Effectiveness of a Novel Index System in Preventing Early Hearing Loss among Furniture Industry Skills Training Students in Malaysia
Abstract
:1. Introduction
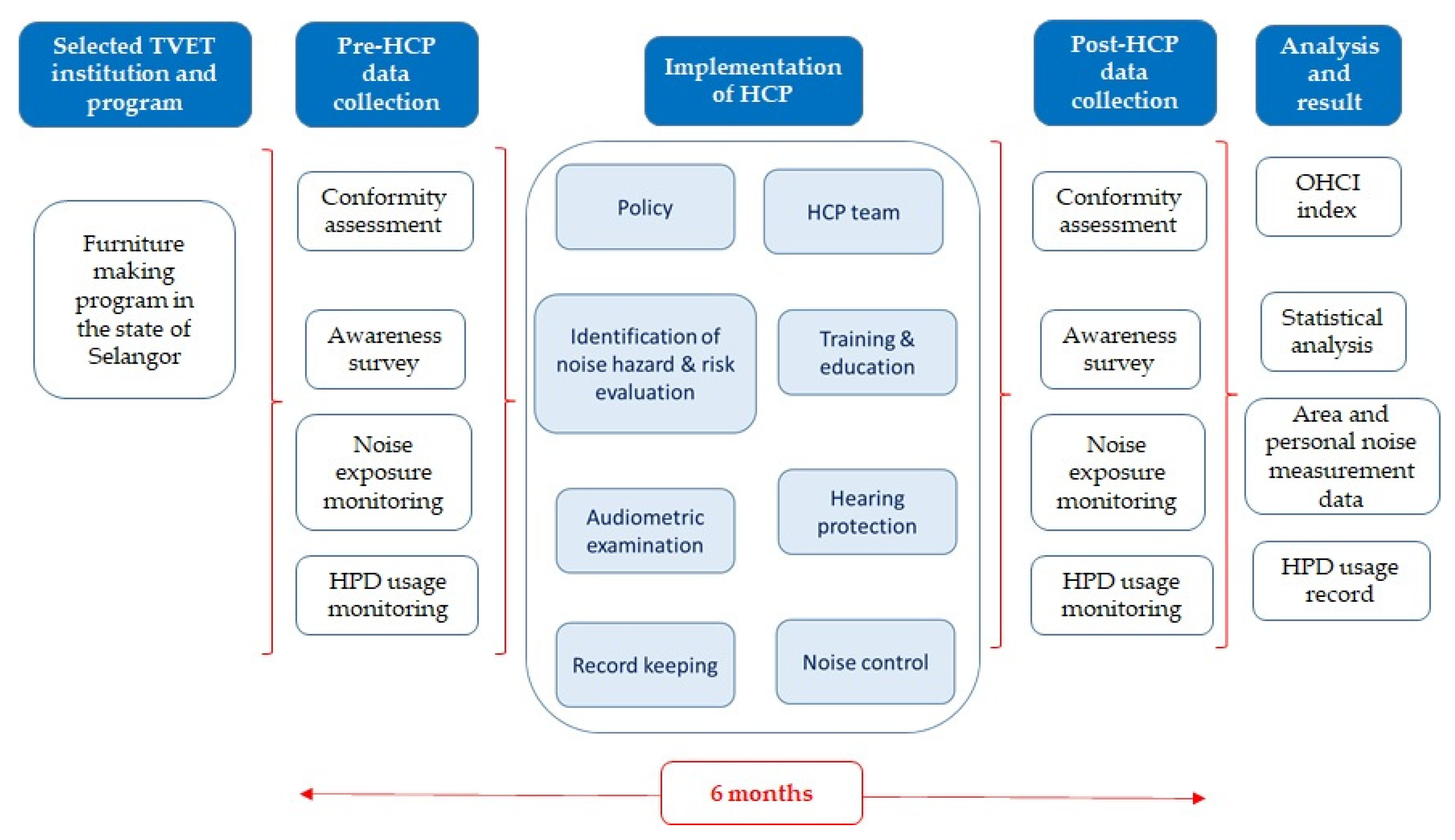
2. Materials and Methods
2.1. HCP Components and Conformity Assessment
2.2. Concept of OHCI
2.3. Field Work and Data Collection
3. Results and Discussion
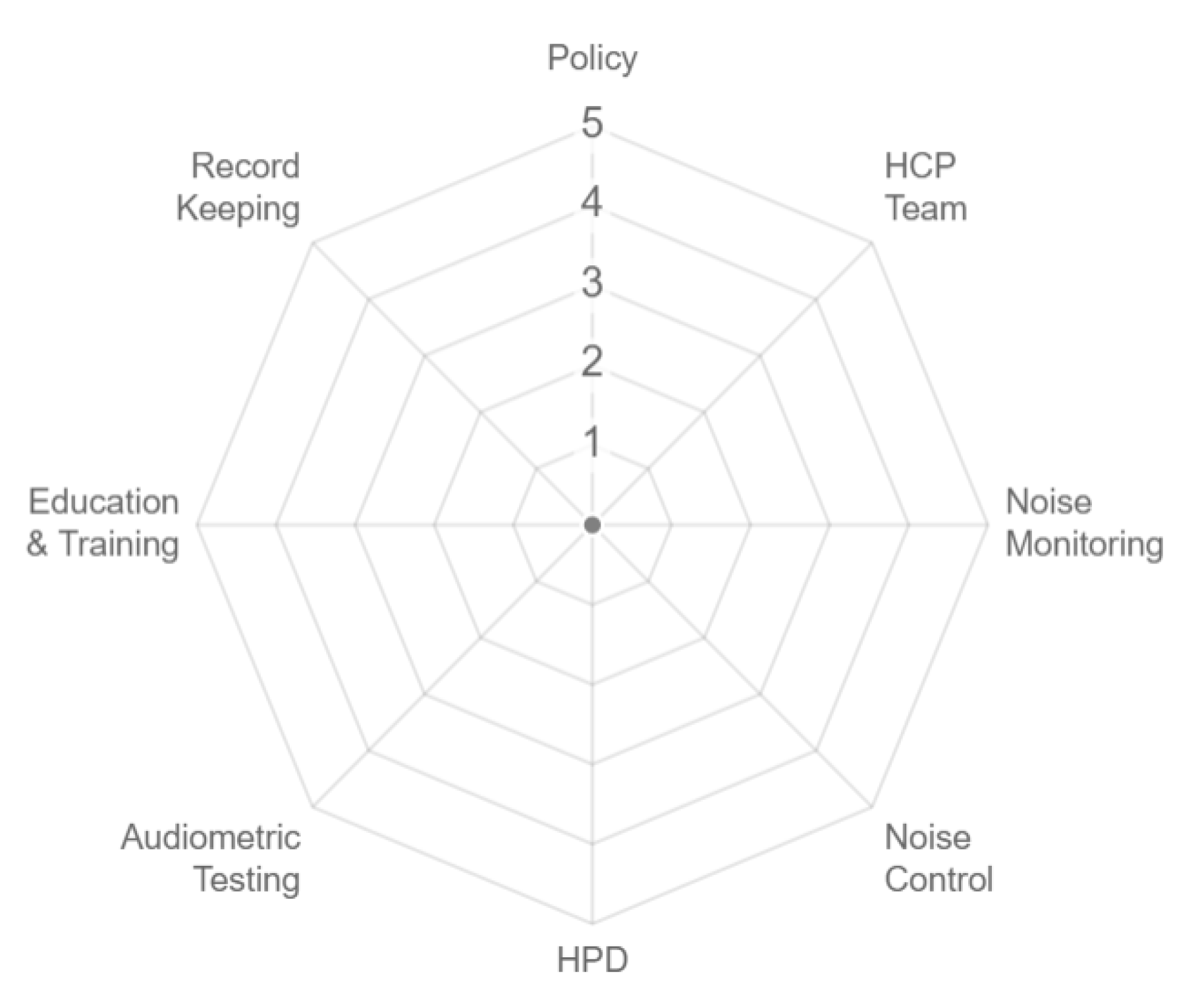
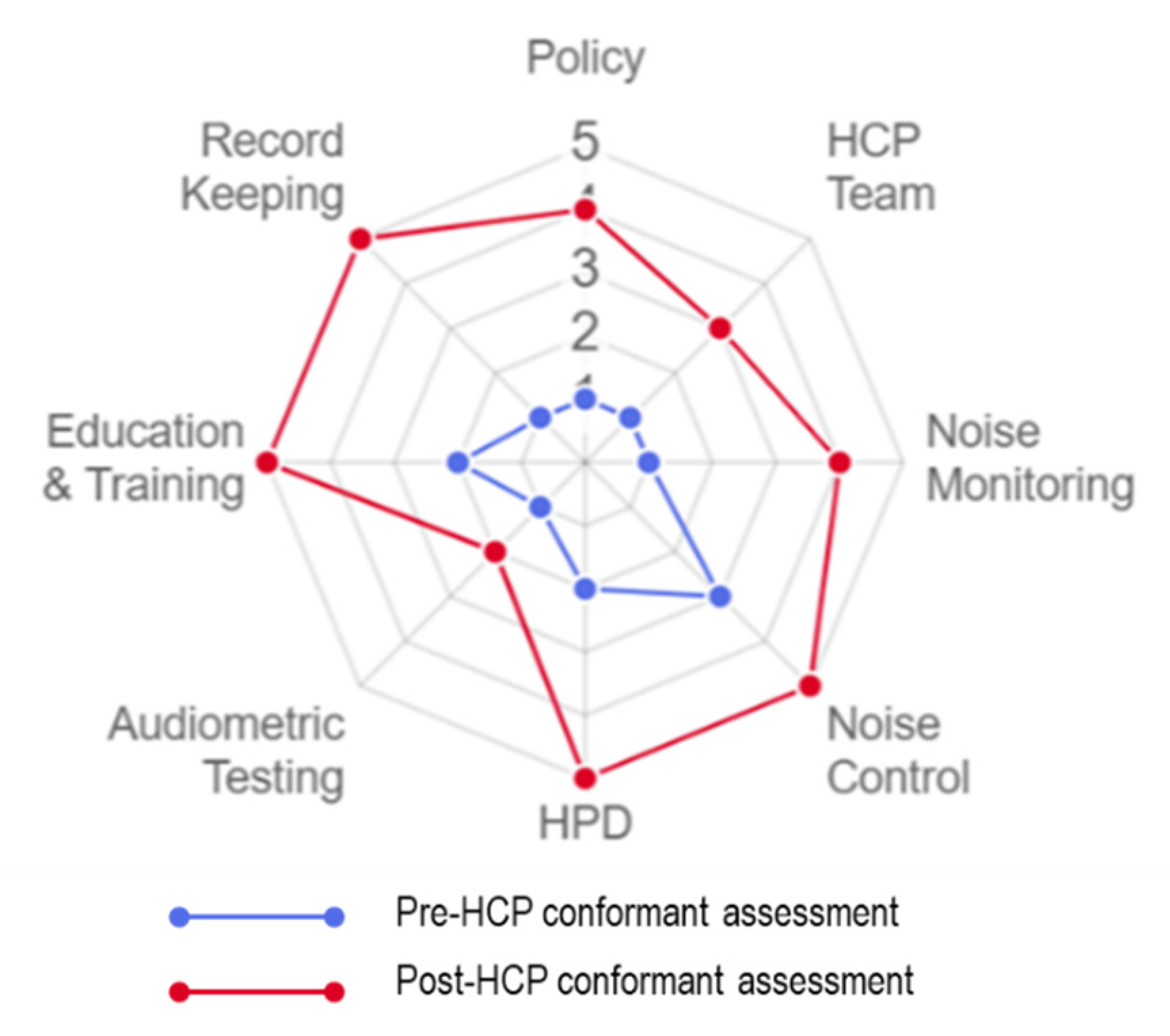
3.1. HCP Components Conformity Assessment and OHCI System
3.2. HPD Usage Report
3.3. Improvement in Self-Reporting Knowledge and Abilities
3.4. Noise Exposure Monitoring and Assessment of Proposed Control Action
