1. Introduction
Respiratory disease is one obvious consequence of inadequate housing [
1,
2,
3], and the risk increases as indoor temperatures fall below 16 °C [
3,
4]. More than half of the people admitted to hospital with a poverty-related condition are there because of a respiratory problem such as asthma, bronchiolitis, acute infection or pneumonia [
5]. According to the New Zealand Health Survey 2017/18, new respiratory disease affects 700,000 people, causes one in 10 hospital stays, costs New Zealand NZ
$7 billion in healthcare every year, and is the third-highest cause of death. One in eight adults (12.5%) and one in seven children (14.3%) have asthma [
6]. For all age groups, hospitalisation rates for asthma of Māori and Pasifika peoples are, respectively, 2.4 and 2.5 times higher than those of other ethnic groups, and hospitalisation rates for those in deprived homes are 2.3 times higher than those in the least deprived homes [
5,
6]. Respiratory diseases tend to be chronic in effect, are often developed in childhood and can shorten life expectancy [
7].
The World Health Organisation recommends a minimum indoor temperature of 18 °C for houses, and 20–21 °C for more vulnerable occupants, such as older people and young children [
8,
9]. It is widely acknowledged that low-quality housing affects occupants’ health and wellbeing [
1,
8,
10,
11]. Previous studies show that the minimum threshold indoor temperature required for limiting respiratory infections is 16 °C [
3,
4]. Indoor temperatures below 12 °C can cause short-term increases in blood pressure and blood viscosity, which may increase winter morbidity and mortality due to heart attacks and strokes. When elderly people are exposed to indoor temperatures of 9 °C or below for two or more hours, their deep body temperature can start decreasing [
12,
13,
14].
Most of the factors that adversely affect health, such as bacteria, viruses, fungi, mites, etc., have increases associated with high indoor relative humidity. Maintaining indoor relative humidity between 40% and 60% can minimise the indirect health effects [
15]. New Zealand has a temperate climate with comfortable warm, dry summers and mild, wet winters. Housing thermal design not only focuses on winter indoor thermal comfort but also indoor health conditions related to high relative humidity. The abundance of two major causes of allergy and trigger asthma, mites and mould, in New Zealand housing increases proportionately with a rise in average indoor relative humidity. For a new house with sufficient insulation and double-glazed windows in Auckland, in order to keep the winter indoor mean relative humidity at 50% and within the range of 40–60%, the winter indoor mean air temperatures have to be heated up to and maintained at 21–22 °C by a central-heating system in a temperate climate with a mild and wet winter [
16]. It is difficult and too expensive for houses only designed for temporary heating or without sufficient insulation to heat up the indoor air temperature of the whole house to 21–22 °C in order to maintain the indoor relative humidity below the thresholds of mould (60%) and mite (50%) survival and growth.
Both indoor relative humidity and temperature can impact indoor dust mite populations and allergen levels. Maintaining the indoor relative humidity below 50% can reduce dust mites and their allergens in the home; mite populations are almost eliminated in winter when indoor relative humidity is maintained within 40 to 50% [
17,
18,
19]. A range of 60–80% for relative humidity provides ideal conditions for the reproduction of mites. The indoor relative humidity required by dust mites to thrive is 75–80% or higher, and dust mites prefer temperatures of around 18–25 °C. A decrease in indoor temperature (between 10 °C and 25 °C) can result in lower dust mite populations [
17,
20,
21,
22,
23].
According to international and national standards, indoor relative humidity should be lower than 60% for optimum indoor air quality [
24,
25,
26]. The threshold of indoor relative humidity for mould survival and growth conditions is 60%. Mould growth is likely on almost any building material if the equilibrium relative humidity of the material exceeds 75–80% [
27,
28,
29]. Mould germination not only requires high relative humidity but also time (see
Table 1) [
30]. One option to prevent mould growth on indoor surfaces is to control the indoor relative humidity to a level below the threshold of mould germination [
31,
32].
