IgG4-Related Disease of the Oral Cavity. Case Series from a Large Single-Center Cohort of Italian Patients
Abstract
:1. Introduction
2. Methods
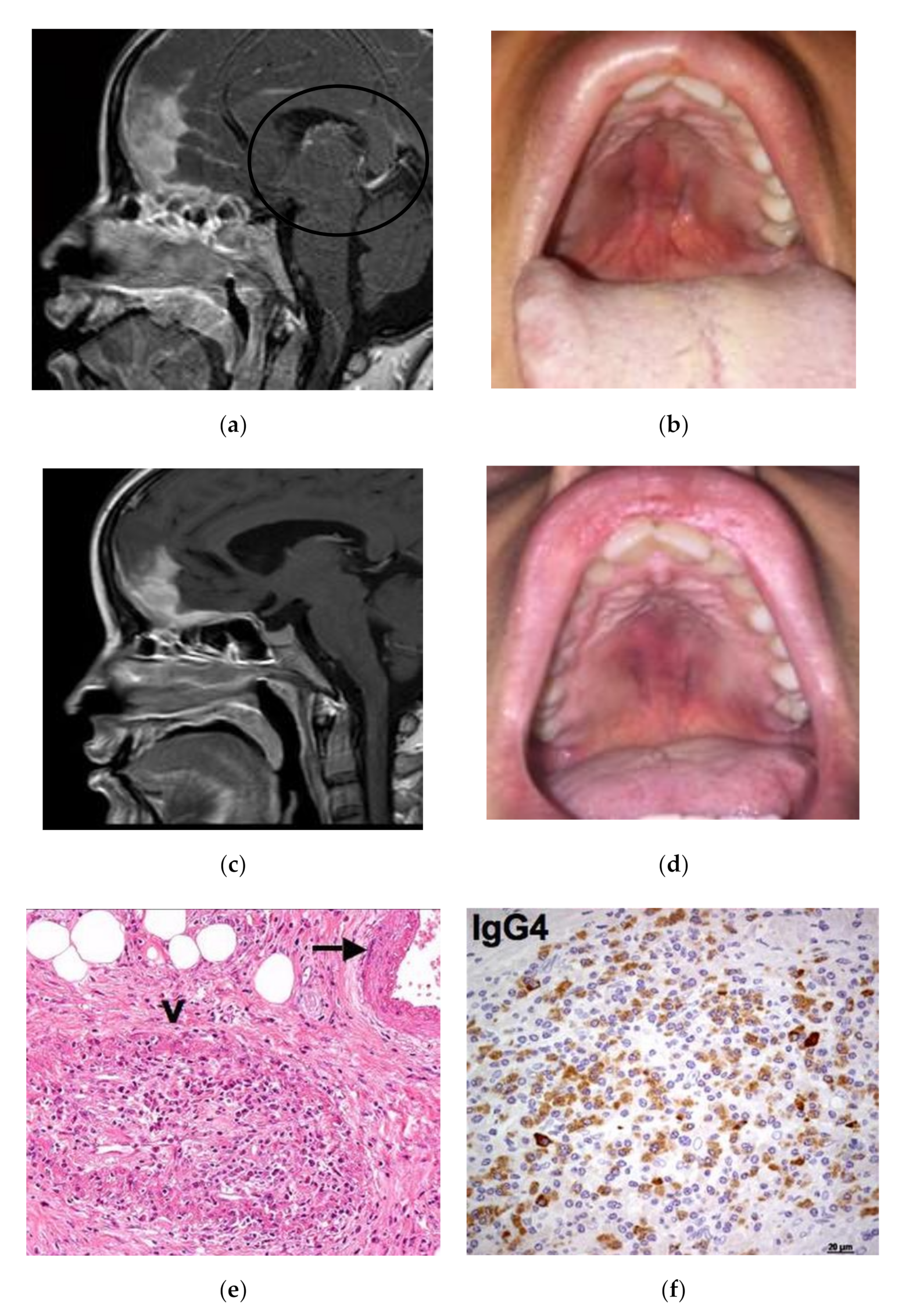
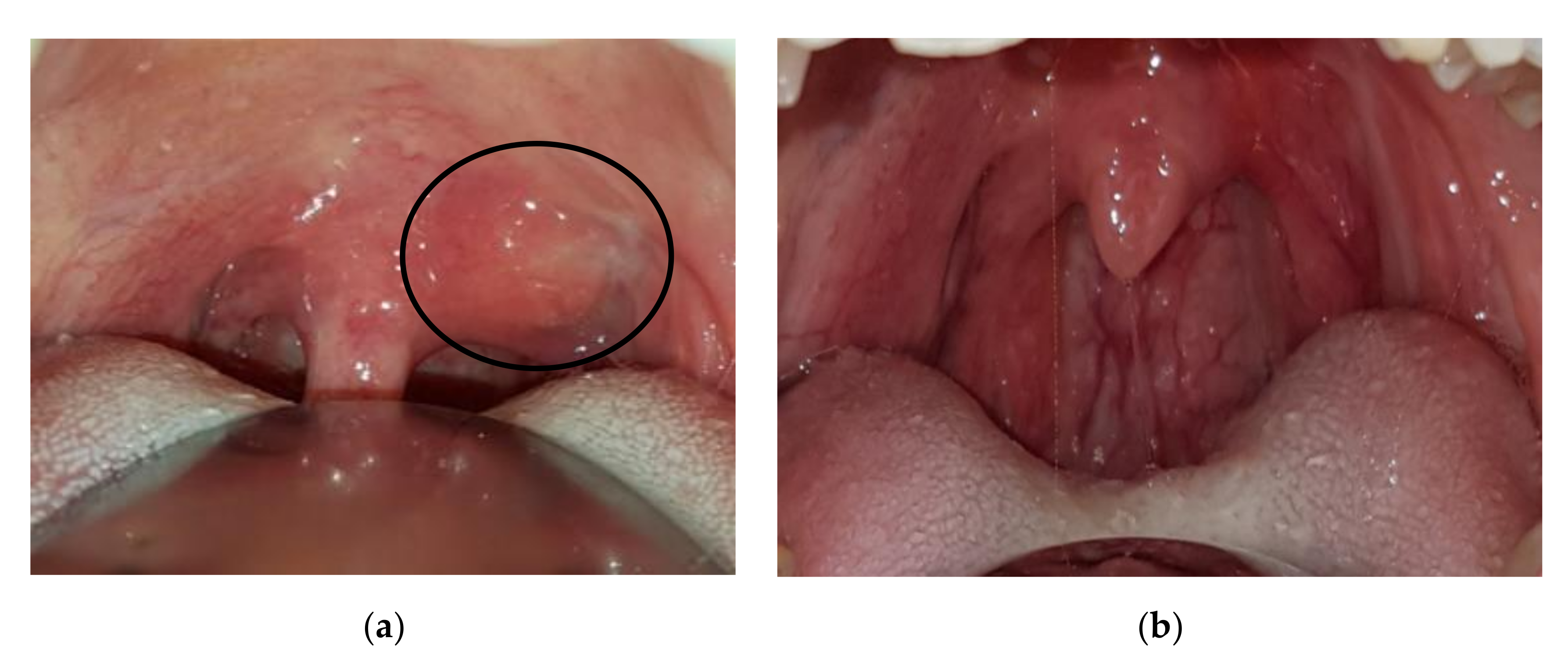
3. Case Presentation
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lanzillotta, M.; Mancuso, G.; Della-Torre, E. Advances in the diagnosis and management of IgG4 related disease. BMJ 2020, 369, m1067. [Google Scholar] [CrossRef] [PubMed]
- Bledsoe, J.R.; Della-Torre, E.; Rovati, L.; Deshpande, V. IgG4-related disease: Review of the histopathologic features, differential diagnosis, and therapeutic approach. APMIS 2018, 126, 459–476. [Google Scholar] [CrossRef] [PubMed]
- Della-Torre, E.; Mancuso, G.; Lanzillotta, M.; Ramirez, G.A.; Arcidiacono, P.G.; Capurso, G.; Falconi, M.; Dagna, L. Urgent manifestations of immunoglobulin G4-related disease. Scand. J. Rheumatol. 2020, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Lanzillotta, M.; Campochiaro, C.; Trimarchi, M.; Arrigoni, G.; Gerevini, S.; Milani, R.; Bozzolo, E.; Biafora, M.; Venturini, E.; Cicalese, M.P.; et al. Deconstructing IgG4-related disease involvement of midline structures: Comparison to common mimickers. Mod. Rheumatol. 2017, 27, 638–645. [Google Scholar] [CrossRef] [PubMed]
- Reder, L.; Della-Torre, E.; Stone, J.H.; Mori, M.; Song, P. Clinical manifestations of IgG4-related disease in the pharynx. Ann. Otol. Rhinol. Laryngol. 2015, 124, 173–178. [Google Scholar] [CrossRef]
- Wallace, Z.S.; Naden, R.P.; Chari, S.; Choi, H.K.; Della-Torre, E.; Dicaire, J.F.; Hart, P.A.; Inoue, D.; Kawano, M.; Khosroshahi, A.; et al. The 2019 American College of Rheumatology/European League against Rheumatism classification criteria for IgG4-related disease. Ann. Rheum. Dis. 2020, 79, 77–87. [Google Scholar] [CrossRef]
- Wallace, Z.S.; Naden, R.P.; Chari, S.; Choi, H.; Della-Torre, E.; Dicaire, J.F.; Hart, P.A.; Inoue, D.; Kawano, M.; Khosroshahi, A.; et al. The 2019 American College of Rheumatology/European League against Rheumatism classification criteria for IgG4-related disease. Arthritis Rheumatol. 2020, 72, 7–19. [Google Scholar] [CrossRef] [Green Version]
