Pharmacists’ Preparedness to Patients Education at the Time of Pandemic—A Cross-Sectional Study with an Example of SARS-CoV-2 Outbreak in Poland
Abstract
:1. Introduction
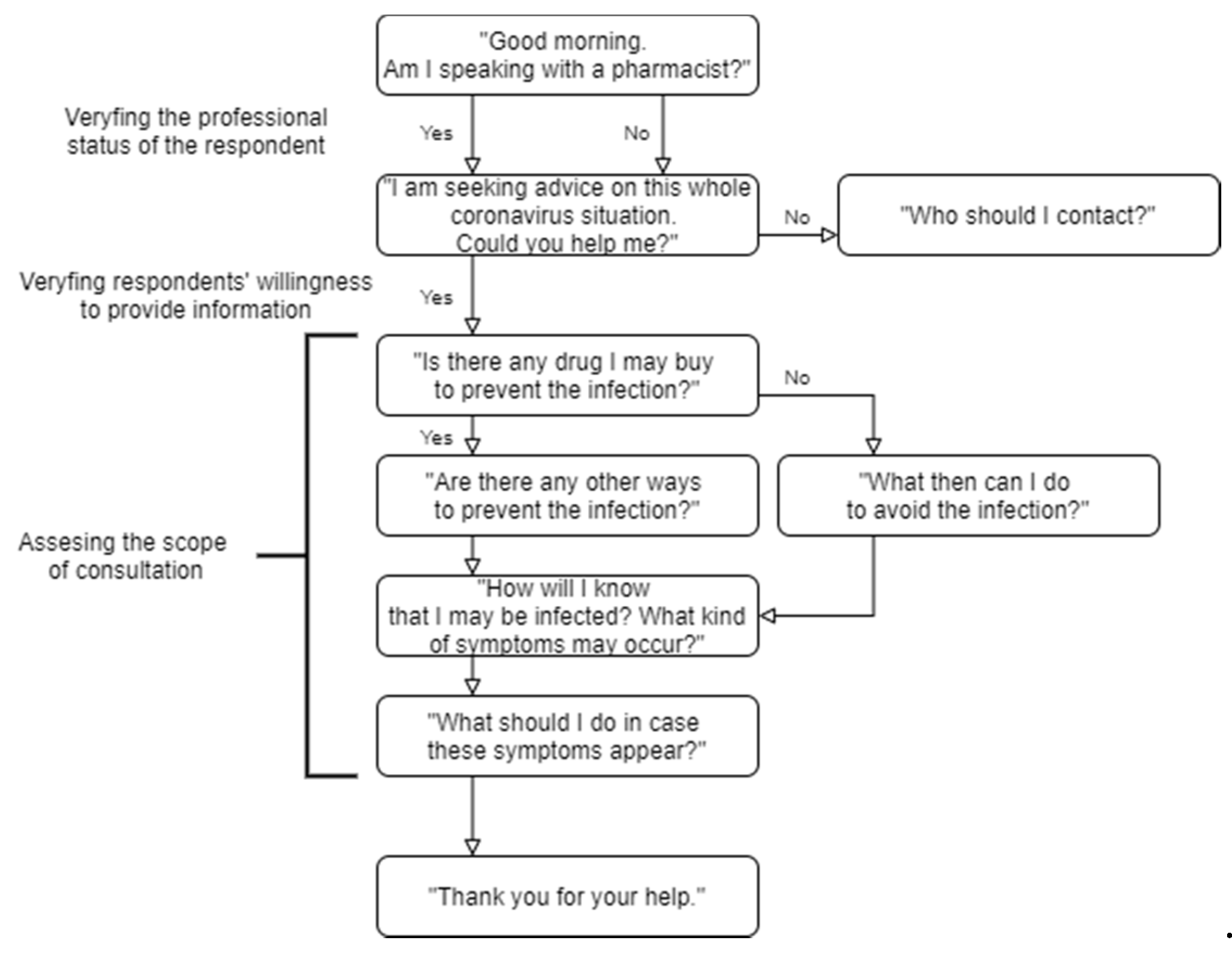
2. Materials and Methods
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Awad, A.I.; Al-Rasheedi, A.; Lemay, J. Public Perceptions, Expectations, and Views of Community Pharmacy Practice in Kuwait. Med. Princ. Pract. 2017, 26, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Al Aqeel, S.; Abanmy, N.; AlShaya, H.; Almeshari, A. Interventions for Improving Pharmacist-Led Patient Counselling in the Community Setting: A Systematic Review. Syst. Rev. 2018, 7, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hindi, A.M.K.; Schafheutle, E.I.; Jacobs, S. Patient and Public Perspectives of Community Pharmacies in the United Kingdom: A Systematic Review. Health Expect. 2018, 21, 409–428. [Google Scholar] [CrossRef] [PubMed]
- Hepler, C.; Strand, L. Opportunities and Responsibilities in Pharmaceutical Care. Am. J. Hosp. Pharm. 1990, 47, 533–542. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Joint FIP/WHO Guidelines on Good Pharmacy Practice: Standards for Quality of Pharmacy Services. WHO Tech. Rep. Ser. 2011, 961, 1–18. [Google Scholar]
- Eades, C.E.; Ferguson, J.S.; O’Carroll, R.E. Public Health in Community Pharmacy: A Systematic Review of Pharmacist and Consumer Views. BMC Public Health 2011, 11, 582. [Google Scholar] [CrossRef] [Green Version]
- Pearson, G.J. Evolution in the Practice of Pharmacy—Not a Revolution! Cmaj 2007, 176, 1295–1296. [Google Scholar] [CrossRef] [Green Version]
- Douglas, E.; Power, A.; Hudson, S. Pharmaceutical Care of the Patient with Diabetes Mellitus: Pharmacists’ Priorities for Services and Educational Needs in Scotland. Int. J. Pharm. Pract. 2007, 15, 47–52. [Google Scholar] [CrossRef]
- Simpson, S.H.; Haggarty, S.; Johnson, J.A.; Schnidel, T.J.; Tsuyuki, R.T.; Lewanczuk, R. Survey of Pharmacist Activities and Attitudes in Diabetes Management. Can. Pharm. J. 2009, 142, 128–134. [Google Scholar] [CrossRef]
- Blom, L.; Krass, I. Introduction: The Role of Pharmacy in Patient Education and Counseling. Patient Educ. Couns. 2011, 83, 285–287. [Google Scholar] [CrossRef]