The living environment experienced by indigenous communities in modern countries is often substandard, with consequent implications for health and wellbeing. In total, 19 sample houses of Māori communities in Minginui, Te Whaiti, Murupara, and Rotorua are used for this study. ‘Māori’ is the modern umbrella term used to refer to the Polynesian peoples who established residence in New Zealand from about 1250 AD [
33]. Sixteen sample houses (six houses in Minginui, five houses in Te Whaiti, and five houses in Murupara) without insulation or with limited old insulation were used for this study. Minginui, with 40 inhabited houses, is an old forestry town. Te Whaiti, with about 15 inhabited houses, is a village 8 km to the north of Minginui. Murupara is a small town with a population of 1650. The study area of Minginui, Te Whaiti, and Murupara is a remote and economically disadvantaged region, where the main industries are forestry and farming. As the three field-study sites are close to Rotorua, three sample houses with basic insulation of the Māori community in Rotorua were also used for this study. Rotorua has a temperate climate with mild and wet winters (see
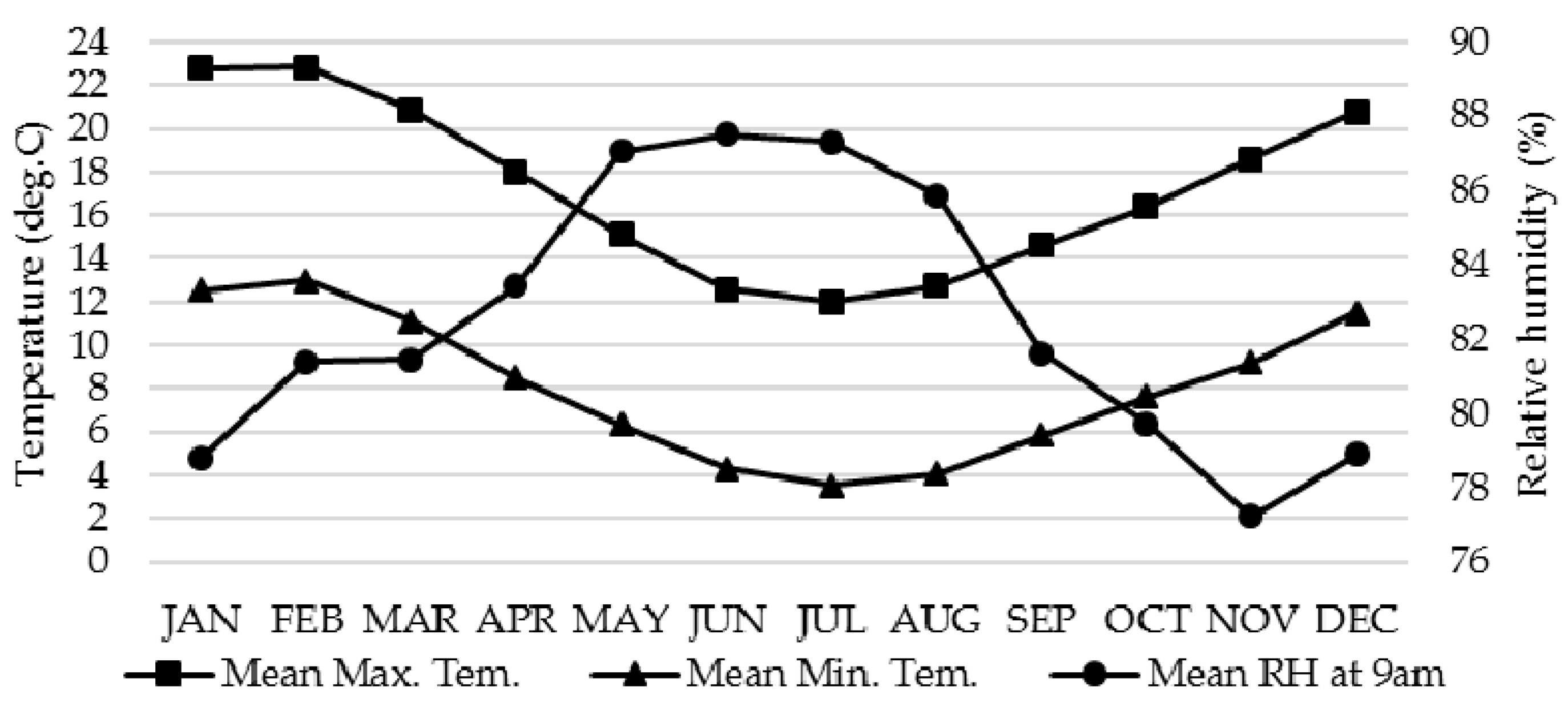
Figure 1).
