; Ho, C.S.H.; Ho, R.C.M. Understanding global hiv stigma and discrimination: Are contextual factors sufficiently studied? (gapresearch). Int. J. Environ. Res. Public Health 2019, 16, 1899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naqvi, J.B.; Helgeson, V.S.; Gary-Webb, T.L.; Korytkowski, M.T.; Seltman, H.J. Sex, race, and the role of relationships in diabetes health: Intersectionality matters. J. Behav. Med. 2020, 43, 69–79. [Google Scholar] [CrossRef]
- Labovitz, D.L. Stroke epidemiology and intersectionality: Understanding stroke outcomes in mexican americans in corpus christi. Stroke 2020. [Google Scholar] [CrossRef]
- DuPont-Reyes, M.J.; Villatoro, A.P.; Phelan, J.C.; Painter, K.; Link, B.G. Adolescent views of mental illness stigma: An intersectional lens. Am. J. Orthopsychiatry 2020, 90, 201–211. [Google Scholar] [CrossRef] [Green Version]
- Jackson-Best, F.; Edwards, N. Stigma and intersectionality: A systematic review of systematic reviews across hiv/aids, mental illness, and physical disability. BMC Public Health 2018, 18, 919. [Google Scholar] [CrossRef] [PubMed]

| Type of Stigma Studied | n | Study | |
|---|---|---|---|
| Stigma type specific | Enacted stigma | 9 | Bonanno et al. (2012); Browne et al. (2013); Chappel et al. (2004); Cho et al. (2013); Gredig et al. (2017); Nyblade et al. (2017); Park et al. (2010); Sarfo et al. (2017); Dyer et al. (2010) |
| Felt stigma: Perceived | 11 | Andrews et al. (2013); Berger et al. (2011); Brown et al. (2014); Browne et al. (2013); Browne et al. (2014); Cataldo et al. (2013); Dyer et al. (2010); Gonzalez et al. (2012); Gredig et al. (2017); Gupta et al. (2015); Lee et al. (2015) | |
| Felt stigma: Internalized | 8 | Bonanno et al. (2012); Chappel et al. (2004); Gupta et al. (2015); Kato et al. (2016); Kato et al. (2017); Meacham et al. (2016); Sarfo et al. (2017); Wood et al. (2017) | |
| Felt stigma: Anticipated | 4 | Bonanno et al. (2012); Chappel et al. (2004); Sarfo et al. (2017); Nyblade et al. (2017) | |
| Stigma type unspecific | Not specified/ generic stigma | 4 | Halding et al. (2011); Stergiou-Kita et al. (2016); Suwakhong et al. (2016); Trusson et al. (2017) |
| Study | n | Quality Score | Type of Study | Type of Stigma Studied | Definition of Stated Stigma in the Study |
|---|---|---|---|---|---|
| CRD—COPD | |||||
| Berger et al. (2011) | 18 | 0.60 | Qualitative | Perceived stigma | * Not explicitly stated. |
| Halding et al. (2011) | 18 | 0.65 | Qualitative | Self-blame and stigmatization | ** “Stigmatization is a lack of social acceptance by broader society because of being different. Stigma is socially constructed, imposing attitudes on all members in a society. A mark of discredit is extremely powerful when it communicates highly valued beliefs in a particular society.” |
| CRD—Asthma | |||||
| Andrews et al. (2013) | 72 | 0.63 | Quantitative | Perceived stigma | * Not explicitly stated. |
| CVD—Stroke | |||||
| Sarfo et al. (2017) | 200 | 0.63 | Quantitative | Enacted stigma and felt stigma (personal stigma; family stigma; community/social stigma) | *** “Enacted stigma represents discrimination against the stigmatized person that is imposed by others; internalized or felt stigma is the fear of “enacted” stigma experienced by the stigmatized person; others—not stated.” |
| Diabetes Type 1 | |||||
| Browne et al. (2014) | 27 | 0.65 | Qualitative | Perception of diabetes-related stigma | * Not explicitly stated. |
| Nishio et al. (2017) | 24 | 0.70 | Qualitative | Stigma (diabetes-specific) | **** “Negative impression and sense of shame for being a diabetes patient due to negative responses of others and their own sense of values.” |
| Diabetes Type 2 | |||||
| Browne et al. (2013) | 26 | 0.80 | Qualitative | Perceived and experienced diabetes-related stigma | * Not explicitly stated. |
| Gredig et al. (2017) | 3347 | 0.63 | Quantitative | Perceived and experienced | *** “Perceived stigma means the perception of stereotypes linked with labeling. Experienced stigma—also referred to in the literature as enacted stigma—means the discrimination and exclusion experienced by those affected.” |
| Kato et al. (2017) | 209 | 0.67 | Quantitative | Internalized stigma | *** “Internalization of society’s negative perceptions towards an illness by someone who has that particular illness.” |