- Lanzillotta, M.; Campochiaro, C.; Mancuso, G.; Ramirez, G.A.; Capurso, G.; Falconi, M.; Dagna, L.; Della-Torre, E. Clinical phenotypes of IgG4-related disease reflect different prognostic outcomes. Rheumatology 2020, 59, 2435–2442. [Google Scholar] [CrossRef]
- Umehara, H.; Okazaki, K.; Masaki, Y.; Kawano, M.; Yamamoto, M.; Saeki, T.; Matsui, S.; Yoshino, T.; Nakamura, S.; Kawa, S.; et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod. Rheumatol. 2012, 22, 21–30. [Google Scholar] [CrossRef]
- Della-Torre, E.; Mattoo, H.; Mahajan, V.S.; Deshpande, V.; Krause, D.; Song, P.; Pillai, S.; Stone, J.H. IgG4-related midline destructive lesion. Ann. Rheum. Dis. 2014, 73, 1434–14369. [Google Scholar] [CrossRef] [Green Version]
- Berti, A.; Della-Torre, E.; Gallivanone, F.; Canevari, C.; Milani, R.; Lanzillotta, M.; Campochiaro, C.; Alvise Ramirez, G.; Bozzalla Cassione, E.; Bozzolo, E.; et al. Quantitative measurement of 18 F-FDG PET/CT uptake reflects the expansion of circulating plasmablasts in IgG4-related disease Rheumatology key messages. Rheumatology 2017, 56, 2084–2092. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laco, J.; Kamarádová, K.; Mottl, R.; Mottlová, A.; Doležalová, H.; Tuček, L.; Žatečková, K.; Slezák, R.; Ryška, A. Plasma cell granuloma of the oral cavity—A mucosal manifestation of immunoglobulin G4-related disease or a mimic? Virchows Arch. 2015, 466, 255–263. [Google Scholar] [CrossRef]
- Baba, A.; Matsushima, S.; Toyoda, K.; Yamauchi, H.; Ikeda, K.; Sugimoto, K.; Ojiri, H. MR imaging of palatine gland lesion-associated IgG4-related disease: A preliminary study. Jpn. J. Radiol. 2020, 38, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Andrew, N.; Kearney, D.; Sladden, N.; Goss, A.; Selva, D. Immunoglobulin G4-related disease of the hard palate. J. Oral Maxillofac. Surg. 2014. [Google Scholar] [CrossRef] [PubMed]
- Della-Torre, E.; Passerini, G.; Furlan, R.; Roveri, L.; Chieffo, R.; Anzalone, N.; Doglioni, C.; Zardini, E.; Sabbadini, M.G.; Franciotta, D. Cerebrospinal fluid analysis in immunoglobulin G4-related hypertrophic pachymeningitis. J. Rheumatol. 2013, 40, 1927–1929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Della-Torre, E.; Galli, L.; Franciotta, D.; Bozzolo, E.P.; Briani, C.; Furlan, R.; Roveri, L.; Sessa, M.; Passerini, G.; Sabbadini, M.G. Diagnostic value of IgG4 Indices in IgG4-related hypertrophic pachymeningitis. J. Neuroimmunol. 2014, 266, 82–86. [Google Scholar] [CrossRef]
