Static Balance Modification during the Workday in Assembly Chain Workers with and without Current Low Back Pain
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Experimental Design and Procedure
2.3. Statistical Analysis
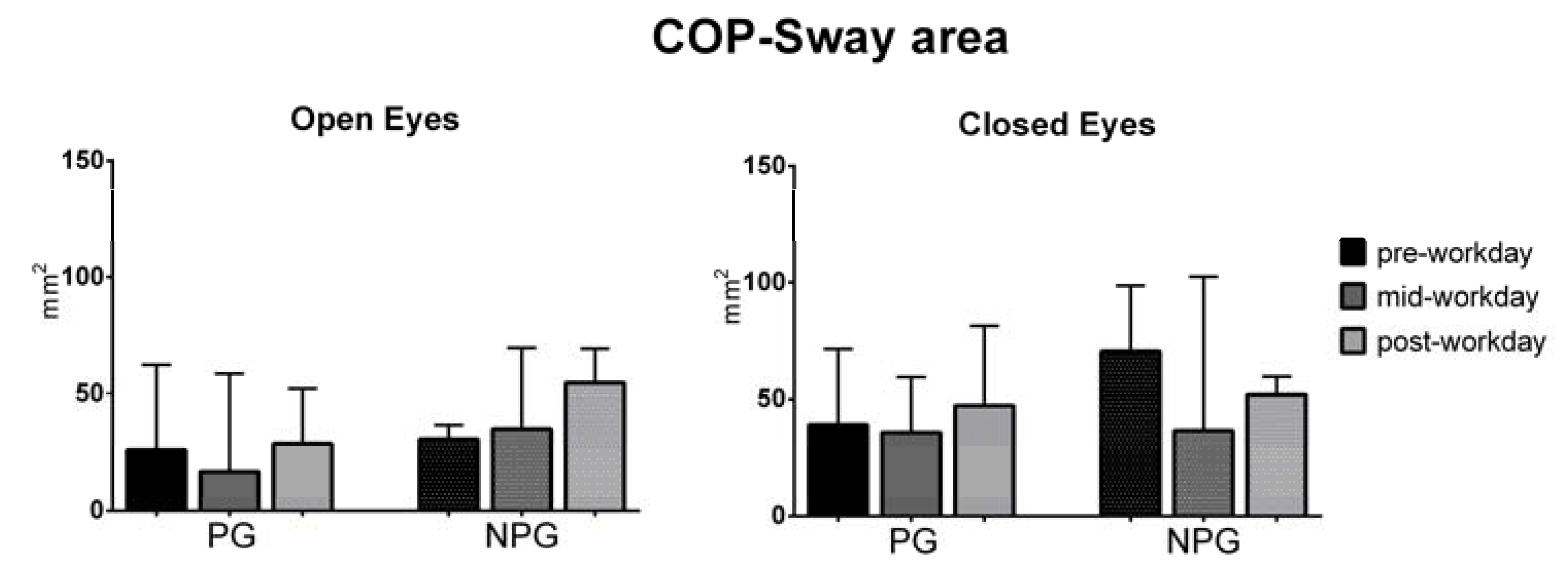
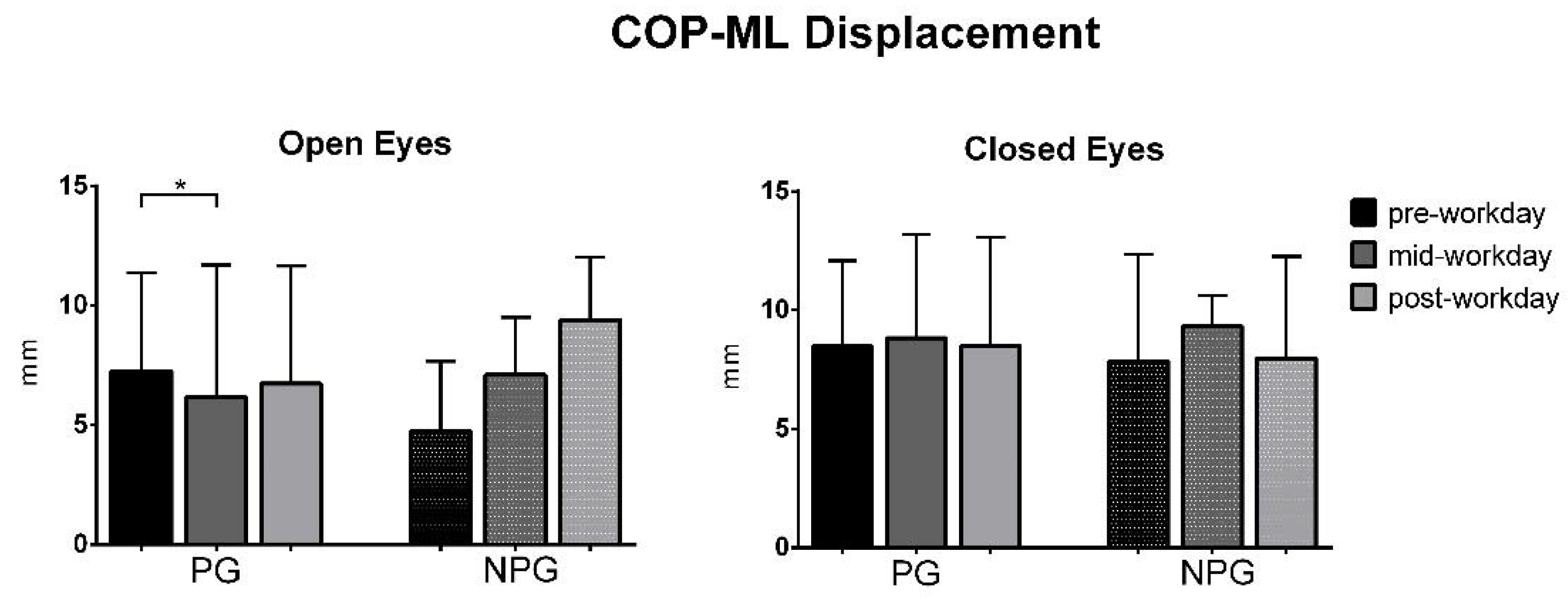
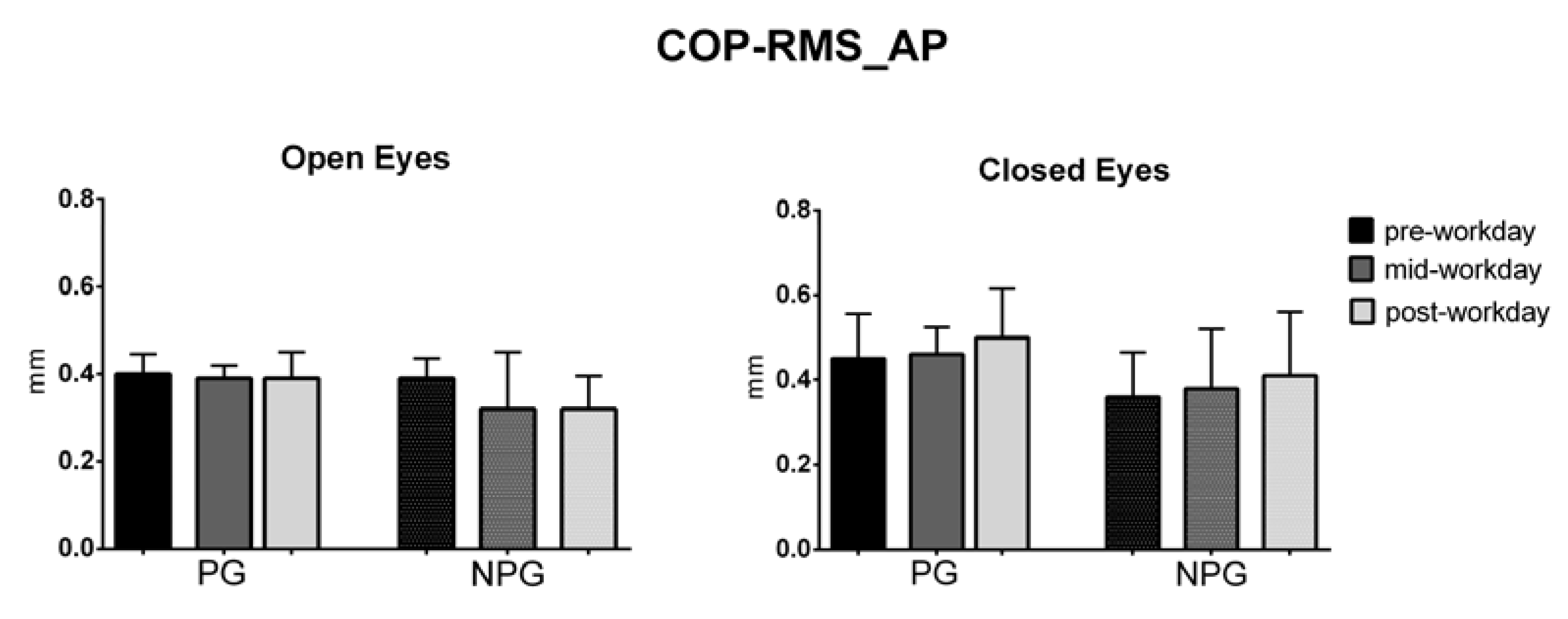
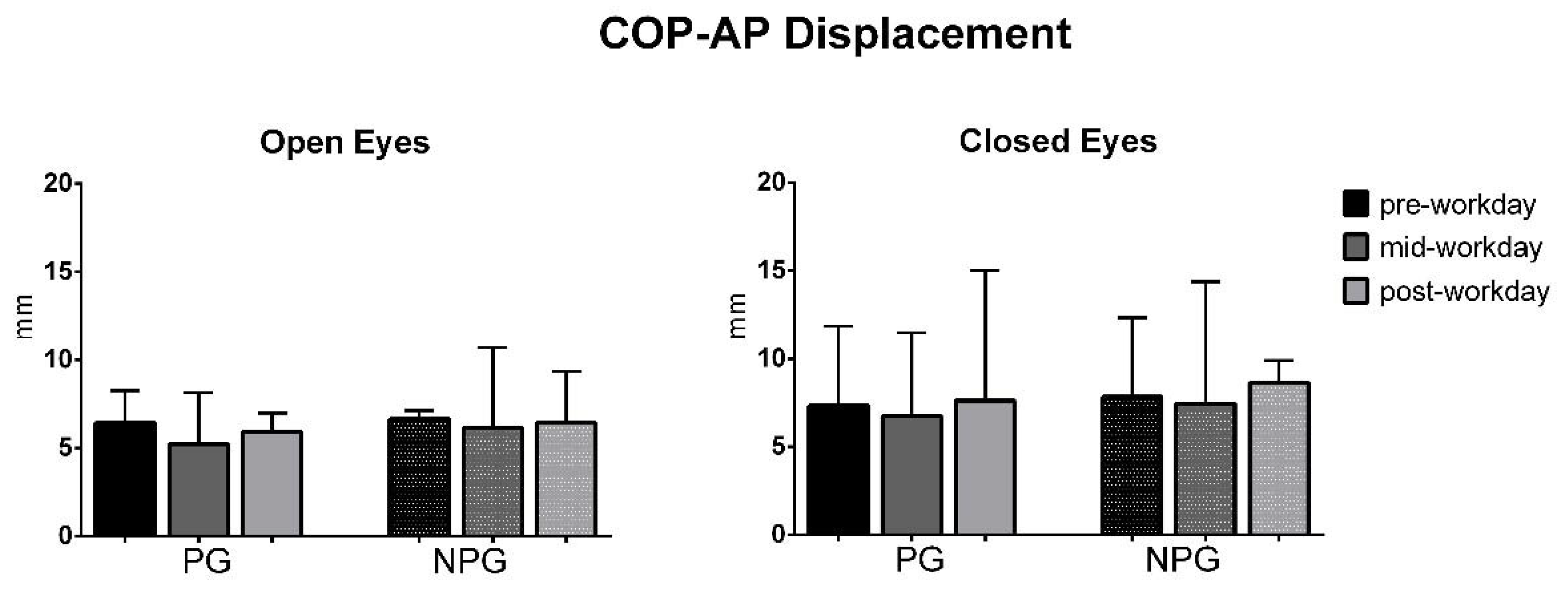
3. Results
Subjects
4. Discussion
4.1. Balance and Low Back Pain
4.2. Balance Evolution during Workday
4.3. Balance and Visual Feferences
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wynne-Jones, G.; Cowen, J.; Jordan, J.L.; Uthman, O.A.; Main, C.J.; Glozier, N.; Van Der Windt, D. Absence from work and return to work in people with back pain: A systematic review and meta-analysis. Occup. Environ. Med. 2013, 71, 448–456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bataller-Cervero, A.V.; Cimarras-Otal, C.; Sanz-López, F.; Lacárcel-Tejero, B.; Alcázar-Crevillén, A.; Ruete, J.A.V. Musculoskeletal disorders assessment using sick-leaves registers in a manufacturing plant in Spain. Int. J. Ind. Ergon. 2016, 56, 124–129. [Google Scholar] [CrossRef]
- Driscoll, T.; Jacklyn, G.; Orchard, J.; Passmore, E.; Vos, T.; Freedman, G.; Lim, S.; Punnett, L. The global burden of occupationally related low back pain: Estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 2014, 73, 975–981. [Google Scholar] [CrossRef] [PubMed]
- Sterud, T.; Tynes, T. Work-related psychosocial and mechanical risk factors for low back pain: A 3-year follow-up study of the general working population in Norway. Occup. Environ. Med. 2013, 70, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Locks, F.; Gupta, N.; Hallman, D.; Jørgensen, M.B.; Oliveira, A.B.; Holtermann, A. Association between objectively measured static standing and low back pain—A cross-sectional study among blue-collar workers. Ergonomics 2018, 61, 1196–1207. [Google Scholar] [CrossRef]