| Kato et al. (2016) | 26 | 0.60 | Qualitative | Internalized stigma | *** “Internalized stigma refers to the negative attitudes individuals hold toward themselves on account of their condition and/or the negative reactions of others.” |
| Lee et al. (2015) | 125 | 0.63 | Quantitative | Perceived stigma | * Not explicitly stated. |
| Cancer—Miscellaneous | |||||
| Cho et al. (2013) | 466 | 0.63 | Quantitative | Enacted stigma (social discrimination) | *** “Disqualification of individuals and groups who have particular health problems.” |
| Gupta et al. (2015) | 39 | 0.60 | Qualitative | Perceived and internalized stigma | *** “Perceived stigma refers to the shame associated with having a condition and to the fear of being discriminated and denied basic welfare rights leading to social exclusion. Actual stigma refers to obvious discrimination, which may lead to feelings of guilt, shame and threatens one’s own identity.” |
| Park et al. (2010) | 748 | 0.67 | Quantitative | Enacted stigma (work-related discrimination) | *** “Discrimination was defined as the experience of any of the following: reduction in salary, denial of a promotion, loss of an opportunity to demonstrate one’s ability, change of an assignment without the employee’s agreement, being treated as if one no longer has the ability to work, difficulty in revealing the cancer diagnosis to one’s employer, or pressure from the employer to quit, retire, or change jobs.” |
| Stergiou-Kita et al. (2016) | 40 | 0.80 | Qualitative | Stigma (unspecific) | ** “Stigma is defined as both a process and an attribute. The process of stigmatization has been described by Link and Phelan as involving three key actions. First, specific human differences are labeled as negative. Second, negative differences are linked to negative social stereotypes, and third such stereotypes are used to distinguish stigmatized individuals as “bothers” within society, resulting in separation, status loss, and discrimination. As an attribute, stigma has been characterized as a label or mark that is placed on individuals (or a group), who deviate from the norm or do not comply with established behavior rules.” |
| Cancer—Lung | |||||
| Brown et al. (2014) | 149 | 0.71 | Quantitative | Lung cancer stigma/perceived health-related stigma | **** “Lung cancer stigma (LCS) is a perceived health-related stigma that results from negative perceptions about the causal relationship between smoking and lung cancer.” |
| Cataldo et al. (2013) | 144 | 0.83 | Quantitative | Lung cancer stigma/perceived health-related stigma | **** “LCS is a perceived stigma and refers to the anticipation or fear of discrimination and an awareness of negative attitudes and actions related to lung cancer. It is a perceived HRS that is defined as a personal experience characterized by exclusion, rejection, blame, or devaluation that results from anticipation of an adverse judgment related to lung cancer.” |
| Chappel et al. (2004) | 45 | 0.60 | Qualitative | Felt and enacted stigma | *** “Stigma occurs when society labels someone as tainted, less desirable, or handicapped. This negative evaluation may be “felt” or “enacted.”—a felt negative evaluation refers to the shame associated with having a condition and to the fear of being discriminated against on the grounds of imputed inferiority or social unacceptability—an enacted negative evaluation refers to actual discrimination of this kind.” |
| Gonzalez et al. (2012) | 95 | 0.67 | Quantitative | Perceived stigma | * Not explicitly stated. |
| Cancer—Breast | |||||
| Meacham et al. (2016) | 20 | 0.60 | Qualitative | Internalized stigma | *** “Internalized stigma or self-stigma, is when a person with a stigmatized disease applies the negative public stigma associated with the disease to his/herself.” |
| Suwakhong et al. (2016) | 20 | 0.80 | Qualitative | Stigma (unspecific) | ** “Stigma is constructed in order to give reasons for the stigmatized person’s inferiority and to justify perceptions of the stigmatized as a threat or to be feared by others. Stigma is a mark or sign of disgrace usually eliciting negative attitudes toward the stigmatized.” |
