Perfectionism and Pain Intensity in Women with Fibromyalgia: Its Influence on Activity Avoidance from The Contextual Perspective
Abstract
1. Introduction
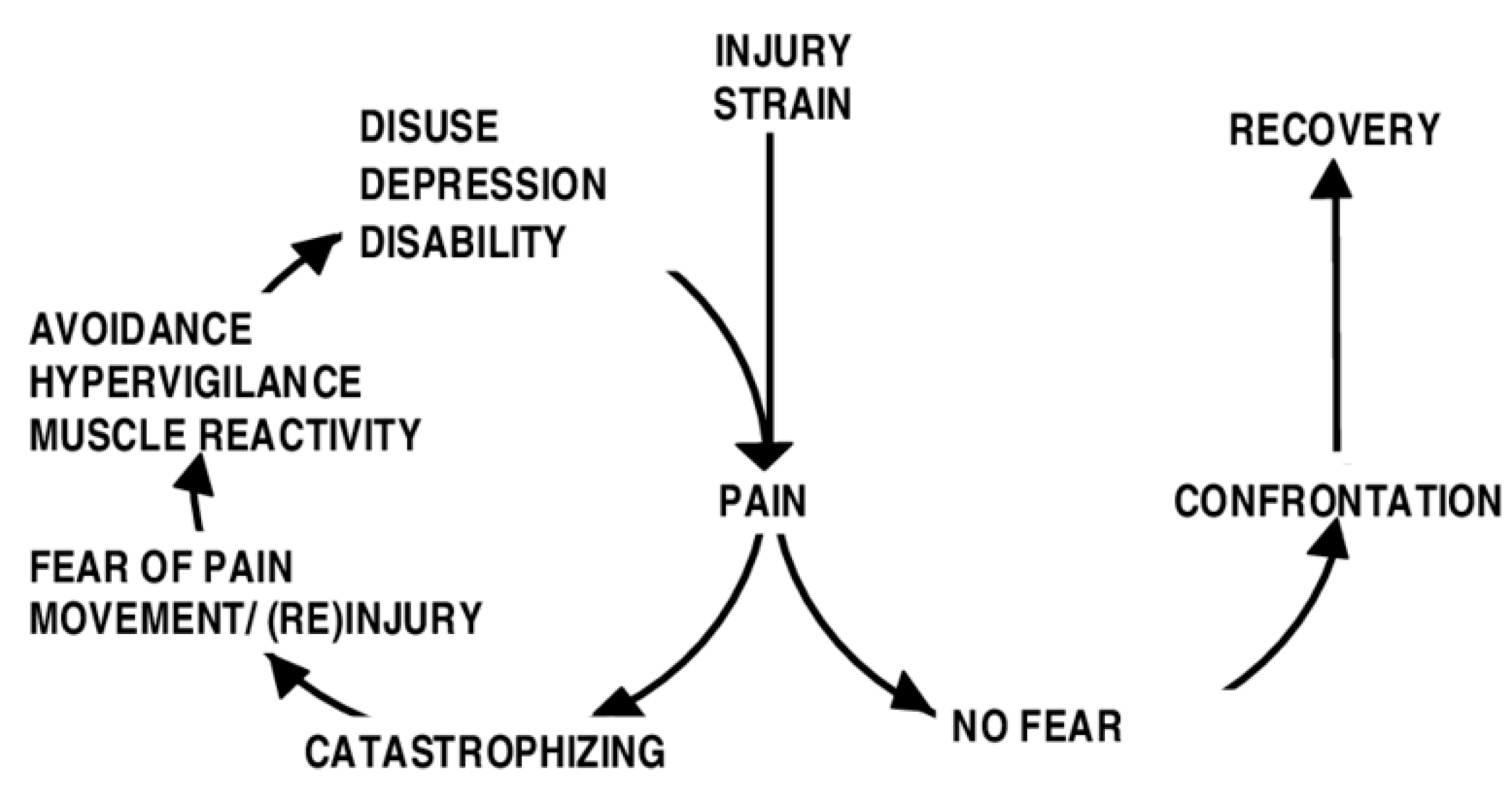
1.1. Activity Avoidance, Fear of Movement and Disability
1.2. Perfectionism and Fibromyalgia. A Contextual-Functional Approach
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Data Analysis
3. Results
3.1. Sociodemographic and Clinical Data of The Study
3.2. Means, Standard Deviations, and Pearson Correlations between Study Variables
3.3. Regression Including Moderation Analyses
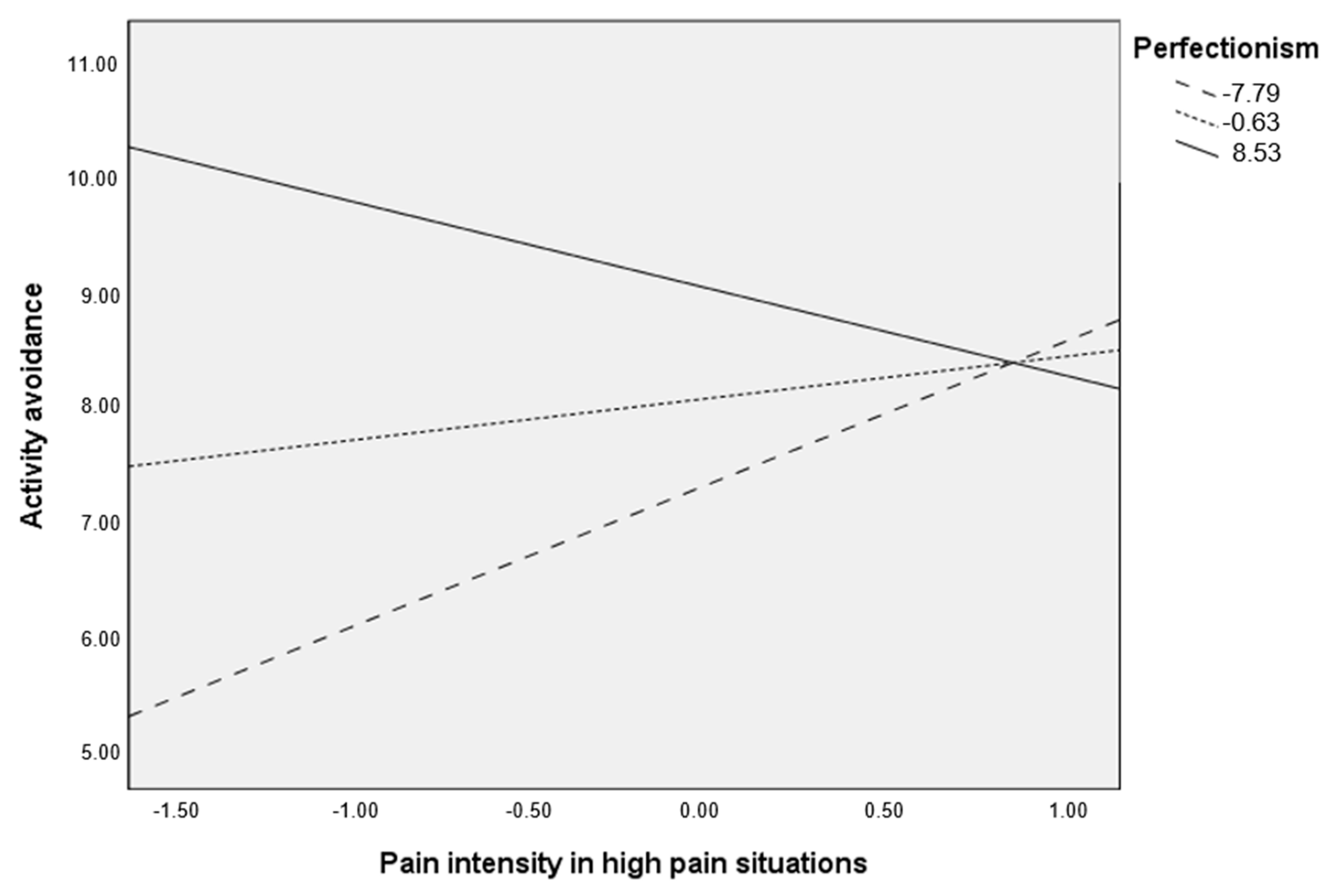
3.3.1. High Severity Group
3.3.2. Low/Moderate Severity Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Velasco, L.; Gutierrez-Hermoso, L.; Mateos-Pintado, B.; de Castro, D.G.; Blanco Rico, S.; Sanroman Canelada, L.; Lopez-Roig, S.; Pastor Mira, M.A.; Peñacoba Puente, C. The 4 U’s Rule of Fibromyalgia: A Proposed Model for Fatigue in a Sample of Women with Fibromyalgia: A Qualitative Study. Int. J. Environ. Res. Public Health 2020, 17, 6224. [Google Scholar] [CrossRef] [PubMed]
- Ojeda, B.; Dueñas, M.; Salazar, A.; Mico, J.A.; Torres, L.M.; Failde, I. Factors influencing cognitive impairment in neuropathic and musculoskeletal pain and fibromyalgia. Pain Med. 2018, 3, 499–510. [Google Scholar] [CrossRef]
- Diaz-Piedra, C.; Di Stasi, L.L.; Baldwin, C.M.; Buela-Casal, G.; Catena, A. Sleep disturbances of adult women suffering from fibromyalgia: A systematic review of observational studies. Sleep Med. Rev. 2015, 21, 86–99. [Google Scholar] [CrossRef] [PubMed]
- Galvez-Sánchez, C.M.; Duschek, S.; Reyes del Paso, G.A. Psychological impact of fibromyalgia: Current perspectives. Psychol. Res. Behav. Manag. 2019, 12, 117–127. [Google Scholar] [CrossRef]
- Wolfe, F.; Smythe, H.A.; Yunus, M.B.; Bennett, R.M.; Bombardier, C.; Goldenberg, D.L.; Tugwell, P.; Campbell, S.M.; Abeles, M.; Clark, P.; et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum. Off. J. Am. Coll. Rheumatol. 1990, 33, 160–172. [Google Scholar] [CrossRef]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Katz, R.S.; Mease, P.; Russell, A.S.; Russell, I.J.; Winfield, J.B.; Yunus, M.B. The American College of Rheumatology Preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 2010, 62, 600–610. [Google Scholar] [CrossRef]
