Personal and Lifestyle Determinants of HIV Transmission Risk in Spanish University Students
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedure
2.2. Measures
2.2.1. HIV Risk
2.2.2. Lifestyles
2.3. Data Analysis
3. Results
3.1. Scores in Each Dimension of HIV Risk of Infection
3.2. Differences in Risk of HIV Infection Depending on Personal and Sociodemographic Characteristics
3.3. Differences in Risk of HIV Infection Depending on Lifestyles
3.4. Personal and Lifestyles Predictors of HIV Risk Factors
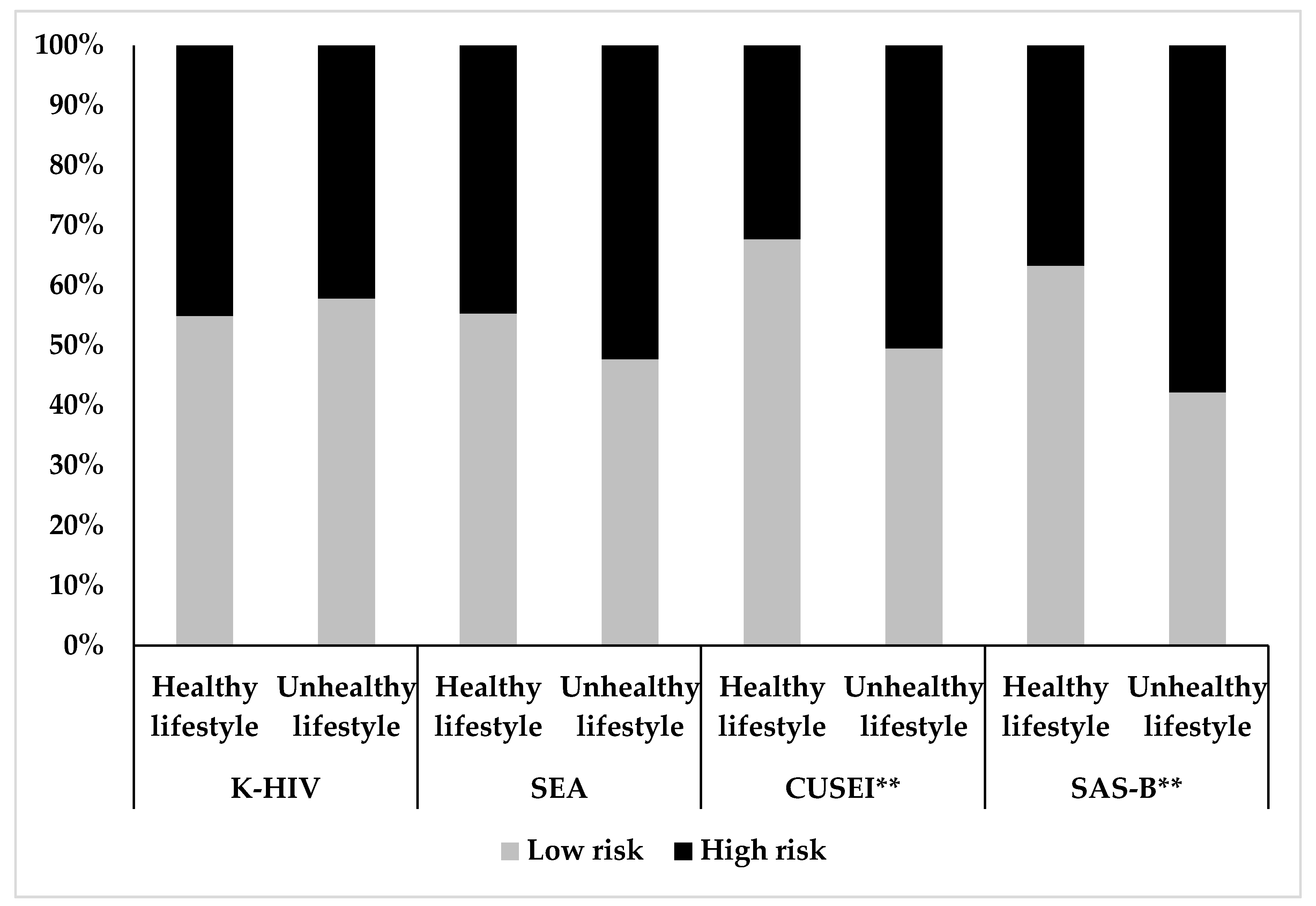
3.5. Risk of HIV Infection Based on the Quality of Total Lifestyle
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Data and Statistics about HIV/AIDS. Available online: http://www.who.int/hiv/data/en/ (accessed on 15 March 2020).
- UNAIDS Communities at the Centre. Defending Rights, Breaking Barriers, Reaching People with HIV Services. Available online: https://www.unaids.org/sites/default/files/media_asset/2019-global-AIDS-update_en.pdf (accessed on 15 March 2020).