- Sakeena, M.H.F.; Bennett, A.A.; McLachlan, A.J. Enhancing Pharmacists’ Role in Developing Countries to Overcome the Challenge of Antimicrobial Resistance: A Narrative Review. Antimicrob. Resist. Infect. Control 2018, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, Y.; Yang, S.; Feng, B.; Ni, Y.; Zhang, K. Pharmacists’ Perception of Pharmaceutical Care in Community Pharmacy: A Questionnaire Survey in Northwest China. Health Soc. Care Community 2011, 19, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Laliberté, M.C.; Perreault, S.; Damestoy, N.; Lalonde, L. Ideal and Actual Involvement of Community Pharmacists in Health Promotion and Prevention: A Cross-Sectional Study in Quebec, Canada. BMC Public Health 2012, 12, 192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldstone, L.W.; Saldaña, S.N.; Werremeyer, A. Pharmacist Provision of Patient Medication Education Groups. Am. J. Health Pharm. 2015, 72, 487–492. [Google Scholar] [CrossRef]
- San Martín-Rodríguez, L.; Beaulieu, M.-D.; D’Amour, D.; Ferrada-Videla, M. The Determinants of Successful Collaboration: A Review of Theoretical and Empirical Studies. J. Interprof. Care 2005, 19 (Suppl. 1), 132–147. [Google Scholar] [CrossRef]
- Majchrowska, A.; Bogusz, R.; Nowakowska, L.; Pawlikowski, J.; Piątkowski, W.; Wiechetek, M. Public Perception of the Range of Roles Played by Professional Pharmacists. Int. J. Environ. Res. Public Health 2019, 16, 2787. [Google Scholar] [CrossRef] [Green Version]
- Goniewicz, M.L.; Lingas, E.O.; Czogala, J.; Koszowski, B.; Zielinska-Danch, W.; Sobczak, A. The Role of Pharmacists in Smoking Cessation in Poland. Eval. Health Prof. 2010, 33, 81–95. [Google Scholar] [CrossRef] [Green Version]
- Waszyk-Nowaczyk, M.; Łuczak, A.; Michalak, D.; Kaczmarczyk, J.; Myrda, H.; Michalak, M.; Ratka, A. Evaluation of opinions on community pharmacy-based health screenings for common chronic diseases. Acta Pol. Pharm. Drug Res. 2017, 74, 1613–1620. [Google Scholar]
- Pawłowska, I.; Pawłowski, L.; Lichodziejewska-Niemierko, M. The Role of a Pharmacist in a Hospice: A Nationwide Survey among Hospice Directors, Pharmacists and Physicians. Eur. J. Hosp. Pharm. 2016, 23, 106–112. [Google Scholar] [CrossRef]
- Waszyk-Nowaczyk, M.; Skura, O.; Michalak, M.; Ratka, A. Opinions of pharmacists on community pharmacy-based health screenings for common chronic diseases. Acta Pol. Pharm.Drug Res. 2018, 75, 819–826. [Google Scholar]