- Boomershine, C. Fibromyalgia: The Prototypical Central Sensitivity Syndrome. Curr. Rheumatol. Rev. 2015, 11, 131–145. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, B.; Baptista, T.M.; Branco, J.C.; Novo, R. Fibromyalgia characterization in a psychosocial approach. Psychol. Health Med. 2015, 20, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Salli, A.; Yilmaz, H.; Ugurlu, H. The relationship between tender point count and disease severity in patients with primary fibromyalgia. Rheumatol. Int. 2012, 32, 105–107. [Google Scholar] [CrossRef]
- Zhao, Y.C.; Hu, T.; Chen, Y.; Du, K.T. Elevated Serum Levels of Monocyte Chemotactic Protein-1/Chemokine C-C Motif Ligand 2 are Linked to Disease Severity in Patients with Fibromyalgia Syndrome. Balk. Med. J. 2019, 36, 331–336. [Google Scholar] [CrossRef]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Häuser, W.; Katz, R.L.; Mease, P.J.; Russell, A.S.; Russell, I.J.; Walitt, B. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin. Arthritis Rheum. 2016, 46, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-de-la-Peña, M.T.; Triñanes, Y.; González-Villar, A.; Romero-Yuste, S.; Gómez-Perretta, C.; Arias, M.; Wolfe, F. Convergence between the 1990 and 2010 ACR diagnostic criteria and validation of the Spanish version of the Fibromyalgia Survey Questionnaire (FSQ). Rheumatol. Int. 2015, 35, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Clauw, D.J. Fibromyalgia: A clinical review. JAMA 2014, 311, 1547–1555. [Google Scholar] [CrossRef] [PubMed]
- Crombez, G.; Eccleston, C.; Van Damme, S.; Vlaeyen, J.W.; Karoly, P. Fear-Avoidance Model of Chronic Pain: The next generation. Clin. J. Pain. 2012, 28, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Estévez-López, F.; Álvarez-Gallardo, I.C.; Segura-Jiménez, V.; Soriano-Maldonado, A.; Borges-Cosic, M.; Pulido-Martos, M.; Aparicio, V.A.; Carbonell-Baeza, A.; Delgado- Fernández, M.; Geenen, R. The discordance between subjectively and objectively measured physical function in women with fibromyalgia: Association with catastrophizing and self-efficacy cognitions. The al-Ándalus project. Disabil. Rehabil. 2018, 40, 329–337. [Google Scholar] [CrossRef]
- Häuser, W.; Ablin, J.; Fitzcharles, M.A.; Littlejohn, G.; Luciano, J.V.; Usui, C.; Walitt, B. Fibromyalgia. Nat. Rev. 2015, 1, 1–16. [Google Scholar] [CrossRef]
- Peñacoba, C.; Pastor, M.Á.; López-Roig, S.; Sanz, Y.; Velasco, L. Healthcare Provider Advice to Engage in Walking Regimens and Adherence in Women With Fibromyalgia. Rehabil. Nurs. 2019, 44, 20–28. [Google Scholar] [CrossRef]