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Addressing The Rising Prevalence of Hearing Loss; World Health Organization: Geneva, Switzeland, 2018. [Google Scholar]
- Brown, C.S.; Emmett, S.D.; Robler, S.K.; Tucci, D.L. Global Hearing Loss Prevention. Otolaryngol. Clin. N. Am. 2018, 51, 575–592. [Google Scholar] [CrossRef] [PubMed]
- Huddle, M.G.; Goman, A.M.; Kernizan, F.C.; Foley, D.M.; Price, C.; Frick, K.D.; Lin, F.R. The economic impact of adult hearing loss: A systematic review. JAMA Otolaryngol. Head Neck Surg. 2017, 143, 1040–1048. [Google Scholar] [CrossRef] [PubMed]
- Mariola, S.-K. New trends in the prevention of occupational noise-induced hearing loss. Int. J. Occup. Med. Environ. Health 2020, 33, 1–8. [Google Scholar] [CrossRef]
- Shroff, F.M.; Jung, D. Here’s to sound action on global hearing health through public health approaches. Int. J. Health Gov. 2020, 25, 235–244. [Google Scholar] [CrossRef]
- Clark, J.L.; Swanepoel, D.W. Technology for hearing loss-as We Know it, and as We Dream it. Disabil. Rehabil. Assist. Technol. 2014, 9, 408–413. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization & World Bank World Report On Disability. World Health Organ. 2011, 8, 1–268.
- Bahagian Kesihatan Pekerjaan. Statistik Penyakit dan Keracunan Pekerjaan 2019 (Sehingga Februari); Department of Safety and Health Malaysia: Putrajaya, Malaysia, 2019; Volume 2019.
- Social Security Organization. Noise Induced Hearing Loss Statistic (NIHL) 2005–2014; Social Security Organization: Woodlawn, MD, USA, 2015.