- Marston, C.; King, E. Factors that shape young people’s sexual behaviour: A systematic review. Lancet 2006, 368, 1581–1586. [Google Scholar] [CrossRef]
- Costa, E.C.V.; McIntyre, T.; Ferreira, D. Safe-Sex Knowledge, Self-Assessed HIV Risk, and Sexual Behaviour of Young Portuguese Women. Port. J. Public Health 2018, 36, 16–25. [Google Scholar] [CrossRef]
- Pettifor, A.E.; van der Straten, A.; Dunbar, M.S.; Shiboski, S.C.; Padian, N.S. Early age of first sex: A risk factor for HIV infection among women in Zimbabwe. AIDS 2004, 18, 1435–1442. [Google Scholar] [CrossRef] [PubMed]
- Saura, S.; Jorquera, V.; Mascort, C.; Castellà, I. Gender meanings of the risk of sexually transmitted infections/HIV transmission among young people. Aten. Primaria 2020, 52, 218–219. [Google Scholar] [CrossRef]
- Mendez, R.V.; Hulsey, T.L.; Archer, R.L. Multiple partners in the age of AIDS: Self-consciousness theory and HIV risk behavior. Curr. Psychol. 2001, 20, 349–362. [Google Scholar] [CrossRef]
- Arasteh, K.; Des Jarlais, D.C.; McKnight, C.; Feelemyer, J. Injection and Heterosexual Risk Behaviors for HIV Infection Among Non-gay Identifying Men Who Have Sex with Men and Women. AIDS Behav. 2019, 23, 3315–3323. [Google Scholar] [CrossRef]
- Beyrer, C.; Baral, S.D.; Walker, D.; Wirtz, A.L.; Johns, B.; Sifakis, F. The expanding epidemics of HIV type 1 among men who have sex with men in low- and middle-income countries: Diversity and consistency. Epidemiol. Rev. 2010, 32, 137–151. [Google Scholar] [CrossRef]
- Icard, L.D.; Zhang, J.; Jemmott, J.B.; Sandfort, T.G.M.; Rutledge, S.E.; Van Greunen, D.; Martinez, O. The Effects of Three Types of Sexual Orientation Victimization on HIV Sexual Risk Behavior Among Black South African Men Who Have Sex With Men (MSM). J. Homosex 2020, 67, 513–527. [Google Scholar] [CrossRef]
- Rogers, A.H.; Jardin, C.; Mayorga, N.A.; Bakhshaie, J.; Leonard, A.; Lemaire, C.; Zvolensky, M.J. The relationship of discrimination related to sexual orientation and HIV-relevant risk behaviors among men who have sex with men. Psychiatry Res. 2018, 267, 102–107. [Google Scholar] [CrossRef]
- Blair, C.S.; Segura, E.R.; Perez-Brumer, A.G.; Sanchez, J.; Lama, J.R.; Clark, J.L. Sexual Orientation, Gender Identity and Perceived Source of Infection Among Men Who Have Sex with Men (MSM) and Transgender Women (TW) Recently Diagnosed with HIV and/or STI in Lima, Peru. AIDS Behav. 2016, 20, 2178–2185. [Google Scholar] [CrossRef][Green Version]
- Golub, S.A.; Starks, T.J.; Payton, G.; Parsons, J.T. The critical role of intimacy in the sexual risk behaviors of gay and bisexual men. AIDS Behav. 2012, 16, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Mayo-Wilson, L.J.; Glass, N.E.; Ssewamala, F.M.; Linnemayr, S.; Coleman, J.; Timbo, F.; Johnson, M.W.; Davoust, M.; Labrique, A.; Yenokyan, G.; et al. Microenterprise intervention to reduce sexual risk behaviors and increase employment and HIV preventive practices in economically-vulnerable African-American young adults (EMERGE): Protocol for a feasibility randomized clinical trial. Trials 2019, 20, 439. [Google Scholar] [CrossRef] [PubMed]
- Richardson, L.; Mammel, M.; Milloy, M.-J.; Hayashi, K. Employment Cessation, Long Term Labour Market Engagement and HIV Infection Risk Among People Who Inject Drugs in an Urban Canadian Setting. AIDS Behav. 2019, 23, 3267–3276. [Google Scholar] [CrossRef] [PubMed]
- Dixon, D.A.; Antoni, M.; Peters, M.; Saul, J. Employment, Social Support, and HIV Sexual-Risk Behavior in Puerto Rican Women. AIDS Behav. 2001, 5, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Ballester Arnal, R.; Gil, M.D.; Giménez, C.; Ruiz, E. Actitudes y conductas sexuales de riesgo para la infección por VIH/SIDA en jóvenes españoles. RPPC 2009, 14, 181–191. [Google Scholar] [CrossRef]
