Alcohol Control Policy in Europe: Overview and Exemplary Countries
Abstract
:1. Introduction
2. Materials and Methods
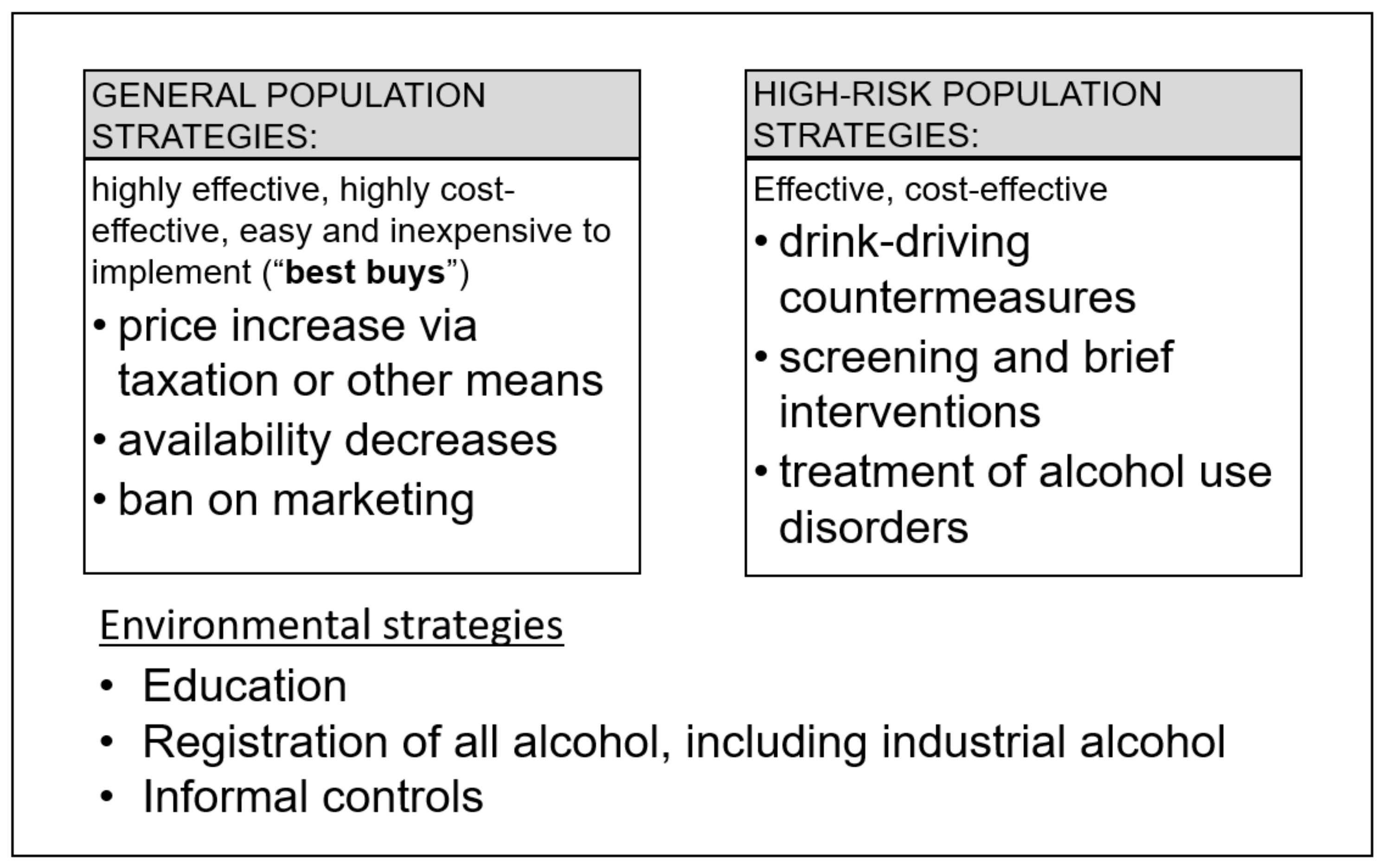
- Alcohol control policies were used as defined by Babor and colleagues [17] as public policies [19] (i.e., authoritative decisions made by governments through laws, rules, and regulations, which pertain to the relation between alcohol, health, and social welfare). The word authoritative indicates that the decisions arose from the legitimate purview of legislators and other public interest group officials, not from private industry or related advocacy groups. It has become customary in the field to distinguish 10 broad categories and areas of policies based on the already mentioned WHO Global Strategy to Reduce the Harmful Use of Alcohol [9]: leadership, awareness, and commitment (usually measured via national alcohol plans); health services response; community action; drinking and driving policies and countermeasures; regulating availability of alcoholic beverages; regulating marketing of alcoholic beverages; pricing policies; reducing the negative consequences of drinking and alcohol intoxication; reducing the public health impact of illicit alcohol and informally produced alcohol; and monitoring and surveillance (for underlying principles in formulating policies, see [20]). Empirically, the so-called “best buys” of the WHO ([21], which comprise increases in price for alcoholic beverages via taxation or other pricing policies, reduction of availability of alcoholic beverages, and bans on advertising and marketing) have been found to be the most effective and cost-effective alcohol policies to reduce health burden [17,22], albeit with different timeframes of impact (taxation and availability tend to include immediate effects on consumption and harm following implementation: [23,24,25]). The three “best buys” have been highlighted in the upper left-hand box of Figure 1.