- Singh, L.P.; Bhardwaj, A.; Deepak, K.K. Occupational noise-induced hearing loss in indian steel industry workers: An exploratory study. Hum. Factors 2013, 55, 411–424. [Google Scholar] [CrossRef]
- Feder, K.; Michaud, D.; McNamee, J.; Fitzpatrick, E.; Davies, H.; Leroux, T. Prevalence of Hazardous Occupational Noise Exposure, Hearing Loss, and Hearing Protection Usage among a Representative Sample of Working Canadians. J. Occup. Environ. Med. 2017, 59, 92–113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rong, T.X.; Hassim, M.H.; Halim, M.Z.B.A. Noise induced hearing loss (NIHL) effect among workers in small medium enterprises (SME) in Malaysia. Chem. Eng. Trans. 2017, 56, 1741–1746. [Google Scholar] [CrossRef]
- Williams, W.; Brumby, S.; Calvano, A.; Hatherell, T.; Mason, H.; Mercer-Grant, C.; Hogan, A. Farmers’ work-day noise exposure: Farmers’ Noise Exposure. Aust. J. Rural Health 2015, 23, 67–73. [Google Scholar] [CrossRef]
- Dudarewicz, A.; Zaborowski, K.; Rutkowska-Kaczmarek, P.; Zamojska-Daniszewska, M.; Śliwińska-Kowalska, M.; Zamysłowska-Szmytke, E.; Pawlaczyk-Śuszczyńska, M. The Hearing Threshold of Employees Exposed to Noise Generated by the Low-Frequency Ultrasonic Welding Devices. Arch. Acoust. 2017, 42, 199–205. [Google Scholar] [CrossRef] [Green Version]
- Tahir, N.; Aljunid, S.M.; Hashim, J.H.; Begum, J. Burden of noise induced hearing loss among manufacturing industrial workers in Malaysia. Iran. J. Public Health 2014, 43, 148–153. [Google Scholar]
- Durcan, F.M.; Burdurlu, E. Effects of some machining parameters on noise level in planing of some wood materials. BioResources 2018, 13, 2702–2714. [Google Scholar] [CrossRef]
- Ratnasingam, J.; Natthondan, V.; Ioras, F.; McNulty, T. Dust, noise and chemical solvents exposure of workers in the wooden furniture industry in South East Asia. J. Appl. Sci. 2010, 10, 1413–1420. [Google Scholar] [CrossRef]
- DOSH. Occupational Safety and Health (Noise Exposure) Regulations 2019; Department of Occupational Safety and Health Malaysia: Putrajaya, Malaysia, 2019.
- United States Environmental Protection Agency EPA Identifies Noise Levels Affecting Health and Welfare. Available online: http://www.epa.gov/aboutepa/epa-identifies-noise-levels-affecting-health-and-welfare (accessed on 15 September 2020).
- Fink, D.J. What is a safe noise level for the public? Am. J. Public Health 2017, 107, 44–45. [Google Scholar] [CrossRef] [PubMed]
- Fink, D. 85 dB is Not a Safe Noise Level to Prevent Hearing Loss. Hear. J. 2019, 51, 26–27. [Google Scholar] [CrossRef]
- DOSH. Industry Code of Practice for Management of Occupational Noise Exposure and Hearing Conversation 2019; Department of Occupational Safety and Health Malaysia: Putrajaya, Malaysia, 2019; pp. 1–83.
- Sriopas, A.; Chapman, R.S.; Sutammasa, S.; Siriwong, W. Occupational noise-induced hearing loss in auto part factory workers in welding units in Thailand. J. Occup. Health 2017, 59, 55–62. [Google Scholar] [CrossRef] [Green Version]
- Fonseca, V.R.; Marques, J.; Panegalli, F.; Gonçalves, C.G.D.O.; Souza, W. Prevention of the Evolution of Workers’ Hearing Loss from Noise-Induced Hearing Loss in Noisy Environments through a Hearing Conservation Program. Int. Arch. Otorhinolaryngol. 2014, 20, 43–47. [Google Scholar] [CrossRef] [Green Version]
- Allooef, M.M. The Effectiveness of Hearing Conservation Program in the Workplace. Glob. J. Otolaryngol. 2017, 5, 117–119. [Google Scholar] [CrossRef]
- Rogers, B.; Meyer, D.; Summey, C.; Scheessele, D.; Atwell, T.; Ostendorf, J.; Randolph, S.A.; Buckheit, K. What makes a successful hearing conservation program? AAOHN J. 2009, 57, 321–336. [Google Scholar] [CrossRef]
- Suter, A.H.; Frank, J.R. a Practical Guide To Effective Hearing Conservation Programs Inthe Workplace.Pdf; National Institue for occupational Safety and Health (NIOSH): Washington, DC, USA, 1990.
- Harris, F. Hearing Conservation; OSHA: Washington, DC, USA, 1978; Volume 71.
