A Health Guidance App to Improve Motivation, Adherence to Lifestyle Changes and Indicators of Metabolic Disturbances among Japanese Civil Servants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
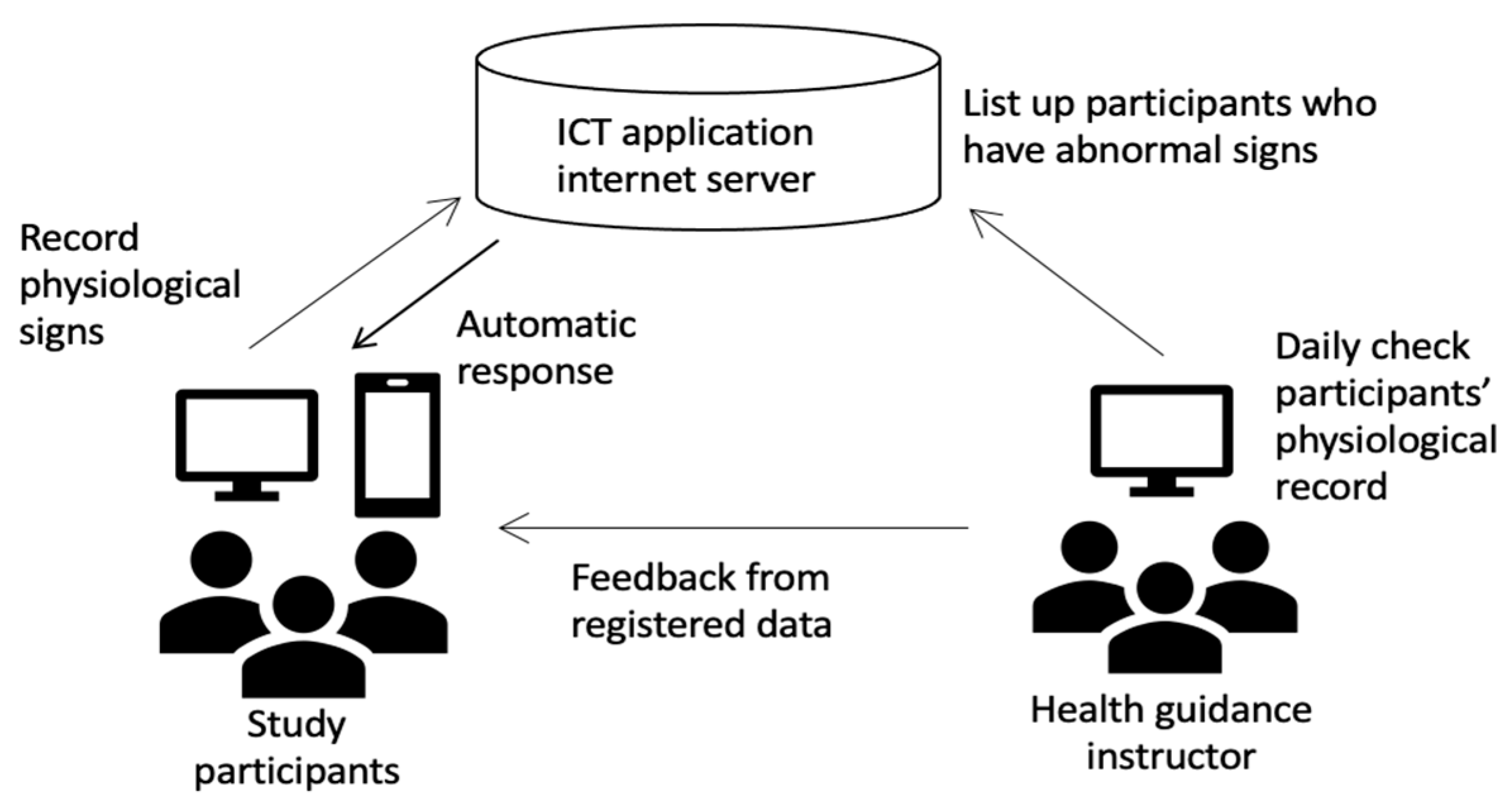
2.2. Study Protocol
2.3. Outcome Measures
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kasper, P.; Martin, A.; Lang, S.; Kütting, F.; Goeser, T.; Demir, M.; Stefen, H.M. NAFLD and cardiovascular diseases: A clinical review. Clin. Res. Cardiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Yadav, D.; Puranik, N.; Sen, A.; Mishra, M.; Kwak, M.; Jin, J.O. Metabolic syndrome criteria and its association with type 2 diabetes and cardiovascular diseases. Progr. Nutr. 2020, 22, 361–369. (In Japanese) [Google Scholar]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [PubMed] [Green Version]
- Bassi, N.; Karagodin, I.; Wang, S.; Vassallo, P.; Priyanath, A.; Massaro, E.; Stone, N.J. Lifestyle Modification for Metabolic Syndrome: A Systematic Review. Am. J. Med. 2014, 127, 1242.e1–1242.e10. [Google Scholar] [CrossRef] [PubMed]
- Joo, Y.L.; Hyeoun, A.; Yul, H. Transtheoretical Model-based Nursing Intervention on Lifestyle Change: A Review Focused on Intervention Delivery Methods. Asian Nurs. Res. 2015, 9, 158–167. [Google Scholar]
- Radhakrishnan, K. The efficacy of tailored interventions for self-management outcomes of type 2 diabetes, hypertension or heart disease: A systematic review. J. Adv. Nurs. 2012, 68, 496–510. [Google Scholar] [CrossRef] [PubMed]
- Barbara, K.R.; Matthew, W.K. Advancing tailored health communication: A persuasion and message effects perspective. J. Commun. 2006, 56, S184–S201. [Google Scholar]
- Noar, S.M.; Benac, C.N.; Harris, M.S. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol. Bull. 2007, 133, 673–693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lau, P.W.; Lau, E.Y.; Wong, D.P.; Ransdell, L. A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. J. Med. Internet. Res. 2011, 13, e48. [Google Scholar] [CrossRef] [PubMed]
- Norman, G.J.; Zabinski, M.F.; Adams, M.A.; Rosenberg, D.E.; Yaroch, A.L.; Atienza, A.A. A review of eHealth interventions for physical activity and dietary behavior change. Am. J. Prev. Med. 2007, 33, 336–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lustria, M.L.; Cortese, J.; Noar, S.M.; Glueckauf, R.L. Computer-tailored health interventions delivered over the web: Review and analysis of key components. Patient Educ. Couns. 2009, 74, 156–173. [Google Scholar] [CrossRef] [PubMed]
- Kuijpers, W.; Groen, W.G.; Aaronson, N.K.; van Harten, W.H. A systematic review of web-based interventions for patient empowerment and physical activity in chronic diseases: Relevance for cancer survivors. J. Med. Internet. Res. 2013, 15, e37. [Google Scholar] [CrossRef] [Green Version]