- Europe was defined here as being equivalent to the WHO European Region, which includes countries that are geographically located in Asia [26]. We chose this definition because alcohol control policies are in part impacted by the WHO regions and, thus, to reach our objectives, it makes sense to use this broader definition.
- Best practices were identified by their proven ability to reduce alcohol-attributable burden of disease and injuries, and reported by their effects on mortality and disability-adjusted life years (see [3]; for underlying concepts and definitions, see [27,28,29]). Obviously, the three “best buys”, if implemented at a sufficiently high level (for instance, taxation increases, which markedly reduce the affordability of alcoholic beverages), would meet the threshold for best practices.
3. Results
3.1. Alcohol Control Policies in Europe During the Past 10 Years: An Overview
3.2. Identifying Best Practices
4. Discussion
4.1. Limitations
4.2. Where Should We Go?
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- GBD 2017 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef] [Green Version]
- Rehm, J.; Imtiaz, S. Alcohol consumption as a risk factor for global burden of disease. A narrative review. Subst. Abus. Treat. Prev. Policy 2016, 11, 37. [Google Scholar] [CrossRef] [Green Version]
- Shield, K.D.; Manthey, J.; Rylett, M.; Probst, C.; Wettlaufer, A.; Parry, C.D.H.; Rehm, J. National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: A comparative risk assessment study. Lancet Public Health 2020, 5, E51–E61. [Google Scholar] [CrossRef] [Green Version]
- Rehm, J.; Casswell, S.; Manthey, J.; Room, R.; Shield, K. Reducing the harmful use of alcohol: Have international targets been met? Eur. J. Risk Regul. 2020, in press. [Google Scholar]
- Manthey, J.; Shield, K.D.; Rylett, M.; Hasan, O.S.M.; Probst, C.; Rehm, J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: A modelling study. Lancet 2019, 393, 2493–2502. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Alcohol and Health 2018; World Health Organization: Geneva, Switzerland, 2018; Available online: https://www.who.int/substance_abuse/publications/global_alcohol_report/en/ (accessed on 20 May 2019).
- World Health Organization Regional Office for Europe. European Charter on Alcohol, 1995; WHO: Copenhagen, Denmark, 2020; Available online: https://www.euro.who.int/en/health-topics/disease-prevention/alcohol-use/publications/pre-2009/european-charter-on-alcohol,-1995 (accessed on 30 August 2020).
- World Health Organization Regional Office for Europe. Declaration on Young People and Alcohol; WHO: Copenhagen, Denmark, 2020; Available online: https://www.euro.who.int/en/publications/policy-documents/declaration-on-young-people-and-alcohol (accessed on 30 August 2020).
- World Health Organization. Global Strategy to Reduce the Harmful Use of Alcohol; WHO: Geneva, Switzerland, 2010; Available online: https://www.who.int/substance_abuse/activities/gsrhua/en/ (accessed on 27 August 2020).
- Rehm, J.; Crepault, J.F.; Wettlaufer, A.; Manthey, J.; Shield, K. What is the best indicator of the harmful use of alcohol? A narrative review. Drug Alcohol Rev. 2020, 39, 624–631. [Google Scholar] [CrossRef]
- World Health Organization. Target 2: Reduce Harmful Use of Alcohol; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/nmh/ncd-tools/target2/en/ (accessed on 27 August 2020).