- Rubin, S.E.; Schulman, R.M.; Roszak, A.R.; Herrmann, J.; Patel, A.; Koonin, L.M. Leveraging Partnerships among Community Pharmacists, Pharmacies, and Health Departments to Improve Pandemic Influenza Response. Biosecurity Bioterrorism 2014, 12, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Chandra-Mouli, V.; Lenz, C.; Adebayo, E.; Lang Lundgren, I.; Gomez Garbero, L.; Chatteriee, S. A Systematic Review of the Use of Adolescent Mystery Clients in Assessing the Adolescent Friendliness of Health Services in High, Middle, and Low-Income Countries. Glob. Health Action 2018, 11, 1536412. [Google Scholar] [CrossRef] [PubMed]
- Sancar, M.; Tezcan, E.; Okuyan, B.; Izzettin, F.V. Assessment of the Attitude of Community Pharmacists and Pharmacy Technicians towards Diarrhea: A Simulated Patient Study in Turkey. Trop. J. Pharm. Res. 2015, 14, 1509–1515. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health. Coronavirus—What Do You Need to Know? [in Polish: Koronawirus—Co musiszwiedzieć?]. Available online: https://www.gov.pl/web/zdrowie/co-musisz-wiedziec-o-koronawirusie (accessed on 5 August 2020).
- VassarStats: Statistical Computation Web Site. Available online: http://vassarstats.net/fisher2x4.html (accessed on 7 September 2020).
- Polish Medical Registers—Registry of Pharmacies. Available online: https://rejestrymedyczne.csioz.gov.pl/ra/search/public (accessed on 12 August 2020).
- IQVIA. Report for September 2019. Available online: https://www.nia.org.pl/2019/10/23/iqvia-podsumowanie-wrzesien-2019/ (accessed on 12 March 2020).
- Ministry of Science and Higher Education. Regulation of the Minister of Science and Higher Education on the Standards of Undergraduate Education of Physicians, Dentists, Pharmacists, Nurses, Midwives, Laboratory Diagnosticians, Physiotherapists and Paramedics. [in Polish: RozporządzenieMinistraNaukiiSzkolnictwaWyższego w SprawieStandardówKształceniaPrzygotowującegodo WykonywaniaZawoduLekarza, LekarzaDentysty, Farmaceuty, Pielęgniarki, Położnej, DiagnostyLaboratoryjnego, FizjoterapeutyiRatownikaMedycznego]. 2019. Available online: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU20190001573/O/D20191573.pdf (accessed on 7 August 2020).