- Safe Work Australia. Code of Practice: Managing and Preventing Hearing Loss at Work; Safe Work Australia: Keswick, Australia, 2015; ISBN 9780642333056. [Google Scholar]
- Bolger, A. Ryan’s Hearing Conservation Program. Am. Ind. Hyg. Assoc. Q. 1956, 17, 52–54. [Google Scholar] [PubMed]
- Minister of Labour. Factories And Machinery (Noise Exposure) Regulations 1989; Minister of Labour: Putrajaya, Malaysia, 1989; pp. 1–3. [Google Scholar]
- Nor Saleha, I.T.; Noor Hassim, I. A study on compliance to Hearing Conservation Programme among industries in Negeri Sembilan, Malaysia. Ind. Health 2006, 44, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Sam, W.Y.; Anita, A.R.; Hayati, K.S.; Haslinda, A.; Lim, C.S. Prevalence of hearing loss and hearing impairment among small and medium enterprise workers in Selangor, Malaysia. Sains Malaysiana 2017, 46, 267–274. [Google Scholar] [CrossRef]
- Ock, M.; Pyo, J.; Kim, O.H.; Chae, C.; Ye, B.J.; Kim, S.H.; An, H.C.; Kim, A.; Park, J.O.; Lee, J. Experience and awareness of health managers, administrators, and workers on a hearing conservation program in Korea: A qualitative study. Int. J. Environ. Res. Public Health 2020, 17, 2302. [Google Scholar] [CrossRef] [Green Version]
- Biabani, A.; Aliabadi, M.; Golmohammadi, R.; Farhadian, M. Individual Fit Testing of Hearing Protection Devices Based on Microphone in Real Ear. Saf. Health Work 2017, 8, 364–370. [Google Scholar] [CrossRef]
- OSHA 1910.95 App B - Methods for estimating the adequacy of hearing protector attenuation. Available online: https://www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.95AppB (accessed on 6 September 2020).
- Aliabadi, M.; Biabani, A.; Golmohammadi, R.; Farhadian, M. A study of the real-world noise attenuation of the current hearing protection devices in typical workplaces using Field Microphone in Real Ear method. Work 2018, 60, 271–279. [Google Scholar] [CrossRef]
- Morata, T.C.; Meinke, D. Uncovering Effective Strategies for Hearing Loss Prevention. Acoust. Aust. 2016, 44, 67–75. [Google Scholar] [CrossRef] [Green Version]
- NIOSH/NHCA/OSHA Alliance Best Practice Bulletin: Hearing Protection - Emerging Trends: Individual Fit Testing. Available online: www.osha.gov/dcsp/alliances/niosh_nhca/niosh_nhca.html (accessed on 6 October 2020).
- Frederiksen, T.; Ramlau-Hansen, C.; Stokholm, Z.; Grynderup, M.; Hansen, Å.; Kristiansen, J.; Vestergaard, J.; Bonde, J.; Kolstad, H. Noise-Induced Hearing Loss-A Preventable Disease? Results of a 10-Year Longitudinal Study of Workers Exposed to Occupational Noise. Noise Health 2017, 19, 103–111. [Google Scholar] [CrossRef]
- Arezes, P.M.; Miguel, A.S. Hearing protection use in industry: The role of risk perception. Saf. Sci. 2005, 43, 253–267. [Google Scholar] [CrossRef]
- Rabinowitz, P.; Cantley, L.F.; Galusha, D.; Trufan, S.; Swersey, A.; Dixon-Ernst, C.; Ramirez, V.; Neitzel, R. Assessing hearing conservation program effectiveness: Results of a multisite assessment. J. Occup. Environ. Med. 2018, 60, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Muhr, P.; Johnson, A.C.; Skoog, B.; Rosenhall, U. A demonstrated positive effect of a hearing conservation program in the Swedish armed forces. Int. J. Audiol. 2016, 55, 168–172. [Google Scholar] [CrossRef]
- Neitzel, R.; Seixas, N. The effectiveness of hearing protection among construction workers. J. Occup. Environ. Hyg. 2005, 2, 227–238. [Google Scholar] [CrossRef]
- Kim, K.S. Occupational hearing loss in Korea. J. Korean Med. Sci. 2010, 25, 62–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NIDCD. U.S. Adults Aged 20 to 69 Years Show Signs of Noise-Induced Hearing Loss|NIDCD. Available online: https://www.nidcd.nih.gov/news/2017/us-adults-aged-20-69-years-show-signs-noise-induced-hearing-loss (accessed on 16 April 2020).
- O’Sullivan, D. Prevention of NIHL and Tinnitus is Possible: Dangerous Decibels® Update. Can. Audiol. 2020, 7, 3–5. [Google Scholar]
- Gilles, A.; Paul, V.d.H. Effectiveness of a preventive campaign for noise-induced hearing damage in adolescents. Int. J. Pediatr. Otorhinolaryngol. 2014, 78, 604–609. [Google Scholar] [CrossRef] [PubMed]
- Reed, D.B.; Westneat, S.C.; Kidd, P. Observation study of students who completed a high school agricultural safety education program. J. Agric. Saf. Health 2003, 9, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Reed, D.B.; Kidd, P.S.; Westneat, S.; Rayens, M.K. Agricultural disability awareness and risk education (AgDARE) for high school students. Inj. Prev. 2001, 7, 59–64. [Google Scholar] [CrossRef]
- NIDCD-NIH Noisy Planet. Available online: https://www.noisyplanet.nidcd.nih.gov/ (accessed on 6 October 2020).