- Probst, C.; Manthey, J.; Neufeld, M.; Rehm, J.; Breda, J.; Rakovac, I.; Ferreira-Borges, C. Meeting the Global NCD Target of at Least 10% Relative Reduction in the Harmful Use of Alcohol: Is the WHO European Region on Track? Int. J. Environ. Res. Public Health 2020, 17, 3423. [Google Scholar]
- Rehm, J.; Manthey, J.; Shield, K.D.; Ferreira-Borges, C. Trends in substance use and in the attributable burden of disease and mortality in the WHO European Region, 2010–2016. Eur. J. Public Health 2019, 29, 723–728. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Journal of Environmental Research and Public Health (IJERPH). Special Issue: “Alcohol Control Policy and Health in Europe”. Available online: https://www.mdpi.com/journal/ijerph/special_issues/alcohol_policy (accessed on 25 August 2020).
- World Health Organization Regional Office for Europe. Status Report on Alcohol Consumption, Harm and Policy Responses in 30 European Countries; WHO Regional Office for Europe: Copenhagen, Denmark, 2019. [Google Scholar]
- World Health Organization Regional Office for Europe. Policy in Action: A Tool for Measuring Alcohol Policy Implementation. Available online: https://www.euro.who.int/__data/assets/pdf_file/0006/339837/WHO_Policy-in-Action_indh_VII-2.pdf?ua=1 (accessed on 25 August 2020).
- Babor, T.F.; Caetano, R.; Casswell, S.; Edwards, G.; Giesbrecht, N.; Graham, K.; Grube, J.; Gruenewald, P.; Hill, L.; Holder, H.; et al. Alcohol: No Ordinary Commodity: Research and Public Policy, 2nd ed.; Oxford University Press: Oxford, UK, 2010. [Google Scholar]
- Siegfried, N.; Parry, C. Do alcohol control policies work? An umbrella review and quality assessment of systematic reviews of alcohol control interventions (2006–2017). PLoS ONE 2019, 14, e0214865. [Google Scholar]
- Longest, B.B. Health Policymaking in the United States; Health Administration Press: Chicago, IL, USA, 1998. [Google Scholar]
- Rehm, J.; Crépault, J.-F.; Hasan, O.S.M.; Lachenmeier, D.W.; Room, R.; Sornpaisarn, B. Regulatory Policies for Alcohol, other Psychoactive Substances and Addictive Behaviours: The Role of Level of Use and Potency. A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 3749. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. ‘Best buys’ and other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases: Updated (2017) Appendix 3 of the Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; WHO: Geneva, Switzerland, 2017; Available online: https://www.who.int/ncds/management/WHO_Appendix_BestBuys_LS.pdf (accessed on 21 June 2018).
- Chisholm, D.; Moro, D.; Bertram, M.; Pretorius, C.; Gmel, G.; Shield, K.; Rehm, J. Are the “Best Buys” for Alcohol Control Still Valid? An Update on the Comparative Cost-Effectiveness of Alcohol Control Strategies at the Global Level. J. Stud. Alcohol Drugs 2018, 79, 514–522. [Google Scholar]
- Sornpaisarn, B.; Shield, K.D.; Österberg, E.; Rehm, J. Resource Tool on Alcohol Taxation and Pricing Policies; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Markowitz, S.; Ding, C. Light, Moderate, and Heavy Drinking. In Handbook of Labor, Human Resources and Population Economics; Zimmermann, K.F., Ed.; Springer International Publishing: Cham, Switzerland, 2020; pp. 1–18. [Google Scholar] [CrossRef]
- Sherk, A.; Stockwell, T.; Chikritzhs, T.; Andréasson, S.; Angus, C.; Gripenberg, J.; Holder, H.; Holmes, J.; Mäkelä, P.; Mills, M. Alcohol consumption and the physical availability of take-away alcohol: Systematic reviews and meta-analyses of the days and hours of sale and outlet density. J. Stud. Alcohol Drugs 2018, 79, 58–67. [Google Scholar]
- World Health Organization Regional Office for Europe. Countries. Available online: https://www.euro.who.int/en/countries (accessed on 25 August 2020).