- Ministry of Education. Regulation of the Minister of Education of 16 May 2019 on the Curricula for Occupational Education and Additional Skills in Selected Professions [in Polish: RozporządzenieMinistraEdukacjiNarodowej z Dnia 16 maja 2019 r. w SprawiePodstawProgramowychKształceniaw ZawodachSzkolnictwaBranżowegoOrazDodatkowychUmiejętnościZawodowych w ZakresieWybranychZawodówSzkolnictwaBranżowego]. 2019. Available online: https://dziennikustaw.gov.pl/DU/2019/991 (accessed on 10 August 2020).
- Tully, M.P.; Beckman-Gyllenstrand, A.; Bernsten, C.B. Factors Predicting Poor Counselling about Prescription Medicines in Swedish Community Pharmacies. Patient Educ. Couns. 2011, 83, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Koehler, T.; Brown, A. A Global Picture of Pharmacy Technician and Other Pharmacy Support Workforce Cadres. Res. Soc. Adm. Pharm. 2017, 13, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Editorial Team. Pharmacies Are Not able to Stay on-Duty. There Is a Shortage of Personnel throughout Poland [in Polish:AptekiNiesą w StanieDyżurować. wCałejPolsceBrakujePersonelu] mgr.farm. 2020. Available online: https://mgr.farm/aktualnosci/apteki-nie-sa-w-stanie-dyzurowac-w-calej-polsce-brakuje-personelu/ (accessed on 3 August 2020).
- Supreme Pharmaceutical Chamber. Educational Materials for Pharmacists. Available online: https://www.nia.org.pl/2020/03/11/koronawirus-materialy-dla-farmaceutow/ (accessed on 12 March 2020).
- Salter, S.M.; Karia, A.; Sanfilippo, F.M.; Clifford, R.M. Effectiveness of E-Learning in Pharmacy Education. Am. J. Pharm. Educ. 2014, 78, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nesterowicz, K.; Librowski, T.; Edelbring, S. Validating E-Learning in Continuing Pharmacy Education: User Acceptance and Knowledge Change. BMC Med. Educ. 2014, 14, 33. [Google Scholar] [CrossRef] [PubMed]
- Coppus, S.F.P.J.; Emparanza, J.I.; Hadley, J.; Kulier, R.; Weinbrenner, S.; Arvanitis, T.N.; Burls, A.; Cabello, J.B.; Decsi, T.; Horvath, A.R.; et al. A Clinically Integrated Curriculum in Evidence-Based Medicine for Just-in-Time Learning through on-the-Job Training: The EU-EBM Project. BMC Med. Educ. 2007, 7, 46. [Google Scholar] [CrossRef] [Green Version]
- Amariles, P.; Ledezma-Morales, M.; Salazar-Ospina, A.; Hincapié-García, J.A. How to Link Patients with Suspicious COVID-19 to Health System from the Community Pharmacies? A Route Proposal. Res. Soc. Adm. Pharm. 2020, 1–2. [Google Scholar] [CrossRef]
- Ooi, G.S.; Hassali, M.A.; Shafie, A.A.; Kong, D.C.M.; Mak, V.S.L.; Chua, G.N. Consumers’ perspectives of Malaysian community pharmacists as health educators: A qualitative insight. J. Pharm.Pract. Res. 2017, 47, 186–192. [Google Scholar] [CrossRef]
- Chen, Y.C.; Kiersma, M.E.; Abdelmageed, A. Evaluation of Student Perceptions of Standardized Patient Simulation on Patient Counseling Confidence during Introductory Pharmacy Practice Experiences. Curr. Pharm. Teach. Learn. 2015, 7, 811–818. [Google Scholar] [CrossRef]
- Gierdys, W. Coronavirus. Pharmacists and Pharmaceutical Technicians on the Front Line. What Does Their Job Look Like Now? [in Polish: Koronawirus. FarmaceuciiTechnicyFarmaceutyczninaPierwszejLiniiFrontu.JakWyglądaTerazIchPraca?] MagazynAptekarski. 2020. Available online: https://www.aptekarski.com/89320-koronawirus-farmaceuci-i-technicy-farmaceutyczni-na-pierwszej-linii-frontu-jak-wyglada-teraz-ich-praca (accessed on 5 August 2020).