- Gregory, D.E.; Callaghan, J.P. Prolonged standing as a precursor for the development of low back discomfort: An investigation of possible mechanisms. Gait Posture 2008, 28, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Ghasemkhani, M.; Mahmudi, E.; Jabbari, H. Musculoskeletal Symptoms in Workers. Int. J. Occup. Saf. Ergon. 2008, 14, 455–462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menegon, F.A.; Fischer, F.M. Musculoskeletal reported symptoms among aircraft assembly workers: A multifactorial approach. Work 2012, 41 (Suppl. 1), 3738–3745. [Google Scholar] [CrossRef] [Green Version]
- Tousignant, M.; Rossignol, M.; Goulet, L.; Dassa, C. Occupational disability related to back pain: Application of a theoretical model of work disability using prospective cohorts of manual workers. Am. J. Ind. Med. 2000, 37, 410–422. [Google Scholar] [CrossRef]
- Alexopoulos, E.C.; Stathi, I.-C.; Charizani, F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskelet. Disord. 2004, 5, 16. [Google Scholar] [CrossRef] [Green Version]
- Josephson, M.; Lagerström, M.; Hagberg, M.; Hjelm, E.W. Musculoskeletal symptoms and job strain among nursing personnel: A study over a three year period. Occup. Environ. Med. 1997, 54, 681–685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sadeghian, F.; Kasaeian, A.; Noroozi, P.; Vatani, J.; Taiebi, S.H. Psychosocial and Individual Characteristics and Musculoskeletal Complaints among Clinical Laboratory Workers. Int. J. Occup. Saf. Ergon. 2014, 20, 355–361. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagasu, M.; Sakai, K.; Ito, A.; Tomita, S.; Temmyo, Y.; Ueno, M.; Miyagi, S. Prevalence and risk factors for low back pain among professional cooks working in school lunch services. BMC Public Health 2007, 7, 171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Della Volpe, R.; Popa, T.; Ginanneschi, F.; Spidalieri, R.; Mazzocchio, R.; Rossi, A. Changes in coordination of postural control during dynamic stance in chronic low back pain patients. Gait Posture 2006, 24, 349–355. [Google Scholar] [CrossRef]
