Is Consultation-Liaison Psychiatry ‘Getting Old’? How Psychiatry Referrals in the General Hospital Have Changed over 20 Years
Abstract
1. Introduction
2. Methodology
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Smith, G.C. From Consultation–Liaison Psychiatry to Integrated Care for Multiple and Complex Needs. Aust. N. Z. J. Psychiatry 2009, 43, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, S.; Blum, J.; Kelly, P. How to collaborate with other specialities. In How to Succeed in Psychiatry: A Guide to Training and Practice; Fiorillo, A., Calliess, I.T., Sass, H., Eds.; J. Wiley & Sons: Chichester, West Sussex, UK, 2012; pp. 211–235. ISBN 978-1-119-99866-2. [Google Scholar]
- Ferrari, S.; Dreher, A.; Mattei, G.; Diefenbacher, A. Liaison psychiatry—Is it possible? In Psychiatry in Practice; Fiorillo, A., Volpe, U., Bhugra, D., Eds.; Oxford University Press: Oxford, UK, 2016; pp. 389–408. ISBN 978-0-19-872364-6. [Google Scholar]
- Engel, G. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Meller, W.; Specker, S.; Schultz, P.; Kishi, Y.; Thurber, S.; Kathol, R. Using the INTERMED complexity instrument for a retrospective analysis of patients presenting with medical illness, substance use disorder, and other psychiatric illnesses. Ann. Clin. Psychiatry 2015, 27, 38–43. [Google Scholar]
- de Jonge, P.; Huyse, F.J.; Slaets, J.P.J.; Söllner, W.; Stiefel, F.C. Operationalization of Biopsychosocial Case Complexity in General Health Care: The INTERMED Project. Aust. N. Z. J. Psychiatry 2005, 39, 795–799. [Google Scholar] [CrossRef]
- Oldham, M.A.; Chahal, K.; Lee, H.B. A systematic review of proactive psychiatric consultation on hospital length of stay. Gen. Hosp. Psychiatry 2019, 60, 120–126. [Google Scholar] [CrossRef]
- Kishi, Y.; Meller, W.H.; Kathol, R.G.; Swigart, S.E. Factors Affecting the Relationship between the Timing of Psychiatric Consultation and General Hospital Length of Stay. Psychosomatics 2004, 45, 470–476. [Google Scholar] [CrossRef]
- Udo, I.; Odeyale, F.; Gash, A.; Fossey, M. The rise of liaison psychiatry: Challenges and implications for sustainability. Br. J. Hosp. Med. 2016, 77, 523–528. [Google Scholar] [CrossRef]
- Yrondi, A.; Petiot, D.; Arbus, C.; Schmitt, L. Economic impact of consultation-liaison psychiatry in a French University Hospital Centre. Encephale 2016, 42, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, V.; Lagarto, L.; Cerejeira, J.; Renca, S.; Firmino, H. Improving quality of care: Focus on liaison old age psychiatry. Ment. Health Fam. Med. 2013, 10, 153–158. [Google Scholar]
- National Center for Health Statistics. Percent Distribution, Rate, Days of Care with Average Length of Stay, and Standard Error of Discharges from Short-Stay Hospitals, by Sex and Age 2010; National Center for Health Statistics: Hyattsville, MD, USA.