| Trusson et al. (2017) | 24 | 0.65 | Qualitative | Stigma (unspecific) | ** “Stigma is the situation of the individual who is disqualified from full social acceptance.” |
| Cancer—Breast and Cervical | |||||
| Nyblade et al. (2017) | 59 | 0.70 | Qualitative | Anticipated stigma and experienced (enacted stigma) | *** “Anticipated: fear of stigma, whether or not it is actually experienced; experienced: stigma that is enacted through interpersonal acts of discrimination.” |
| Cancer-Cervical | |||||
| Dyer et al. (2010) | 19 | 0.60 | Qualitative | Perceived and experienced stigma | * Not explicitly stated. |
| Cancer—Prostate | |||||
| Wood et al. (2017) | 85 | 0.63 | Quantitative | Social and internalized stigma | *** “Social stigma is the most common form of experienced and researched stigma, and it exists when the larger society expresses a sense of “otherness” toward individuals due to specific characteristics (e.g., physical deformities). Internalized social stigma, wherein the opinions and views expressed in social stigma are taken in by the stigmatized and become part of their self-concept.” |
| Cancer—Head and Neck | |||||
| Bonanno et al. (2012) | 19 | 0.70 | Qualitative | Felt stigma and enacted stigma (disease-specific) | **** “Felt stigma indicates the patients’ own shame about her/his disfigurement and the fear of actions of discrimination against her/him. It further indicates the fact that interaction was bothersome to patients; enacted stigma refers to episodes of discrimination against patients related to the disfigurement.” |
| Study | Stigma Outcome/ Dependent Variable | n (male %) | Measurement Tool | Score Range | Validity | Reliability | Prevalence (%)/ Level of Stigma (Mean, SD) | Explored Associations with Correlates |
|---|---|---|---|---|---|---|---|---|
| CRD—Asthma | ||||||||
| Andrews et al. (2013) | Perceived stigma | 72 (26.3% male) | 19-item stigma scale for mental health | 0 to 100 (%) | Pre-validated: details NR | α = 0.89 | Perceived stigma: 86% (51% low stigma; 21% medium stigma; 14% high stigma; 14% no stigma) | Asthma control/morbidity (d = 0.820, p = 0.02) Physical health score (r = −0.41, p = 0.001) Mental health score (r = −0.23, p = 0.045) |
| CVD—Stroke | ||||||||
| Sarfo et al. (2017) | Perceived stigma (personal stigma; family stigma; community/social stigma) | 200 (52.5%) | 8-item Stigma Scale for Chronic Illness (SSCI-8) | 8 to 40 | Pre-validated: details NR | NR | Perceived personal stigma: 79% (13.7, SD 5.7) Perceived family stigma: 63% (11.9, SD 4.6) Perceived community stigma: 62% (11.4, SD 4.4) | Perceived personal stigma vs: No family history of stroke (β = 1.58; p = 0.03) Depression (NS) Employment (Employed vs. Unemployed) (NS) Stroke severity (NS) HRQoL (NS) |
| Diabetes Type 2 | ||||||||
| Gredig et al. (2017) | Perceived stigma and experienced stigma | 3347 (54.8% male) | 33-item Experienced Stigma and 26-item Perceived Stigma (self-developed questionnaire) | 0 to 100 (%) | Pre-validated: construct validity | NR | Experienced stigma: 68.5% Perceived stigma: 84.4% | Experienced stigma vs: Self-esteem (β = −0.067; p = 0.002) Psychological distress (β = 0.166; p < 0.001) Depressive symptoms (β = 0.156; p < 0.001) Perceived social support (β = −0.073; p < 0.002) Perceived stigma vs: Self-esteem (β = −0.176; p < 0.001) Psychological distress (β = 0.367; p < 0.001) Depressive symptoms (β = 0.331; p < 0.001) Perceived social support (β = −0.220; p < 0.001) |
| Kato et al. (2017) | Self (internalized)-stigma | 209 (80.4% male) | 39-item self-stigma scale in Japanese (SSSJ) | 0 to 117 | Pre-validated: details NR | α = 0.96 | Mean self/internalized stigma: 72.5, SD 6.38 | Self-esteem and social participation (d = 0.79, p < 0.001) |
| Lee et al. (2015) | Perceived stigma | 125 (68% male) | 8-item questionnaire to assess perceived stigma (self-developed questionnaire) | 0 to 100% | NR | NR | Perceived stigma: 12% | Diabetes affects work (d = 0.41; p < 0.05) Diabetes affects work prospect (d = 0.39; p < 0.05) |
| Cancer—Miscellaneous | ||||||||