- Balachova, T.; Shaboltas, A.; Nasledov, A.; Chaffin, M.; Batluk, J.; Bohora, S.; Bonner, B.; Bryant, K.; Tsvetkova, L.; Volkova, E. Alcohol and HIV Risk Among Russian Women of Childbearing Age. AIDS Behav. 2017, 21, 1857–1867. [Google Scholar] [CrossRef]
- Zhan, W.; Shaboltas, A.V.; Skochilov, R.V.; Kozlov, A.P.; Krasnoselskikh, T.V.; Abdala, N. Alcohol misuse, drinking contexts and intimate partner violence in St. Petersburg, Russia: Results from a cross-sectional study. BMC Public Health 2011, 11, 629. [Google Scholar] [CrossRef]
- Balachova, T.; Bonner, B.; Chaffin, M.; Bard, D.; Isurina, G.; Tsvetkova, L.; Volkova, E. Women’s alcohol consumption and risk for alcohol-exposed pregnancies in Russia. Addiction 2012, 107, 109–117. [Google Scholar] [CrossRef]
- Martinez, O.; Muñoz-Laboy, M.; Levine, E.C.; Starks, T.; Dolezal, C.; Dodge, B.; Icard, L.; Moya, E.; Chavez-Baray, S.; Rhodes, S.D.; et al. Relationship Factors Associated with Sexual Risk Behavior and High-Risk Alcohol Consumption Among Latino Men Who Have Sex with Men: Challenges and Opportunities to Intervene on HIV Risk. Arch. Sex. Behav. 2017, 46, 987–999. [Google Scholar] [CrossRef]
- Mutchler, M.G.; McDavitt, B.; Gordon, K.K. “Becoming bold”: Alcohol use and sexual exploration among Black and Latino young men who have sex with men (YMSM). J. Sex. Res. 2014, 51, 696–710. [Google Scholar] [CrossRef]
- Boulos, R.; Halsey, N.A.; Holt, E.; Ruff, A.; Brutus, J.R.; Quinn, T.C.; Adrien, M.; Boulos, C. HIV-1 in Haitian women 1982-1988. The Cite Soleil/JHU AIDS Project Team. J. Acquir. Immune Defic. Syndr. 1990, 3, 721–728. [Google Scholar] [PubMed]
- Burns, D.N.; Kramer, A.; Yellin, F.; Fuchs, D.; Wachter, H.; DiGioia, R.A.; Sanchez, W.C.; Grossman, R.J.; Gordin, F.M.; Biggar, R.J. Cigarette smoking: A modifier of human immunodeficiency virus type 1 infection? J. Acquir. Immune Defic. Syndr. 1991, 4, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Chao, A.; Bulterys, M.; Musanganire, F.; Habimana, P.; Nawrocki, P.; Taylor, E.; Dushimimana, A.; Saah, A. Risk factors associated with prevalent HIV-1 infection among pregnant women in Rwanda. National University of Rwanda-Johns Hopkins University AIDS Research Team. Int. J. Epidemiol. 1994, 23, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Halsey, N.A.; Coberly, J.S.; Holt, E.; Coreil, J.; Kissinger, P.; Moulton, L.H.; Brutus, J.R.; Boulos, R. Sexual behavior, smoking, and HIV-1 infection in Haitian Women. JAMA 1992, 267, 2062–2066. [Google Scholar] [CrossRef] [PubMed]
- Siraprapasiri, T.; Foy, H.M.; Kreiss, J.K.; Pruithitada, N.; Thongtub, W. Frequency and risk of HIV infection among men attending a clinic for STD in Chiang Mai, Thailand. Southeast Asian J. Trop. Med. Public Health 1996, 27, 96–101. [Google Scholar] [PubMed]
- Marshall, M.M.; McCormack, M.C.; Kirk, G.D. Effect of cigarette smoking on HIV acquisition, progression, and mortality. AIDS Educ. Prev. 2009, 21, 28–39. [Google Scholar] [CrossRef]
- Harden, K.P.; Hill, J.E.; Turkheimer, E.; Emery, R.E. Gene-environment correlation and interaction in peer effects on adolescent alcohol and tobacco use. Behav. Genet. 2008, 38, 339–347. [Google Scholar] [CrossRef]
- Matuszka, B.; Bácskai, E.; Czobor, P.; Gerevich, J. Physical Aggression and Concurrent Alcohol and Tobacco Use Among Adolescents. Int. J. Ment. Health Addict. 2017, 15, 90–99. [Google Scholar] [CrossRef]
- Wei, C.; Yu, C.; Gao, M. Parental Marital Conflict and Tobacco and Alcohol Use among Adolescents: A Moderated Mediation Model. JPBS J. Psychol. 2019, 7, 64–73. [Google Scholar] [CrossRef]
