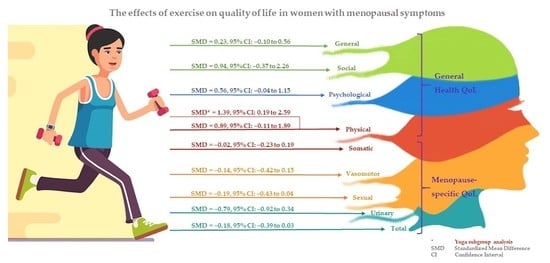
Exercise and Quality of Life in Women with Menopausal Symptoms: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria
- (1)
- Participants: studies of women with at least one menopausal symptom due to the natural decline of reproductive hormones, comprehensive cancer treatment program, hysterectomy, and/or premature ovarian failure were included. Studies of menopausal women that did not mention any menopausal symptoms as inclusion criteria were excluded;
- (2)
- Intervention and control groups: studies comparing exercise with no active treatment were included. In the present study, exercise was defined as a planned, structured, repetitive, and purposeful subcategory of physical activity, aimed at the maintenance or improvement of one or more components of physical fitness [35]. There were no restrictions on the frequency and duration of the intervention as well as whether exercises were supervised by instructors or self-delivered. Studies in which exercises were combined with non-exercise methods were excluded because these combined methods possibly influence the actual effect of exercise on QoL in women with menopausal symptoms. We also excluded