The 16 sample houses with a light timber structure in Minginui, Te Whaiti, and Murupara were built in the 1920s to the 1970s. The floor areas of the 16 sample houses are 44 m2 to 342 m2. Roof materials are tin (eight houses), iron (five houses), aluminium (one house), tile (one house), and asbestos (one house). Wall materials are old weatherboard (14 houses), brick (one house), and concrete block (one house). Nine sample houses do not have any insulation in their envelopes; seven sample houses have only limited, old insulation in either their roof space only or both roof space and floor. For space heating, 12 sample houses used firewood as fuel for fireplaces, three sample houses used coal or firewood as fuel for stoves (cooking and space heating), one sample house did not use any space heating. Only one sample house used both a fireplace and an oil heater. Fifteen sample houses did not use any electricity as fuel for space heating. Three sample houses with the light timber structure in Rotorua were built in the 1980s to the 1990s with the basic insulation (Roof: 1.9, Wall: 1.5, Floor: 0.9) and single-glazed windows and used electronic heaters for space heating.
This study focuses on participants’ health conditions related to their living conditions (indoor thermal conditions and indoor allergens) of Māori communities in Minginui, Te Whaiti, Murupara and Rotorua of North Central Island of New Zealand. This study also provides guidelines or a strategy for new house development or retrofitting old house, with adequate space heating methods, to maintain indoor allergens at the acceptable level and to maintain healthy indoor conditions for occupants under the local climate with a mild and wet winter.
2. Methods
Field studies of the indoor microclimate of 19 sample houses (six houses in Minginui, five houses in Te Whaiti, five houses in Murupara and three houses in Rotorua) were carried out by the authors from March 2018 to January 2019. Air temperatures and relative humidity adjacent to floors and ceilings of different indoor spaces in the 19 sample houses and the shaded outdoor spaces under the eaves of the roofs were continuously measured and recorded at 15-min intervals, 24 h a day, by HOBO temperature and relative humidity (RH) loggers, from March 2018 to January 2019. All field-study data of the temperature and relative humidity of indoors and outdoors were converted into percentages of time in autumn and winter when indoor temperature and relative humidity were in different ranges for the purposes of identifying and comparing healthy indoor thermal conditions and identifying thresholds or ranges of indoor temperature and relative humidity related to mould germination, mould growth levels, the most common type of mould, and different levels of indoor dust-mite allergens. Field studies of dust-mite allergens and mould in 16 sample houses (13 sample houses in Minginui, Te Whaiti and Murupara; three sample houses in Rotorua) were carried out by the authors in the winter of 2018. According to the instructions for the Ventia™ Rapid Allergen Test, dust samples on the carpets of living rooms and bedrooms of the 16 sample houses were collected by a vacuum cleaner fitted with a DUSTREAM® collector, and dust samples were then tested using the Rapid Test cassette. Test results can identify four different levels of dust-mite allergens: 1. Undetectable dust-mite allergens. 2. Low levels of dust-mite allergens (less than 0.2 micrograms per gram of dust). 3. Medium levels of dust-mite allergens (0.2–1.0 micrograms per gram of dust). 4. High levels of dust-mite allergens (≥1 microgram per gram of dust). For level 1 and 2, no action is needed to reduce the indoor mite-allergen level (acceptable levels), for level 3 and 4, action should be taken to reduce indoor dust-mite allergen levels to protect occupants’ health (unacceptable levels). Field-study data of indoor microclimate and dust-mite allergen test data can be used to identify thresholds and ranges of indoor temperature and relative humidity associated with different levels of indoor dust-mite allergens. The threshold of indoor temperature and relative humidity associated with the low level (the acceptable level) of indoor dust-mite allergens can be used as a guideline for housing thermal design and space heating to minimise indoor allergy problems.
According to the instructions of Biodet Services Ltd. (consulting industrial microbiologists), the researchers used clear, standard Sellotape to collect mould samples from the indoor surface areas of the 16 sample houses (13 sample houses in Minginui, Te Whaiti and Murupara; 3 sample houses in Rotorua). The Sellotape with the mould samples was then folded in non-stick baking paper and placed into a plastic bag; the samples were then sent to the local testing laboratory where they were examined both macroscopically and microscopically. Field-study data of indoor temperature and relative humidity can be used to estimate whether or not, or when, mould spores can germinate. Field-study data of indoor microclimate and mould tests can be used to identify thresholds and ranges of indoor temperature and relative humidity associated with different levels of mould growth. Field-study data of the indoor microclimate and mould and dust-mite allergen test data can be used to identify correlations between dust-mite allergens and mould growth
The respiratory survey questionnaire used in this study was adapted from the European Community Respiratory Health Survey, which has been used for 200,000 participants to date. The major change in the survey was that the survey questions were converted to an online form which is easy for researchers to use [
34]. The questionnaire (total of 76 survey questions) investigates the participant’s basic health profile, respiratory symptom prevalence, risk factors, medication and related medical history, and all possible related factors. Research ethical approval (Application No. 2016–1007) was obtained from Unitec Research Ethics Committee (recognised by Health Research Council of New Zealand) before this study. After the occupants signed the consent form, the Respiratory Health Survey was carried out in 2018, and both Māori and English languages were used during the interviews and for explaining the questionnaire. A total of 23 occupants from 19 sample houses in Minginui, Te Whaiti, Murupara and Rotorua signed the consent form of the Respiratory Health Survey. In total, 20 participants from 15 sample houses in Minginui, Te Whaiti, Murupara and Rotorua finally took part in the Respiratory Health Survey. The Respiratory Health Survey results, field-study data of indoor temperature and relative humidity, and test data of dust mites and mould can be used to establish a relationship between occupants’ respiratory health conditions and indirect indoor health effects such as dust mites and mould.
