Investigation of the Role of Anxiety and Depression on the Formation of Phantom Vibration and Ringing Syndrome Caused by Working Stress during Medical Internship
Abstract
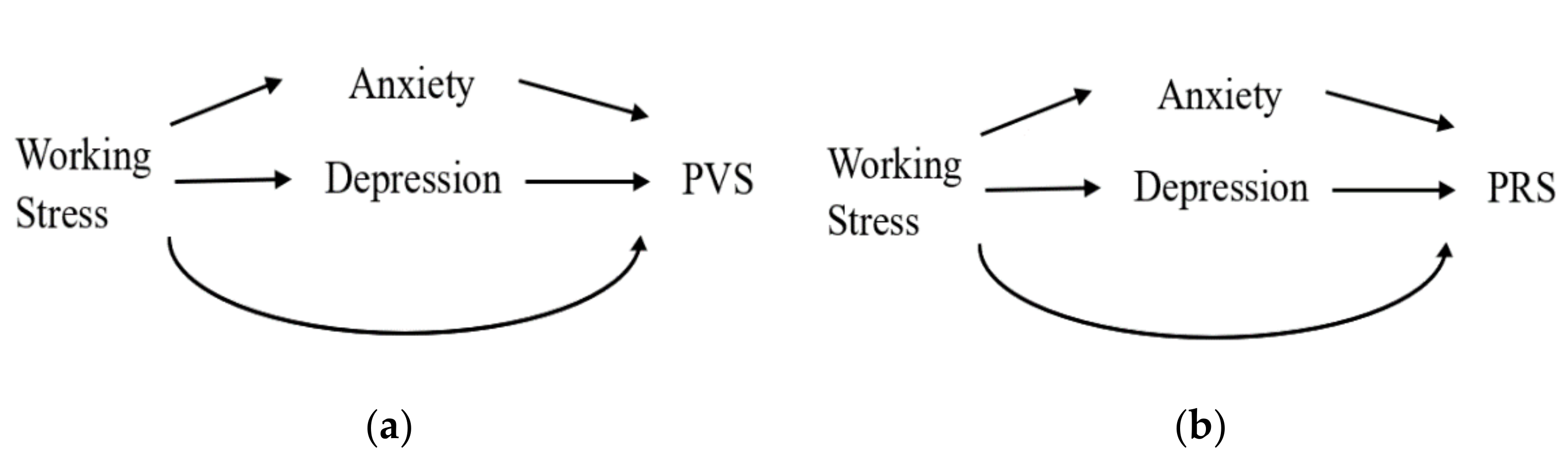
:1. Introduction
2. Methods
2.1. Participants
2.2. Measurements
2.2.1. Phantom Vibration and Ringing Questionnaire
2.2.2. The Beck Depression and Anxiety Inventories
2.3. Statistical Analysis
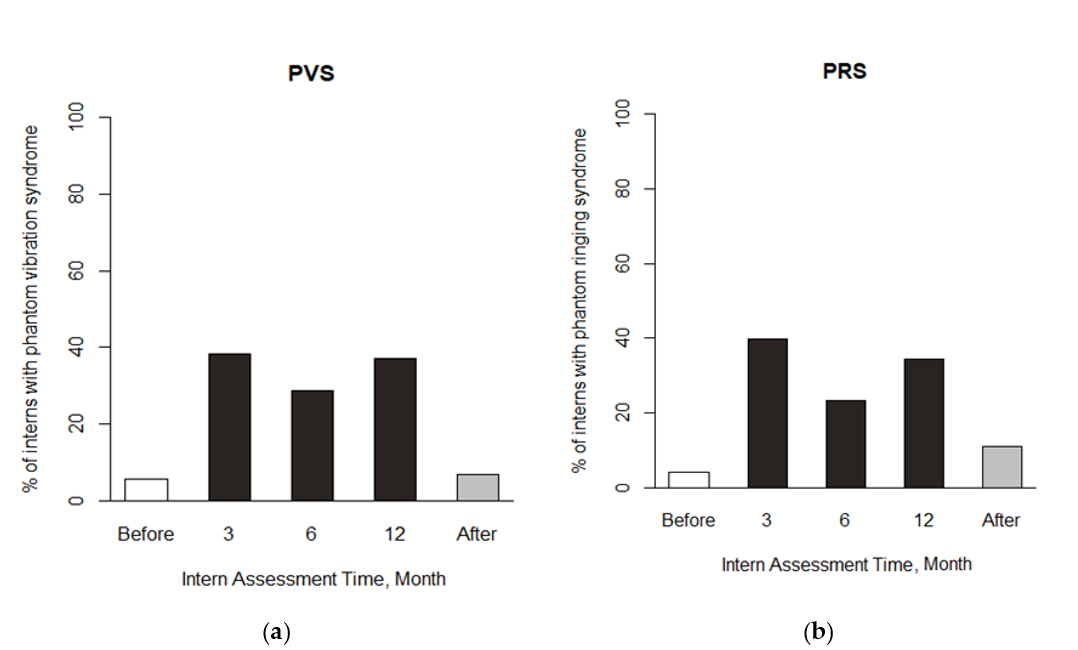
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| 1 | 2 | 3 | 4 | 5 | ||
|---|---|---|---|---|---|---|
| 1 | Working stress | - | 0.355 (0.257–0.453) | 0.262 (0.164–0.361) | 0.248 (0.156–0.339) | 0.215 (0.124–0.307) |
| 2 | Anxiety | - | 0.513 (0.425–0.601) | 0.171 (0.076–0.265) | 0.228 (0.135–0.321) | |
| 3 | Depression | - | 0.167 (0.065–0.268) | 0.205 (0.104–0.306) | ||
| 4 | Phantom vibration syndrome | - | 0.557 (0.452–0.663) | |||
| 5 | Phantom ringing syndrome | - |
References
- Lin, Y.H.; Lin, S.H.; Li, P.; Huang, W.L.; Chen, C.Y. Prevalent hallucinations during medical internships: Phantom vibration and ringing syndromes. PLoS ONE 2013, 8, e65152. [Google Scholar] [CrossRef]
- Lin, Y.H.; Chen, C.Y.; Li, P.; Lin, S.H. A dimensional approach to the phantom vibration and ringing syndrome during medical internship. J. Psychiatr. Res. 2013, 47, 1254–1258. [Google Scholar] [CrossRef]
- Mangot, A.G.; Murthy, V.S.; Kshirsagar, S.V.; Deshmukh, A.H.; Tembe, D.V. Prevalence and pattern of phantom ringing and phantom vibration among medical interns and their relationship with smartphone use and perceived stress. Indian J. Psychol. Med. 2018, 40, 440–445. [Google Scholar] [CrossRef]
- Rothberg, M.B.; Arora, A.; Hermann, J.; Kleppel, R.; Marie, P.S.; Visintainer, P. Phantom vibration syndrome among medical staff: A cross sectional survey. BMJ 2010, 341, c6914. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.-P.; Wu, C.-C.; Chang, L.-R.; Lin, Y.-H. Possible association between phantom vibration syndrome and occupational burnout. Neuropsychiatr. Dis. Treat. 2014, 10, 2307–2314. [Google Scholar] [CrossRef] [Green Version]