- Rehm, J.; Gmel, G.E.; Gmel, G.; Hasan, O.S.M.; Imtiaz, S.; Popova, S.; Probst, C.; Roerecke, M.; Room, R.; Samokhvalov, A.V.; et al. The relationship between different dimensions of alcohol use and the burden of disease-an update. Addiction 2017, 112, 968–1001. [Google Scholar] [CrossRef] [Green Version]
- Rehm, J.; Monteiro, M.; Room, R.; Gmel, G.; Jernigan, D.; Frick, U.; Graham, K. Steps towards constructing a global comparative risk analysis for alcohol consumption: Determining indicators and empirical weights for patterns of drinking, deciding about theoretical minimum, and dealing with different consequences. Eur. Addict. Res. 2001, 7, 138–147. [Google Scholar] [CrossRef] [Green Version]
- Rehm, J.; Room, R.; Monteiro, M.; Gmel, G.; Graham, K.; Rehn, T. Comparative Quantification of Health Risks. In Global and Regional Burden of Disease Attributable to Selected Major Risk Factors; World Health Organization: Geneva, Switzerland, 2004; Volume 1, pp. 959–1108. [Google Scholar]
- Miščikienė, L.; Midttun, N.G.; Galkus, L.; Belian, G.; Petkevičienė, J.; Vaitkevičiūtė, J.; Štelemėkas, M. Review of the Lithuanian Alcohol Control Legislation in 1990–2020. Int. J. Environ. Res. Public Health 2020, 17, 3454. [Google Scholar] [CrossRef]
- Lachenmeier, D.W. Is There a Need for Alcohol Policy to Mitigate Metal Contamination in Unrecorded Fruit Spirits? Int. J. Environ. Res. Public Health 2020, 17, 2452. [Google Scholar]
- Kilian, C.; Manthey, J.; Moskalewicz, J.; Sieroslawski, J.; Rehm, J. How Attitudes toward Alcohol Policies Differ across European Countries: Evidence from the Standardized European Alcohol Survey (SEAS). Int. J. Environ. Res. Public Health 2019, 16, 4461. [Google Scholar] [CrossRef] [Green Version]
- Neufeld, M.; Bunova, A.; Gornyi, B.; Ferreira-Borges, C.; Gerber, A.; Khaltourina, D.; Yurasova, E.; Rehm, J. Russia’s national concept to reduce alcohol abuse and alcohol dependence in the population 2010-2020: Which policy targets have been achieved? Int. J. Environ. Res. Public Health 2020, in press. [Google Scholar]
- Neufeld, M.; Ferreira-Borges, C.; Rehm, J. Implementing health warnings on alcoholic beverages—On the leading role of countries of the Commonwealth of Independent States. Int. J. Environ. Res. Public Health 2020. (under review). [Google Scholar]
- Rice, P. Plus ça change, plus c’est la même chose: A Review of Recent Alcohol Policy Developments in Europe. Alcohol Alcohol. 2019, 54, 123–127. [Google Scholar] [CrossRef]
- Neufeld, M.; Bobrova, A.; Davletov, K.; Štelemėkas, M.; Stoppel, R.; Ferreira-Borges, C.; Breda, J.; Rehm, J. Alcohol control policies in Former Soviet Union countries—A narrative review of a series of natural experiments in implementing the “best buys”. Drug Alcohol Rev. 2020, in press. [Google Scholar]
- Jernigan, D.; Trangenstein, P. Global Developments in Alcohol Policies: Progress in Implementation of the WHO Global Strategy to Reduce the Harmful Use of Alcohol since 2010. Background Paper Developed for the WHO Forum on Alcohol, Drugs and Addictive Behaviours, 26–28 June 2017; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/substance_abuse/activities/fadab/msb_adab_gas_progress_report.pdf?ua=1 (accessed on 26 August 2020).
- World Health Organization Regional Office for Europe. Alcohol Pricing in the WHO European Region: Update Report on the Evidence and Recommended Policy Actions; WHO: Copenhagen, Denmark, 2020; Available online: https://www.euro.who.int/en/health-topics/disease-prevention/alcohol-use/publications/frequently-asked-questions-faq-about-alcohol-and-covid-19/alcohol-pricing-in-the-who-european-region-update-report-on-the-evidence-and-recommended-policy-actions-2020 (accessed on 30 August 2020).
- Seabrook, R. A new measure of alcohol affordability for the UK. Alcohol Alcohol. 2010, 45, 581–585. [Google Scholar] [CrossRef] [Green Version]
- Rabinovich, L.; Brutscher, P.B.; de Vries, H.; Tiessen, J.; Clift, J.; Reding, A. The Affordability of Alcoholic Beverages in the European Union Understanding the Link between Alcohol Affordability, Consumption and Harms; Prepared for the European Commission; RAND Europe: Cambridge, UK, 2009; Available online: https://ec.europa.eu/health/ph_determinants/life_style/alcohol/documents/alcohol_rand_en.pdf (accessed on 26 August 2020).