- Santos, A.M.; Campos, E.; Párraga-Montilla, J.A.; Aragón-Vela, J.; Latorre-román, P.A. Effects of a functional training program in patients with fibromyalgia: A 9-year prospective longitudinal cohort study. Scand. J. Med. Sci. Sports 2020, 30, 904–913. [Google Scholar] [CrossRef] [PubMed]
- Heneweer, H.; Staes, F.; Aufdemkampe, G.; van Rijn, M.; Vanhees, L. Physical activity and low back pain: A systematic review of recent literature. Eur. Spine J. 2011, 20, 826–845. [Google Scholar] [CrossRef] [PubMed]
- Gavilán-Carrera, B.; Segura-Jiménez, V.; Estévez-López, F.; Álvarez-Gallardo, I.C.; Soriano-Maldonado, A.; Borges-Cosica, M.; Herrador-Colmenero, M.; Acosta-Manzano, P.; Delgado-Fernández, M. Association of sedentary time and physical activity with pain, fatigue, and impact of fibromyalgia: The al-Ándalus study. Scand. J. Med. Sci. Sports 2017, 27, 83–92. [Google Scholar] [CrossRef]
- Mcloughlin, M.J.; Colbert, L.H.; Stegner, A.J.; Cook, D.B. Are Women with Fibromyalgia Less Physically Active than Healthy Women? Med. Sci. Sports Exerc. 2011, 43, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Dailey, D.L.; Frey Law, L.A.; Vance, C.G.T.; Rakel, B.A.; Merriwether, E.N.; Darghosian, L.; Golchha, M.; Geasland, K.M.; Spitz, R.; Crofford, L.J.; et al. Perceived function and physical performance are associated with pain and fatigue in women with fibromyalgia. Arthritis Res. Ther. 2016, 18, 68. [Google Scholar] [CrossRef] [PubMed]
- Vlaeyen, J.W.; Kole-Snijders, A.M.J.; Boeren, R.G.B.; van Eek, H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain 1995, 62, 363–372. [Google Scholar] [CrossRef]
- Nijs, J.; Roussel, N.; Van Oosterwijck, J.; De Kooning, M.; Ickmans, K.; Struyf, F.; Meeus, M.; Lundberg, M. Fear of movement and avoidance behaviour toward physical activity in chronic-fatigue syndrome and fibromyalgia: State of the art and implications for clinical practice. Clin. Rheumatol. 2013, 32, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Pastor-Mira, M.A.; López-Roig, S.; Martínez-Zaragoza, F.; León, E.; Abad, E.; Lledó, A.; Peñacoba, C. Goal preferences, affect, activity patterns and health outcomes in women with fibromyalgia. Front. Psychol. 2019, 10, 1912. [Google Scholar] [CrossRef] [PubMed]