studies in which the control groups performed active non-exercise interventions such as MHT and cognitive behavior therapy. In addition, we excluded studies where both the intervention and the control groups performed exercises (i.e., aerobics vs. resistance training);
- (3)
- Outcomes: QoL scores of both the intervention and the control groups must be provided;
- (4)
- Only RCTs of humans published in English were included. Publications in commentary, editorial, or review form were excluded;
- (5)
- Studies with unavailable full texts were excluded.
2.3. Screening Data
2.4. Data Extraction
2.5. Risk-of-Bias Assessment
2.6. QoL Outcomes
2.7. Meta-Analysis
3. Results
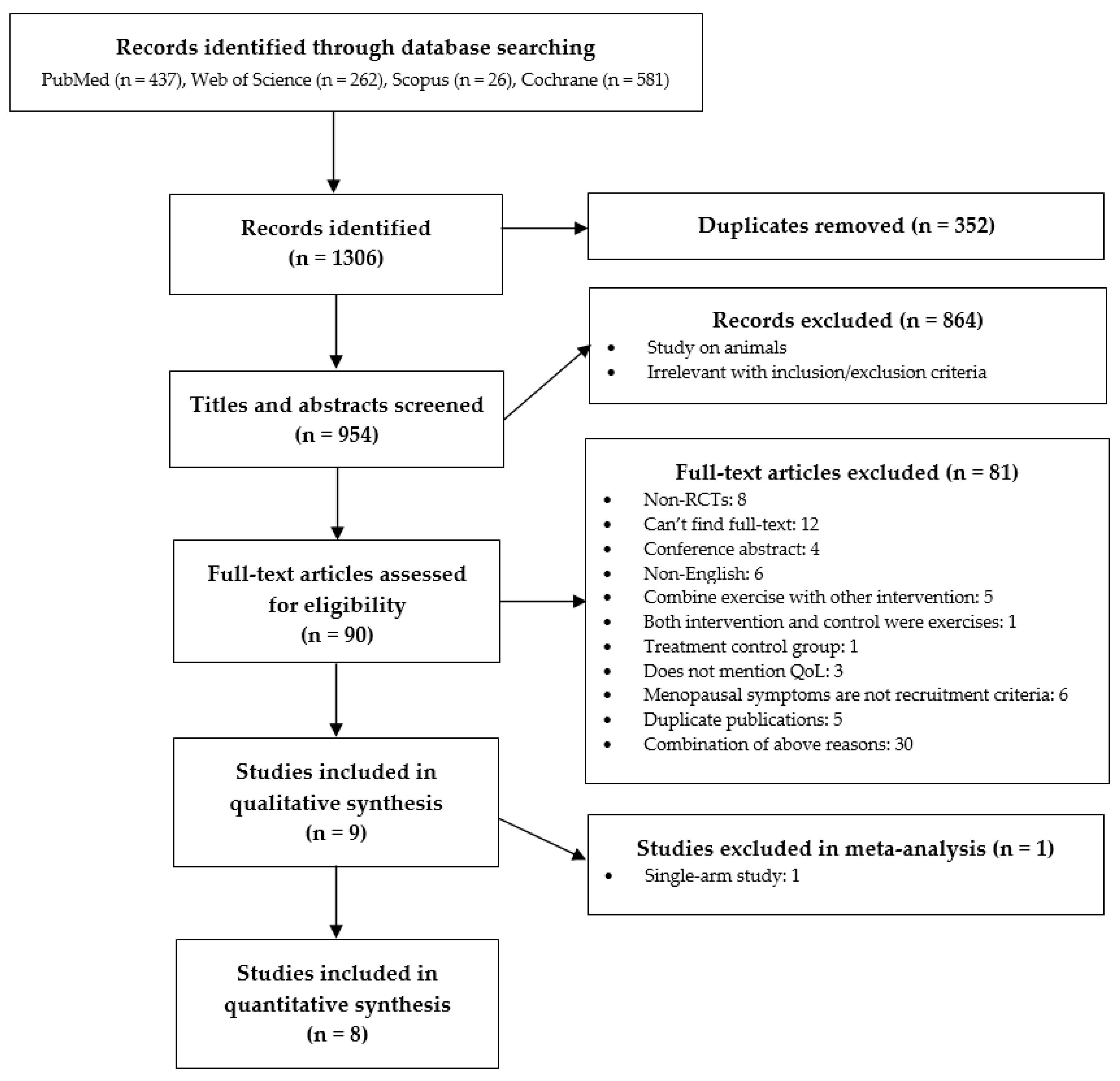
3.1. Study Selection
3.2. Characteristics of Included Studies
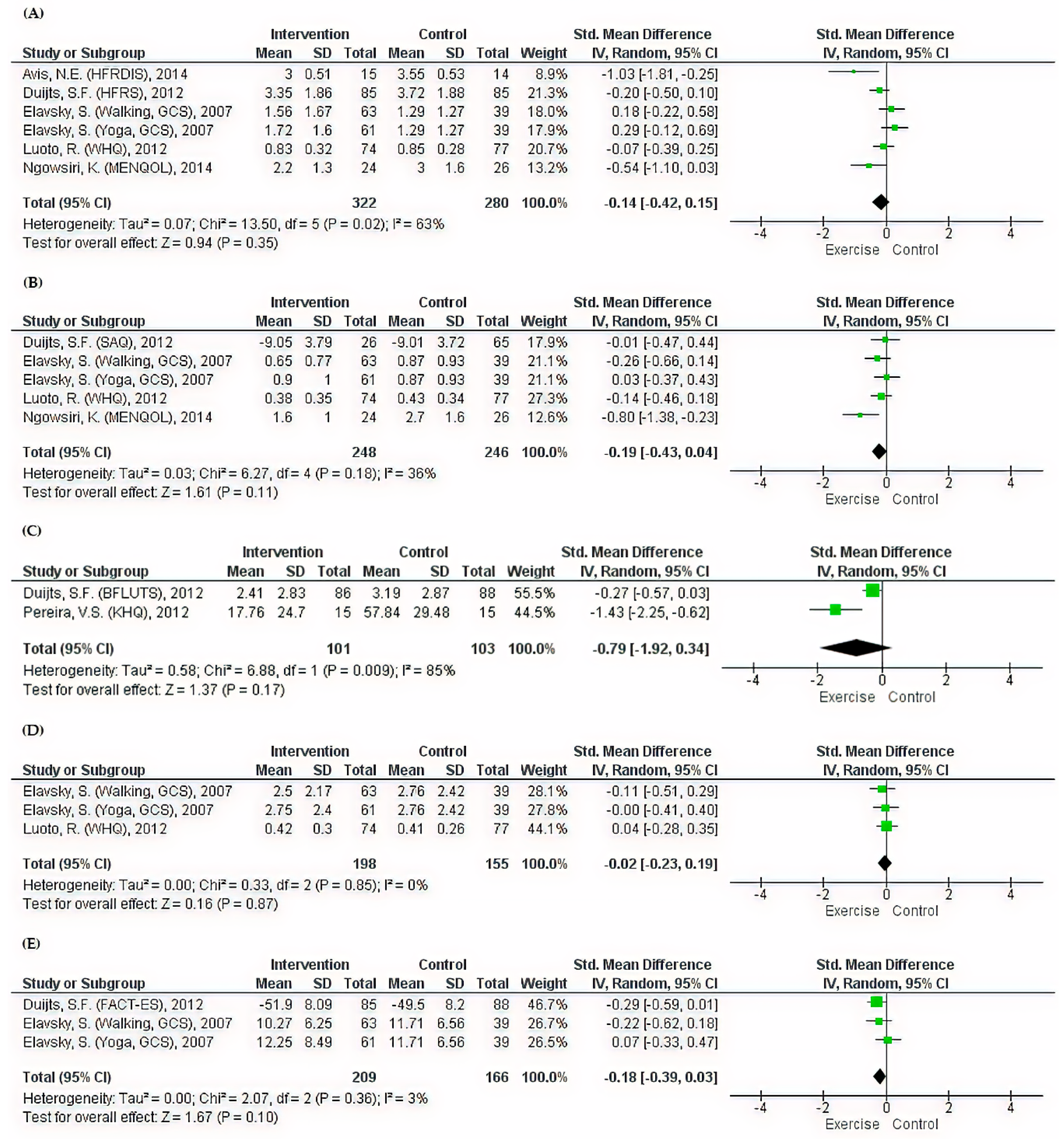
3.3. General Health QoL Outcomes
3.4. Menopause-Specific QoL Outcomes
3.5. Subgroup Analyses
3.6. Risk-of-Bias Assessment
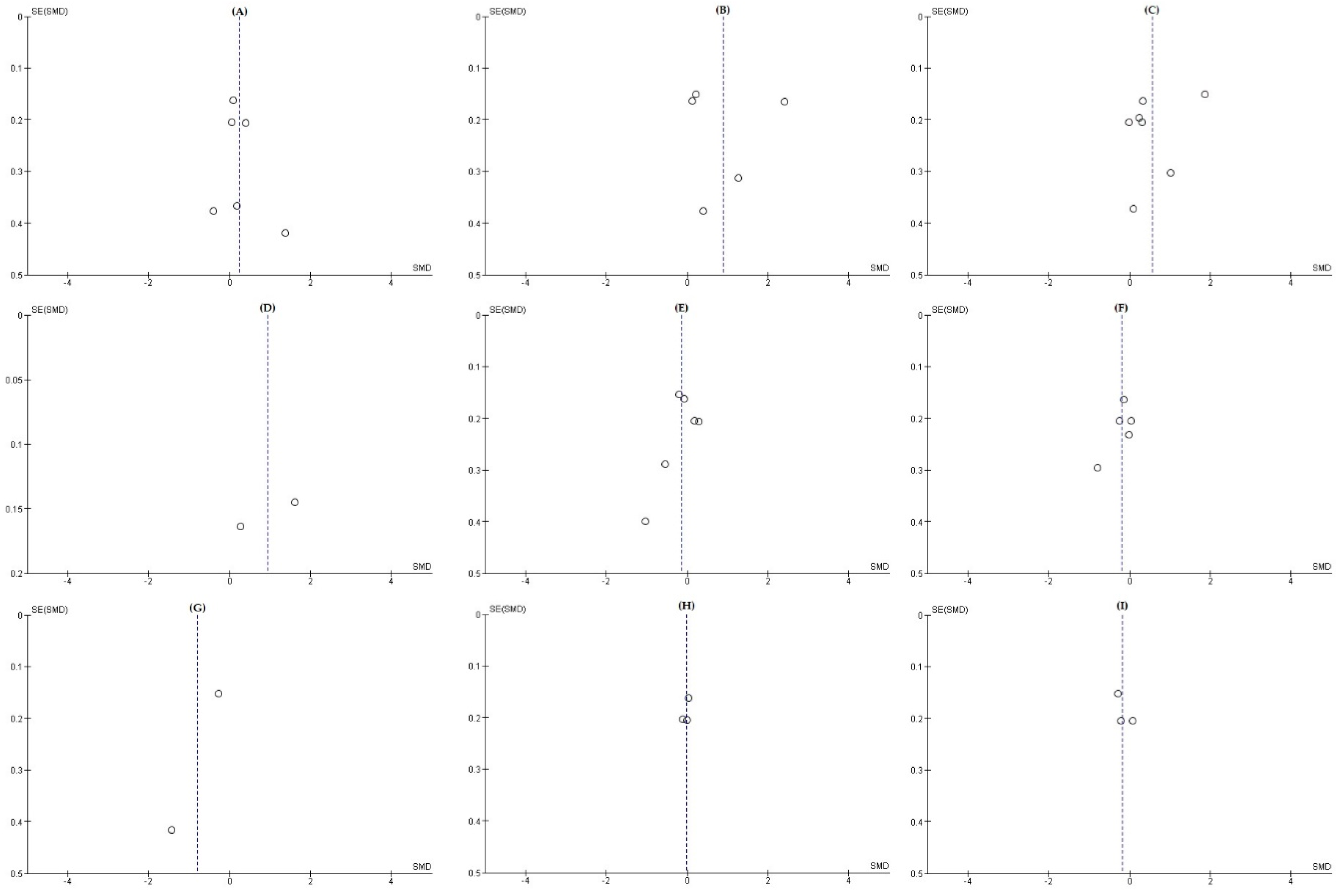
3.7. Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Population | Outcomes | Intervention | Study Design |
|---|---|---|---|