4. Discussion
Based on field-study data of indoor microclimates, dust-mite allergens and mould growth, and occupants’ Respiratory Health Survey data from the sample houses with insufficient insulation and poor thermal performance, the study provided evidence and physical data to prove that poor health conditions of occupants are closely related to their poor indoor living conditions. Houses with poor thermal performance and insufficient insulation can have extremely low indoor temperatures and serious indoor allergens from dust mites and mould, which can directly harm or negatively impact occupants’ health.
The study identified that not only in winter, but also in autumn, the indoor relative humidity of the sample houses with insufficient insulation met the threshold conditions for mould to germinate and dust mites to thrive. Some sample houses were likely to have had dust mite and mould problems during the autumn and a worse situation during the winter. Occupants could suffer from dust-mite and mould allergies for a long period of time every year. The study identified strong correlations between dust-mite and mould problems in indoor spaces of the sample houses with insufficient insulation. If a house had a dust-mite allergen problem (medium or high levels of dust-mite allergens), it was likely to have a mould problem, and vice versa, in a temperate climate with mild and wet winters.
Dust mites and mould prefer warm and humid conditions. If temporary space heating in a house with insufficient insulation cannot increase the indoor temperature to a level that can decrease and maintain the indoor relative humidity below the threshold for mould to germinate and dust mites to thrive, the limited increase in indoor air temperature (a couple of degrees increase from a very low baseline) can create a better thermal condition for dust mite development and mould growth, and indoor health conditions can become worse.
For a local conventional house with lightweight timber structure, designed for temporary heating, under a temperate climate with a mild and wet winter, it is possible for a house (a retrofitting old house or a new house) with sufficient insulation in its building envelope and temporary space heating to maintain indoor health living conditions. Sufficient insulation and double-glazed windows could raise the baseline winter indoor temperatures and significantly reduce indoor mean relative humidity; it would then be possible in those houses with adequate temporary space heating to maintain the indoor relative humidity below the threshold for mould to germinate and dust mites to thrive. If there were no mould spore germination, there would be no problem of mould growth on indoor surfaces. If dust-mite allergens were controlled at a low or undetectable level, there would be no dust-mite allergy problems in indoor spaces.
This is the first state-funded, cross-disciplinary collaborative research project studying the health and living conditions of an isolated indigenous community in remote areas of New Zealand. The study provides first-hand field study data and physical evidence to identify that the poor health of occupants of the isolated Māori communities is closely related to their inadequate living conditions, which can attract the government and health authority’s attention to occupants’ health conditions and their living conditions in remote and economically disadvantaged regions of New Zealand. A new housing project with 33 new houses, funded by the Ministry of Māori Development in 2020, is going to be developed by Matekuare Whanau Trust for the local Māori residents at the same study site (Te Whaiti). The new housing development can potentially become a national sample of affordable, healthy and sustainable housing development for the isolated Māori communities. The new houses can be used for a further comparison study of occupants’ health conditions with different living conditions of the local Māori community.
The sites for the field studies and the Respiratory Health Survey for the isolated Māori communities are in the remote areas with a very low population density. Maori occupants in those communities have very large variation of residential mobility in different families due to many different reasons. This residential mobility may affect the duration of living in dwellings. It is difficult for the Respiratory Health Survey to have a large number of participants who are the owners of the sample houses or the long-term tenants of the sample houses. Although the sample size of the respiratory survey results was small, a strong correlation between the respiratory survey results and dust mite and mould test results can be still identified. The extremely high percentages of occupants who had respiratory symptoms were strongly associated with the high levels of indoor dust mites and mould allergens in the sample houses in the Minginui, Te Whaiti and Murupara areas. The low percentages of participants who had respiratory symptoms were apparently associated with the low levels of indoor dust mites and mould allergens in the sample houses in Rotorua.