- Mientjes, M.; Frank, J.S. Balance in chronic low back pain patients compared to healthy people under various conditions in upright standing. Clin. Biomech. 1999, 14, 710–716. [Google Scholar] [CrossRef]
- Ruhe, A.; Fejer, R.; Walker, B.F. Is there a relationship between pain intensity and postural sway in patients with non-specific low back pain? BMC Musculoskelet. Disord. 2011, 12, 162. [Google Scholar] [CrossRef] [Green Version]
- Da Silva, R.A.; Vieira, E.R.; Fernandes, K.B.P.; Andraus, R.A.; Oliveira, M.R.; Sturion, L.A.; Calderon, M.G. People with chronic low back pain have poorer balance than controls in challenging tasks. Disabil. Rehabil. 2017, 40, 1294–1300. [Google Scholar] [CrossRef]
- Ruhe, A.; Fejer, R.; Walker, B. Center of pressure excursion as a measure of balance performance in patients with non-specific low back pain compared to healthy controls: A systematic review of the literature. Eur. Spine J. 2010, 20, 358–368. [Google Scholar] [CrossRef] [Green Version]
- Brumagne, S.; Cordo, P.; Lysens, R.; Verschueren, S.; Swinnen, S. The Role of Paraspinal Muscle Spindles in Lumbosacral Position Sense in Individuals with and Without Low Back Pain. Spine 2000, 25, 989–994. [Google Scholar] [CrossRef]
- Rossi, A.; Decchi, B.; Ginanneschi, F. Presynaptic excitability changes of group Ia fibres to muscle nociceptive stimulation in humans. Brain Res. 1999, 818, 12–22. [Google Scholar] [CrossRef]
- Baratto, L.; Morasso, P.G.; Re, C.; Spada, G. A new look at posturographic analysis in the clinical context: Sway-density versus other parameterization techniques. Mot. Control 2002, 6, 246–270. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W. Changes in motor planning of feedforward postural responses of the trunk muscles in low back pain. Exp. Brain Res. 2001, 141, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Alexander, K.M.; LaPier, T.L.K. Differences in Static Balance and Weight Distribution between Normal Subjects and Subjects with Chronic Unilateral Low Back Pain. J. Orthop. Sports Phys. Ther. 1998, 28, 378–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tjernström, F.; Björklund, M.; Malmström, E.