- Anderson, D.; Nortcliffe, M.; Dechenne, S.; Wilson, K. The rising demand for consultation-liaison psychiatry for older people: Comparisons within Liverpool and the literature across time. Int. J. Geriatr. Psychiatry 2011, 26, 1231–1235. [Google Scholar] [CrossRef]
- Ferrari, S.; Signorelli, M.S.; Cerrato, F.; Pingani, L.; Massimino, M.; Valente, S.; Forlani, M.; Bonasegla, P.; Arcidiacono, E.; De Ronchi, D.; et al. Never too late to be anxious: Validation of the geriatric anxiety inventory, Italian version. Clin. Ter. 2017, 168, 120–127. [Google Scholar] [CrossRef]
- Schellhorn, S.E.; Barnhill, J.W.; Raiteri, V.; Faso, V.L.; Ferrando, S.J. A comparison of psychiatric consultation between geriatric and non-geriatric medical inpatients. Int. J. Geriatr. Psychiatry 2009, 24, 1054–1061. [Google Scholar] [CrossRef] [PubMed]
- Wild, B.; Heider, D.; Maatouk, I.; Slaets, J.; König, H.-H.; Niehoff, D.; Saum, K.-U.; Brenner, H.; Söllner, W.; Herzog, W. Significance and costs of complex biopsychosocial health care needs in elderly people: Results of a population-based study. Psychosom. Med. 2014, 76, 497–502. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (Ed.) Global Age-Friendly Cities: A Guide; World Health Organization: Geneva, Switzerland, 2007; ISBN 978-92-4-154730-7. [Google Scholar]
- Stiefel, F.C.; Huyse, F.J.; Söllner, W.; Slaets, J.P.J.; Lyons, J.S.; Latour, C.H.M.; van der Wal, N.; de Jonge, P. Operationalizing Integrated Care on a Clinical Level: The INTERMED Project. Med. Clin. N. Am. 2006, 90, 713–758. [Google Scholar] [CrossRef]
- Wild, B.; Herzog, W.; Schellberg, D.; Böhlen, F.; Brenner, H.; Saum, K.; Maatouk, I. A short intervention targeting psychosomatic care in older adults with complex health care needs—Results of a randomized controlled trial. Int. J. Geriatr. Psychiatry 2019, 34, 272–279. [Google Scholar] [CrossRef]
- Glass, O.M.; Hermida, A.P.; Hershenberg, R.; Schwartz, A.C. Considerations and Current Trends in the Management of the Geriatric Patient on a Consultation–Liaison Service. Curr. Psychiatry Rep. 2020, 22, 21. [Google Scholar] [CrossRef]