- Blecher, E.; Liber, A.; Van Walbeek, C.; Rossouw, L. An international analysis of the price and affordability of beer. PLoS ONE 2018, 13, e0208831. [Google Scholar] [CrossRef]
- Gil, A.; Khaltourina, D.; Korotaev, A. Alcohol consumption in Russia: Affordability of alcohol, changes and effects of alcohol control policy and future prospects. In Changes in Alcohol Affordability and Availability. Twenty Years of Transition in Eastern Europe; Österberg, J.M.E., Ed.; National Institute for Health and Welfare: Helsinki, Finland, 2016; pp. 18–50. [Google Scholar]
- Lithuanian Department of Statistics. Official Statistics Portal. Available online: https://osp.stat.gov.lt/statistiniu-rodikliu-analize#/ (accessed on 26 August 2020).
- Thompson, K.; Stockwell, T.; Wettlaufer, A.; Giesbrecht, N.; Thomas, G. Minimum alcohol pricing policies in practice: A critical examination of implementation in Canada. J. Public Health Policy 2017, 38, 39–57. [Google Scholar] [CrossRef]
- Scottish Government gov.scot. Policy: Alcohol and Drugs. Available online: https://www.gov.scot/policies/alcohol-and-drugs/minimum-unit-pricing/ (accessed on 27 August 2020).
- Boniface, S.; Scannell, J.W.; Marlow, S. Evidence for the effectiveness of minimum pricing of alcohol: A systematic review and assessment using the Bradford Hill criteria for causality. BMJ Open 2017, 7, e013497. [Google Scholar] [CrossRef]
- O’Donnell, A.; Anderson, P.; Jané-Llopis, E.; Manthey, J.; Kaner, E.; Rehm, J. Immediate impact of minimum unit pricing on alcohol purchases in Scotland: Controlled interrupted time series analysis for 2015–2018. BMJ 2019, 366, l5274. [Google Scholar] [CrossRef] [Green Version]
- Angus, C.; Holmes, J.; Maheswaran, R.; Green, M.A.; Meier, P.; Brennan, A. Mapping Patterns and Trends in the Spatial Availability of Alcohol Using Low-Level Geographic Data: A Case Study in England 2003–2013. Int. J. Environ. Res. Public Health 2017, 14, 406. [Google Scholar] [CrossRef] [Green Version]
- Wicki, M.; Bertholet, N.; Gmel, G. Estimated changes in hospital admissions for alcohol intoxication after partial bans on off-premises sales of alcoholic beverages in the canton of Vaud, Switzerland: An interrupted time–series analysis. Addiction 2020, 115, 1459–1469. [Google Scholar] [CrossRef]
- Mobilizing Community for Responsibility towards Alcohol (MOSA). Alcohol Policy in Slovenia. 2020. Available online: http://www.infomosa.si/en/facts/alcohol-policy-in-slovenia.html (accessed on 30 August 2020).
- Room, R.; Bloomfield, K.; Gmel, G.; Grittner, U.; Gustafsson, N.-K.; Mäkelä, P.; Österberg, E.; Ramstedt, M.; Rehm, J.; Wicki, M. What happened to alcohol consumption and problems in the Nordic countries when alcohol taxes were decreased and borders opened? Int. J. Alcohol Drug Res. 2013, 2, 77–87. [Google Scholar] [CrossRef] [Green Version]
- Rehm, J.; Štelemėkas, M.; Badaras, R. Research protocol to evaluate the effects of alcohol policy changes in Lithuania. Alcohol Alcohol. 2019, 54, 112–118. [Google Scholar] [CrossRef]
- Pellechia, T. Online Alcohol Sales Grew In 2019, Yet All Is Not Rosy; Forbes: Jersey City, NJ, USA, 2020; Available online: https://www.forbes.com/sites/thomaspellechia/2020/01/18/2019-online-beverage-alcohol-sales-grewyet-all-is-not-rosy/#3968c68a1018 (accessed on 28 August 2020).