- McCracken, L.M. Committed Action: An Application of the Psychological Flexibility Model to Activity Patterns in Chronic Pain. J. Pain 2013, 14, 828–835. [Google Scholar] [CrossRef]
- Suso-Ribera, C.; García-Palacios, A.; Botella, C.; Ribera-Canudas, M.V. Pain catastrophizing and its relationship with health outcomes: Does pain intensity matter? Pain Res. Manag. 2017, 2017, 9762864. [Google Scholar] [CrossRef]
- Gonzalez, B.; Baptista, T.M.; Branco, J.C. Life history of women with fibromyalgia: Beyond the illness. Qual. Rep. 2015, 20, 526–540. [Google Scholar]
- Sirois, F.M.; Molnar, D.S. Perfectionism and Maladaptive Coping Styles in Patients with Chronic Fatigue Syndrome, Irritable Bowel Syndrome and Fibromyalgia/Arthritis and in Healthy Controls. Psychother. Psychosom. 2014, 83, 384–385. [Google Scholar] [CrossRef]
- Sirois, F.M.; Toussaint, L.; Hirsch, J.K.; Kohls, N.; Weber, A.; Offenbächer, M. Trying to be perfect in an imperfect world: A person-centred test of perfectionism and health in fibromyalgia patients versus healthy controls. Pers. Individ. Dif. 2019, 137, 27–32. [Google Scholar] [CrossRef]
- Pinto, A.; Pereira, A.; Costa, C.; Marqeus, M.; da Silva, J.A.P.; Marcelo, A. AB0841 Perfectionism in Chronic Pain: Are There Differences between fibromyalgia, Rheumatoid Arthritis and Healthy Controls. Ann. Rheum. Dis. 2016, 75, 1190. [Google Scholar] [CrossRef]
- Delor, B.; Douilliez, C.; Philippot, P. Une approche transdiagnostique et basée sur les processus du perfectionnisme inadapté = A transdiagnostic and process-based approach of maladaptive perfectionism. Rev. Francoph. Clin. Comport. Cogn. 2019, 24, 20–38. [Google Scholar]
- Treatment of Clinical Perfectionism Using Acceptance and Commitment Therapy. Available online: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2020-67315-256&site=ehost-live&scope=site (accessed on 16 July 2020).
- Crosby, J.M.; Bates, S.C.; Twohig, M.P. Examination of the relationship between perfectionism and religiosity as mediated by psychological inflexibility. Curr. Psychol. 2011, 30, 117–129. [Google Scholar] [CrossRef]
- Bisgaier, S. Acceptance and Commitment Therapy for the Treatment of Perfectionism. In Dissertation Abstracts International: Section B: The Sciences and Engineering; 2018; Volume 35, p. 10–B (E). Available online: http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2018-34221-159&site=ehost-live&scope=site (accessed on 21 July 2020).