| Menopause Climacteric Hot flash Night sweat Vasomotor symptom | Quality of life Life quality Value of life Quality of well-being QoL HRQoL HRQL QWB | Exercise Physical activity Yoga Tai Ji Qi Gong Aerobics Sport Pilates Movement Walking Swimming Running Training Dancing Climbing | Randomized controlled trials Controlled clinical trials Trials Randomly Randomized Groups RCTs |
References
- NIH State-of-the-Science Conference Statement on management of menopause-related symptoms. NIH Consens. State-Sci. Statements 2005, 22, 1–38.
- Soules, M.R.; Sherman, S.; Parrott, E.; Rebar, R.; Santoro, N.; Utian, W.; Woods, N. Executive summary: Stages of Reproductive Aging Workshop (STRAW). Climacteric 2001, 4, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Wan, J.; Gai, Y.; Li, G.; Tao, Z.; Zhang, Z. Incidence of chemotherapy- and chemoradiotherapy-induced amenorrhea in premenopausal women with stage II/III colorectal cancer. Clin. Colorectal Cancer 2015, 14, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Santoro, N.; Epperson, C.N.; Mathews, S.B. Menopausal symptoms and their management. Endocrin. Metab. Clin. 2015, 44, 497–515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ACOG Practice Bulletin No. 141: Management of menopausal symptoms. Obstet. Gynecol. 2014, 123, 202–216.