- Smith, G.C. From Consultation—Liaison Psychiatry to Psychosocial Advocacy: Maintaining Psychiatry’s Scope. Aust. N. Z. J. Psychiatry 1998, 32, 753–761. [Google Scholar] [CrossRef]
- Wild, B.; Heider, D.; Schellberg, D.; Böhlen, F.; Schöttker, B.; Muhlack, D.C.; König, H.-H.; Slaets, J. Caring for the elderly: A person-centered segmentation approach for exploring the association between health care needs, mental health care use, and costs in Germany. PLoS ONE 2019, 14, e0226510. [Google Scholar] [CrossRef]
- Pingani, L.; Fiorillo, A.; Luciano, M.; Catellani, S.; Vinci, V.; Ferrari, S.; Rigatelli, M. Who cares for it? How to provide psychosocial interventions in the community. Int. J. Soc. Psychiatry 2013, 59, 701–705. [Google Scholar] [CrossRef]
- Rigatelli, M.; Ferrari, S. The Modena Consultation–Liaison Psychiatry Service, Italy. Br. J. Psychiatry 2004, 184, 268–269. [Google Scholar] [CrossRef]
- Huyse, F.J.; Herzog, T.; Lobo, A.; Malt, U.F.; Opmeer, B.C.; Stein, B.; Creed, F.; Crespo, M.D.; Gardoso, G.; Guimaraes-Lopes, R.; et al. European Consultation-LiaisonPsychiatric Services:the ECLW Collaborative Study. Acta Psychiatr. Scand. 2000, 101, 360–366. [Google Scholar] [CrossRef] [PubMed]
- Huyse, F.J.; Herzog, T.; Lobo, A.; Malt, U.F.; Opmeer, B.C.; Stein, B.; de Jonge, P.; van Dijck, R.; Creed, F.; Crespo, M.D.; et al. Consultation-Liaison psychiatric service delivery: Results from a European study. Gen. Hosp. Psychiatry 2001, 23, 124–132. [Google Scholar] [CrossRef]
- Gala, C.; Rigatelli, M.; De Bertolini, C.; Rupolo, G.; Gabrielli, F.; Grassi, L. A multicenter investigation of consultation-liaison psychiatry in Italy. Gen. Hosp. Psychiatry 1999, 21, 310–317. [Google Scholar] [CrossRef]
- De Giorgio, G.; Quartesan, R.; Sciarma, T.; Giulietti, M.; Piazzoli, A.; Scarponi, L.; Ferrari, S.; Ferranti, L.; Moretti, P.; Piselli, M. Consultation-Liaison Psychiatry—From theory to clinical practice: An observational study in a general hospital. BMC Res. Notes 2015, 8, 475. [Google Scholar] [CrossRef]
- Kastenschmidt, E.K.; Kennedy, G.J. Depression and Anxiety in Late Life: Diagnostic Insights and Therapeutic Options. Mt. Sinai J. Med. 2011, 78, 527–545. [Google Scholar] [CrossRef]