-M. Romberg ratio in quiet stance posturography—Test to retest reliability. Gait Posture 2015, 42, 27–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choy, N.L.; Brauer, S.G.; Nitz, J. Changes in postural stability in women aged 20 to 80 years. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2003, 58, M525–M530. [Google Scholar] [CrossRef] [Green Version]
- Vereeck, L.; Wuyts, F.; Truijen, S.; Van De Heyning, P. Clinical assessment of balance: Normative data, and gender and age effects. Int. J. Audiol. 2008, 47, 67–75. [Google Scholar] [CrossRef]
- World Medical Association General Assembly. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects Revised October 7, 2000. HIV Clin. Trials 2001, 2, 92–95. [Google Scholar] [CrossRef]
- Hjermstad, M.J.; Fayers, P.M.; Haugen, D.F.; Caraceni, A.; Hanks, G.W.; Loge, J.H.; Fainsinger, R.; Aass, N.; Kaasa, S. Studies Comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for Assessment of Pain Intensity in Adults: A Systematic Literature Review. J. Pain Symptom Manag. 2011, 41, 1073–1093. [Google Scholar] [CrossRef]
- Romero-Franco, N.; Martínez-Amat, A.; Hita-Contreras, F.; Martínez-López, E.J. Short-term Effects of a Proprioceptive Training Session with Unstable Platforms on the Monopodal Stabilometry of Athletes. J. Phys. Ther. Sci. 2014, 26, 45–51. [Google Scholar] [CrossRef] [Green Version]
- Krewer, C.; Bergmann, J.; Gräfrath, P.C.; Jahn, K. Influence of foot position on static and dynamic standing balance in healthy young adults. Hear. Balance Commun. 2018, 16, 208–214. [Google Scholar] [CrossRef]
- Paillard, T.; Noe, F. Techniques and Methods for Testing the Postural Function in Healthy and Pathological Subjects. BioMed Res. Int. 2015, 2015, 891390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruhe, A.; Fejer, R.; Walker, B.F. The test–retest reliability of centre of pressure measures in bipedal static task conditions—A systematic review of the literature. Gait