Tuberculosis and Other Airborne Microbes in Occupational Health and Safety
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey Data Collection and Handling
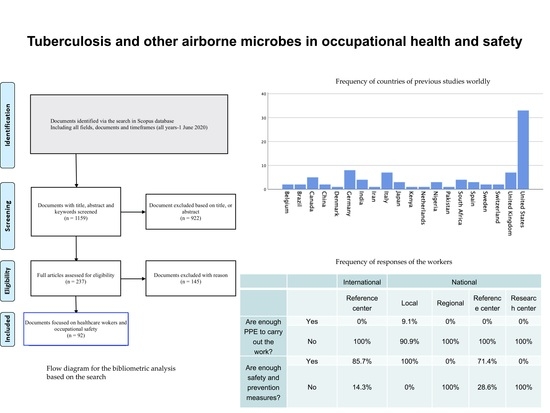
2.2. Bibliographic Search
3. Results
3.1. Results of the Survey
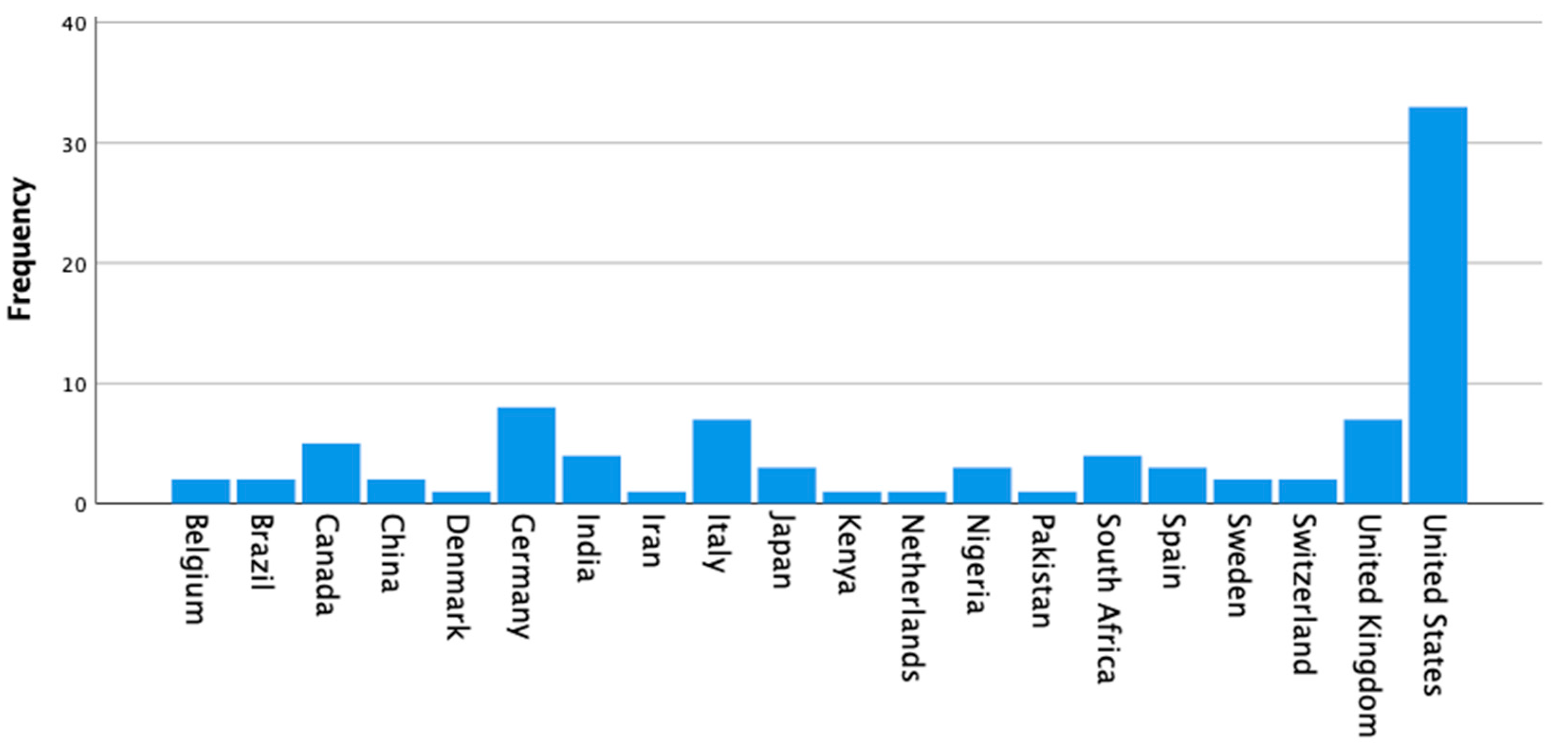
3.2. Results of the Bibliographic Search
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Chiodi, M.B.; Marziale, M.H.P.; Robazzi, M.L.D.C.C. Occupational accidents involving biological material among public health workers. Rev. Lat. Am. Enferm. 2007, 15, 632–638. [Google Scholar] [CrossRef] [PubMed]
- Harrison, J. Occupational Safety and Health in the United Kingdom: Securing Future Workplace Health and Wellbeing. Ind. Health 2012, 50, 261–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niemand, A.; Jordaan, A.J.; Minnaar, H. Some international perspectives on legislation for the management of human-induced safety risks. Jàmbá J. Disaster Risk Stud. 2016, 8, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aiello, A.E. Invited Commentary: Evolution of Social Networks, Health, and the Role of Epidemiology. Am. J. Epidemiol. 2017, 185, 1089–1092. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, E. La salud publica en España en el contexto europeo, 1890–1925. Rev. Sanid. Hig. Pública. 1994, 68, 11–27. [Google Scholar]
- De Almeida, M.C.M.; da Canini, S.R.M.S.; Reis, R.K.; Toffano, S.E.M.; Pereira, F.M.V.; Gir, E. Clinical treatment adherence of health care workers and students exposed to potentially infectious biological material. Rev. Esc. Enferm. USP 2015, 49, 259–264. [Google Scholar] [CrossRef] [Green Version]
- Bianchini, A.; Donini, F.; Pellegrini, M.; Saccani, C. An innovative methodology for measuring the effective implementation of an Occupational Health and Safety Management System in the European Union. Saf. Sci. 2017, 92, 26–33. [Google Scholar] [CrossRef]
- Colosio, C.; Mandic-Rajcevic, S.; Godderis, L.; van der Laan, G.; Hulshof, C.; van Dijk, F. Workers’ health surveillance: Implementation of the Directive 89/391/EEC in Europe. Occup. Med. Oxf. Engl. 2017, 67, 574–578. [Google Scholar] [CrossRef] [Green Version]
- Rafiei, M.; Ezzatian, R.; Farshad, A.; Sokooti, M.; Tabibi, R.; Colosio, C. Occupational Health Services Integrated in Primary Health Care in Iran. Ann. Glob. Health 2015, 81, 561. [Google Scholar] [CrossRef] [Green Version]
- Díaz, D.B.; García, R.R.; Baraibar, D.E. Key Corporate Social Responsibility Initiatives: An Empirical Evidence from Spain. In Key Initiatives in Corporate Social Responsibility: Global Dimension of CSR in Corporate Entities; Idowu, S.O., Ed.; CSR, Sustainability, Ethics & Governance; Springer International Publishing: New York, NY, USA, 2016; pp. 71–102. ISBN 978-3-319-21641-6. [Google Scholar]
- Kim, Y.; Park, J.; Park, M. Creating a Culture of Prevention in Occupational Safety and Health Practice. Saf. Health Work 2016, 7, 89–96. [Google Scholar] [CrossRef] [Green Version]