- Rosen, L.D.; Whaling, K.; Rab, S.; Carrier, L.M.; Cheever, N.A. Is facebook creating “iDisorders”? The link between clinical symptoms of psychiatric disorders and technology use, attitudes and anxiety. Comput. Hum. Behav. 2013, 29, 1243–1254. [Google Scholar] [CrossRef]
- Wang, Y.P.; Gorenstein, C. Psychometric properties of the beck depression inventory-II: A comprehensive review. Rev. Bras. Psiquiatr. 2013, 35, 416–431. [Google Scholar] [CrossRef] [Green Version]
- Tingley, D.; Yamamoto, T.; Hirose, K.; Keele, L.; Imai, K. Mediation: R package for causal mediation analysis. J. Stat. Softw. 2014, 59. [Google Scholar] [CrossRef] [Green Version]
- Kruger, D.J.; Djerf, J.M. High ringxiety: Attachment anxiety predicts experiences of phantom cell phone ringing. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 56–59. [Google Scholar] [CrossRef] [Green Version]
- Mata, D.A.; Ramos, M.A.; Bansal, N.; Khan, R.; Guille, C.; Di Angelantonio, E.; Sen, S. Prevalence of depression and depressive symptoms among resident physicians: A systematic review and meta-analysis. JAMA 2015, 314, 2373–2383. [Google Scholar] [CrossRef]
- Schwenk, T.L.; Davis, L.; Wimsatt, L.A. Depression, stigma, and suicidal ideation in medical students. JAMA 2010, 304, 1181–1190. [Google Scholar] [CrossRef] [Green Version]
- Asch, D.A.; Bilimoria, K.Y.; Desai, S.V. Resident duty hours and medical education policy—raising the evidence bar. N. Engl. J. Med. 2017, 376, 1704–1706. [Google Scholar] [CrossRef]
- Serafini, G.; Gonda, X.; Canepa, G.; Pompili, M.; Rihmer, Z.; Amore, M.; Engel-Yeger, B. Extreme sensory processing patterns show a complex association with depression, and impulsivity, alexithymia, and hopelessness. J. Affect. Disord. 2017, 210, 249–257. [Google Scholar] [CrossRef]
- Shizgal, P. Neural basis of utility estimation. Curr. Opin. Neurobiol. 1997, 7, 198–208. [Google Scholar] [CrossRef] [Green Version]
- Berridge, K.C.; Robinson, T.E. What is the role of dopamine in reward: Hedonic impact, reward learning, or incentive salience? Brain Res. Rev. 1998, 28, 309–369. [Google Scholar] [CrossRef]