Posture 2010, 32, 436–445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive Statistics for Studies in Sports Medicine and Exercise Science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mann, L.; Kleinpaul, J.F.; Moro, A.R.P.; Mota, C.B.; Carpes, F.P. Effect of low back pain on postural stability in younger women: Influence of visual deprivation. J. Bodyw. Mov. Ther. 2010, 14, 361–366. [Google Scholar] [CrossRef]
- Nies, N.; Sinnott, P.L. Variations in balance and body sway in middle-aged adults. Subjects with healthy backs compared with subjects with low-back dysfunction. Spine 1991, 16, 325–330. [Google Scholar]
- Harringe, M.; Halvorsen, K.; Renström, P.; Werner, S. Postural control measured as the center of pressure excursion in young female gymnasts with low back pain or lower extremity injury. Gait Posture 2008, 28, 38–45. [Google Scholar] [CrossRef] [Green Version]
- Luoto, S.; Taimela, S.; Hurri, H.; Aalto, H.; Pyykko, I.; Alaranta, H. Psychomotor speed and postural control in chronic low back pain patients: A controlled follow-up study. Spine 1996, 21, 2621–2627. [Google Scholar] [CrossRef]
- Mok, N.W.; Brauer, S.G.; Hodges, P.W. Hip Strategy for Balance Control in Quiet Standing Is Reduced in People with Low Back Pain. Spine 2004, 29, E107–E112. [Google Scholar] [CrossRef]
- Salavati, M.; Mazaheri, M.; Negahban, H.; Ebrahimi, I.; Jafari, A.H.; Kazemnejad, A.; Parnianpour, M. Effect of Dual-Tasking on Postural Control in Subjects With Nonspecific Low Back Pain. Spine 2009, 34, 1415–1421. [Google Scholar] [CrossRef]
- Van Emmerik, R.; Van Wegen, E.E. On the Functional Aspects of Variability in Postural Control. Exerc. Sport Sci. Rev. 2002, 30, 177–183. [Google Scholar] [CrossRef]
- Lafond, D.; Champagne, A.; Descarreaux, M.; Dubois, J.-D.; Prado, J.M.; Duarte, M. Postural control during prolonged standing in persons with chronic low back pain. Gait Posture 2009, 29, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, K.M.; Nelson-Wong, E.; Callaghan, J.P. Do individuals who develop transient low back pain exhibit different postural changes than non-pain developers during prolonged standing? Gait Posture 2011, 34, 490–495. [Google Scholar] [CrossRef] [PubMed]