- Van Mill, J.W.F.; Schulz, M. A Review of Pharmaceutical Care in Community Pharmacy in Europe. Harvard Health Policy Rev. 2006, 7, 155–168. [Google Scholar]
- El Hajj, M.S.; AL-Saeed, H.S.; Khaja, M. Qatar Pharmacists’ Understanding, Attitudes, Practice and Perceived Barriers Related to Providing Pharmaceutical Care. Int. J. Clin. Pharm. 2016, 38, 330–343. [Google Scholar] [CrossRef] [PubMed]
- Ung, C.O.L. Community Pharmacist in Public Health Emergencies: Quick to Action against the Coronavirus 2019-NCoV Outbreak. Res. Soc.Adm. Pharm. 2020, 583–586. [Google Scholar] [CrossRef]
- Wiedenmayer, K.; Summers, R.S.; Mackie, C.A.; Gous, A.G.S.; Everard, M. World Health Organization, Developing Pharmacy Practice: A Focus on Patient Care. 2006. Available online: http://www.fip.org/files/fip/publications/DevelopingPharmacyPractice/DevelopingPharmacyPracticeEN.pdf (accessed on 15 July 2020).
- The appeal of the President of the Supreme Pharmaceutical Chamber to the Minister of Healthto Take Action to Increase the Safety of Community Pharmacies’ Staff. 2020. Available online: https://www.nia.org.pl/2020/03/12/naczelna-rada-aptekarska-apeluje-do-ministra-zdrowia/ (accessed on 7 September 2020).
- Editorial Team. The Reimbursement of Flu Vaccines for Physicians and Teachers. What about pharmacists? [in Polish:RefundowaneSzczepionkinaGrypęDlaLekarzyiNauczycielia co z Farmaceutami?] mgr.farm. 2020. Available online: https://mgr.farm/aktualnosci/refundowane-szczepionki-na-grype-dla-lekarzy-i-nauczycieli-a-co-z-farmaceutami/ (accessed on 7 September 2020).
- Pharmaceutical Chambers Act. [in Polish: Ustawa z Dnia 10 Stycznia 2008 r. o ZmianieUstawy o IzbachAptekarskich (Dz.U. Nr 47 Poz. 273 Dnia 19 Marca 2008)]. 2008. Available online: http://prawo.sejm.gov.pl/isap.nsf/download.xsp/WDU20080470273/T/D20080273L.pdf (accessed on 8 September 2020).
- The Ordinance of the Minister of Health of 8 July 2020 on the Establishment of the Pharmaceutical Care Expert Team [in Polish: ZarządzenieMinistraZdrowia z Dnia 8 Lipca 2020 r. w SprawiePowołaniaZespołu do SprawOpiekiFarmaceutycznej]. Available online: http://dziennikmz.mz.gov.pl/#/legalact/2020/49/ (accessed on 8 September 2020).
- Chancellery of the Prime Minister. The draft of the Pharmacy Profession Act. 2020. Available online: https://www.gov.pl/web/premier/projekt-ustawy-o-zawodzie-farmaceuty (accessed on 8 September 2020).