- Santoro, N.; Komi, J. Prevalence and impact of vaginal symptoms among postmenopausal women. J. Sex. Med. 2009, 6, 2133–2142. [Google Scholar] [CrossRef]
- Ambler, D.R.; Bieber, E.J.; Diamond, M.P. Sexual function in elderly women: A review of current literature. Rev. Obstet. Gynecol. 2012, 5, 16–27. [Google Scholar]
- Rathnayake, N.; Lenora, J.; Alwis, G.; Lekamwasam, S. Prevalence and severity of menopausal symptoms and the quality of life in middle-aged women: A study from Sri Lanka. Nurs. Res. Pract. 2019, 2019, 2081507. [Google Scholar] [CrossRef] [Green Version]
- Fuh, J.L.; Wang, S.J.; Lee, S.J.; Lu, S.R.; Juang, K.D. Quality of life and menopausal transition for middle-aged women on Kinmen island. Qual. Life Res. 2003, 12, 53–61. [Google Scholar] [CrossRef]
- Avis, N.E.; Colvin, A.; Bromberger, J.T.; Hess, R.; Matthews, K.A.; Ory, M.; Schocken, M. Change in health-related quality of life over the menopausal transition in a multiethnic cohort of middle-aged women: Study of Women’s Health Across the Nation. Menopause 2009, 16, 860–869. [Google Scholar] [CrossRef] [Green Version]
- Fayers, P.M.; Machin, D. Quality of Life: The Assessment, Analysis and Reporting of Patient-Reported Outcomes, 3rd ed.; Wiley Blackwell: Hoboken, NJ, USA, 2016; pp. 1–33. [Google Scholar]
- Nelson, H.D.; Haney, E.; Humphrey, L.; Miller, J.; Nedrow, A.; Nicolaidis, C.; Vesco, K.; Walker, M.; Bougatsos, C.; Nygren, P. Management of menopause-related symptoms: Summary. In AHRQ Evidence Report Summaries; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2005; Volume 120. Available online: https://www.ncbi.nlm.nih.gov/books/NBK11956/ (accessed on 22 July 2020).
- The 2017 hormone therapy position statement of the North American Menopause Society. Menopause 2018, 24, 728–753.
- Portman, D.J.; Gass, M.L. Genitourinary syndrome of menopause: New terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Menopause 2014, 21, 1063–1068. [Google Scholar] [CrossRef] [PubMed]
- Rossouw, J.E.; Anderson, G.L.; Prentice, R.L.; LaCroix, A.Z.; Kooperberg, C.; Stefanick, M.L.; Jackson, R.D.; Beresford, S.A.; Howard, B.V.; Johnson, K.C.; et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results from the Women’s Health Initiative randomized controlled trial. JAMA 2002, 288, 321–333. [Google Scholar] [PubMed] [Green Version]
- Posadzki, P.; Lee, M.S.; Moon, T.W.; Choi, T.Y.; Park, T.Y.; Ernst, E. Prevalence of complementary and alternative medicine (CAM) use by menopausal women: A systematic review of surveys. Maturitas 2013, 75, 34–43. [Google Scholar] [CrossRef]
- Peng, W.; Adams, J.; Sibbritt, D.W.; Frawley, J.E. Critical review of complementary and alternative medicine use in menopause: Focus on prevalence, motivation, decision-making, and communication. Menopause 2014, 21, 536–548. [Google Scholar] [CrossRef]
- Franco, O.H.; Chowdhury, R.; Troup, J.; Voortman, T.; Kunutsor, S.; Kavousi, M.; Oliver-Williams, C.; Muka, T. Use of plant-based therapies and menopausal symptoms: A systematic review and meta-analysis. JAMA 2016, 315, 2554–2563. [Google Scholar] [CrossRef] [Green Version]
- Huntley, A.L.; Ernst, E. A systematic review of herbal medicinal products for the treatment of menopausal symptoms. Menopause 2003, 10, 465–476. [Google Scholar] [CrossRef]
- Bair, Y.A.; Gold, E.B.; Zhang, G.; Rasor, N.; Utts, J.; Upchurch, D.M.; Chyu, L.; Greendale, G.A.; Sternfeld, B.; Adler, S.R. Use of complementary and alternative medicine during the menopause transition: Longitudinal results from the Study of Women’s Health Across the Nation. Menopause 2008, 15, 32–43. [Google Scholar] [CrossRef]