- New York City Department of Environmental Protection Sound & Noise Education Module-DEP. Available online: https://www1.nyc.gov/site/dep/environment/sound-noise-education-module.page (accessed on 6 October 2020).
- Folmer, R.L. The importance of hearing conservation instruction. J. Sch. Nurs. 2003, 19, 140–148. [Google Scholar] [CrossRef]
- Bernama Malaysia to have 35pc Skilled Workers by 2020. Available online: http://www.themalaymailonline.com/money/article/malaysia-to-have-35pc-skilled-workers-by-2020 (accessed on 10 April 2020).
- Edward, M.; Manohar, S.; Somayaji, G.; Kallikkadan, H.H. Prevalence, awareness, and preventive practices of noise-induced hearing loss in a plywood industry. Indian J. Otol. 2016, 22, 14–18. [Google Scholar] [CrossRef]
- Ratnasingam, J.; Ioras, F.; Abrudan, I.V. An evaluation of occupational accidents in the wooden furniture industry - A regional study in South East Asia. Saf. Sci. 2012, 50, 1190–1195. [Google Scholar] [CrossRef]
- Abduljabbar Ibrahim, S. Study Noise Effects on The Students of The Faculty of Engineering/ Mustansiriyah University. Al-Nahrain J. Eng. Sci. 2018, 21, 178–186. [Google Scholar] [CrossRef] [Green Version]
- NS, M.; M, M. Occupational Health and Safety Training: Knowledge, Attitude and Practice Among Technical Education Students. Egypt. J. Occup. Med. 2014, 38, 153–165. [Google Scholar] [CrossRef]
- Schulte, P.A.; Stephenson, C.M.; Okun, A.H.; Palassis, J.; Biddle, E. Integrating occupational safety and health information into vocational and technical education and other workforce preparation programs. Am. J. Public Health 2005, 95, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Meinke, D.K.; Morata, T.C. Awarding and promoting excellence in hearing loss prevention. Int. J. Audiol. 2012, 51, S63–S70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sayapathi, B.S.; Ting Su, A.; Koh, D. Knowledge, attitudes and practice in relation to noise-induced hearing loss in two factories. In Proceedings of the International Conference on Innovative Trends in Multidisciplinary Academic Research, Istanbul, Turkey, 20–21 October 2014; Global Illuminators: Istanbul, Turkey, 2014; Volume 2004, pp. 562–576. [Google Scholar]
- ISO. ISO 9612: Determination of Occupational Noise Exposure; Engineering Method: Basel, Switzerland, 2009. [Google Scholar]
- Andersson, I.M.; Gunnarsson, K.; Rosèn, G. Role of headmasters, teachers, and supervisors in knowledge transfer about occupational health and safety to pupils in vocational education. Saf. Health Work 2015, 6, 317–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sayler, S.K.; Rabinowitz, P.M.; Cantley, L.F.; Galusha, D.; Neitzel, R.L. Costs and effectiveness of hearing conservation programs at 14 US metal manufacturing facilities. Int. J. Audiol. 2018, 57, S3–S11. [Google Scholar] [CrossRef] [PubMed]
- Trabeau, M.; Neitzel, R.; Meischke, H.; Daniell, W.E.; Seixas, N.S. A comparison of “Train-the-Trainer” and expert training modalities for hearing protection use in construction. Am. J. Ind. Med. 2008, 51, 130–137. [Google Scholar] [CrossRef]
- Thepaksorn, P.; Siriwong, W.; Neitzel, R.L.; Somrongthong, R.; Techasrivichien, T. Relationship Between Noise-Related Risk Perception, Knowledge, and the Use of Hearing Protection Devices Among Para Rubber Wood Sawmill Workers. Saf. Health Work 2018, 9, 25–29. [Google Scholar] [CrossRef]
- Beach, E.F.; Nielsen, L.; Gilliver, M. Providing earplugs to young adults at risk encourages protective behaviour in music venues. Glob. Health Promot. 2016, 23, 45–56. [Google Scholar] [CrossRef] [Green Version]
- DelGiacco, A.M.; Serpanos, Y.C.; Gunderson, E. Education and Knowledge of Noise Exposure, Hearing Loss, and Hearing Conservation in College Students. Contemp. Issues Commun. Sci. Disord. 2015, 42, 88–99. [Google Scholar] [CrossRef]