- Alexopoulos, G.S.; Bruce, M.L.; Hull, J.; Sirey, J.A.; Kakuma, T. Clinical Determinants of Suicidal Ideation and Behavior in Geriatric Depression. Arch. Gen. Psychiatry 1999, 56, 1048. [Google Scholar] [CrossRef]
- Neviani, F.; Belvederi Murri, M.; Mussi, C.; Triolo, F.; Toni, G.; Simoncini, E.; Tripi, F.; Menchetti, M.; Ferrari, S.; Ceresini, G.; et al. Physical exercise for late life depression: Effects on cognition and disability. Int. Psychogeriatr. 2017, 29, 1105–1112. [Google Scholar] [CrossRef]
- Stanners, M.N.; Barton, C.A.; Shakib, S.; Winefield, H.R. Depression diagnosis and treatment amongst multimorbid patients: A thematic analysis. BMC Fam. Pract. 2014, 15, 124. [Google Scholar] [CrossRef]
- Olivieri, T.; Magistri, P.; Guidetti, C.; Baroni, S.; Rinaldi, S.; Assirati, G.; Catellani, B.; Chierego, G.; Cantaroni, C.; Bondi, F.; et al. University of Modena Experience with Liver Grafts From Donation after Circulatory Death: What Really Matters in Organ Selection? Transplant. Proc. 2019, 51, 2967–2970. [Google Scholar] [CrossRef]
- Rigatelli, M.; Ferrari, S.; Uguzzoni, U.; Natali, A. Teaching and Training in the Psychiatric-Psychosomatic Consultation-Liaison Setting. Psychother. Psychosom. 2000, 69, 221–228. [Google Scholar] [CrossRef]
- Ferrari, S.; Poloni, N.; Diefenbacher, A.; Barbosa, A.; Cosci, F. From hysteria to somatic symptom disorders: Searching for a common psychopathological ground. J. Psychopathol. 2015, 21, 372–379. [Google Scholar]
- Mattei, G.; Laghi, A.; Balduzzi, S.; Moscara, M.; Piemonte, C.; Reggianini, C.; Rigatelli, M.; Ferrari, S.; Pingani, L.; Galeazzi, G.M. Indicators of Complex Care During the Consultation-Liaison Psychiatry Activity at the Transplant Center of the Policlinico Hospital, Modena. Transpl. Proc. 2017, 49, 2105–2109. [Google Scholar] [CrossRef] [PubMed]
- Craig Nelson, J. Management of Late-Life Depression. In Antidepressants; Macaluso, M., Preskorn, S.H., Eds.; Handbook of Experimental Pharmacology; Springer International Publishing: Cham, Switzerland, 2018; Volume 250, pp. 389–413. ISBN 978-3-030-10948-6. [Google Scholar]