- Asikainen, T.M.; Kukkonen-Harjula, K.; Miilunpalo, S. Exercise for health for early postmenopausal women: A systematic review of randomised controlled trials. Sports Med. 2004, 34, 753–778. [Google Scholar] [CrossRef]
- Sternfeld, B.; Dugan, S. Physical activity and health during the menopausal transition. Obstet. Gynecol. Clin. N. Am. 2011, 38, 537–566. [Google Scholar] [CrossRef] [Green Version]
- Warburton, D.E.R.; Bredin, S.S.D. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef] [PubMed]
- Mercier, J.; Morin, M.; Zaki, D.; Reichetzer, B.; Lemieux, M.C.; Khalife, S.; Dumoulin, C. Pelvic floor muscle training as a treatment for genitourinary syndrome of menopause: A single-arm feasibility study. Maturitas 2019, 125, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Bertotto, A.; Schvartzman, R.; Uchoa, S.; Wender, M.C.O. Effect of electromyographic biofeedback as an add-on to pelvic floor muscle exercises on neuromuscular outcomes and quality of life in postmenopausal women with stress urinary incontinence: A randomized controlled trial. Neurourol. Urodynam. 2017, 36, 2142–2147. [Google Scholar] [CrossRef] [PubMed]
- Ngowsiri, K.; Tanmahasamut, P.; Sukonthasab, S. Rusie Dutton traditional Thai exercise promotes health related physical fitness and quality of life in menopausal women. Complement. Ther. Clin. Pract. 2014, 20, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Jayabharathi, B.; Judie, A. Complementary health approach to quality of life in menopausal women: A community-based interventional study. Clin. Interv. Aging 2014, 9, 1913–1921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Avis, N.E.; Legault, C.; Russell, G.; Weaver, K.; Danhauer, S.C. Pilot study of integral yoga for menopausal hot flashes. Menopause 2014, 21, 846–854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pereira, V.S.; de Melo, M.V.; Correia, G.N.; Driusso, P. Vaginal cone for postmenopausal women with stress urinary incontinence: Randomized, controlled trial. Climacteric 2012, 15, 45–51. [Google Scholar] [CrossRef]
- Luoto, R.; Moilanen, J.; Heinonen, R.; Mikkola, T.; Raitanen, J.; Tomas, E.; Ojala, K.; Mansikkamaki, K.; Nygard, C.H. Effect of aerobic training on hot flushes and quality of life-a randomized controlled trial. Ann. Med. 2012, 44, 616–626. [Google Scholar] [CrossRef]
- Duijts, S.F.; van Beurden, M.; Oldenburg, H.S.; Hunter, M.S.; Kieffer, J.M.; Stuiver, M.M.; Gerritsma, M.A.; Menke-Pluymers, M.B.; Plaisier, P.W.; Rijna, H.; et al. Efficacy of cognitive behavioral therapy and physical exercise in alleviating treatment-induced menopausal symptoms in patients with breast cancer: Results of a randomized, controlled, multicenter trial. J. Clin. Oncol. 2012, 30, 4124–4133. [Google Scholar] [CrossRef]
- Elavsky, S.; McAuley, E. Physical activity and mental health outcomes during menopause: A randomized controlled trial. Ann. Behav. Med. 2007, 33, 132–142. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horsley, T.; Dingwall, O.; Sampson, M. Checking reference lists to find additional studies for systematic reviews. Cochrane Database Syst. Rev. 2011, 8, MR000026. [Google Scholar] [CrossRef]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hyland, M.E.; Sodergren, S.C. Development of a new type of global quality of life scale, and comparison of performance and preference for 12 global scales. Qual. Life. Res. 1996, 5, 469–480. [Google Scholar] [CrossRef]
- Hooker, S.A. SF-36. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 1784–1786. [Google Scholar]
- Division of Mental Health. WHOQOL-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment: Field Trial Version; World Health Organization: Geneva, Switzerland, 1996; Available online: https://apps.who.int/iris/handle/10665/63529 (accessed on 22 July 2020).