- Heinz, A. Anhedonia—A general nosology surmounting correlate of a dysfunctional dopaminergic reward system? Der Nervenarzt 1999, 70, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Kapur, S.; Mizrahi, R.; Li, M. From dopamine to salience to psychosis—Linking biology, pharmacology and phenomenology of psychosis. Schizophr. Res. 2005, 79, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Schultz, W. Getting formal with dopamine and reward. Neuron 2002, 36, 241–263. [Google Scholar] [CrossRef] [Green Version]
- Phillips, P.E.; Stuber, G.D.; Heien, M.L.; Wightman, R.M.; Carelli, R.M. Subsecond dopamine release promotes cocaine seeking. Nature 2003, 422, 614–618. [Google Scholar] [CrossRef]
- Rees, W.D. The hallucinations of widowhood. Br. Med. J. 1971, 4, 37–41. [Google Scholar] [CrossRef] [Green Version]
- Ulrich-Lai, Y.M.; Herman, J.P. Neural regulation of endocrine and autonomic stress responses. Nat. Rev. Neurosci. 2009, 10, 397–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.-Y.; Lin, S.-H.; Li, P.; Huang, W.-L.; Lin, Y.-H. The role of the harm avoidance personality in depression and anxiety during the medical internship. Medicine 2015, 94, e389. [Google Scholar] [CrossRef]
- Lin, Y.H.; Chen, C.Y.; Lin, S.H.; Liu, C.H.; Weng, W.H.; Kuo, T.B.; Yang, C.C. Gender differences in cardiac autonomic modulation during medical internship. Psychophysiology 2013, 50, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.H.; Kuo, T.B.; Ho, Y.C.; Lin, S.H.; Liu, C.Y.; Yang, C.C. Physiological and psychological impacts on male medical interns during on-call duty. Stress 2012, 15, 21–30. [Google Scholar] [CrossRef]
- Task Force of the European Society of Cardiology; The North American Society of Pacing and Electrophysiology. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef] [Green Version]
- Chien, J.-W.; Chen, C.-Y.; Lin, S.-H.; Lin, S.-W.; Lin, Y.-H. Cardiac autonomic modulation during on-call duty under working hours restriction. Int. J. Environ. Res. Public Health 2020, 17, 1118. [Google Scholar] [CrossRef] [Green Version]
- Lin, Y.-H.; Chen, S.-Y.; Lin, P.-H.; Tai, A.-S.; Pan, Y.-C.; Hsieh, C.-E.; Lin, S.-H. Survival analysis for assessing user retention of a mobile application. JMIR MHealth UHealth 2019, in press. [Google Scholar] [CrossRef]

| Mediator of Interest | Anxiety | Depression | ||||||
|---|---|---|---|---|---|---|---|---|
| Effect | Estimate | 95% CI | p Value | Estimate | 95% CI | p Value | ||