- Schulte, P.; Vainio, H. Well-being at work—Overview and perspective. Scand. J. Work. Environ. Health 2010, 36, 422–429. [Google Scholar] [CrossRef] [Green Version]
- Ncube, F.; Kanda, A. Current Status and the Future of Occupational Safety and Health Legislation in Low- and Middle-Income Countries. Saf. Health Work 2018, 9, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Apisarnthanarak, A.; Babcock, H.M.; Fraser, V.J. The effect of nondevice interventions to reduce needlestick injuries among health care workers in a Thai tertiary care center. Am. J. Infect. Control 2008, 36, 74–75. [Google Scholar] [CrossRef] [PubMed]
- Hernández, N.M.J.; Montes, V.F.J.; Solano, B.V.M.; Sánchez, M.D.; del Val García, J.L.; Gil, M.E.; Arribas, L.J.L. Accidents with biological material in health care workers in two primary health care areas (1990–1999). Aten. Primaria 2001, 28, 255–258. [Google Scholar]
- Spinazzè, A.; Cattaneo, A.; Cavallo, D.M. COVID-19 Outbreak in Italy: Protecting Worker Health and the Response of the Italian Industrial Hygienists Association. Ann. Work Expo. Health 2020, wxaa044. [Google Scholar] [CrossRef] [Green Version]
- Friese, C.R.; Veenema, T.G.; Johnson, J.S.; Jayaraman, S.; Chang, J.C.; Clever, L.H. Respiratory Protection Considerations for Healthcare Workers during the COVID-19 Pandemic. Health Secur. 2020, 18, 237–240. [Google Scholar] [CrossRef] [Green Version]
- Peng, C.-T.; Wu, T.-Y.; Chen, Y.; Atkin, D.J. Comparing and modeling via social media: The social influences of fitspiration on male instagram users’ work out intention. Comput. Hum. Behav. 2019, 99, 156–167. [Google Scholar] [CrossRef]
- Vaquero, M.; Gómez, P.; Romero, M.; Casal, M.J. Investigation of biological risk in mycobacteriology laboratories: A multicentre study. Int. J. Tuberc. Lung Dis. 2003, 7, 879–885. [Google Scholar]
- Coelho, A.C.; García Díez, J. Biological Risks and Laboratory-Acquired Infections: A Reality That Cannot be Ignored in Health Biotechnology. Front. Bioeng. Biotechnol. 2015, 3, 56. [Google Scholar] [CrossRef] [Green Version]
- Heinzerling, A.; Stuckey, M.J.; Scheuer, T.; Xu, K.; Perkins, K.M.; Resseger, H.; Magill, S.; Verani, J.R.; Jain, S.; Acosta, M.; et al. Transmission of COVID-19 to Health Care Personnel During Exposures to a Hospitalized Patient—Solano County, California, February 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 472–476. [Google Scholar] [CrossRef] [Green Version]
- Coppeta, L.; Pietroiusti, A.; Neri, A.; Janni, A.; Baldi, S.; Papa, F.; Magrini, A. Prevalence and Risk Factors for Latent Tuberculosis Infection among Healthcare Workers in a Low Incidence Country. Open Respir. Med. J. 2019, 13, 1–4. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Universal health coverage, multisectoral action and social determinants. In Global Tuberculosis Report 2019; World Health Organization: Geneva, Switzerland, 2019; pp. 141–163. ISBN 978-92-4-156571-4. [Google Scholar]