- Wantland, D.J.; Portillo, C.J.; Holzemer, W.L.; Slaughter, R.; McGhee, E.M. The effectiveness of Web-based vs. non-Web-based interventions: A meta-analysis of behavioral change outcomes. J. Med. Internet. Res. 2004, 6, e40. [Google Scholar] [CrossRef] [PubMed]
- Tsushita, K.; Hosler, A.S.; Miura, K.; Ito, Y.; Fukuda, T.; Kitamura, A.; Tatara, K. Rationale and Descriptive Analysis of Specific Health Guidance: The Nationwide Lifestyle Intervention Program Targeting Metabolic Syndrome in Japan. J. Atheroscler. Thromb. 2018, 25, 308–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohro, T.; Furui, Y.; Mitsutake, N.; Fujii, R.; Morita, H.; Oku, S.; Ohe, K.; Nagai, R. The Japanese national health screening and intervention program aimed at preventing worsening of the metabolic syndrome. Int. Heart. J. 2008, 49, 193–203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mizushima, S.; Tsushita, K. New strategy on prevention and control of non-communicable lifestyle-related diseases focusing on metabolic syndrome in Japan. In Asian Perspectives and Evidence on Health Promotion and Education; Springer: Tokyo, Japan, 2011; pp. 31–39. [Google Scholar]
- Diagnostic Criteria Review Committee of Japan. Definition and diagnostic criteria of metabolic syndrome. J. Jpn. Soc. Intern. Med. 2005, 94, 188–203. [Google Scholar]
- Richard, C.; Couture, P.; Desroches, S.; Lamarche, B. Effect of the Mediterranean Diet with and Without Weight Loss on Markers of Inflammation in Men with Metabolic Syndrome. Obesity 2013, 21, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Balkau, B.; Picard, P.; Vol, S.; Fezeu, L.; Eschwège, E.; The DESIR Study Group. Consequences of Change in Waist Circumference on Cardiometabolic Risk Factors Over 9 Years. Data from an Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetes Care 2007, 30, 1901–1903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, J.O. Can a small-changes approach help address the obesity epidemic? A report of the Joint Task Force of the American Society for Nutrition, Institute of Food Technologists, and International Food Information Council. Am. J. Clin. Nutr. 2009, 89, 477–484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wyatt, H.R.; Wing, R.R.; Hill, J.O. The National Weight Control Registry. In Evaluation and Management of Obesity; Hanley & Belfus Inc: Philadelphia, PA, USA, 2002; pp. 119–224. [Google Scholar]


| Indicators of Metabolic Disturbances | Baseline Assessment | Assessment at Completion of Intervention 6 Months | Change Between Control and ICT Groups | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Control Group (N = 38) | ICT Group (N = 50) | p-Value 1 | Control Group (N = 38) | p-Value 2 | ICT Group (N = 50) | p-Value 3 | Control Group (N = 38) | ICT Group (N = 50) | p-Value 4 | |