| Entire Population (N = 19278) | Not Over 65 Subpopulations (NOV65) | Over 65 Subpopulations (OV65) | Not Over 65 (NOV65) vs. Over 65 (OV65) Subpopulations during Years | Variation of Mean/Ratio during Years | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | DS | Mean | DS | Mean | DS | NOV65 | OV65 | ||
| Number of consultations | 963.90 | ±157.93 | 589.05 | ±108.06 | 374.65 | ±75.46 | t = 9.69; df = 19; p ˂ 0.001 | t = 24.38; df = 19; p ˂ 0.001 | t = 22.21; df = 19; p ˂ 0.001 |
| Age | 57.86 | ±18.09 | 45.93 | ±12.29 | 75.90 | ±7.25 | Not calculated | F = 15.59; df = 19; p ˂ 0.001 | F = 4.08; df = 19; p ˂ 0.001 |
| Mean waiting time from referral to assessment (days) | 1.52 | ±4.47 | 1.75 | ±5.09 | 1.17 | ±3.31 | t = 7.62; df = 14473; p ˂ 0.001 | F = 19.86; df = 16; p ˂ 0.001 | F = 12.47; df = 16; p ˂ 0.001 |
| N | % | N | % | N | % | ||||
| Sex | |||||||||
| Male | 8885 | 46.09% | 5394 | 45.78% | 3489 | 46.55% | Χ2 = 134.97; df = 19; p ˂ 0.001 | Χ2 = 84.11; df = 19; p ˂ 0.001 | Χ2 = 62.31; df = 19; p ˂ 0.001 |
| Female | 10,376 | 53.82% | 6373 | 54.08% | 4001 | 53.38% | |||
| Missing | 17 | 0.09% | 16 | 0.14% | 5 | 0.07% | |||
| Number of referrals according to ward | |||||||||
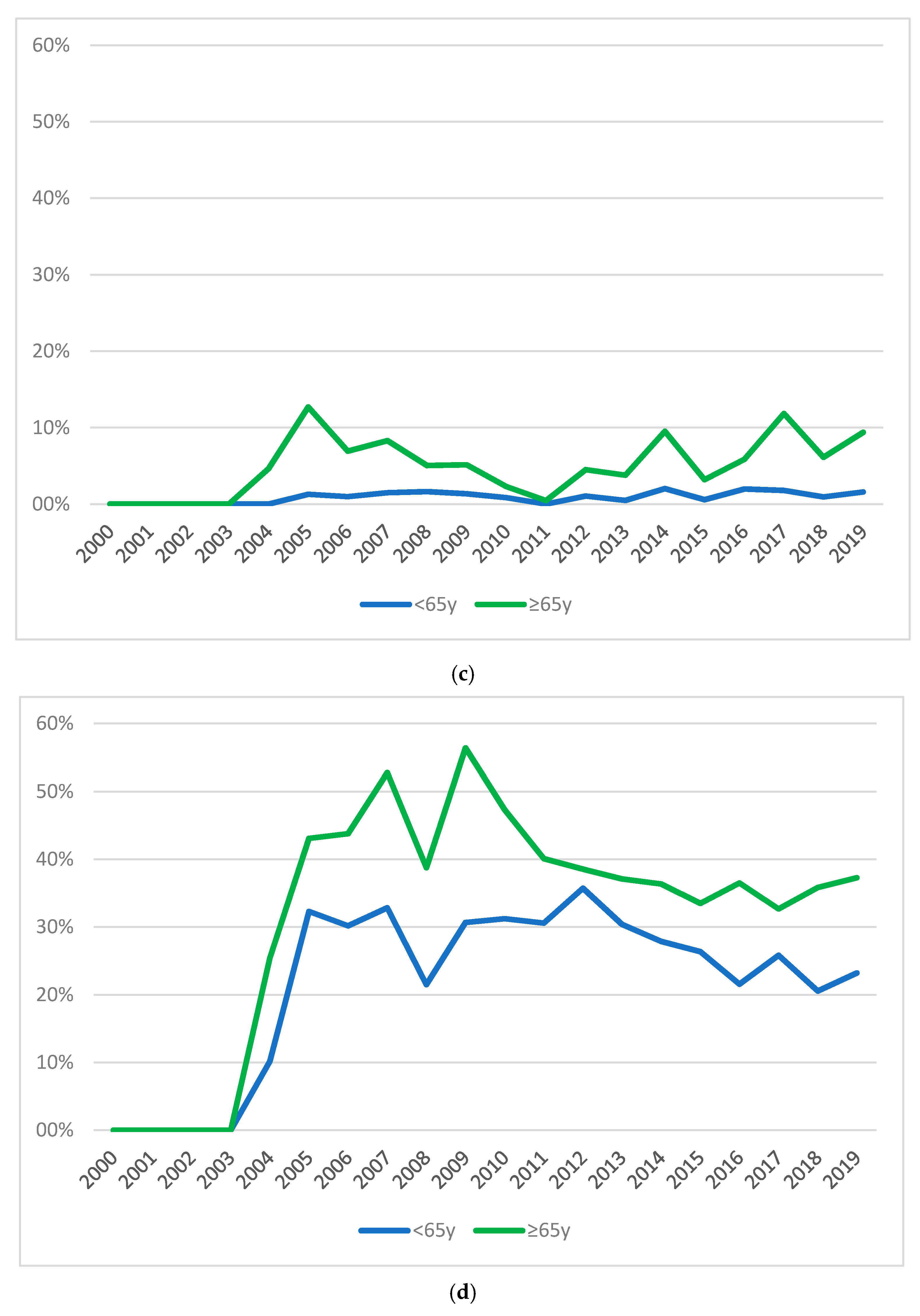
| Internal medicine | 6749 | 35.01% | 3411 | 28.95% | 3338 | 44.54% | Χ2 = 297.45; df = 19; p ˂ 0.001 | Not calculated | |
| Oncology | 1840 | 9.54% | 950 | 8.06% | 890 | 11.87% | Χ2 = 43.51; df = 16; p ˂ 0.001 | ||
| Gastroenterology | 1088 | 5.64% | 799 | 6.78% | 288 | 3.84% | Χ2 = 26.38; df = 17; p = 0.07 | ||
| Headache centre | 945 | 4.90% | 870 | 7.38% | 75 | 1.00% | Χ2 = 32.84; df = 19; p = 0.03 | ||
| Transplant surgery | 979 | 5.08% | 798 | 6.77% | 179 | 2.39% | Χ2 = 44.90; df = 11; p ˂ 0.001 | ||
| Surgery | 902 | 4.68% | 508 | 4.31% | 394 | 5.26% | Χ2 = 175.45; df = 19; p ˂ 0.001 | ||
| Nephrology-dialysis | 624 | 3.24% | 265 | 2.25% | 359 | 4.79% | Χ2 = 29.83; df = 19; p = 0.06 | ||
| Reason for referral | |||||||||
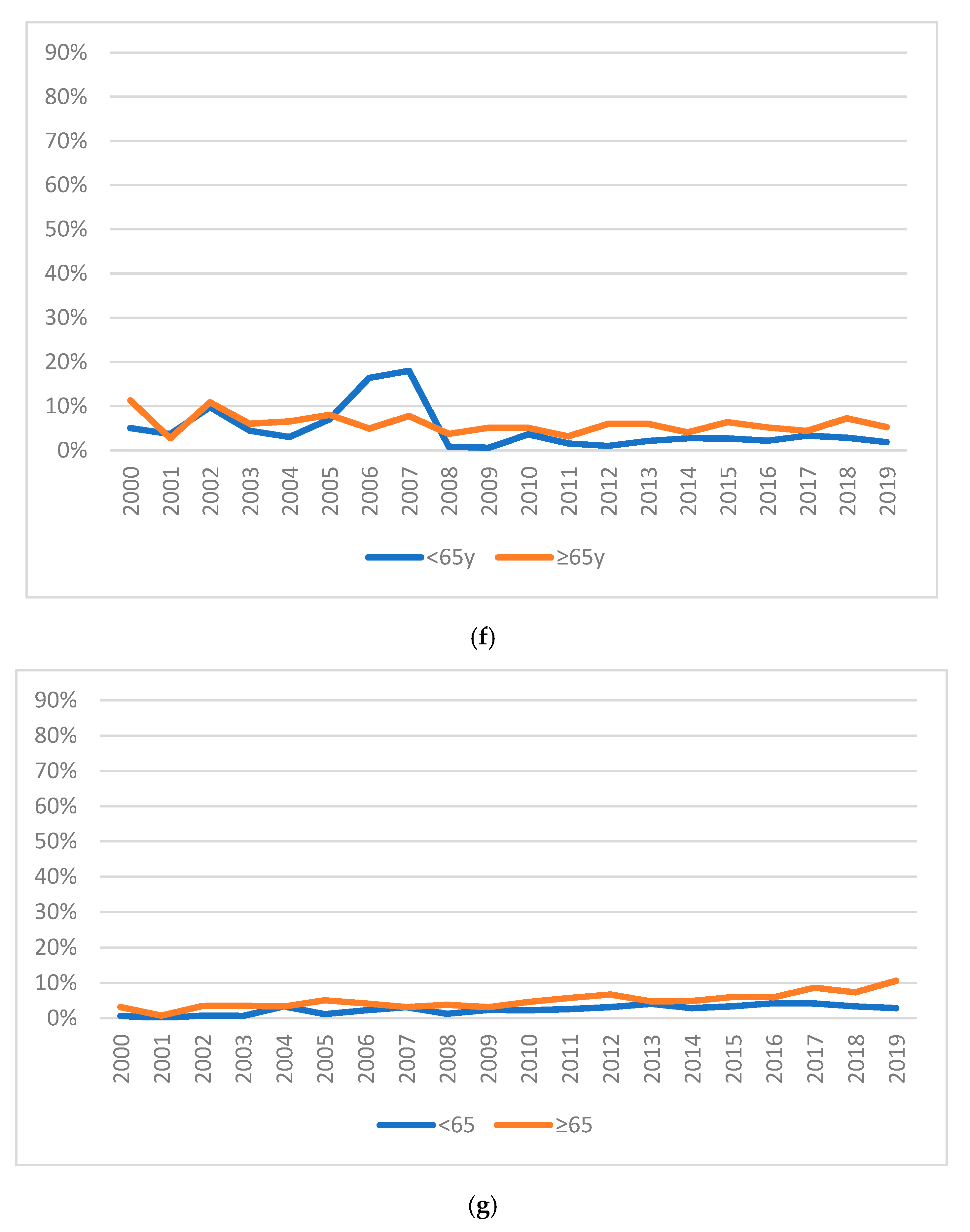
| Abuse of alcohol/drugs/psychotropic drugs | 665 | 3.45% | 587 | 4.48% | 78 | 1.04% | Χ2 = 25.50; df = 15; p = 0.04 | Not calculated | |
| Anxiety | 1414 | 7.33% | 981 | 8.33% | 432 | 5.76% | Χ2 = 23.76; df = 15; p = 0.07 | ||
| Delirium | 449 | 2.33% | 93 | 0.79% | 356 | 4.75% | Χ2 = 16.94; df = 15; p = 0.32 | ||