- Chop, E.; Duggaraju, A.; Malley, A.; Burke, V.; Caldas, S.; Yeh, P.T.; Narasimhan, M.; Amin, A.; Kennedy, C.E. Food insecurity, sexual risk behavior, and adherence to antiretroviral therapy among women living with HIV: A systematic review. Health Care Women Int. 2017, 38, 927–944. [Google Scholar] [CrossRef]
- Eaton, L.A.; Cain, D.N.; Pitpitan, E.V.; Carey, K.B.; Carey, M.P.; Mehlomakulu, V.; Simbayi, L.C.; Mwaba, K.; Kalichman, S.C. Exploring the relationships among food insecurity, alcohol use, and sexual risk taking among men and women living in South African townships. J. Prim. Prev. 2014, 35, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Masa, R.; Graham, L.; Khan, Z.; Chowa, G.; Patel, L. Food insecurity, sexual risk taking, and sexual victimization in Ghanaian adolescents and young South African adults. Int. J. Public Health 2019, 64, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Barrett, C.B. Measuring Food Insecurity. Science 2010, 327, 825–828. [Google Scholar] [CrossRef] [PubMed]
- Hendricks, K.M.; Herbold, N.; Fung, T. Diet and other lifestyle behaviors in young college women. Nutr. Res. 2004, 24, 981–991. [Google Scholar] [CrossRef]
- Spencer, S.J.; Korosi, A.; Layé, S.; Shukitt-Hale, B.; Barrientos, R.M. Food for thought: How nutrition impacts cognition and emotion. NPJ Sci. Food 2017, 1, 7. [Google Scholar] [CrossRef]
- Grenard, J.L.; Ames, S.L.; Stacy, A.W. Deliberative and spontaneous cognitive processes associated with HIV risk behavior. J. Behav. Med. 2013, 36, 95–107. [Google Scholar] [CrossRef][Green Version]
- Miller, K.E.; Barnes, G.M.; Melnick, M.J.; Sabo, D.F.; Farrell, M.P. Gender and racial/ethnic differences in predicting adolescent sexual risk: Athletic participation versus exercise. J. Health Soc. Behav. 2002, 43, 436–450. [Google Scholar] [CrossRef]
- Lebron, C.; Stoutenberg, M.; Janowsky, M.; Asfour, L.; Huang, S.; Prado, G. The Role of Physical Activity and Sedentary Behavior in Substance Use and Risky Sex Behaviors in Hispanic Adolescents. J. Early Adolesc. 2017, 37, 910–924. [Google Scholar] [CrossRef]
- Vuori, M.T.; Kannas, L.K.; Villberg, J.; Ojala, S.A.K.; Tynjälä, J.A.; Välimaa, R.S. Is physical activity associated with low-risk health behaviours among 15-year-old adolescents in Finland? Scand. J. Public Health 2012, 40, 61–68. [Google Scholar] [CrossRef]
- Gil-Llario, M.D.; Ruiz-Palomino, E.; Morell-Mengual, V.; Giménez-García, C.; Ballester-Arnal, R. Validation of the AIDS Prevention Questionnaire: A Brief Self-Report Instrument to Assess Risk of HIV Infection and Guide Behavioral Change. AIDS Behav. 2019, 23, 272–282. [Google Scholar] [CrossRef]
- Godwin, M.; Streight, S.; Dyachuk, E.; van den Hooven, E.C.; Ploemacher, J.; Seguin, R.; Cuthbertson, S. Testing the Simple Lifestyle Indicator Questionnaire: Initial psychometric study. Can. Fam. Physician 2008, 54, 76–77. [Google Scholar] [PubMed]
- Mahat, G.; Scoloveno, M.A. Effectiveness of Adolescent Peer Education Programs on Reducing HIV/STI Risk: An Integrated Review. Res. Theory Nurs. Pract. 2018, 32, 168–198. [Google Scholar] [CrossRef] [PubMed]
- Sani, A.S.; Abraham, C.; Denford, S.; Ball, S. School-based sexual health education interventions to prevent STI/HIV in sub-Saharan Africa: A systematic review and meta-analysis. BMC Public Health 2016, 16, 1069. [Google Scholar] [CrossRef] [PubMed]
- Millard, T.; Elliott, J.; Girdler, S. Self-management education programs for people living with HIV/AIDS: A systematic review. AIDS Patient Care STDS 2013, 27, 103–113. [Google Scholar] [CrossRef]
- Bardo, M.T.; Compton, W.M. Does physical activity protect against drug abuse vulnerability? Drug Alcohol Depend. 2015, 153, 3–13. [Google Scholar] [CrossRef]