- Della-Torre, E.; Bozzolo, E.P.; Passerini, G.; Doglioni, C.; Sabbadini, M.G. IgG4-related pachymeningitis: Evidence of intrathecal IgG4 on cerebrospinal fluid analysis. Ann. Intern. Med. 2012, 156, 401–403. [Google Scholar] [CrossRef] [Green Version]
- Della-Torre, E.; Campochiaro, C.; Cassione Bozzalla, E.; Albano, L.; Gerevini, S.; Bianchi-Marzoli, S.; Bozzolo, E.; Passerini, G.; Lanzillotta, M.; Terreni, M.; et al. Intrathecal rituximab for IgG 4-related hypertrophic pachymeningitis. J. Neurol. Neurosurg. Psychiatry 2018, 89, 441–444. [Google Scholar] [CrossRef]
- Della-Torre, E.; Stone, J.H. “How I manage” IgG4-Related Disease. J. Clin. Immunol. 2016, 36, 754–763. [Google Scholar] [CrossRef]
- Chen, B.N. IgG4-related disease presenting with destructive sinonasal lesion mimicking malignancy. Eur. Arch. Oto-Rhino-Laryngol. 2016, 273, 4027–4029. [Google Scholar] [CrossRef]
- Marinelli, J.P.; Marvisi, C.; Vaglio, A.; Peters, P.A.; Dowling, E.M.; Palumbo, A.A.; Lane, J.I.; Appelbaum, E.N.; Sweeney, A.D.; Carlson, M.L. Manifestations of Skull Base IgG4-Related Disease: A Multi-Institutional Study. Laryngoscope 2019, 130, 2574–2580. [Google Scholar] [CrossRef] [PubMed]
- Biafora, M.; Bertazzoni, G.; Trimarchi, M. Maxillary sinusitis caused by dental implants extending into the maxillary sinus and the nasal cavities. J. Prosthodont. 2014, 23, 227–231. [Google Scholar] [CrossRef]
- Alfano, M.; Grivel, J.C.; Ghezzi, S.; Corti, D.; Trimarchi, M.; Poli, G.; Margolis, L. Pertussis toxin B-oligomer dissociates T cell activation and HIV replication in CD4 T cells released from infected lymphoid tissue. AIDS 2005, 20, 160–164. [Google Scholar] [CrossRef]
- Trimarchi, M.; Lombardi, D.; Tomenzoli, D.; Farina, D.; Nicolai, P. Pneumosinus dilatans of the maxillary sinus: A case report and review of the literature. Eur. Arch. Oto-Rhino-Laryngol. 2003, 260, 386–389. [Google Scholar] [CrossRef]
- Morassi, M.L.; Trimarchi, M.; Nicolai, P.; Gregorini, G.; Maroldi, R.; Specks, U.; Facchetti, F. Cocaina, ANCA e granulomatosi di Wegener. Pathologica 2001, 93, 581–583. [Google Scholar]
- Capparé, P.; Teté, G.; Romanos, G.E.; Nagni, M.; Sannino, G.; Gherlone, E.F. The “All-on-four” protocol in HIV-positive patients: A prospective, longitudinal 7-year clinical study. Int. J. Oral Implantol. 2019, 12, 501–510. [Google Scholar]