- Rehm, J.; Kilian, C.; Ferreira-Borges, C.; Jernigan, D.; Monteiro, M.; Parry, C.D.; Sanchez, Z.M.; Manthey, J. Alcohol use in times of the COVID 19: Implications for monitoring and policy. Drug Alcohol Rev. 2020, 39, 301–304. [Google Scholar] [CrossRef]
- Monteiro, M.G.; Rehm, J.; Duennbier, M. Alcohol Policy and Coronavirus: An Open Research Agenda. J. Stud. Alcohol Drugs 2020, 81, 297–299. [Google Scholar] [CrossRef]
- Carah, N.; Brodmerkel, S. Alcohol marketing in the era of digital media platforms. J. Stud. Alcohol Drugs 2020, in press. [Google Scholar]
- Carah, N. Alcohol corporations and marketing in social media. In Youth Drinking Cultures in a Digital World: Alcohol, Social Media and Cultures of Intoxication; Lyons, A., McCreanor, T., Goodwi, I., Barnes, H.M., Eds.; Routledge: London, UK, 2017; pp. 115–131. [Google Scholar]
- World Health Organization Regional Office for Europe. Monitoring and Restricting Digital Marketing of Unhealthy Products to Children and Adolescents; WHO: Moscow, Russia, 2019; Available online: https://www.euro.who.int/__data/assets/pdf_file/0008/396764/Online-version_Digital-Mktg_March2019.pdf (accessed on 30 August 2020).
- Kelsey, J. How Might Digital Trade Agreements Constrain Regulatory Autonomy: The Case of Regulating Alcohol Marketing in the Digital Age. N. Z. Univ. Law Rev. 2020, 29, 153–179. [Google Scholar]
- Rehm, J.; Anderson, P.; Manthey, J.; Shield, K.D.; Struzzo, P.; Wojnar, M.; Gual, A. Alcohol Use Disorders in Primary Health Care: What Do We Know and Where Do We Go? Alcohol Alcohol. 2016, 51, 422–427. [Google Scholar] [CrossRef] [Green Version]
- Scheideler, J.K.; Klein, W.M.P. Awareness of the Link between Alcohol Consumption and Cancer across the World: A Review. Cancer Epidemiol. Biomark. Prev. 2018, 27, 429–437. [Google Scholar] [CrossRef] [Green Version]
- Neufeld, M.; Rehm, J. Effectiveness of policy changes to reduce harm from unrecorded alcohol in Russia between 2005 and now. Int. J. Drug Policy 2018, 51, 1–9. [Google Scholar] [CrossRef]
- Wagenaar, A.C.; Salois, M.J.; Komro, K.A. Effects of beverage alcohol price and tax levels on drinking: A meta-analysis of 1003 estimates from 112 studies. Addiction 2009, 104, 179–190. [Google Scholar] [CrossRef]
- Wagenaar, A.C.; Tobler, A.L.; Komro, K.A. Effects of alcohol tax price policies on morbidity and mortality: A systematic review. Am. J. Public Health 2010, 100, 2270–2278. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for Europe. Alcohol Policy Impact Case Study. The Effects of Alcohol Control Measures on Mortality and Life Expectancy in the Russian Federation; WHO Regional Office for Europe: Copenhagen, Denmark, 2019; Available online: http://www.euro.who.int/en/health-topics/disease-prevention/alcohol-use/publications/2019/alcohol-policy-impact-case-study-the-effects-of-alcohol-control-measures-on-mortality-and-life-expectancy-in-the-russian-federation-2019 (accessed on 23 April 2020).