- Dodge, T.; Clarke, P.; Dwan, R. The Relationship between Physical Activity and Alcohol Use among Adults in the United States. Am. J. Health Promot. 2017, 31, 97–108. [Google Scholar] [CrossRef]
- deRuiter, W.; Faulkner, G. Tobacco harm reduction strategies: The case for physical activity. Nicotine Tob. Res. 2006, 8, 157–168. [Google Scholar] [CrossRef]
- Pate, R.R.; Trost, S.G.; Levin, S.; Dowda, M. Sports participation and health-related behaviors among US youth. Arch. Pediatr. Adolesc. Med. 2000, 154, 904–911. [Google Scholar] [CrossRef]
- Kulig, K.; Brener, N.D.; McManus, T. Sexual activity and substance use among adolescents by category of physical activity plus team sports participation. Arch. Pediatr. Adolesc. Med. 2003, 157, 905–912. [Google Scholar] [CrossRef]
- Fetner, T.; Dion, M.; Heath, M.; Andrejek, N.; Newell, S.L.; Stick, M. Condom use in penile-vaginal intercourse among Canadian adults: Results from the sex in Canada survey. PLoS ONE 2020, 15, e0228981. [Google Scholar] [CrossRef]
- Protogerou, C.; Turner-Cobb, J. Predictors of non-condom use intentions by university students in Britain and Greece: The impact of attitudes, time perspective, relationship status, and habit. J. Child. Adolesc. Ment. Health 2011, 23, 91–106. [Google Scholar] [CrossRef] [PubMed]
- Wang, X. The role of attitude functions, efficacy, anticipated emotions, and relationship status on college students’ condom use intentions. J. Sex. Res. 2013, 50, 704–714. [Google Scholar] [CrossRef] [PubMed]
- Macaluso, M.; Demand, M.J.; Artz, L.M.; Hook, E.W. Partner type and condom use. AIDS 2000, 14, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Lan, C.-W.; Scott-Sheldon, L.A.J.; Carey, K.B.; Johnson, B.T.; Carey, M.P. Prevalence of Alcohol Use, Sexual Risk Behavior, and HIV Among Russians in High-Risk Settings: A Systematic Review and Meta-Analysis. Int. J. Behav. Med. 2017, 24, 180–190. [Google Scholar] [CrossRef] [PubMed]
- Mola, R.; Pitangui, A.C.R.; Barbosa, S.A.M.; Almeida, L.S.; de Sousa, M.R.M.; de Lima Pio, W.P.; de Araújo, R.C. Condom use and alcohol consumption in adolescents and youth. Einstein 2016, 14, 143–151. [Google Scholar] [CrossRef]
- Vagenas, P.; Lama, J.R.; Ludford, K.T.; Gonzales, P.; Sanchez, J.; Altice, F.L. A systematic review of alcohol use and sexual risk-taking in Latin America. Rev. Panam. Salud. Publica 2013, 34, 267–274. [Google Scholar]
- Feldstein Ewing, S.W.; Ryman, S.G.; Gillman, A.S.; Weiland, B.J.; Thayer, R.E.; Bryan, A.D. Developmental Cognitive Neuroscience of Adolescent Sexual Risk and Alcohol Use. AIDS Behav. 2016, 20, S97–S108. [Google Scholar] [CrossRef]
- Laska, M.N.; Pasch, K.E.; Lust, K.; Story, M.; Ehlinger, E. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prev. Sci. 2009, 10, 376–386. [Google Scholar] [CrossRef]
- Serra, M.C.; Dondero, K.R.; Larkins, D.; Burns, A.; Addison, O. Healthy Lifestyle and Cognition: Interaction between Diet and Physical Activity. Curr. Nutr. Rep. 2020. [Google Scholar] [CrossRef]
- Tandon, P.S.; Tovar, A.; Jayasuriya, A.T.; Welker, E.; Schober, D.J.; Copeland, K.; Dev, D.A.; Murriel, A.L.; Amso, D.; Ward, D.S. The relationship between physical activity and diet and young children’s cognitive development: A systematic review. Prev. Med. Rep. 2016, 3, 379–390. [Google Scholar] [CrossRef]
- Campos, M.W.; Serebrisky, D.; Castaldelli-Maia, J.M. Smoking and Cognition. Curr. Drug Abuse Rev. 2016, 9, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.M.; Duperrouzel, J.; Vega, M.; Gonzalez, R. The Neuropsychology of Risky Sexual Behavior. J. Int. Neuropsychol. Soc. 2016, 22, 586–594. [Google Scholar] [CrossRef] [PubMed]
| Variable | Categories | Total Sample N = 335 |
|---|---|---|
| Age | 19.62 ± 2.22 | |
| Sex | Male | 71 (21.2%) |