- Gherlone, E.F.; Capparé, P.; Tecco, S.; Polizzi, E.; Pantaleo, G.; Gastaldi, G.; Grusovin, M.G. Implant Prosthetic Rehabilitation in Controlled HIV-Positive Patients: A Prospective Longitudinal Study with 1-Year Follow-Up. Clin. Implant. Dent. Relat. Res. 2016, 18, 725–734. [Google Scholar] [CrossRef]
- Gherlone, E.F.; Capparé, P.; Tecco, S.; Polizzi, E.; Pantaleo, G.; Gastaldi, G.; Grusovin, M.G. A Prospective Longitudinal Study on Implant Prosthetic Rehabilitation in Controlled HIV-Positive Patients with 1-Year Follow-Up: The Role of CD4+ Level, Smoking Habits, and Oral Hygiene. Clin. Implant. Dent. Relat. Res. 2016, 18, 955–964. [Google Scholar] [CrossRef]
- Tecco, S.; Parisi, M.R.; Gastaldi, G.; Polizzi, E.; D’Amicantonio, T.; Zilocchi, I.; Gardini, I.; Gherlone, E.F.; Lazzarin, A.; Capparè, P. Point-of-care testing for hepatitis C virus infection at an Italian dental clinic: Portrait of the Pilot study population. N. Microbiol. 2019, 42, 133–138. [Google Scholar]
- Trimarchi, M.; Bellini, C.; Toma, S.; Bussi, M. Back-and-forth endoscopic septoplasty: Analysis of the technique and outcomes. Int. Forum Allergy Rhinol. 2012, 2, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Trimarchi, M.; Miluzio, A.; Nicolai, P.; Morassi, M.L.; Bussi, M.; Marchisio, P.C. Massive apoptosis erodes nasal mucosa of cocaine abusers. Am. J. Rhinol. 2006, 20, 160–164. [Google Scholar] [CrossRef]
- Kusuke, N.; Custódio, M.; de Sousa, S.C.O.M. Oral lesion as the primary diagnosis of non-Hodgkin’s lymphoma: A 20-year experience from an oral pathology service and review of the literature. Eur. Arch. Oto-Rhino-Laryngol. 2019, 276, 2873–2879. [Google Scholar] [CrossRef]
- Trimarchi, M.; Mortini, P. Cocaine-Induced Midline Destructive Lesion and Wegener Granulomatosis. Neurosurgery 2012, 70, E1339. [Google Scholar] [CrossRef]
- Di Santo, D.; Trimarchi, M.; Galli, A.; Bussi, M. Columella reconstruction with an inferiorly-based philtral advancement flap in a cocaine abuser. Indian J. Plast. Surg. 2017, 50, 96–99. [Google Scholar] [CrossRef]