- Kempke, S.; Luyten, P.; Mayes, L.C.; van Houdenhove, B.; Claes, S. Self-critical perfectionism predicts lower cortisol response to experimental stress in patients with chronic fatigue syndrome. Health Psychol. 2016, 35, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Molnar, D.S.; Flett, G.L.; Sadava, S.W.; Colautti, J. Perfectionism and health functioning in women with fibromyalgia. J. Psychosom. Res. 2012, 73, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, B.; Novo, R.; Ferreira, A.S. Fibromyalgia: Heterogeneity in personality and psychopathology and its implications. Psychol. Health Med. 2019, 25, 703–709. [Google Scholar] [CrossRef]
- Randall, E.T.; Gray, L.S.; Fletcher, A.A. Topical Review: Perfectionism and Pediatric Chronic Pain: Theoretical Underpinnings, Assessment, and Treatment. J. Pediatric Psychol. 2018, 43, 326–330. [Google Scholar] [CrossRef]
- Randall, E.; Smith, K.; Perron, V.; Robbins, H.; Smith, A.; Conroy, C.; Simons, L. Feeling the pressure to be perfect: The role of child and parental perfectionism on pain, pain-related distress, and functional disability. In Proceedings of the Society of Pediatric Psychology Annual Conference, Portland, OR, USA, 30 March–1 April 2017. [Google Scholar]
- Van Koulil, S.; Kraaimaat, V.; van Lankveld, W.; van Helmond, T.; Vedder, A.; van Hoorn, H.; Cats, H.; van Riel, P.L.C.M.; Evers, A.W.M. Screening for pain-persistence and pain-avoidance patterns in fibromyalgia. Int. J. Behav. Med. 2008, 15, 211–220. [Google Scholar] [CrossRef]
- Angarita-Osorio, N.; Angarita-Osorio, N.; Pérez-Aranda, A.; Feliu-Soler, A.; Andrés-Rodríguez, L.; Borràs, X.; Suso-Ribera, C.; Slim, M.; Herrera-Mercadal, P.; Fernández-Vergel, R.; et al. Patients With Fibromyalgia Reporting Severe Pain but Low Impact of the Syndrome: Clinical and Pain-Related Cognitive Features. Pain Pract. 2020, 20, 255–261. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Esteve, R.; Ramírez-Maestre, C.; Peters, M.L.; Serrano-Ibáñez, E.R.; Ruíz-Párraga, G.T.; López-Martínez, A.E. Development and initial validation of the activity patterns scale in patients with chronic pain. J. Pain. 2016, 17, 451–461. [Google Scholar] [CrossRef] [PubMed]
- Gelabert, E.; García-Esteve, L.; Martín-Santos, R.; Gutiérrez, F.; Torres, A.; Subirà, S. Psychometric properties of the Spanish version of the Frost Multidimensional Perfectionism Scale in women. Psicothema 2011, 23, 133–139. [Google Scholar] [PubMed]