| Cho et al. (2013) | Perceived cancer stigma (attitudes towards cancer) and experienced ancer stigma (social discrimination) | 466 (46.1% male) | 12-item questionnaire to assess cancer stigma (8-item attitudes towards cancer, and 4-items social discrimination) (self-developed questionnaire) | 0 to 100% | NR | Attitudes towards Cancer: impossibility of recovery (α = 0.75) and stereotypes (α = 0.76) Social discrimination (α = 0.89) | Perceived and experienced cancer stigma: 30% [Impossibility of recovery: cancer impossible to be treated (30.8%), difficult to be healthy again (40%), cannot be socially active because of cancer (36.2%)] [Stereotypes: cancer patients recognized by appearance (31.3%), have difficult time having sexual intimacy (31.3%)] [Social discrimination: avoided by friends (10.1%), avoided by neighbors (8.2%), problems with family (10.5%), discrimination from employers and coworkers (5%)] | Negative attitude towards cancer (Ref: positive attitude) vs: Depression (OR: 2.72, p < 0.05) Experience of discrimination (Ref: No) vs: Depression (OR: 2.27, p < 0.05) |
| Park et al. (2010) | Experienced stigma (discrimination) | 748 (59.0% male) | Single-item indicator for experienced stigma and 10-items for types of discrimination experienced (self-developed questionnaire) | 0 to 100% | NR | NR | Experienced discrimination in the workplace: 5.6% [reduction in salary (27.1%), loss of opportunity to display ability (13.6%), pressure to quit or change job (13.6%), difficulty of revealing cancer diagnosis (11.9%)] | Experienced discrimination vs: Disability (OR: 4.82, CI: 2.07–11.20) Change in employment status (NS) Unemployed (NS) |
| Cancer—Lung | ||||||||
| Brown et al. (2014) | Perceived health-related stigma (lung cancer stigma) | 149 (25% male) | 31-item Cataldo Lung Cancer Stigma Scale (CLCSS) | 31 to 124 | Pre-validated: construct validity | α = 0.96 | Mean perceived stigma level: 75.9, SD 18.20 | QoL (β = −0.136, p = 0.015) Anxiety (r = 0.418, p < 0.001) Depression (r = 0.562, p < 0.001), |
| Cataldo et al. (2013) | Perceived health-related stigma (lung cancer stigma) | 144 (26% male) | 31-item Cataldo Lung Cancer Stigma Scale (CLCSS) | 31 to 124 | Pre-validated: construct validity | α = 0.97 | Mean perceived stigma level: 75.7, SD 18.30 | Symptom severity (β = 0.140, p < 0.05) Anxiety (r = 0.413; p < 0.001) Depression (r = 0.559, p < 0.001) Symptom severity (r = 0.483, p < 0.001) |
| Gonzalez et al. (2012) | Perceived stigma | 95 (41.1% male) | 24-item Social Impact Scale (SIS) | Total score SIS (0 to 80) | Pre-validated: details NR | α = 0.81 | Mean total SIS score (perceived stigma): 42.9, SD 11.87 | Depression (β = 0.19, p = 0.03) |
| Cancer—Prostate | ||||||||
| Wood et al. (2017) | Self/internalized stigma and social stigma | 85 (all male) | 24-item Social Impact Scale (SIS): internalized shame/stigma, social rejection, financial insecurity, social isolation | Internalized shame/stigma (5 to13) Social rejection (9 to 20) Social isolation (7 to 23) Financial insecurity (3 to 12) | Pre-validated: details NR | Internalized shame (α = 0.73), social rejection (α = 0.84), financial insecurity (α = 0.85), social isolation (α = 0.92) | SIS internalized shame: 7, SD 2.42 SIS social rejection: 10.63, SD 2.71 SIS social isolation: 9.61, SD 3.80 SIS financial insecurity: 4, SD 1.48 | SIS internalized shame vs. QoL (β = −0.15, p < 0.001) SIS social rejection vs. QoL (β = 0.18, p < 0.001) SIS social isolation vs. QoL (β = −0.36, p < 0.001) SIS financial insecurity vs. QoL (β = −0.34, p < 0.001) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rai, S.S.; Syurina, E.V.; Peters, R.M.H.; Putri, A.I.; Zweekhorst, M.B.M. Non-Communicable Diseases-Related Stigma: A Mixed-Methods Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6657. https://doi.org/10.3390/ijerph17186657
Rai SS, Syurina EV, Peters RMH, Putri AI, Zweekhorst MBM. Non-Communicable Diseases-Related Stigma: A Mixed-Methods Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(18):6657. https://doi.org/10.3390/ijerph17186657
Chicago/Turabian StyleRai, Sarju Sing, Elena V. Syurina, Ruth M. H. Peters, Annisa Ika Putri, and Marjolein B. M. Zweekhorst. 2020. "Non-Communicable Diseases-Related Stigma: A Mixed-Methods Systematic Review" International Journal of Environmental Research and Public Health 17, no. 18: 6657. https://doi.org/10.3390/ijerph17186657