| Female | 264 (78.8%) | |
| Relationship status | Single | 234 (69.9%) |
| In a relationship | 101 (30.1%) | |
| Employment status | Employed | 52 (15.5%) |
| Non-employed | 283 (84.5%) | |
| Economic status a | EUR < 500 | 284 (84.8%) |
| EUR > 500 | 51 (15.2%) | |
| Sexual orientation | Heterosexual | 250 (74.6%) |
| Non-heterosexual | 85 (25.4%) | |
| Diet | Poor | 123 (36.7%) |
| Moderate | 162 (48.4%) | |
| Good | 50 (14.9%) | |
| Exercise | Light | 49 (14.6%) |
| Moderate | 101 (30.1%) | |
| Vigorous | 185 (55.2%) | |
| Alcohol consumption | Low | 273 (81.5%) |
| Moderate | 42 (12.5%) | |
| High | 20 (6%) | |
| Smoking | Non-smoker | 137 (40.9%) |
| Former smoker | 147 (43.9%) | |
| Current smoker | 51 (15.2%) | |
| Life stress | Low | 58 (17.3%) |
| Moderate | 191 (57%) | |
| High | 86 (25.7%) | |
| Total Healthy Lifestyle | Low | 109 (32.5%) |
| Moderate | 151 (45.1%) | |
| High | 75 (22.4%) |
| Variable | Min. | Max. | Mean | SD | N (%) | |
|---|---|---|---|---|---|---|
| Low Risk | High Risk | |||||
| K-HIV | 7.00 | 24.00 | 17.74 | 2.83 | 187 (55.8%) | 148 (44.2%) |
| SEA | 15.00 | 45.00 | 29.49 | 4.44 | 177 (52.8%) | 158 (47.2%) |
| CUSEI | 1.00 | 18.00 | 11.87 | 3.89 | 207 (61.8%) | 128 (38.2%) |
| SAS-B | 0.00 | 18.00 | 11.33 | 4.33 | 189 (56.4%) | 146 (43.6%) |
| Variable | Categories | K-HIV | SEA | CUSEI | SAS-B |
|---|---|---|---|---|---|
| Age | 18 years (n = 163) | 17.39 ± 2.88 | 29.22 ± 4.89 | 12.35 ± 3.70 | 11.87 ± 4.11 |
| >18 years (n = 172) | 18.08 ± 2.74 | 29.75 ± 4.06 | 11.41 ± 4.01 | 10.83 ± 4.49 | |
| Sex | Female (n = 264) | 17.85 ± 2.80 | 29.34 ± 4.53 | 11.81 ± 3.98 | 11.19 ± 4.42 |
| Male (n = 71) | 17.33 ± 2.89 | 30.07 ± 4.05 | 12.09 ± 3.51 | 11.85 ± 3.98 | |
| Relationship status | Single (n = 234) | 17.76 ± 2.89 | 29.33 ± 4.67 | 12.24 ± 3.94 | 11.90 ± 4.23 |
| In a relationship (n = 101) | 17.70 ± 2.69 | 29.87 ± 3.85 | 11.00 ± 3.64 | 10.02 ± 4.31 | |
| Employment status | Employed (n = 52) | 18.94 ± 2.54 | 29.57 ± 5.01 | 10.86 ± 3.96 | 10.07 ± 4.37 |
| Non-employed (n = 283) | 17.52 ± 2.83 | 29.48 ± 4.33 | 12.05 ± 3.85 | 11.56 ± 4.29 | |
| Economic status a | <500 euros (n = 284) | 17.68 ± 2.79 | 29.48 ± 4.37 | 11.83 ± 3.86 | 11.41 ± 4.22 |
| >500 euros (n = 51) | 18.07 ± 3.02 | 29.56 ± 4.83 | 11.82 ± 4.09 | 10.88 ± 4.95 | |
| Sexual Orientation | Heterosexual (n = 250) | 17.71 ± 2.91 | 29.44 ± 4.46 | 11.71 ± 4.06 | 11.21 ± 4.33 |
| Non-heterosexual (n = 85) | 17.84 ± 2.59 | 29.65 ± 4.40 | 12.34 ± 3.29 | 11.70 ± 4.36 |
| Variable | Categories | K-HIV | SEA | CUSEI | SAS-B |
|---|---|---|---|---|---|
| Diet | Poor (n = 123) | 17.43 ± 2,84 | 28,80 ± 4.74 | 11.04 ± 4.49 | 10.60 ± 4.95 |
| Moderate (n = 162) | 17.83 ± 2.83 | 29.75 ± 4.17 | 12.29 ± 3.50 | 11.61 ± 3.93 | |
| Good (n = 50) | 18.22 ± 2.75 | 30.34 ± 4.36 | 12.56 ± 3.14 | 12.20 ± 3.72 | |
| Exercise | Light (n = 49) | 17.64 ± 2.72 | 29.14 ± 3.91 | 10.89 ± 4.70 | 10.20 ± 5.33 |
| Moderate (n = 101) | 17.37 ± 2.87 | 28.28 ± 4.86 | 11.67 ± 3.93 | 11.09 ± 4.30 | |
| Vigorous (n = 185) | 18.02 ± 2.82 | 30.24 ± 4.18 | 12.23 ± 3.59 | 11.76 ± 4.01 | |
| Alcohol consumption | Low (n = 273) | 17.84 ± 2.93 | 29.61 ± 4.42 | 12.19 ± 3.87 | 11.63 ± 4.33 |
| Moderate (n = 42) | 17.19 ± 2.32 | 28.40 ± 4.91 | 10.02 ± 3.68 | 9.73 ± 4.09 | |
| High (n = 20) | 17.60 ± 2.25 | 30.15 ± 3.39 | 11.30 ± 3.59 | 10.60 ± 4.28 | |
| Smoking | Non-smoker (n = 137) | 17.62 ± 2.79 | 29.18 ± 4.38 | 13.07 ± 3.63 | 12.50 ± 4.20 |
| Former smoker (n = 147) | 17.74 ± 2.94 | 29.49 ± 4.50 | 11.56 ± 3.54 | 11.00 ± 4.08 | |
| Current smoker (n = 51) | 18,09 ± 2.58 | 30,33 ± 4.38 | 9.52 ± 4.33 | 9.15 ± 4.48 | |
| Life stress | Low (n = 58) | 17.17 ± 2.88 | 29.43 ± 3.81 | 11.74 ± 3.82 | 11.51 ± 4.37 |