- Neufeld, M.; Ferreira-Borges, C.; Gil, A.; Manthey, J.; Rehm, J. Alcohol policy has saved lives in the Russian Federation. Int. J. Drug Policy 2020, 80, 102636. [Google Scholar] [CrossRef]
- Štelemėkas, M.; Manthey, J.; Badaras, R.; Casswell, S.; Ferreira-Borges, C.; Kalėdienė, R.; Lange, S.; Neufeld, M.; Petkevičienė, J.; Radišauskas, R.; et al. Alcohol control policy measures and all-cause mortality in Lithuania: An interrupted time-series analyses. 2020; (submitted). [Google Scholar]
- Nemtsov, A.; Neufeld, M.; Rehm, J. Are Trends in Alcohol Consumption and Cause-Specific Mortality in Russia Between 1990 and 2017 the Result of Alcohol Policy Measures? J. Stud. Alcohol Drugs 2019, 80, 489–498. [Google Scholar] [CrossRef]
- Nemtsov, A.V. A Contemporary History of Alcohol in Russia; Södertörns Högskola: Stockholm, Sweden, 2011. [Google Scholar]
- Neufeld, M.; Rehm, J. Alcohol consumption and mortality in Russia since 2000: Are there any changes following the alcohol policy changes starting in 2006? Alcohol Alcohol. 2013, 48, 222–230. [Google Scholar] [CrossRef]
- Rehm, J.; Manthey, J.; Lange, S.; Badaras, R.; Zurlyte, I.; Passmore, J.; Breda, J.; Ferreira-Borges, C.; Štelemėkas, M. Alcohol control policy and changes in alcohol-related traffic harm. Addiction 2020, 115, 655–665. [Google Scholar] [CrossRef] [Green Version]
- Lachenmeier, D.W.; Gmel, G.; Rehm, J. Unrecorded alcohol consumption. In Alcohol: Science, Policy, and Public Health; Boyle, P., Boffetta, P., Lowenfels, A.B., Burns, H., Brawley, O., Zatonski, W., Rehm, J., Eds.; Oxford University Press: Oxford, UK, 2013; pp. 132–142. [Google Scholar]
- Rehm, J.; Kailasapillai, S.; Larsen, E.; Rehm, M.X.; Samokhvalov, A.V.; Shield, K.D.; Roerecke, M.; Lachenmeier, D.W. A systematic review of the epidemiology of unrecorded alcohol consumption and the chemical composition of unrecorded alcohol. Addiction 2014, 109, 880–893. [Google Scholar] [CrossRef] [PubMed]
- Lachenmeier, D.W.; Neufeld, M.; Rehm, J. The impact of unrecorded alcohol use on health—What do we know in 2020? J. Stud. Alcohol Drugs 2020. in review. [Google Scholar]
- Neufeld, M.; Lachenmeier, D.W.; Ferreira-Borges, C.; Rehm, J. Is Alcohol an “Essential Good” during COVID-19? Yes, but Only as a Disinfectant! Alcohol Clin. Exp. Res. 2020. [Google Scholar] [CrossRef]
- Shadish, W.R.; Cook, T.D.; Campbell, D.T. Experimental and Quasi-Experimental Designs for Generalized Causal Inference; Houghton Mifflin Company: New York, NY, USA, 2002. [Google Scholar]
- Rovira, P.; Kilian, C.; Neufeld, M.; Rumgay, H.; Soerjomataram, I.; Ferreira-Borges, C.; Shield, K.D.; Sornpaisarn, B.; Rehm, J. Fewer cancer cases in four countries of the WHO European Region in 2018 through increased alcohol excise taxation: A modelling study. Eur. Addict. Res. 2020. [Google Scholar] [CrossRef]
- WHO Framework Convention on Tobacco Control (FCTC). Home Page; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/fctc/en/ (accessed on 28 August 2020).
- International Agency for Research on Cancer. Monographs on the Evaluation of Carcinogenic Risks to Humans: Vol. 42. Alcohol Drinking; International Agency for Research on Cancer: Lyon, France, 1988; pp. 1–416. [Google Scholar]
- Jané-Llopis, E.; Kokole, D.; Neufeld, M.; Hasan, O.S.M.; Rehm, J. What is the Current Alcohol Labelling Practice in the WHO European Region and what are Barriers and Facilitators to Development and Implementation of Alcohol Labelling policy? WHO Regional Office for Europe: Copenhagen, Denmark, 2020. [Google Scholar]
- Buykx, P.; Gilligan, C.; Ward, B.; Kippen, R.; Chapman, K. Public support for alcohol policies associated with knowledge of cancer risk. Int. J. Drug Policy 2015, 26, 371–379. [Google Scholar] [CrossRef]
- Bowden, J.A.; Delfabbro, P.; Room, R.; Miller, C.L.; Wilson, C. Alcohol consumption and NHMRC guidelines: Has the message got out, are people conforming and are they aware that alcohol causes cancer? Aust. N. Z. J. Public Health 2014, 38, 66–72. [Google Scholar] [CrossRef]
- Neufeld, M.; Rehm, J. Newest policy developments regarding surrogate alcohol consumption in Russia. Int. J. Drug Policy 2018, 54, 58–59. [Google Scholar] [CrossRef]
- Euronews.com. Will a Booze Tax War in the Baltics Leave Latvia & Estonia with a Bad Hangover? Available online: https://www.euronews.com/2019/07/27/money-before-man-baltic-booze-war-threatens-latvia-estonia-with-health-hangover (accessed on 28 August 2020).