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||||
| Body mass index (BMI), kg/m2 | 25.3 ± 3.9 | 25.1 ± 4.3 | 0.787 a | 24.8 ± 3.9 | 0.008 c | 24.7 ± 4.1 | 0.088 c | −0.38 ± 0.87 | −0.39 ± 1.00 | 0.787 a |
| Male waist circumference, cm (n = 75) | 89.9 ± 9.4 | 89.1 ± 11.0 | 0.720 b | 86.7 ± 9.2 | <0.001 d | 86.2 ± 10.5 | <0.001 d | −3.2 ± 3.6 | −2.9 ± 3.8 | 0.683 b |
| Female waist circumference, cm (n = 13) | 85.5 ± 11.7 | 75.8 ± 6.6 | 0.239 b | 83.7 ± 11.6 | 0.076 d | 76.7 ± 11.0 | 0.496 d | −1.8 ± 2.3 | −1.5 ± 4.6 | 0.880 b |
| Systolic blood pressure, mmHg | 127.9 ± 19.2 | 124.3 ± 14.3 | 0.325 b | 125.6 ± 13.1 | 0.005 d | 121.7 ± 11.3 | 0.122 d | −2.24 ± 14.46 | −2.60 ± 12.62 | 0.896 b |
| Diastolic blood pressure, mmHg | 82.6 ± 13.1 | 77.9 ± 10.8 | 0.062 b | 77.8 ± 10.7 | <0.001 d | 74.1 ± 9.0 | 0.003 d | -4.74 ± 9.69 | −3.83 ± 9.26 | 0.645 b |
| Triglyceride (TG), mg/dL | 138.0 ± 93.3 | 148.3 ± 199.9 | 0.234 a | 119.2 ± 58.7 | 0.059 c | 128.6 ± 104.3 | 0.237c | −18.87 ± 56.45 | −19.67 ± 168.12 | 0.234 a |
| High-density lipoprotein (HDL) cholesterol, mg/dL | 58.9 ± 13.3 | 61.5 ± 17.0 | 0.438 a | 63.6 ± 16.9 | 0.008 c | 63.9 ± 16.0 | 0.032 d | 4.68 ± 9.954 | 2.4 3 ± 8.40 | 0.438 a |
| Low-density lipoprotein (LDL) cholesterol, mg/dL | 128.7 ± 29.8 | 124.1 ± 29.1 | 0.637 a | 134.0 ± 30.6 | 0.097 c | 124.1 ± 27.0 | 0.987 d | 5.32 ± 21.82 | −0.05 ± 24.92 | 0.637 a |
| Glycated hemoglobin A1c (HbA1c), % | 6.0 ± 0.9 | 5.7 ± 0.3 | 0.085 a | 5.8 ± 1.3 | 0.001 c | 5.4 ± 0.3 | <0.001 c | −0.18 ± 0.64 | −0.22 ± 0.21 | 0.085 a |
| Use of ICT Application to Monitor: | <1 Time/Month | 1–4 Times/Month | ≥5 Times/Month | Mean/Month | |
|---|---|---|---|---|---|
| Blood pressure (n = 38) | n (%) | 8 (21.1%) | 7 (18.4%) | 23 (60.5%) | 7.1 |
| Body weight (n = 47) | n (%) | 12 (25.5%) | 11 (23.4%) | 24 (51.1%) | 9.3 |
| Number of steps (n = 47) | n (%) | 0 | 10 (21.3%) | 37 (78.7%) | 15.1 |
| Measurement | Use of ICT Application to Register * | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Blood Pressure | Body Weight | Number of Steps | ||||||||
| Control n = 38 | <5 times n = 15 | ≥5 times n = 23 | Control n = 38 | <5 times n = 23 | ≥5 times n = 24 | Control n = 38 | <5 times n = 10 | ≥5 times n = 37 | ||
| Body mass index (BMI), kg/m2 | Mean | −0.4 | −0.1 | −0.8 | −0.4 | −0.2 | −0.7 | −0.4 | −0.1 | −0.6 |
| SD | ±0.9 | ±0.8 | ±1.1 | ±0.9 | ±0.9 | ±1.1 | ±0.9 | ±0.7 | ±1.1 | |
| p value | 0.007 | 0.053 | 0.093 | |||||||
| Systolic blood pressure, mmHg | Mean | −2.2 | −0.1 | -6.8 | −2.2 | −0.9 | −5 | −2.2 | 2.4 | −5.7 |
| SD | ±14.5 | ±12.9 | ±11.3 | ±14.5 | ±12.3 | ±12.9 | ±14.5 | ±12.6 | ±11.8 | |