- Utian, W.H.; Janata, J.W.; Kingsberg, S.A.; Schluchter, M.; Hamilton, J.C. The Utian Quality of Life (UQOL) scale: Development and validation of an instrument to quantify quality of life through and beyond menopause. Menopause 2018, 25, 1224–1231. [Google Scholar] [CrossRef]
- Radtke, J.V.; Terhorst, L.; Cohen, S.M. The Menopause-Specific Quality of Life questionnaire: Psychometric evaluation among breast cancer survivors. Menopause 2011, 18, 289–295. [Google Scholar] [CrossRef] [Green Version]
- Abrams, P.; Cardozo, L.; Wein, A. 3rd International Consultation on Incontinence—Research Society 2011. Neurourol. Urodyn. 2012, 31, 291–292. [Google Scholar] [CrossRef]
- Kelleher, C.J.; Cardozo, L.D.; Khullar, V.; Salvatore, S. A new questionnaire to assess the quality of life of urinary incontinent women. Br. J. Obstet. Gynaecol. 1997, 104, 1374–1379. [Google Scholar] [CrossRef]
- Thirlaway, K.; Fallowfield, L.; Cuzick, J. The Sexual Activity Questionnaire: A measure of women’s sexual functioning. Qual. Life Res. 1996, 5, 81–90. [Google Scholar] [CrossRef]
- Greene, J.G. Constructing a standard climacteric scale. Maturitas 1998, 29, 25–31. [Google Scholar] [CrossRef]
- Hunter, M. The Women’s Health Questionnaire (WHQ): The development, standardization and application of a measure of mid-aged women’s emotional and physical health. Qual. Life Res. 2000, 9, 733–738. [Google Scholar] [CrossRef]
- Carpenter, J.S. The Hot Flash Related Daily Interference Scale: A tool for assessing the impact of hot flashes on quality of life following breast cancer. J. Pain Symptom Manag. 2001, 22, 979–989. [Google Scholar] [CrossRef]
- Hunter, M.S.; Liao, K.L. A psychological analysis of menopausal hot flushes. Br. J. Clin. Psychol. 1995, 34, 589–599. [Google Scholar] [CrossRef]
- Jackson, S.; Donovan, J.; Brookes, S.; Eckford, S.; Swithinbank, L.; Abrams, P. The Bristol Female Lower Urinary Tract Symptoms questionnaire: Development and psychometric testing. Br. J. Urol. 1996, 77, 805–812. [Google Scholar] [CrossRef]
- Fallowfield, L.J.; Leaity, S.K.; Howell, A.; Benson, S.; Cella, D. Assessment of quality of life in women undergoing hormonal therapy for breast cancer: Validation of an endocrine symptom subscale for the FACT-B. Breast Cancer Res. Treat. 1999, 55, 189–199. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; The Cochrane Collaboration: London, UK, 2011; Available online: www.handbook.cochrane.org (accessed on 22 July 2020).
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.T.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J. The t test for means. In Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: New York, NY, USA, 1988; pp. 19–66. [Google Scholar]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [Green Version]
- Cramer, H.; Peng, W.; Lauche, R. Yoga for menopausal symptoms: A systematic review and meta-analysis. Maturias 2018, 109, 13–25. [Google Scholar] [CrossRef]
- van Driel, C.M.; Stuursma, A.; Schroevers, M.J.; Mourits, M.J.; de Bock, G.H. Mindfulness, cognitive behavioural and behaviour-based therapy for natural and treatment-induced menopausal symptoms: A systematic review and meta-analysis. BJOG 2019, 126, 330–339. [Google Scholar] [CrossRef]
- Daley, A.; Stokes-Lampard, H.; Thomas, A.; MacArthur, C. Exercise for vasomotor menopausal symptoms. Cochrane Database Syst. Rev. 2014, 11, CD006108. [Google Scholar] [CrossRef] [PubMed]
- Carcelen-Fraile, M.D.C.; Aibar-Almazan, A.; Martinez-Amat, A.; Cruz-Diaz, D.; Diaz-Mohedo, E.; Redecillas-Peiro, M.T.; Hita-Contreras, F. Effects of physical exercise on sexual function and quality of sexual life related to menopausal symptoms in peri- and postmenopausal women: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 2680. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woods, N.F.; Mitchell, E.S. Symptoms during the perimenopause: Prevalence, severity, trajectory, and significance in women’s lives. Am. J. Med. 2005, 118 (Suppl. 12B), 14–24. [Google Scholar] [CrossRef] [Green Version]
- Hoga, L.; Rodolpho, J.; Goncalves, B.; Quirino, B. Women’s experience of menopause: A systematic review of qualitative evidence. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 250–337. [Google Scholar] [CrossRef]
- Division of Mental Health and Prevention of Substance Abuse. WHOQOL: Measuring Quality of Life; World Health Organization: Geneva, Switzerland, 1997; Available online: https://apps.who.int/iris/handle/10665/63482 (accessed on 22 July 2020).