- Pau, M.; Kim, S.; Nussbaum, M.A. Fatigue-induced balance alterations in a group of Italian career and retained firefighters. Int. J. Ind. Ergon. 2014, 44, 615–620. [Google Scholar] [CrossRef]
- Derave, W.; Tombeux, N.; Cottyn, J.; Pannier, J.L.; De Clercq, D. Treadmill Exercise Negatively Affects Visual Contribution to Static Postural Stability. Int. J. Sports Med. 2002, 23, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Corbeil, P.; Blouin, J.-S.; Bégin, F.; Nougier, V.; Teasdale, N. Perturbation of the postural control system induced by muscular fatigue. Gait Posture 2003, 18, 92–100. [Google Scholar] [CrossRef]
- Brumagne, S.; Janssens, L.; Janssens, E.; Goddyn, L. Altered postural control in anticipation of postural instability in persons with recurrent low back pain. Gait Posture 2008, 28, 657–662. [Google Scholar] [CrossRef]
- Yahia, A.; Jribi, S.; Ghroubi, S.; Baklouti, S.; Elleuch, M.H. Evaluation of the posture and muscular strength of the trunk and inferior members of patients with chronic lumbar pain. Jt. Bone Spine 2011, 78, 291–297. [Google Scholar] [CrossRef] [PubMed]



| Total (n = 22) | NPG (n = 5) | PG (n = 17) | p-Value | |
|---|---|---|---|---|
| Age (years) | 43 ± 7 | 48 ± 10 | 43 ± 5 | 0.145 |
| Height (cm) | 175.2 ± 8.9 | 169.2 ± 7.3 | 176.6 ± 8.7 | 0.138 |
| Weight (kg) | 80.8 ± 12.2 | 76.2 ± 14.5 | 81.9 ± 11.8 | 0.417 |
| BMI (kg/m2) | 26.3 ± 4.0 | 27.03 ± 7.3 | 26.23 ± 2.9 | 0.844 |
| Current LBP | 2.8 ± 1.8 | 0 ± 0 | 3.7 ± 0.9 | 0.002 * |
| Group | NPG (n = 5) | PG (n = 17) | p-Value | ES |
|---|---|---|---|---|
| AP_OE(mm) | 6.03 ± 1.75 | 6.77 ± 2.80 | 0.587 | 0.31 |
| ML_OE (mm) | 5.53 ± 1.58 | 9.20 ± 5.38 | 0.158 | 0.92 |
| Area_OE (mm2) | 26.40 ± 12.67 | 36.32 ± 26.29 | 0.431 | 0.48 |
| MV_OE (mm/s) | 5.22 ± 1.92 | 6.01 ± 2.02 | 0.449 | 0.40 |
| RMS-AP_OE (mm) | 0.38 ± 0.08 | 0.47 ± 0.15 | 0.200 | 0.74 |