| p value | 0.152 | 0.397 | 0.126 | |||||||
| Diastolic blood pressure, mmHg | Mean | −4.7 | −3.6 | −4.2 | −4.7 | −4.4 | −3 | −4.7 | −3.7 | −3.9 |
| SD | ±9.7 | ±9.3 | ±9.5 | ±9.7 | ±9.6 | ±8.9 | ±9.7 | ±7.8 | ±10.2 | |
| p value | 0.79 | 0.597 | 0.745 | |||||||
| Waist circumference, cm | Mean | −2.9 | −1.5 | −4.7 | −2.9 | −1.6 | −4.3 | −2.9 | −1.7 | −3.3 |
| SD | ±3.5 | ±3.4 | ±4.2 | ±3.5 | ±3.3 | ±4.4 | ±3.5 | ±2.7 | ±4.5 | |
| p value | 0.001 | 0.010 | 0.161 | |||||||
| Triglycerides, mg/dL | Mean | −0.4 | −0.1 | −0.8 | −0.4 | −0.2 | −0.7 | −0.4 | −0.1 | −0.6 |
| SD | ±0.9 | ±0.8 | ±1.1 | ±0.9 | ±0.9 | ±1.1 | ±0.9 | ±0.7 | ±1.1 | |
| p value | 0.007 | 0.053 | 0.093 | |||||||
| HDL cholesterol, mg/dL | Mean | −2.2 | −0.1 | −6.8 | −2.2 | −0.9 | −5 | −2.2 | 2.4 | −5.7 |
| SD | ±14.5 | ±12.9 | ±11.3 | ±14.5 | ±12.3 | ±12.9 | ±14.5 | ±12.6 | ±11.8 | |
| p value | 0.152 | 0.397 | 0.126 | |||||||
| LDL cholesterol, mg/dL | Mean | −4.7 | −3.6 | −4.2 | −4.7 | −4.4 | −3 | −4.7 | −3.7 | −3.9 |
| SD | ±9.7 | ±9.3 | ±9.5 | ±9.7 | ±9.6 | ±8.9 | ±9.7 | ±7.8 | ±10.2 | |
| p value | 0.79 | 0.597 | 0.745 | |||||||
| HbA1c, % | Mean | −2.9 | −1.5 | −4.7 | −2.9 | −1.6 | −4.3 | −2.9 | −1.7 | −3.3 |
| SD | ±3.5 | ±3.4 | ±4.2 | ±3.5 | ±3.3 | ±4.4 | ±3.5 | ±2.7 | ±4.5 | |
| p value | 0.001 | 0.010 | 0.161 | |||||||
| Indicator | ICT Group | Control Group | p-Value * |
|---|---|---|---|
| Body mass index | 31 (62.0%) | 24 (63.2%) | 0.912 |
| Waist circumference | 25 (50.0%) | 19 (50.0%) | 1.000 |
| Systolic blood pressure | 38 (76.0%) | 14 (36.8%) | 0.191 |
| Diastolic blood pressure | 44 (88.0%) | 29 (76.3%) | 0.149 |
| Triglycerides | 37 (74.0%) | 28 (73.7%) | 0.973 |
| HDL cholesterol | 47 (94.0%) | 37 (97.4%) | 0.452 |
| LDL cholesterol | 25 (50.0%) | 14 (36.8%) | 0.218 |
| HbA1c | 39 (78.0%) | 25 (65.8%) | 0.203 |
| Improvement of Lifestyle (n, %) | p-Value * | |||||
|---|---|---|---|---|---|---|
| (1) I am following a diet that is suitable for preventing lifestyle-related diseases. | ||||||
| Strongly agree | Agree | Neither | Disagree | Strongly disagree | 0.966 | |
| ICT group | 4 (9.8%) | 24 (58.5%) | 8 (19.5%) | 3 (7.3%) | 2 (4.9%) | |
| Control group | 3 (11.1%) | 15 (56.6%) | 6 (22.2%) | 3 (11.1%) | 0 | |
| (2) I regularly do exercise that is suitable for preventing lifestyle-related diseases. | ||||||
| Strongly agree | Agree | Neither | Disagree | Strongly disagree | 0.226 | |
| ICT group | 5 (12.2%) | 27 (65.9%) | 4 (9.8%) | 1 (2.4%) | 4 (9.8%) | |
| Control group | 3 (11.1%) | 13 (48.1%) | 5 (18.5%) | 5 (18.5%) | 1 (3.7%) | |
| (3) I know my average blood pressure. | ||||||
| Strongly agree | Agree | Neither | Disagree | Strongly disagree | 0.197 | |
| ICT group | 21 (51.2%) | 15 (36.6%) | 3 (7.3%) | 1 (2.4%) | 1 (2.4%) | |