- Reddy, R.; Welch, D.; Ameratunga, S.; Thorne, P. An ecological approach to hearing-health promotion in workplaces. Int. J. Audiol. 2017, 56, 316–327. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, M.R.; Shaw, P.B.; Stephenson, C.M.; Graydon, P.S. Hearing loss prevention for carpenters: Part 2—Demonstration projects using individualized and group training. Noise Health 2011, 13, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Berger, E.H.; Neitzel, R.; Kladden, C.A. Noise Navigator; 3M personal safety division: Indianapolis, Indiana, 2013; ISBN 3176923031. [Google Scholar]

| Components | Policy (n = 5) | Noise Monitoring (n = 8) | Noise Control (n = 4) | Hearing Protection Devices (HPD) (n = 6) | Audiometric Test (n = 4) | Education and Training (n = 5) | Record-Keeping (n = 4) | HCP Team (n = 4) |
|---|---|---|---|---|---|---|---|---|
| Indicators | HCP Policy | Conduct identification of excessive noise annually | Implement engineering control solely or | Provision of HPD | Perform Audiometric testing on the exposed employee | Dissemination of information regarding noise exposure and HCP | Maintain a proper record of Noise identification assessment | Appointment of Hearing Conservation Administrator (HCA) |
| Action plan for each HCP component | Conduct noise risk assessment by a registered assessor | Implement engineering control and administrative control or | HPD according to the approved standard | Notify employee within 21 days after report received | Dissemination of Instruction regarding noise exposure and HCP | Maintain a proper record of Noise risk assessment | HCA shall coordinate all aspects of HCP | |
| Establish target to reduce personal noise exposure level to below LAeq 82 dBA | Conduct Personal noise exposure monitoring | Implement administrative control solely | Provides full information on the attenuation values to employees and HCA | If negative for any STS inform the employee to maintain and improve preventive practice or | Organize training and education program regarding noise exposure | Maintain a proper record of Employee audiometric testing | HCA and team member shall possess knowledge on HCP and related legal requirement | |
| Review HCP annually | Conduct area noise exposure monitoring | Provision of HPD | HPD suitable to the working environment | Implement control measure for the employee with positive for TSTS and retest after three months or | Training on HPD | Maintain a proper record of Supporting documents on HCP implementation | HCA and team member shall be sent to HCP competency training | |
| Establishment of buy quiet policy | Use approved equipment for noise exposure monitoring | Designate hearing protection zone | Perform individual fitting test | Implement control measure for the employee diagnosed with ONIHL, HI, PSTS | Conduct awareness survey/ability assessment | |||
| Construct noise mapping | Enforce rules and regulation for the hearing protection zone | Consideration on the safety of the HPD wearer and others surround | Carry out audiometric test within three months after employee commencing work at noisy area | |||||
| Findings and recommendation is presented to the exposed employee | ||||||||
| Carry out report recommendation |
| Compliance Level | Compliance Percentage | OHCI Score | Mean OHCI Score | OHCI Class |
|---|---|---|---|---|
| Excellent | 80%–100% | 5 | 4.01–5.00 | 5 |
| Good | 60%–79% | 4 | 3.01–4.00 | 4 |
| Moderate | 40%–59% | 3 | 2.01–3.00 | 3 |
| Fair | 20%–39% | 2 | 1.01–2.00 | 2 |
| Poor | 0–19% | 1 | ≤1 | 1 |
| HCP Components | Pre-HCP | Post-HCP | p Value | ||
|---|---|---|---|---|---|
| Compliance (%) | OHCI Score | Compliance (%) | OHCI Score | ||
| Policy | 0 | 1 | 70 | 4 | 0.005 |
| Noise monitoring | 0 | 1 | 68.8 | 4 | 0.001 |
| Noise control | 50 | 3 | 87.5 | 5 | 0.058 |
| HPD | 25 | 2 | 100 | 5 | 0.001 |
| Audiometric testing | 0 | 1 | 37.5 | 2 | 0.058 |
| Education and training | 20 | 2 | 100 | 5 | 0.003 |
| HCP team | 0 | 1 | 50 | 3 | 0.092 |
| Record-keeping | 0 | 1 | 100 | 5 | 0.006 |
| OHCI mean score | 1.5 | 4.1 | |||
| OHCI class | 2 | 5 | |||