- Cerbin-Koczorowska, M.; Zielinska-Tomczak, L.; Waszyk-Nowaczyk, M.; Michalak, M.; Skowron, A. As the twig is bent, so is the tree inclined: A survey of student attitudes toward interprofessional collaboration supported with the curricula analysis. J.Interprof. Care 2019, 33, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Waszyk-Nowaczyk, M.; Nowaczyk, P.; Simon, M. Physicians’ and patients’ valuation of pharmaceutical care implementation in Poznan (Poland) community pharmacies. Saudi Pharm. J. 2014, 22, 537–544. [Google Scholar] [CrossRef] [Green Version]
- Payroll Report 2020. Earnings in Pharmacies all Over Poland. [in Polish: Raportpłac 2020. Zarobki w Aptekach w CałejPolsce]. Available online: https://praca.farmacja.pl/sites/default/files/Raport_P%C5%82ac_2020.pdf (accessed on 8 September 2020).
- Editorial Team. PLN 1000 Bonus for 100% Presence. Pharmacies Are Fighting for Staff [in Polish: 1000 złPremiiza 100 proc. Obecności. AptekiWalczą o Personel]. 2020. Available online: https://mgr.farm/aktualnosci/1000-zl-premii-za-100-proc-obecnosci-apteki-walcza-o-personel/ (accessed on 8 September 2020).
- Deloitte Advisory Company 2018 Report: How to Introduce Pharmaceutical Care in Poland? The Role and Challenges of a Modern Pharmacy [in Polish: JakWprowadzić w PolsceOpiekęFarmaceutyczną? RolaiWyzwaniaWspółczesnejApteki]. Available online: https://www2.deloitte.com/content/dam/Deloitte/pl/Documents/Reports/pl-raport-jak%20wprowadzic-w-Polsce-opieke-farmaceutyczna.pdf (accessed on 8 September 2020).
- Żak, K. Pharmaceutical care or professional advice? Barriers to the implementation of pharmaceutical care in Poland. Ekon. Wrocław Econ. Rev. 2018, 24, 65–81. [Google Scholar] [CrossRef] [Green Version]
- Krejcie, R.V.; Morgan, D.W. Determining Sample Size for Research Activities. Educ. Psychol. Meas. 1970, 38, 607–610. [Google Scholar] [CrossRef]
| Characteristic | n (%) | |
|---|---|---|
| Province [in Polish] (total number of community pharmacies) | ||
| Lower Silesian [dolnośląskie] (991) | 6 (8.70) | |
| Kuyavian-Pomeranian [kujawsko-pomorskie] (611) | 3 (4.35) | |
| Lublin [lubelskie] (785) | 5 (7.25) | |
| Lubusz [lubuskie] (331) | 1 (1.45) | |
| Łódź [łódzkie] (855) | 5 (7.25) | |
| Lesser Poland [małopolskie] (1073) | 6 (8.70) | |
| Masovian [mazowieckie] (1701) | 10 (14.49) | |
| Opole [opolskie] (310) | 1 (1.45) | |
| Subcarpathian [podkarpackie] (665) | 3 (4.35) | |
| Podlaskie [podlaskie] (387) | 2 (2.90) | |
| Pomeranian [pomorskie] (704) | 5 (7.25) | |
| Silesian [śląskie] (1437) | 10 (14.49) | |
| Holy Cross [świętokrzyskie] (393) | 2 (2.90) | |
| Warmian-Masurian [warmińsko-mazurskie] (418) | 2 (2.90) | |
| Greater Poland [wielkopolskie] (1278) | 5 (7.25) | |
| West Pomeranian [zachodniopomorskie] (560) | 3 (4.35) | |
| Exact location a | ||
| large towns | 20 (28.99) | |
| medium towns | 17 (24.64) | |
| small towns | 21 (30.43) | |
| villages | 11 (15.94) | |
| Type of pharmacy b | ||
| chain | 18 (26.09) | |
| non-chain | 51 (73.91) | |
| Consultations Details | Pharmacists | Pharmacy Technicians | Total a | ||||