- Coppeta, L.; Pietroiusti, A.; Balbi, O.; Baldi, S. QuantiFERON-TB Gold Plus evaluation for latent tuberculosis infection among Italian healthcare workers: A cross-sectional study. Epidemiol. Biostat. Public Health 2019, 16. [Google Scholar] [CrossRef]
- Durando, P.; Sotgiu, G.; Spigno, F.; Piccinini, M.; Mazzarello, G.; Viscoli, C.; Copello, F.; Poli, A.; Ansaldi, F.; Icardi, G. Latent tuberculosis infection and associated risk factors among undergraduate healthcare students in Italy: A cross-sectional study. BMC Infect. Dis. 2013, 13, 443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joshi, R.; Reingold, A.L.; Menzies, D.; Pai, M. Tuberculosis among health-care workers in low- and middle-income countries: A systematic review. PLoS Med. 2006, 3, e494. [Google Scholar] [CrossRef] [PubMed]
- Navarrete, M.J.H.; Marti, M.C.; Sanchez, E.V.M.; Perez, F.R.; Ilario, A.G.D.; Llorente, J.L.A. Occupational exposures to blood and biological material in healthcare workers. EPINETAC Project 1996–2000. Med. Clin. 2004, 122, 3–81. [Google Scholar]
- Verelst, F.; Kuylen, E.; Beutels, P. Indications for healthcare surge capacity in European countries facing an exponential increase in coronavirus disease (COVID-19) cases, March 2020. Eurosurveillance 2020, 25, 2000323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huh, S. How to train health personnel to protect themselves from SARS-CoV-2 (novel coronavirus) infection when caring for a patient or suspected case. J. Educ. Eval. Health Prof. 2020, 17, 10. [Google Scholar] [CrossRef]
- Ferioli, M.; Cisternino, C.; Leo, V.; Pisani, L.; Palange, P.; Nava, S. Protecting healthcare workers from SARS-CoV-2 infection: Practical indications. Eur. Respir. Rev. 2020, 29, 200068. [Google Scholar] [CrossRef]
- Bahl, P.; Doolan, C.; de Silva, C.; Chughtai, A.A.; Bourouiba, L.; MacIntyre, C.R. Airborne or Droplet Precautions for Health Workers Treating Coronavirus Disease 2019? J. Infect. Dis. 2020, jiaa189. [Google Scholar] [CrossRef] [Green Version]
- Seidler, A.; Nienhaus, A.; Diel, R. Review of Epidemiological Studies on the Occupational Risk of Tuberculosis in Low-Incidence Areas. Respiration 2005, 72, 431–446. [Google Scholar] [CrossRef]
- Kim, S.J.; Lee, S.-H.; Kim, I.; Kim, H.J.; Kim, S.; Rieder, H. Risk of occupational tuberculosis in National Tuberculosis Programme laboratories in Korea. Int. J. Tuberc. Lung Dis. 2007, 11, 138–142. [Google Scholar] [PubMed]
- Ridderhof, J.C.; van Deun, A.; Kam, K.M.; Narayanan, P.R.; Aziz, M.A. Roles of laboratories and laboratory systems in effective tuberculosis programmes. Bull. World Health Organ. 2007, 85, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Health and Safety Executive Coronavirus (COVID-19): Update. Available online: https://www.hse.gov.uk/toolbox/ppe.htm# (accessed on 11 May 2020).
- United States Department of Labor Laboratory Workers and Employers. Available online: https://www.osha.gov/SLTC/covid-19/laboratory.html (accessed on 11 May 2020).