- Villaverde-Gutierrez, C.; Araujo, E.; Cruz, F.; Roa, J.M.; Barbosa, W.; Ruiz-Villaverde, G. Quality of life of rural menopausal women in response to a customized exercise programme. J. Adv. Nurs. 2006, 54, 11–19. [Google Scholar] [CrossRef]
- Dabrowska, J.; Dabrowska-Galas, M.; Rutkowska, M.; Michalski, B.A. Twelve-week exercise training and the quality of life in menopausal women—Clinical trial. Prz. Menopauzalny 2016, 15, 20–25. [Google Scholar] [CrossRef]
- Asghari, M.; Mirghafourvand, M.; Mohammad-Alizadeh-Charandabi, S.; Malakouti, J.; Nedjat, S. Effect of aerobic exercise and nutrition education on quality of life and early menopause symptoms: A randomized controlled trial. Women Health 2017, 57, 173–188. [Google Scholar] [CrossRef] [PubMed]
- Asgari, P.; Bahramnezhad, F.; Narenji, F.; Golitaleb, M.; Askari, M. A clinical study of the effect of Glycyrrhiza glabra plant and exercise on the quality of life of menopausal women. Chronic Dis. J. 2015, 3, 79–86. [Google Scholar]
- Atapattu, P.M.; Fernando, D.; Wasalathanthri, S.; de Silva, A. Menopause and exercise: Linking pathophysiology to effects. Arch. Med. 2015, 28, 1–8. [Google Scholar]
- Jenabi, E.; Shobeiri, F.; Hazavehei, S.M.; Roshanaei, G. Assessment of questionnaire measuring quality of life in menopausal women: A systematic review. Oman Med. J. 2015, 30, 151–156. [Google Scholar] [CrossRef]
- Dumoulin, C.; Morin, M.; Mayrand, M.H.; Tousignant, M.; Abrahamowicz, M. Group physiotherapy compared to individual physiotherapy to treat urinary incontinence in aging women: Study protocol for a randomized controlled trial. Trials 2017, 18, 544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cacciari, L.P.; Dumoulin, C.; Hay-Smith, E.J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: A cochrane systematic review abridged republication. Braz. J. Phys. Ther. 2019, 23, 93–107. [Google Scholar] [CrossRef] [PubMed]

| QoL Questionnaire | Abbreviation | Type 2 | QoL Domain 3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| General Health | Menopause-Specific | ||||||||||
| General | Physical | Psychological | Social | Vasomotor | Sexual | Urinary | Somatic | Total Symptoms | |||
| Global QoL [37] | GQOL/VAS 1 | G | P | - | - | - | - | - | - | - | - |
| 36-Item Short-Form Health Survey [38] | SF-36 | G | P | P | P | P | - | - | - | - | - |
| World Health Organization QoL—Brief Version [39] | WHOQOL-BREF | G | - | P | P | P | - | - | - | - | - |
| Utian QoL [40] | UQOL | S | P | - | N | - | - | - | - | - | - |
| Menopause-Specific QoL [41] | MENQOL | S | - | N | N | - | N | N | - | - | - |
| International Consultation on Incontinence Questionnaire (Short Form) [42] | ICIQ-SF | S | N | - | - | - | - | - | - | - | - |
| King’s Health Questionnaire [43] | KHQ | S | N | - | - | - | - | - | N | - | - |
| Sexual Activity Questionnaire [44] | SAQ | S | - | - | - | - | - | P | - | - | - |
| Greene Climacteric Scale [45] | GCS | S | - | - | - | - | N | N | - | N | N |
| Women’s Health Questionnaire [46] | WHQ | S | - | - | - | - | N | N | - | N | - |
| Hot-Flash-Related Daily Interference Scale [47] | HFRDIS | S | - | - | - | - | N | - | - | - | - |
| Hot Flash Rating Scale [48] | HFRS | S | - | - | - | - | N | - | - | - | - |
| Bristol Female Lower Urinary Tract Symptoms [49] | BFLUTS | S | - | - | - | - | - | - | N | - | - |
| Functional Assessment of Cancer Therapy for Endocrine Subscale [50] | FACT-ES | S | - | - | - | - | - | - | - | - | P |
| Study | Participant | Country | Dropout Rate | Intervention | Frequency 1 | Duration 1 | Control | QoL Questionnaire | Result |
|---|---|---|---|---|---|---|---|---|---|
| Mercier et al. [24] | 32 women with GSM; ≥55 years old | Canada | 9.4% (3/32) | PFMT; Supervised and home-based (n = 32) | Supervised: 1 b/w, 60 min/b Home-based: 5 d/w | 12 w | None (n = 0) | ICIQ-VS | QoL and sexual function of women with GSM improved after the intervention. |
| Bertotto et al. [25] | 49 postmenopausal women with urinary symptoms; 50–65 years old | Brazil | 8.2% (4/49) | PFMT: contraction (n = 15) | 2 b/w, 20 min/b | 4 w | No treatment (n = 14) | ICIQ-SF | The PFMT group exhibited significant increases in ICIQ-SF scores. |
| Ngowsiri et al. [26] | 54 menopausal women with menopausal symptoms; 45–59 years old | Thailand | 7.4% (4/54) | Rusie Dutton dance of 16 yoga-like postures; Supervised (n = 24) | 3 b/w, 90 min/b | 13 w | Provided a handbook (n = 26) | MENQOL | There was a significant improvement in all MENQOL domains in the experiment group and between the two groups. |