|---|---|---|---|---|---|---|---|
| Number of consultations | 54 (100.00) | 15 (100.00) | 69 (100.00) | ||||
| Average time of a single consultation | 2:22 | 1:54 | 2:16 | ||||
| Category | Information Provided by Pharmacy Staff | p-value | |||||
| Prevention | Keep safe distance | 51 (94.44) | 12 (80.00) | 63 (91.30) | 0.112 | ||
| Wash your hands often | 43 (79.63) | 9 (60.00) | 52 (75.36) | 0.174 | |||
| alcohol-based liquids/gels | 27 (50.00) | 4 (26.67) | 31 (44.93) | 0.146 | |||
| water with soap | 27 (50.00) | 3 (20.00) | 30 (43.48) | 0.045 | |||
| Avoid touching eyes, nose and mouth | 17 (31.48) | 1 (6.67) | 18 (26.09) | 0.093 | |||
| Cover mouth/nose while sneezing/coughing | 9 (16.67) | 0 (0.00) | 9 (13.04) | 0.189 | |||
| the average number of information provided by a single respondent | Q1 | 2 | 1 | 2 | 0.006 | ||
| Q2 | 3 | 2 | 3 | ||||
| Q3 | 6 | 3 | 6 | ||||
| Drug usage | No drug helps to prevent the infection | 45 (83.33) | 8 (53.33) | 53 (76.81) | 0.033 | ||
| Symptoms | fever | 49 (90.74) | 13 (86.67) | 62 (89.86) | 0.641 | ||
| breathing difficulties | 45 (83.33) | 8 (53.33) | 53 (76.81) | 0.033 | |||
| dry cough | 36 (66.67) | 12 (80.00) | 48 (69.57) | 0.527 | |||
| the average number of information provided by a single respondent | Q1 | 2 | 2 | 2 | 0.222 | ||
| Q2 | 3 | 2 | 2 | ||||
| Q3 | 3 | 3 | 3 | ||||
| Source of aid | Chief Sanitary Inspectorate | 40 (74.07) | 8 (53.33) | 48 (69.57) | 0.203 | ||
| isolation ward at the local hospital | 28 (51.85) | 4 (26.67) | 32 (46.38) | 0.142 | |||
| National Health Fund hotline | 14 (25.93) | 6 (40.00) | 20 (28.99) | 0.341 | |||
| emergency ward at the local hospital | 4 (7.41) | 1 (6.67) | 5 (7.25) | 0.999 | |||
| emergency telephone number (112) | 3 (5.56) | 0 (0.00) | 3 (4.35) | 0.999 | |||
| local physician’s office | 2 (3.70) | 1 (6.67) | 3 (4.35) | 0.527 | |||
| the average number of information provided by a single respondent b | Q1 | 1 | 1 | 1 | 0.141 | ||
| Q2 | 2 | 1 | 2 | ||||
| Q3 | 2 | 2 | 2 | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cerbin-Koczorowska, M.; Waszyk-Nowaczyk, M.; Przymuszała, P. Pharmacists’ Preparedness to Patients Education at the Time of Pandemic—A Cross-Sectional Study with an Example of SARS-CoV-2 Outbreak in Poland. Int. J. Environ. Res. Public Health 2020, 17, 6659. https://doi.org/10.3390/ijerph17186659
Cerbin-Koczorowska M, Waszyk-Nowaczyk M, Przymuszała P. Pharmacists’ Preparedness to Patients Education at the Time of Pandemic—A Cross-Sectional Study with an Example of SARS-CoV-2 Outbreak in Poland. International Journal of Environmental Research and Public Health. 2020; 17(18):6659. https://doi.org/10.3390/ijerph17186659
Chicago/Turabian StyleCerbin-Koczorowska, Magdalena, Magdalena Waszyk-Nowaczyk, and Piotr Przymuszała. 2020. "Pharmacists’ Preparedness to Patients Education at the Time of Pandemic—A Cross-Sectional Study with an Example of SARS-CoV-2 Outbreak in Poland" International Journal of Environmental Research and Public Health 17, no. 18: 6659. https://doi.org/10.3390/ijerph17186659