- Jensen, P.A.; Lambert, L.A.; Iademarco, M.F.; Ridzon, R. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. Morb. Mortal. Wkly. Rep. 2005, 54, 1–141. [Google Scholar]
- Fuss, E.P.; Israel, E.; Baruch, N.; Roghmann, M.-C. Improved tuberculosis infection control practices in Maryland acute care hospitals. Am. J. Infect. Control 2000, 28, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Meredith, S.; Watson, J.M.; Citron, K.M.; Cockcroft, A.; Darbyshire, J.H. Are healthcare workers in England and Wales at increased risk of tuberculosis? BMJ 1996, 313, 522–525. [Google Scholar] [CrossRef] [Green Version]
- Slater, M.L.; Welland, G.; Pai, M.; Parsonnet, J.; Banaei, N. Challenges with QuantiFERON-TB Gold Assay for Large-Scale, Routine Screening of U.S. Healthcare Workers. Am. J. Respir. Crit. Care Med. 2013, 188, 1005–1010. [Google Scholar] [CrossRef]
- Casas, I.; Latorre, I.; Esteve, M.; Ruiz-Manzano, J.; Rodriguez, D.; Prat, C.; García-Olivé, I.; Lacoma, A.; Ausina, V.; Domínguez, J. Evaluation of Interferon-Gamma Release Assays in the Diagnosis of Recent Tuberculosis Infection in Health Care Workers. PLoS ONE 2009, 4, e6686. [Google Scholar] [CrossRef] [Green Version]
- Galgalo, T.; Dalal, S.; Cain, K.P.; Oeltmann, J.; Tetteh, C.; Kamau, J.G.; Njenga, M.K.; Breiman, R.F.; Chakaya, J.M.; Irimu, H.M.; et al. Tuberculosis risk among staff of a large public hospital in Kenya. Int. J. Tuberc. Lung Dis. 2008, 12, 949–954. [Google Scholar]
- McCarthy, K.M.; Scott, L.E.; Gous, N.; Tellie, M.; Venter, W.D.F.; Stevens, W.S.; Van Rie, A. High incidence of latent tuberculous infection among South African health workers: An urgent call for action. Int. J. Tuberc. Lung Dis. 2015, 19, 647–653. [Google Scholar] [CrossRef]
- Beggs, C.B.; Kerr, K.G.; Donnelly, J.K.; Sleigh, P.A.; Mara, D.D.; Cairns, G. An engineering approach to the control of Mycobacterium tuberculosis and other airborne pathogens: A UK hospital based pilot study. Trans. R. Soc. Trop. Med. Hyg. 2000, 94, 141–146. [Google Scholar] [CrossRef]
- Kato, M.; Osuga, K.; Fujita, M.; Jimba, M. Ensuring tuberculosis infection control to support greater involvement of people living with HIV in health care. Int. Health 2011, 3, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Aliabadi, A.A.; Rogak, S.N.; Bartlett, K.H.; Green, S.I. Preventing Airborne Disease Transmission: Review of Methods for Ventilation Design in Health Care Facilities. Adv. Prev. Med. 2011, 2011, 124064. [Google Scholar] [CrossRef] [PubMed]
- Giménez-Marín, A.; Rivas-Ruiz, F.; García-Raja, A.M.; Venta-Obaya, R.; Fusté-Ventosa, M.; Caballé-Martín, I.; Benítez-Estevez, A.; Quinteiro-García, A.I.; Bedini, J.L.; León-Justel, A.; et al. Assessment of patient safety culture in clinical laboratories in the Spanish National Health System. Biochem. Medica 2015, 25, 363–376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, H.; Bilal, M.; Iqbal, H. Improved Biosafety and Biosecurity Measures and/or Strategies to Tackle Laboratory-Acquired Infections and Related Risks. Int. J. Environ. Res. Public Health 2018, 15, 2697. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, R.M.; Brosseau, L.M. Aerosol transmission of infectious disease. J. Occup. Environ. Med. 2015, 57, 501–508. [Google Scholar] [CrossRef]