| Moderate (n = 191) | 17.75 ± 2.65 | 29.58 ± 4.59 | 11.96 ± 3.80 | 11.57 ± 4.21 | |
| High (n = 86) | 18,10 ± 3,12 | 29.34 ± 4,53 | 11.75 ± 4,15 | 10,68 ± 4.56 | |
| Low (n = 109) | 17.33 ± 2.76 | 28.93 ± 4.72 | 10.55 ± 4.26 | 9.96 ± 4.67 | |
| Total Healthy Lifestyle | Moderate (n = 151) | 17.66 ± 2.90 | 29.63 ± 4.31 | 12.21 ± 3.60 | 11.69 ± 4.08 |
| High (n = 75) | 17.93 ± 2.81 | 30.02 ± 4.25 | 13.09 ± 3.32 | 12.61 ± 3.81 |
| Variable | Knowledge about HIV (K-HIV) | Variable | Attitudes and Perceived Self-Efficacy (SEA) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 1 | ||||||||||
| B | SE | β | p | 95% CI | B | SE | β | p | 95% CI | ||
| Age | 0.073 | 0.075 | 0.057 | 0.334 | [−0.075, 0.221] | Age | 0.188 | 0.119 | 0.094 | 0.117 | [−0.047, 0.423] |
| Sex | 0.391 | 0.381 | 0.056 | 0.306 | [−0.358, 1.139] | Sex | −0.910 | 0.604 | −0.084 | 0.133 | [−2.098, 0.279] |
| Relationship status | −0.076 | 0.338 | −0.012 | 0.822 | [−0.740, 0.588] | Relationship status | 0.506 | 0.536 | 0.052 | 0.346 | [−0.548, 1.560] |
| Employment status | 1.230 | 0.460 | 0.158 | 0.008 | [0.326, 2.135] | Employment status | −0.150 | 0.730 | −0.012 | 0.837 | [−1.586, 1.285] |
| Economic status | −0.019 | 0.449 | −0.002 | 0.966 | [−0.902, 0.864] | Economic status | −0.203 | 0.712 | −0.016 | 0.776 | [−1.604, 1.199] |
| Sexual orientation | −0.017 | 0.357 | −0.003 | 0.962 | [−0.719, 0.685] | Sexual orientation | 0.249 | 0.566 | 0.024 | 0.660 | [−0.865, 1.363] |
| F(6334) = 2.240, p = 0.039 R2 = 0.022 | F(6334) = 0.934, p = 0.471 R2 = −0.001 | ||||||||||
| Model 2 | Model 2 | ||||||||||
| B | SE | β | p | 95% CI | B | SE | β | p | 95% CI | ||
| Age | 0.045 | 0.078 | 0.035 | 0.564 | [−0.108, 0.198] | Age | 0.195 | 0.123 | 0.098 | 0.112 | [−0.046, 0.437] |
| Sex | 0.412 | 0.395 | 0.060 | 0.297 | [−0.365, 1.189] | Sex | −0.792 | 0.622 | −0.073 | 0.204 | [−2.015, 0.432] |
| Relationship status | −0.077 | 0.337 | −0.012 | 0.820 | [−0.740, 0.586] | Relationship status | 0.606 | 0.531 | 0.063 | 0.254 | [−0.438, 1.650] |
| Employment status | 1.259 | 0.459 | 0.161 | 0.006 | [0.357, 2.161] | Employment status | −0.211 | 0.722 | −0.017 | 0.770 | [−1.631, 1.209] |
| Economic status | 0.003 | 0.446 | 0.000 | 0.995 | [−0.874, 0.880] | Economic status | −0.108 | 0.702 | −0.009 | 0.878 | [−1.488, 1.273] |
| Sexual orientation | −0.052 | 0.359 | −0.008 | 0.885 | [−0.758, 0.654] | Sexual orientation | 0.189 | 0.565 | 0.019 | 0.738 | [−0.922, 1.300] |
| Diet | 0.032 | 0.052 | 0.036 | 0.537 | [−0.070, 0.133] | Diet | 0.160 | 0.081 | 0.115 | 0.049 | [0.001, 0.320] |
| Exercise | 0.073 | 0.032 | 0.135 | 0.023 | [0.010, 0.136] | Exercise | 0.112 | 0.050 | 0.132 | 0.026 | [0.013, 0.212] |
| Alcohol consumption | −0.057 | 0.036 | −0.098 | 0.110 | [−0.127, 0.013] | Alcohol consumption | −0.021 | 0.056 | −0.022 | 0.715 | [−0.131, 0.090] |
| Smoking | −0.372 | 0.246 | −0.093 | 0.132 | [−0.857, 0.113] | Smoking | −0.748 | 0.388 | −0.119 | 0.055 | [−1.511, 0.015] |
| Life stress | −0.086 | 0.138 | −0.036 | 0.535 | [−0.356, 0.185] | Life stress | 0.037 | 0.217 | 0.010 | 0.866 | [−0.389, 0.463] |
| F(11,334) = 2.171, p = 0.016 R2 = 0.037 ΔR2 = 0.029, p = 0.072 | F(11,334) = 1.977, p = 0.030 R2 = 0.031 ΔR2 = 0.046, p = 0.008 | ||||||||||
| Variable | Condom Use Intention (CUSEI) | Variable | Safe Sexual Behavior (SAS-B) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 1 | ||||||||||
| B | SE | β | p | 95% CI | B | SE | β | p | 95% CI | ||
| Age | −0.155 | 0.103 | −0.089 | 0.133 | [−0.358, 0.048] | Age | −0.204 | 0.113 | −0.105 | 0.073 | [−0.427, 0.019] |
| Sex | −0.088 | 0.521 | −0.009 | 0.866 | [−1.113, 0.936] | Sex | −0.377 | 0.573 | −0.036 | 0.512 | [−1.505, 0.751] |