| Depression | 4591 | 23.81% | 2364 | 20.06% | 2227 | 29.71% | Χ2 = 45.66; df = 15; p ˂ 0.001 | ||
| Medical Unexplained Physical Symptoms | 1246 | 6.46% | 93 | 0.79% | 312 | 4.16% | Χ2 = 33.42; df = 19; p = 0.02 | ||
| Pre-OLTx | 1160 | 6.02% | 1043 | 8.85 | 116 | 1.55% | Χ2 = 53.82; df = 14; p ˂ 0.001 | ||
| Psychomotor agitation | 1581 | 8.02% | 512 | 4.35% | 1068 | 14.25% | Χ2 = 18.29; df = 15; p = 0.25 | ||
| Re-evaluation of psychopharmacological therapy | 831 | 4.31% | 481 | 4.08% | 350 | 4.67% | Χ2 = 26.80; df = 14; p = 0.02 | ||
| Number of urgent referrals | |||||||||
| Urgent | 4689 | 24.32% | 3070 | 26.05% | 1619 | 21.60% | Χ2 = 428.99; df = 19; p ˂ 0.001 | Χ2 = 248.38; df = 19; p ˂ 0.001 | |
| Not urgent | 12,210 | 63.34% | 7178 | 60.92% | 5032 | 67.14% | |||
| Missing information | 2379 | 12.34% | 1535 | 13.03% | 844 | 11.26% | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrari, S.; Mattei, G.; Marchi, M.; Galeazzi, G.M.; Pingani, L. Is Consultation-Liaison Psychiatry ‘Getting Old’? How Psychiatry Referrals in the General Hospital Have Changed over 20 Years. Int. J. Environ. Res. Public Health 2020, 17, 7389. https://doi.org/10.3390/ijerph17207389
Ferrari S, Mattei G, Marchi M, Galeazzi GM, Pingani L. Is Consultation-Liaison Psychiatry ‘Getting Old’? How Psychiatry Referrals in the General Hospital Have Changed over 20 Years. International Journal of Environmental Research and Public Health. 2020; 17(20):7389. https://doi.org/10.3390/ijerph17207389
Chicago/Turabian StyleFerrari, Silvia, Giorgio Mattei, Mattia Marchi, Gian Maria Galeazzi, and Luca Pingani. 2020. "Is Consultation-Liaison Psychiatry ‘Getting Old’? How Psychiatry Referrals in the General Hospital Have Changed over 20 Years" International Journal of Environmental Research and Public Health 17, no. 20: 7389. https://doi.org/10.3390/ijerph17207389
APA StyleFerrari, S., Mattei, G., Marchi, M., Galeazzi, G. M., & Pingani, L. (2020). Is Consultation-Liaison Psychiatry ‘Getting Old’? How Psychiatry Referrals in the General Hospital Have Changed over 20 Years. International Journal of Environmental Research and Public Health, 17(20), 7389. https://doi.org/10.3390/ijerph17207389