- Sydnor, E.R.M.; Perl, T.M. Hospital epidemiology and infection control in acute-care settings. Clin. Microbiol. Rev. 2011, 24, 141–173. [Google Scholar] [CrossRef] [Green Version]
- Wurtz, N.; Papa, A.; Hukic, M.; Di Caro, A.; Leparc-Goffart, I.; Leroy, E.; Landini, M.P.; Sekeyova, Z.; Dumler, J.S.; Bădescu, D.; et al. Survey of laboratory-acquired infections around the world in biosafety level 3 and 4 laboratories. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 1247–1258. [Google Scholar] [CrossRef] [Green Version]
- Rojo-Molinero, E.; Alados, J.C.; de la Pedrosa, E.G.G.; Leiva, J.; Pérez, J.L. Safety in the Microbiology laboratory. Enferm. Infecc. Microbiol. Clin. 2015, 33, 404–410. [Google Scholar] [CrossRef]
- Dudarev, A.A.; Karnachev, I.P.; Øyvind Odland, J. Occupational accidents in Russia and the Russian Arctic. Int. J. Circumpolar Health 2013, 72. [Google Scholar] [CrossRef] [Green Version]
- Turin, T.; Ahmed, S.; Vaska, M. Conducting a Literature Review in Health Research: Basics of the Approach, Typology and Methodology. J. Natl. Heart Found. Bangladesh 2016, 5, 44–51. [Google Scholar]
- Gopalakrishnan, S.; Ganeshkumar, P. Systematic Reviews and Meta-analysis: Understanding the Best Evidence in Primary Healthcare. J. Fam. Med. Prim. Care 2013, 2, 9–14. [Google Scholar]
- Altman, D.; Simera, I. Using Reporting Guidelines Effectively to Ensure Good Reporting of Health Research. In Guidelines for Reporting Health Research: A User’s Manual; Wiley: Hoboken, NJ, USA, 2014; pp. 32–40. [Google Scholar]
- Parrish, N.M.; Carroll, K.C. Role of the Clinical Mycobacteriology Laboratory in Diagnosis and Management of Tuberculosis in Low-Prevalence Settings. J. Clin. Microbiol. 2011, 49, 772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowen, R.; Benavides, R.; Colón-Franco, J.M.; Katzman, B.M.; Muthukumar, A.; Sadrzadeh, H.; Straseski, J.; Klause, U.; Tran, N. Best practices in mitigating the risk of biotin interference with laboratory testing. Clin. Biochem. 2019, 74, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ombelet, S.; Ronat, J.-B.; Walsh, T.; Yansouni, C.P.; Cox, J.; Vlieghe, E.; Martiny, D.; Semret, M.; Vandenberg, O.; Jacobs, J. Clinical bacteriology in low-resource settings: Today’s solutions. Lancet Infect. Dis. 2018, 18, e248–e258. [Google Scholar] [CrossRef]
- Weinstein, R.A.; Singh, K. Laboratory-Acquired Infections. Clin. Infect. Dis. 2009, 49, 142–147. [Google Scholar]
- Jilcha, K.; Kitaw, D. Industrial occupational safety and health innovation for sustainable development. Eng. Sci. Technol. Int. J. 2017, 20, 372–380. [Google Scholar] [CrossRef] [Green Version]