| Jayabharathi et al. [27] | 260 women with menopausal symptoms; 45–55 years old | India | 2.3% (6/260) | Yoga; Supervised and home-based (n = 128) | Supervised: 5 consecutive days: 2 b/d, ~45 min/b; Later: 2 d/w Home-based: 35–40 min/d | 18 w | No intervention (n = 126) | WHOQOL-BREF | A statistically significant difference between the study group and the control group was observed in terms of all domains of QoL. |
| Avis et al. [28] | 54 menopausal women with ≥4 hot flashes/day; 45–58 years old | USA | 20.4% (11/54) | Integral yoga Supervised and home-based qualified DVD for self-practice (n = 15) | Supervised: 1 b/w, 90 min/b Home-based: 3 b/w, 15 min/b | 10 w | Waitlist (n = 14) | SF-36 HFRDIS VAS | Yoga can act as a behavioral option which helps in reducing hot flashes. There was no advantage of yoga over other types of exercise. |
| Pereira et al. [29] | 45 postmenopausal women with urinary symptoms; 53–73 years old | Brazil | 8.9% (4/45) | PFMT: contraction; Supervised by a physical therapist (n = 15) | 2 b/w, 40 min/b | 6 w | No intervention (n = 15) | KHQ | Several positive results of PFMT in treatment for urinary leakage, pelvic floor muscle pressure, and QoL were observed. |
| Luoto et al. [30] | 176 menopausal women with daily hot flashes; 40–63 years old | Finland | 12.5% (22/176) | Unsupervised aerobic training (n = 74) | 4 b/w, 50 min/b | 24 w | 1–2 lectures/ month; 60–75 min (n = 80) | SF-36 WHQ | Women in the intervention group had significantly higher SF-36 scores in mental health than those in the control group. |
| Duijts et al. [31] | 422 breast cancer patients with menopause symptoms; 48.2 ± 5.6 years old | The Netherlands | 16.6% (70/422) | Home-based, self-directed exercise program; Assisted by a physiotherapist (n = 104) | Home-based: 150–180 min/w | 12 w | Waitlist (n = 103) | SF-36 HFRS SAQ FACT-ES BFLUTS | There were significant differences in improvement for menopause symptoms, SAQ, and SF-36 between the intervention and the control group. |
| Elavsky et al. [32] | 164 sedentary women with menopausal symptoms; 42–58 years old | USA | 24.4% (40/164) | (1) Walking: supervised; (n = 63) (2) Iyengar yoga: supervised (n = 62) | (1) 3 b/w; 60 min/b; (2) 2 b/w; 90 min/b | 16 w | Waitlist (n = 39) | UQOL GCS | The yoga and walking interventions showed positive effects on menopause-specific QoL. |
| QoL Domain | No. Studies | No. Participants (Exercise) | No. Participants (Control) | SMD (95% CI) | p-Value | Heterogeneity 1 I2; χ2; p-Value |
|---|---|---|---|---|---|---|
| PFMT | ||||||
| General | 2 | 30 | 29 | 0.76 (−0.40 to 1.92) | 0.20 | 78%; 4.52; 0.03 |
| Yoga | ||||||
| General | 2 | 76 | 53 | −0.07 (−0.46 to 0.33) | 0.74 | 12%; 1.14; 0.29 |
| Physical | 3 | 167 | 166 | 1.39 (0.19 to 2.59) | 0.02 | 93%; 29.31; p * |
| Psychological | 4 | 228 | 205 | 0.76 (−0.3 to 1.81) | 0.16 | 95%; 63.01; p * |
| Sexual | 2 | 85 | 65 | −0.36 (−1.18 to 0.46) | 0.39 | 81%; 5.39; 0.02 |
| Vasomotor | 3 | 100 | 79 | −0.37 (−1.15 to 0.4) | 0.34 | 82%; 11.18; p ** |
| Study | RandomIzation Process | Deviations from Intended Interventions | Missing Outcome Data | Measurement of the Outcome | Selection of the Reported Result | Overall |
|---|---|---|---|---|---|---|
| Mercier et al. [24] | Low | Some concerns | Low | Low | Low | Some concerns |
| Bertotto et al. [25] | Low | Some concerns | Some concerns | Some concerns | Low | Some concerns |
| Ngowsiri et al. [26] | Some concerns | Some concerns | Some concerns | Some concerns | Low | Some concerns |
| Jayabharathi et al. [27] | Low | Some concerns | Low | Some concerns | Low | Some concerns |
| Avis et al. [28] | Some concerns | Some concerns | Some concerns | Some concerns | Low | Some concerns |
| Pereira et al. [29] | Low | Some concerns | Low | Some concerns | Low | Some concerns |
| Luoto et al. [30] | Low | High | Some concerns | Some concerns | Low | High |
| Duijts et al. [31] | Low | Some concerns | Low | Some concerns | Low | Some concerns |
| Elavsky et al. [32] | Low | Some concerns | Some concerns | Low | Low | Some concerns |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, T.M.; Do, T.T.T.; Tran, T.N.; Kim, J.H. Exercise and Quality of Life in Women with Menopausal Symptoms: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2020, 17, 7049. https://doi.org/10.3390/ijerph17197049
Nguyen TM, Do TTT, Tran TN, Kim JH. Exercise and Quality of Life in Women with Menopausal Symptoms: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. International Journal of Environmental Research and Public Health. 2020; 17(19):7049. https://doi.org/10.3390/ijerph17197049
Chicago/Turabian StyleNguyen, Thi Mai, Thi Thanh Toan Do, Tho Nhi Tran, and Jin Hee Kim. 2020. "Exercise and Quality of Life in Women with Menopausal Symptoms: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" International Journal of Environmental Research and Public Health 17, no. 19: 7049. https://doi.org/10.3390/ijerph17197049