- Trimarchi, M.; Nicolai, P.; Lombardi, D.; Facchetti, F.; Morassi, M.L.; Maroldi, R.; Gregorini, G.; Specks, U. Sinonasal osteocartilaginous necrosis in cocaine abusers: Experience in 25 patients. Am. J. Rhinol. 2003, 17, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Trimarchi, M.; Bellini, C.; Fabiano, B.; Gerevini, S.; Bussi, M. Un caso di pemfigoide mucosinechiante con coinvolgimento nasale e laringeo. Acta Otorhinolaryngol. Ital. 2009, 29, 222–225. [Google Scholar]
- Trimarchi, M.; Bertazzoni, G.; Bussi, M. Cocaine induced midline destructive lesions. Rhinology 2014, 52, 104–111. [Google Scholar] [CrossRef] [Green Version]
- Trimarchi, M.; Bussi, M.; Sinico, R.A.; Meroni, P.; Specks, U. Cocaine-induced midline destructive lesions—An autoimmune disease? Autoimmun. Rev. 2013, 12, 496–500. [Google Scholar] [CrossRef]
- Wallace, Z.S.; Deshpande, V.; Mattoo, H.; Mahajan, V.S.; Kulikova, M.; Pillai, S.; Stone, J.H. IgG4-related disease: Clinical and laboratory features in one hundred twenty-five patients. Arthritis Rheumatol. 2015, 67, 2466–2475. [Google Scholar] [CrossRef] [Green Version]
- Campochiaro, C.; Ramirez, G.A.; Bozzolo, E.P.; Lanzillotta, M.; Berti, A.; Baldissera, E.; Dagna, L.; Praderio, L.; Scotti, R.; Tresoldi, M.; et al. IgG4-related disease in Italy: Clinical features and outcomes of a large cohort of patients. Scand. J. Rheumatol. 2016, 45, 135–145. [Google Scholar] [CrossRef]
- Thompson, A.; Whyte, A. Imaging of IgG4-related disease of the head and neck. Clin. Radiol. 2018, 73, 106–120. [Google Scholar] [CrossRef]
- Deshpande, V.; Zen, Y.; Chan, J.K.C.; Yi, E.E.; Sato, Y.; Yoshino, T.; Klöppel, G.; Godfrey Heathcote, J.; Khosroshahi, A.; Ferry, J.A.; et al. Consensus statement on the pathology of IgG4-related disease. Mod. Pathol. 2012, 25, 1181–1192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Della-Torre, E.; Lanzillotta, M.; Doglioni, C. Immunology of IgG4-related disease. Clin. Exp. Immunol. 2015, 181, 191–206. [Google Scholar] [CrossRef] [Green Version]
- Ebbo, M.; Grados, A.; Bernit, E.; Vély, F.; Boucraut, J.; Harlé, J.-R.; Daniel, L.; Schleinitz, N. Pathologies Associated with Serum IgG4 Elevation. Int. J. Rheumatol. 2012, 2012, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Carruthers, M.N.; Khosroshahi, A.; Augustin, T.; Deshpande, V.; Stone, J.H. The diagnostic utility of serum IgG4 concentrations in IgG4-related disease. Ann. Rheum. Dis. 2015, 74, 14–18. [Google Scholar] [CrossRef] [Green Version]