- Parsons, L.M.; Somoskövi, Á.; Gutierrez, C.; Lee, E.; Paramasivan, C.N.; Abimiku, A.; Spector, S.; Roscigno, G.; Nkengasong, J. Laboratory Diagnosis of Tuberculosis in Resource-Poor Countries: Challenges and Opportunities. Clin. Microbiol. Rev. 2011, 24, 314. [Google Scholar] [CrossRef] [Green Version]
- Gagliardi, D.; Marinaccio, A.; Valenti, A.; Iavicoli, S. Occupational Safety and Health in Europe: Lessons from the Past, Challenges and Opportunities for the Future. Ind. Health 2012, 50, 7–11. [Google Scholar] [CrossRef] [Green Version]
- de la Fuente, V.S.; López, M.A.C.; González, I.F.; Alcántara, O.J.G.; Ritzel, D.O. The impact of the economic crisis on occupational injuries. J. Saf. Res. 2014, 48, 77–85. [Google Scholar] [CrossRef]
- Kimman, T.G.; Smit, E.; Klein, M.R. Evidence-based biosafety: A review of the principles and effectiveness of microbiological containment measures. Clin. Microbiol. Rev. 2008, 21, 403–425. [Google Scholar] [CrossRef] [Green Version]
- Sadaf, R.; Munir, T.; Farrukh, S.; Abbasi, S. Prevalence of latent tuberculosis infection in healthcare workers in tertiary care hospitals of Pakistan. Pak. J. Med. Sci. 2020, 36, 198–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erawati, M.; Andriany, M. The Prevalence and Demographic Risk Factors for Latent Tuberculosis Infection (LTBI) Among Healthcare Workers in Semarang, Indonesia. J. Multidiscip. Healthc. 2020, 13, 197–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, X.; Jia, H.; Liu, F.; Pan, L.; Xing, A.; Gu, S.; Du, B.; Sun, Q.; Wei, R.; Zhang, Z. Prevalence and Risk Factors for Latent Tuberculosis Infection among Health Care Workers in China: A Cross-Sectional Study. PLoS ONE 2013, 8, e66412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shinnick, T.M.; Iademarco, M.F.; Ridderhof, J.C. National plan for reliable tuberculosis laboratory services using a systems approach. Recommendations from CDC and the Association of Public Health Laboratories Task Force on Tuberculosis Laboratory Services. Morb. Mortal. Wkly. Rep. 2005, 54, 1–12. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Plan to combat extensively drug-resistant tuberculosis: Recommendations of the Federal Tuberculosis Task Force. Morb. Mortal. Wkly. Rep. 2009, 58, 1–43. [Google Scholar]


| Procedure | Sample | N | Frequencies |
|---|---|---|---|
| Sent out survey email invitation to one worker of each center | 56 email survey email invitations sent | 32 for Spain (2 per the 17 regions, except for Ceuta and Melilla) in Spain (2 per region) 6 for other European centers 6 for American centers 4 for African centers 4 for Asian centers 4 for Australia/Oceanian centers | - |
| Average response of the surveys sent to each worker for each center | 30 surveys completed | 23 in Spain 4 in other European centers 3 in American centers 0 for Asian centers 0 for Australia/Oceanian centers | 71.9% in Spain 67.7% in European centers 50% in American centers 0% in Asian centers 0 in Australia/Oceanian centers |