| Relationship status | −1.165 | 0.462 | −0.138 | 0.012 | [−2.074, −0.257] | Relationship status | −1.770 | 0.509 | −0.188 | 0.001 | [−2.771, −0.770] |
| Employment status | −1.083 | 0.629 | −0.101 | 0.086 | [−2.321, 0.155] | Employment status | −1.189 | 0.693 | −0.099 | 0.087 | [−2.552, 0.174] |
| Economic status | 0.354 | 0.614 | 0.033 | 0.565 | [−0.854, 1.562] | Economic status | −0.031 | 0.676 | −0.003 | 0.963 | [−1.361, 1.299] |
| Sexual orientation | 0.710 | 0.488 | 0.080 | 0.147 | [−0.250, 1.670] | Sexual orientation | 0.641 | 0.537 | 0.064 | 0.234 | [−0.416, 1.698] |
| F(6334) = 2.742, p = 0.013 R2 = 0.030 | F(6334) = 4.203, p = 0.000 R2 = 0.054 | ||||||||||
| Model 2 | Model 2 | ||||||||||
| B | SE | β | p | 95% CI | B | SE | β | p | 95% CI | ||
| Age | −0.168 | 0.101 | −0.096 | 0.098 | [−0.367, 0.031] | Age | −0.197 | 0.114 | −0.101 | 0.084 | [−0.420, 0.027] |
| Sex | 0.206 | 0.514 | 0.022 | 0.688 | [−0.805, 1.217] | Sex | −0.074 | 0.576 | −0.007 | 0.898 | [−1.207, 1.059] |
| Relationship status | −1.156 | 0.438 | −0.137 | 0.009 | [−2.019, −0.294] | Relationship status | −1.751 | 0.492 | −0.185 | 0.000 | [−2.718, −0.784] |
| Employment status | −0.859 | 0.596 | −0.080 | 0.151 | [−2.032, 0.314] | Employment status | −0.971 | 0.669 | −0.081 | 0.147 | [−2.287, 0.344] |
| Economic status | 0.374 | 0.580 | 0.035 | 0.519 | [−0.767, 1.515] | Economic status | 0.011 | 0.650 | 0.001 | 0.986 | [−1.268, 1.290] |
| Sexual orientation | 0.975 | 0.467 | 0.109 | 0.038 | [0.057, 1.893] | Sexual orientation | 0.902 | 0.523 | 0.091 | 0.086 | [−0.128, 1.931] |
| Diet | 0.077 | 0.067 | 0.063 | 0.254 | [−0.055, 0.209] | Diet | 0.114 | 0.075 | 0.083 | 0.131 | [−0.034, 0.262] |
| Exercise | 0.062 | 0.042 | 0.084 | 0.136 | [−0.020, 0.144] | Exercise | 0.045 | 0.047 | 0.054 | 0.333 | [−0.047, 0.137] |
| Alcohol consumption | −0.090 | 0.046 | −0.112 | 0.053 | [−0.181, 0.001] | Alcohol consumption | −0.088 | 0.052 | −0.098 | 0.092 | [−0.190, 0.014] |
| Smoking | 1.384 | 0.320 | 0.251 | 0.000 | [0.754, 2.014] | Smoking | 1.269 | 0.359 | 0.206 | 0.000 | [0.562, 1.976] |
| Life stress | −0.052 | 0.179 | −0.016 | 0.771 | [−0.404, 0.300] | Life stress | 0.096 | 0.201 | 0.026 | 0.633 | [−0.299, 0.491] |
| F(11,334) = 5.849, p = 0.013 R2 = 0.138 ΔR2 = 0.118, p = 0.000 | F(11,334) = 5.455, p = 0.000 R2 = 0.128 ΔR2 = 0.085, p = 0.000 | ||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alcocer-Bruno, C.; Ferrer-Cascales, R.; Ruiz-Robledillo, N.; Sánchez-SanSegundo, M.; Zaragoza-Martí, A. Personal and Lifestyle Determinants of HIV Transmission Risk in Spanish University Students. Int. J. Environ. Res. Public Health 2020, 17, 8332. https://doi.org/10.3390/ijerph17228332
Alcocer-Bruno C, Ferrer-Cascales R, Ruiz-Robledillo N, Sánchez-SanSegundo M, Zaragoza-Martí A. Personal and Lifestyle Determinants of HIV Transmission Risk in Spanish University Students. International Journal of Environmental Research and Public Health. 2020; 17(22):8332. https://doi.org/10.3390/ijerph17228332
Chicago/Turabian StyleAlcocer-Bruno, Cristian, Rosario Ferrer-Cascales, Nicolás Ruiz-Robledillo, Miriam Sánchez-SanSegundo, and Ana Zaragoza-Martí. 2020. "Personal and Lifestyle Determinants of HIV Transmission Risk in Spanish University Students" International Journal of Environmental Research and Public Health 17, no. 22: 8332. https://doi.org/10.3390/ijerph17228332
APA StyleAlcocer-Bruno, C., Ferrer-Cascales, R., Ruiz-Robledillo, N., Sánchez-SanSegundo, M., & Zaragoza-Martí, A. (2020). Personal and Lifestyle Determinants of HIV Transmission Risk in Spanish University Students. International Journal of Environmental Research and Public Health, 17(22), 8332. https://doi.org/10.3390/ijerph17228332