| Total effect | 0.287 | 0.189 | 0.378 | <0.001 | 0.291 | 0.195 | 0.382 | <0.001 |
| Mediation effect | 0.036 | 0.010 | 0.067 | 0.008 | 0.065 | 0.016 | 0.116 | 0.006 |
| Alternative effect | 0.252 | 0.154 | 0.339 | <0.001 | 0.226 | 0.123 | 0.322 | <0.001 |
| Proportion mediated | 0.078 | 0.021 | 0.189 | 0.008 | 0.150 | 0.038 | 0.319 | 0.006 |
| Mediator of Interest | Anxiety | Depression | ||||||
|---|---|---|---|---|---|---|---|---|
| Effect | Estimate | 95% CI | p Value | Estimate | 95% CI | p Value | ||
| Total effect | 0.282 | 0.192 | 0.376 | <0.001 | 0.280 | 0.191 | 0.365 | <0.001 |
| Mediation effect | 0.039 | 0.013 | 0.072 | 0.002 | 0.094 | 0.052 | 0.142 | <0.001 |
| Alternative effect | 0.243 | 0.156 | 0.331 | <0.001 | 0.186 | 0.098 | 0.269 | 0.002 |
| Proportion mediated | 0.084 | 0.028 | 0.190 | 0.002 | 0.219 | 0.114 | 0.416 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, Y.-H.; Lin, K.-I.; Pan, Y.-C.; Lin, S.-H. Investigation of the Role of Anxiety and Depression on the Formation of Phantom Vibration and Ringing Syndrome Caused by Working Stress during Medical Internship. Int. J. Environ. Res. Public Health 2020, 17, 7480. https://doi.org/10.3390/ijerph17207480
Lin Y-H, Lin K-I, Pan Y-C, Lin S-H. Investigation of the Role of Anxiety and Depression on the Formation of Phantom Vibration and Ringing Syndrome Caused by Working Stress during Medical Internship. International Journal of Environmental Research and Public Health. 2020; 17(20):7480. https://doi.org/10.3390/ijerph17207480
Chicago/Turabian StyleLin, Yu-Hsuan, Kuan-I Lin, Yuan-Chien Pan, and Sheng-Hsuan Lin. 2020. "Investigation of the Role of Anxiety and Depression on the Formation of Phantom Vibration and Ringing Syndrome Caused by Working Stress during Medical Internship" International Journal of Environmental Research and Public Health 17, no. 20: 7480. https://doi.org/10.3390/ijerph17207480
APA StyleLin, Y. -H., Lin, K. -I., Pan, Y. -C., & Lin, S. -H. (2020). Investigation of the Role of Anxiety and Depression on the Formation of Phantom Vibration and Ringing Syndrome Caused by Working Stress during Medical Internship. International Journal of Environmental Research and Public Health, 17(20), 7480. https://doi.org/10.3390/ijerph17207480