| Workers of Each Center that Completed the Survey (N = 30) | |||
| Variables | Mean (SD) | N | Frequencies |
| Age | 42.3(7.4) | - | - |
| Sex | - | 20 men 10 women | 66.7% men 33.3% female |
| Ethnic background | - | 23 white (European) 3 Latino 2 African descent 2 undefined | 76.6% white (European) 10% Latino 6.7% African descent 6.7% undefined |
| Spanish and International | - | 23 Spanish workers 7 international workers | 76.7% Spanish 23.3% International |
| MeSH Terms | Description | Related Terms |
|---|---|---|
| Tuberculosis | Any of the infectious diseases of humans and other animals caused by species of Mycobacterium tuberculosis | Tuberculoses Kochs Disease Koch’s Disease Koch Disease Mycobacterium tuberculosis Infection Infection, Mycobacterium tuberculosis Infections, Mycobacterium tuberculosis Mycobacterium tuberculosis Infections |
| Air microbiology | The presence of bacteria, viruses, and fungi in the air. This term is not restricted to pathogenic organisms. | Microbiology, Air |
| Occupational health | The promotion and maintenance of physical and mental health in the work environment. | Health, Occupational Industrial Hygiene Hygiene, Industrial Industrial Health Health, Industrial Safety, Occupational Occupational Safety Employee Health Health, Employee |
| Questions | Response | International | National | |||
|---|---|---|---|---|---|---|
| Reference Center | Local | Regional | Reference Center | Research Center | ||
| Is there sufficient PPE to carry out the work? | Yes | 0% | 9.1% | 0% | 0% | 0% |
| No | 100% | 90.9% | 100% | 100% | 100% | |
| Are there enough safety and preventative measures? | Yes | 85.7% | 100% | 0% | 71.4% | 0% |
| No | 14.3% | 0% | 100% | 28.6% | 100% | |
| Question | Answer | International | National | |||
|---|---|---|---|---|---|---|
| Reference Center | Local | Regional | Reference Center | Research Center | ||
| Do you go outside in your work clothes? | Yes | 0% | 9.1% | 0% | 0% | 0% |
| No | 100% | 90.9% | 100% | 100% | 100% | |
| Do you smoke or eat close to your working area? | Yes | 0% | 0% | 0% | 0% | 0% |
| No | 100% | 90.9% | 100% | 100% | 100% | |
| Do you clean your workspace following protocol? | Yes | 100% | 100% | 100% | 100% | 100% |
| No | 0% | 0% | 0% | 0% | 0% | |
| Do you decontaminate following protocol? | Yes | 100% | 54.5% | 100% | 57.1% | 100% |
| No | 0% | 45.5% | 0% | 42.9% | 0% | |
| Do you wash your hands according to protocol? | Yes | 100% | 54.5% | 100% | 28.6% | 100% |
| No | 0% | 45.5% | 0% | 71.4% | 0% | |
| Title | Year | Country | Sample | Work environment | Variables | Results | Source | Citations |
|---|---|---|---|---|---|---|---|---|
| Are healthcare workers in England and Wales at an increased risk of tuberculosis? [39] | 1993 | United Kingdom | Healthcare workers (N = 119) | National Health System | Sex, ethnicity, association with other workers | Crude notification rate among healthcare workers was 11.8 per 100,000 per year | British Medical Journal (BMJ) | 63 |