- Della-Torre, E.; Bozzalla-Cassione, E.; Sciorati, C.; Ruggiero, E.; Lanzillotta, M.; Bonfiglio, S.; Mattoo, H.; Perugino, C.A.; Bozzolo, E.; Rovati, L.; et al. A CD8α− Subset of CD4+SLAMF7+ Cytotoxic T Cells Is Expanded in Patients With IgG4-Related Disease and Decreases Following Glucocorticoid Treatment. Arthritis Rheumatol. 2018, 70, 1133–1143. [Google Scholar] [CrossRef]
- Wallace, Z.S.; Khosroshahi, A.; Carruthers, M.D.; Perugino, C.A.; Choi, H.; Campochiaro, C.; Culver, E.L.; Cortazar, F.; Della-torre, E.; Ebbo, M.; et al. An International Multispecialty Validation Study of the IgG4-Related Disease Responder Index. Arthritis Care Res. 2018, 70, 1671–1678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Della-Torre, E.; Rigamonti, E.; Perugino, C.; Baghai-Sain, S.; Sun, N.; Kaneko, N.; Maehara, T.; Rovati, L.; Ponzoni, M.; Milani, R.; et al. B lymphocytes directly contribute to tissue fibrosis in patients with IgG4-related disease. J. Allergy Clin. Immunol. 2020, 145, 968–981.e14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lanzillotta, M.; Della-Torre, E.; Stone, J.H. Roles of plasmablasts and B cells in IgG4-related disease: Implications for therapy and early treatment outcomes. Curr. Top. Microbiol. Immunol. 2017, 401, 85–92. [Google Scholar] [CrossRef]
- Della-Torre, E.; Feeney, E.; Deshpande, V.; Mattoo, H.; Mahajan, V.; Kulikova, M.; Wallace, Z.S.; Carruthers, M.; Chung, R.T.; Pillai, S.; et al. B-cell depletion attenuates serological biomarkers of fibrosis and myofibroblast activation in IgG4-related disease. Ann. Rheum. Dis. 2015, 74, 2236–2243. [Google Scholar] [CrossRef] [Green Version]



| Patient | Age, Sex | Oral Cavity Involvement | Other Structures Involved | ESR 1,2 | CPR 1,3 | Serum IgG4 1,4 |
|---|---|---|---|---|---|---|
| 1 | 35, F | Hard palate | Pachymeninges, optic nerves, nasal septum | 33 | 44 | 151 |
| 2 | 20, F | Hard palate | Cervical lymph nodes, parotids, oropharynx, pterygopalatine fossa | 5 | 0.3 | 421 |
| 3 | 45, M | Superior alveolar processes | Nasal and maxillary structures, cervical lymph nodes, lungs | 420 | ||
| 4 | 37, F | Tonsillar and peritonsillar region | Cervical Lymph nodes | 72 | 8 | 131 |