- Frank, R. The Darwin Economy: Liberty, Competition, and the Common Good; Princeton University Press: Princeton, NJ, USA, 2011. [Google Scholar]
- World Health Organization. Executive Board, 146th Session, Jan 24,2020. International mechanisms for alcohol control (provisional agenda item 7.2): Accelerating action to reduce the harmful use of alcohol. In Draft Decision Proposed by Bangladesh, Bhutan, India, Indonesia, Islamic Republic of Iran, Philippines, Russian Federation, Sierra Leone, Sri Lanka, Thailand and Viet Nam; WHO: Geneva, Switzerland, 4 November 2020; Available online: https://apps.who.int/gb/ebwha/pdf_files/EB146/B146_CONF1Rev1-en.pdf (accessed on 4 November 2020).
- Casswell, S.; Rehm, J. Reduction in global alcohol-attributable harm unlikely after setback at WHO Executive Board. Lancet 2020, 395, 1020–1021. [Google Scholar] [CrossRef]
- Movendi International. Where Next for the Global Governance of Alcohol and Public Health? Available online: https://movendi.ngo/blog/2020/07/27/where-next-for-the-global-governance-of-alcohol-and-public-health/ (accessed on 30 August 2020).
- Official Journal of the European Union. Council Conclusions on an EU Strategy on the Reduction of Alcohol-Related Harm (2015/C 418/03) 16.12.2015. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:52015XG1216(01)&from=EN (accessed on 29 August 2020).
- Official Journal of the European Union. Opinion of the European Committee of the Regions—The Need for and Way towards an EU Strategy on Alcohol-Related Issues (2017/C 207/12). C 207/61. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:52016IR1831&rid=10 (accessed on 28 September 2020).
- De Coninck, P.; Gilmore, I. Long overdue: A fresh start for EU policy on alcohol and health. Lancet 2020, 395, 10–13. [Google Scholar] [CrossRef]
- COWI Consortium for DG Health and Consumers of the European Commission. Assessment of the Added Value of the EU Strategy to Support Member States in Reducing Alcohol-Related Harm. Available online: https://ec.europa.eu/health/sites/health/files/alcohol/docs/report_assessment_eu_alcohol_strategy_2012_en.pdf (accessed on 2 September 2020).
- World Health Organization Regional Office for Europe. Action Plan on Youth Drinking and on Heavy Episodic Drinking (Binge Drinking) (2014–2016) Progress Evaluation Report (2019). Available online: https://www.euro.who.int/en/health-topics/disease-prevention/alcohol-use/publications/2019/action-plan-on-youth-drinking-and-on-heavy-episodic-drinking-binge-drinking-20142016-progress-evaluation-report-2019 (accessed on 2 September 2020).
- Gornall, J. Europe under the influence. BMJ 2014, 348, g1166. [Google Scholar] [CrossRef]
- Nutt, D. Drugs without the Hot Air: Making Sense of Legal and Illegal Drugs; UIT Cambridge Ltd.: Cambridge, UK, 2020. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berdzuli, N.; Ferreira-Borges, C.; Gual, A.; Rehm, J. Alcohol Control Policy in Europe: Overview and Exemplary Countries. Int. J. Environ. Res. Public Health 2020, 17, 8162. https://doi.org/10.3390/ijerph17218162
Berdzuli N, Ferreira-Borges C, Gual A, Rehm J. Alcohol Control Policy in Europe: Overview and Exemplary Countries. International Journal of Environmental Research and Public Health. 2020; 17(21):8162. https://doi.org/10.3390/ijerph17218162
Chicago/Turabian StyleBerdzuli, Nino, Carina Ferreira-Borges, Antoni Gual, and Jürgen Rehm. 2020. "Alcohol Control Policy in Europe: Overview and Exemplary Countries" International Journal of Environmental Research and Public Health 17, no. 21: 8162. https://doi.org/10.3390/ijerph17218162
APA StyleBerdzuli, N., Ferreira-Borges, C., Gual, A., & Rehm, J. (2020). Alcohol Control Policy in Europe: Overview and Exemplary Countries. International Journal of Environmental Research and Public Health, 17(21), 8162. https://doi.org/10.3390/ijerph17218162