| Challenges with QuantiFERON-TB Gold Assay for Large-Scale, Routine Screening of U.S. Healthcare Workers [40] | 2008–2010 | United States | Serial testing results of healthcare workers (N = 9153) | National Health System | QuantiFERON-TB Gold In-Tube test, age, sex, QFT results, including the T.B. Antigen, Nil, and Mitogen; and the test run date. | Remaining false positive (p < 0.001) | American Journal of Respiratory and Critical Care Medicine | 61 |
| Evaluation of Interferon-Gamma Release Assays in the Diagnosis of Recent Tuberculosis Infection in Healthcare Workers [41] | 2004–2005 | Spain | Testing of healthcare workers (N = 147) | National Health System (West) | QuantiFERON-TB GOLD In-Tube and T-SPOT. T.B. in H.C.W.s, comparing the results with a tuberculin skin test (T.S.T.) | A low frequency of B.G.G. vaccination (15.6%); the occupational degree exposure was significant when the outcome was a positive T-SPOT. T.B. result (OR = 2.03) | Plos One | 30 |
| Tuberculosis Risk Among Staff of a Large Public Hospital in Kenya [42] | 2003–2005 | Kenya | Healthcare workers (N = 4833) | National Health System | Sex, job designation, years working, household, and guidelines | The time with the patient was liked to tuberculosis (OR = 1.3) Working role (p = 0.07) | International Union Against Tuberculosis and Lung Disease | 24 |
| High incidence of latent tuberculous infection among South African health workers: An urgent call for action [43] | 2008 | Kenya | Healthcare workers (N = 199) | National Health System | Sociodemographic details, knowledge and risk perceptions of T.B. and L.T.B.I., and training and practice in infection control, I.G.R.A. compared with tuberculin skin test (T.S.T.) | Knowledge and infection control training and practice were associated with a 50–60% reduction in the risk of tuberculosis acquisition | International Union Against Tuberculosis and Lung Disease | 23 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vaquero-Álvarez, E.; Cubero-Atienza, A.; Ruiz-Martínez, P.; Vaquero-Abellán, M.; Redel-Macías, M.D.; Aparicio-Martínez, P. Tuberculosis and Other Airborne Microbes in Occupational Health and Safety. Int. J. Environ. Res. Public Health 2020, 17, 7088. https://doi.org/10.3390/ijerph17197088
Vaquero-Álvarez E, Cubero-Atienza A, Ruiz-Martínez P, Vaquero-Abellán M, Redel-Macías MD, Aparicio-Martínez P. Tuberculosis and Other Airborne Microbes in Occupational Health and Safety. International Journal of Environmental Research and Public Health. 2020; 17(19):7088. https://doi.org/10.3390/ijerph17197088
Chicago/Turabian StyleVaquero-Álvarez, Esther, Antonio Cubero-Atienza, Pilar Ruiz-Martínez, Manuel Vaquero-Abellán, María Dolores Redel-Macías, and Pilar Aparicio-Martínez. 2020. "Tuberculosis and Other Airborne Microbes in Occupational Health and Safety" International Journal of Environmental Research and Public Health 17, no. 19: 7088. https://doi.org/10.3390/ijerph17197088