| Control group | 8 (29.6%) | 17 (63.0%) | 1 (3.7%) | 0 | 1 (3.7%) | |
| (4)I know my average blood glucose level. | ||||||
| Strongly agree | Agree | Neither | Disagree | Strongly disagree | 0.980 | |
| ICT group | 7 (17.1%) | 10 (24.4) | 6 (14.6) | 10 (24.4) | 8 (19.5) | |
| Control group | 3 (11.1%) | 8 (29.6) | 6 (22.2) | 5 (18.5) | 5 (18.5) | |
| (5) I know my average body weight. | ||||||
| Strongly agree | Agree | Neither | Disagree | Strongly disagree | 0.188 | |
| ICT group | 25 (61.0%) | 14 (34.1%) | 0 | 1 (2.4%) | 1 (2.4%) | |
| Control group | 12 (44.4%) | 13 (48.1%) | 0 | 1 (3.7%) | 1 (3.7%) | |
| (6) I can judge when to start clinical treatment for diabetes, hypertension, dyslipidemia. | ||||||
| Very well | Well | Neither | Not well | Badly/Not at all | 0.078 | |
| ICT group | 4 (9.8%) | 12 (29.3%) | 12 (29.3%) | 3 (7.3%) | 10 (24.3%) | |
| Control group | 10 (37.0%) | 5 (18.5%) | 4 (14.8%) | 4 (14.8%) | 4 (14.8%) | |
| (7) I rate the effectiveness of the program on continuous lifestyle improvement as | ||||||
| Very effective | Effective | Neither | Somewhat ineffective | Not effective at all | 0.399 | |
| ICT group | 1 (2.4%) | 21 (51.2%) | 8 (19.5%) | 2 (4.9%) | 9 (22.0%) | |
| Control group | 2 (7.4%) | 11 (40.7%) | 2 (7.4%) | 2 (7.4%) | 10 (37.0%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takeyama, N.; Moriyama, M.; Kazawa, K.; Steenkamp, M.; Rahman, M.M. A Health Guidance App to Improve Motivation, Adherence to Lifestyle Changes and Indicators of Metabolic Disturbances among Japanese Civil Servants. Int. J. Environ. Res. Public Health 2020, 17, 8147. https://doi.org/10.3390/ijerph17218147
Takeyama N, Moriyama M, Kazawa K, Steenkamp M, Rahman MM. A Health Guidance App to Improve Motivation, Adherence to Lifestyle Changes and Indicators of Metabolic Disturbances among Japanese Civil Servants. International Journal of Environmental Research and Public Health. 2020; 17(21):8147. https://doi.org/10.3390/ijerph17218147
Chicago/Turabian StyleTakeyama, Naoko, Michiko Moriyama, Kana Kazawa, Malinda Steenkamp, and Md Moshiur Rahman. 2020. "A Health Guidance App to Improve Motivation, Adherence to Lifestyle Changes and Indicators of Metabolic Disturbances among Japanese Civil Servants" International Journal of Environmental Research and Public Health 17, no. 21: 8147. https://doi.org/10.3390/ijerph17218147
APA StyleTakeyama, N., Moriyama, M., Kazawa, K., Steenkamp, M., & Rahman, M. M. (2020). A Health Guidance App to Improve Motivation, Adherence to Lifestyle Changes and Indicators of Metabolic Disturbances among Japanese Civil Servants. International Journal of Environmental Research and Public Health, 17(21), 8147. https://doi.org/10.3390/ijerph17218147