| Item | Subject | Pre-HCP (n = 33) | Post-HCP (n = 33) | Paired Samples t-Test | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t | df | p | ||
| 1 | Knowledge on Occupational Noise Induced Hearing Loss (ONIHL) | 2.5 | 1.1 | 3.6 | 0.94 | −8.2 | 32 | <0.001 |
| 2 | Knowledge on social disadvantages of Occupational Noise Induced Hearing Loss (ONIHL) | 3.1 | 1.1 | 3.7 | 0.8 | −3.9 | 32 | 0.001 |
| 3 | Knowledge on hearing mechanism | 1.9 | 1.0 | 3.2 | 0.8 | −7.0 | 32 | <0.001 |
| 4 | Knowledge on risk factors lead to hearing loss | 2.7 | 0.9 | 3.3 | 0.7 | −4.9 | 32 | <0.001 |
| 5 | Knowledge on purpose of audiometric testing | 2.7 | 1.0 | 3.0 | 0.8 | −2.2 | 32 | 0.037 |
| 6 | Knowledge on noise control plan at the workplace | 2.4 | 1.0 | 3.3 | 0.7 | −4.5 | 32 | <0.001 |
| 7 | Ability to identify excessive noise warning sign at the workplace | 2.8 | 1.0 | 3.2 | 0.7 | −2.0 | 32 | >0.05 |
| 8 | Knowledge on rules and regulations in hearing protection zone | 1.9 | 0.9 | 3.3 | 0.5 | −8.9 | 32 | <0.001 |
| 9 | Ability to identify excessive noise source or area at the workplace | 2.3 | 0.8 | 3.3 | 0.5 | −8.1 | 32 | <0.001 |
| 10 | Knowledge on noise exposure limit | 1.9 | 0.9 | 3.0 | 0.8 | −6.0 | 32 | <0.001 |
| 11 | Knowledge on hearing conservation program (HCP) | 2.6 | 0.8 | 2.9 | 0.9 | −1.8 | 32 | >0.05 |
| 12 | Knowledge on the purpose of Hearing Protection Devices (HPD) | 1.9 | 0.9 | 3.7 | 0.6 | −8.8 | 32 | <0.001 |
| 13 | Ability to select appropriate type of HPD based on job | 2.5 | 1.1 | 3.2 | 0.7 | −5.0 | 32 | <0.001 |
| 14 | Ability to ensure HPD is properly fit when use | 2.2 | 1.1 | 3.9 | 0.7 | −8.9 | 32 | <0.001 |
| 15 | Ability to maintain good condition of HPD | 2.2 | 1.1 | 3.3 | 0.7 | −6.0 | 32 | <0.001 |
| Furniture Making Training Activities | Machines/Tools | Average Time (Min) | Pre-HCP Measurement | Post-HCP Measurement | ||
|---|---|---|---|---|---|---|
| Source Measurement (dBA) n = 3 Mean (SD) | Personal Exposure Measurement (dBA) n = 3 Mean (SD) LAeq | Source Measurement (dBA) n = 3 Mean (SD) | Personal Exposure Measurement (dBA) n = 3 Mean (SD) LAeq | |||
| Surface planing | Thicknesser planer Portable thicknesser planer | 120 | 101.1 (1.3) | 90.7 (2.4) * | 100.7 (2.6) | 85.6 (0.6) * |
| Wood shaping | Lathe machine Band saw Portable jig saw Scroll saw Orbital sander | 120 | 96.2 (1.3) | 95.8 (1.8) | ||
| Wood cutting | Portable circular saw Sliding table saw Auto rip saw | 90 | 98.7 (1.4) | 98.9 (0.7) | ||
| Wood edging | Portable trimmer Portable router Sanding machine Jointer planer | 60 | 94.4 (0.8) | 93.9 (1.2) | ||
| Part assemble | Drilling machine Cordless drill | 90 | 88.4 (1.6) | 87.3 (0.8) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdul Rahim, K.A.; Jewaratnam, J.; Che Hassan, C.R.; Hamid, M.D. Effectiveness of a Novel Index System in Preventing Early Hearing Loss among Furniture Industry Skills Training Students in Malaysia. Int. J. Environ. Res. Public Health 2020, 17, 8032. https://doi.org/10.3390/ijerph17218032
Abdul Rahim KA, Jewaratnam J, Che Hassan CR, Hamid MD. Effectiveness of a Novel Index System in Preventing Early Hearing Loss among Furniture Industry Skills Training Students in Malaysia. International Journal of Environmental Research and Public Health. 2020; 17(21):8032. https://doi.org/10.3390/ijerph17218032
Chicago/Turabian StyleAbdul Rahim, Khairul Azhar, Jegalakshimi Jewaratnam, Che Rosmani Che Hassan, and Mahar Diana Hamid. 2020. "Effectiveness of a Novel Index System in Preventing Early Hearing Loss among Furniture Industry Skills Training Students in Malaysia" International Journal of Environmental Research and Public Health 17, no. 21: 8032. https://doi.org/10.3390/ijerph17218032
APA StyleAbdul Rahim, K. A., Jewaratnam, J., Che Hassan, C. R., & Hamid, M. D. (2020). Effectiveness of a Novel Index System in Preventing Early Hearing Loss among Furniture Industry Skills Training Students in Malaysia. International Journal of Environmental Research and Public Health, 17(21), 8032. https://doi.org/10.3390/ijerph17218032