| 5 | 57, M | Tongue base extending to oropharynx | Retroperitoneum encasing aorta | 28 | 1.3 | 30 |
| 6 | 29, M | Tongue base | Salivary glands, Rhino pharynx | 8 | 23 | 257 |
| Patient | Histologic Findings | First-Line Therapy and Outcome | Second-Line Therapy and Outcome |
|---|---|---|---|
| 1 | Palate: storiform fibrosis, IgG4+: 100 × HPF, IgG4+/IgG+ plasma cells > 40% | Prednisone 1 gm/die for 3 days, then 0.6 mg/kg/die and gradual tapering. Partial response. | Two 1 gm doses of rituximab 15 days apart. Marked improvement. |
| 2 | Small salivary gland: fibrosis, IgG4+ 50 × HPF, IgG4+/IgG+ plasma cells 70% | Rituximab 375 mg/m2, four weekly infusions IV. Prompt resolution of symptoms. | |
| 3 | Nose: storiform fibrosis, IgG4+: > 80 × HPF, IgG4+/IgG+ plasma cells 30–40% | Prednisone 0.6 mg/kg/die and gradual tapering. Lung response, persistence of maxillofacial lesions. | Under consideration for surgery. |
| 4 | Tonsil: fibrosis, IgG4+ > 180 × HPF, IgG4+/IgG+ plasma cells 30% | Prednisone 0.6 mg/kg/die and gradual tapering. Complete response. | |
| 5 | Tongue: undiagnostic. Retroperitoneum: IgG4+: > 100 × HPF, IgG4+/IgG+ plasma cells > 40% | Prednisone 0.6 mg/kg/die and gradual tapering. Marked improvement. | |
| 6 | Labial salivary glands and tongue base: unspecific inflammation | Watchful waiting. Stable disease. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rampi, A.; Lanzillotta, M.; Mancuso, G.; Vinciguerra, A.; Dagna, L. IgG4-Related Disease of the Oral Cavity. Case Series from a Large Single-Center Cohort of Italian Patients. Int. J. Environ. Res. Public Health 2020, 17, 8179. https://doi.org/10.3390/ijerph17218179
Rampi A, Lanzillotta M, Mancuso G, Vinciguerra A, Dagna L. IgG4-Related Disease of the Oral Cavity. Case Series from a Large Single-Center Cohort of Italian Patients. International Journal of Environmental Research and Public Health. 2020; 17(21):8179. https://doi.org/10.3390/ijerph17218179
Chicago/Turabian StyleRampi, Andrea, Marco Lanzillotta, Gaia Mancuso, Alessandro Vinciguerra, and Lorenzo Dagna. 2020. "IgG4-Related Disease of the Oral Cavity. Case Series from a Large Single-Center Cohort of Italian Patients" International Journal of Environmental Research and Public Health 17, no. 21: 8179. https://doi.org/10.3390/ijerph17218179