| RMS-ML_OE (mm) | 0.35 ± 0.09 | 0.39 ± 0.12 | 0.520 | 0.37 |
| AP_CE(mm) | 9.76 ± 5.93 | 8.79 ± 4.00 | 0.674 | 0.19 |
| ML_CE (mm) | 8.88 ± 3.38 | 9.34 ± 3.55 | 0.799 | 0.13 |
| Area_CE (mm2) | 58.80 ± 46.62 | 51.93 ± 39.89 | 0.750 | 0.15 |
| MV_CE (mm/s) | 5.63 ±1.58 | 6.46 ± 1.75 | 0.357 | 0.49 |
| RMS-AP_CE (mm) | 0.53 ± 0.13 | 0.52 ± 0.11 | 0.963 | 0.08 |
| RMS-ML_CE (mm) | 0.39 ± 0.07 | 0.48 ± 0.19 | 0.300 | 0.62 |
| Romberg | 0.89 ± 0.12 | 0.87 ± 0.14 | 0.719 | 0.49 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bataller-Cervero, A.V.; Cimarras-Otal, C.; Roche-Seruendo, L.E.; Alcázar-Crevillén, A.; Villalba-Ruete, J.A.; Berzosa, C. Static Balance Modification during the Workday in Assembly Chain Workers with and without Current Low Back Pain. Int. J. Environ. Res. Public Health 2020, 17, 7385. https://doi.org/10.3390/ijerph17207385
Bataller-Cervero AV, Cimarras-Otal C, Roche-Seruendo LE, Alcázar-Crevillén A, Villalba-Ruete JA, Berzosa C. Static Balance Modification during the Workday in Assembly Chain Workers with and without Current Low Back Pain. International Journal of Environmental Research and Public Health. 2020; 17(20):7385. https://doi.org/10.3390/ijerph17207385
Chicago/Turabian StyleBataller-Cervero, Ana Vanessa, Cristina Cimarras-Otal, Luis Enrique Roche-Seruendo, Andrés Alcázar-Crevillén, José Antonio Villalba-Ruete, and César Berzosa. 2020. "Static Balance Modification during the Workday in Assembly Chain Workers with and without Current Low Back Pain" International Journal of Environmental Research and Public Health 17, no. 20: 7385. https://doi.org/10.3390/ijerph17207385
APA StyleBataller-Cervero, A. V., Cimarras-Otal, C., Roche-Seruendo, L. E., Alcázar-Crevillén, A., Villalba-Ruete, J. A., & Berzosa, C. (2020). Static Balance Modification during the Workday in Assembly Chain Workers with and without Current Low Back Pain. International Journal of Environmental Research and Public Health, 17(20), 7385. https://doi.org/10.3390/ijerph17207385