- Sirois, F.M.; Molnar, D.S. Perfectionistic strivings and concerns are differentially associated with self-rated health beyond negative affect. J. Res. Pers. 2017, 70, 73–83. [Google Scholar] [CrossRef]
- Molnar, D.S.; Sadava, S.W.; Flett, G.L.; Colautti, J. Perfectionism and health: A mediational analysis of the roles of stress, social support and health-related behaviours. Psychol. Health. 2012, 27, 846–864. [Google Scholar] [CrossRef]
- Jensen, M.P.; Turner, L.R.; Turner, J.A.; Romano, J.M. The use of multiple-item scales for pain intensity measurement in chronic pain patients. Pain 1996, 67, 35–40. [Google Scholar] [CrossRef]
- Jensen, M.P.; Turner, J.A.; Romano, J.M.; Fisher, L.D. Comparative reliability and validity of chronic pain intensity measures. Pain 1999, 83, 157–162. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach; Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- Eccleston, C.; Crombez, G. Worry and chronic pain: A misdirected problem solving model. Pain 2007, 132, 233–236. [Google Scholar] [CrossRef]
- Aldrich, S.; Eccleston, C.; Crombez, G. Worrying about chronic pain: Vigilance to threat and misdirected problem solving. Behav. Res. Ther. 2000, 38, 457–470. [Google Scholar] [CrossRef]
- Tavallaii, A.; Kargar, K.H.; Farzanegan, G.H.; Saeidi, S.Y.; Radfar, S. Personality characteristics of patients with chronic low back pain. Procedia -Soc. Behav. Sci. 2010, 5, 372–376. [Google Scholar] [CrossRef][Green Version]
- McCracken, L.M.; Morley, S. The Psychological Flexibility Model: A Basis for Integration and Progress in Psychological Approaches to Chronic Pain Management. J. Pain 2014, 15, 221–234. [Google Scholar] [CrossRef]
- Estévez-López, F.; Segura-Jiménez, V.; Álvarez-Gallardo, I.C.; Borges-Cosic, M.; Pulido-Martos, M.; Carbonell-Baeza, A.; Aparicio, V.A.; Geenen, R.; Delgado-Fernández, M. Adaptation profiles comprising objective and subjective measures in fibromyalgia: The al-Ándalus project. Rheumatology 2017, 56, 2015–2024. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fleeson, W.; Jayawickreme, E. Whole Trait Theory. J. Res Pers. 2015, 1, 82–92. [Google Scholar] [CrossRef] [PubMed]
- Keefe, R.; Goldberg, T.E.; Harvey, P.D.; Gold, J.; Poe, M.; Coughenour, L. The Brief Assessment of Cognition in Schizophrenia: Reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr. Res. 2004, 68, 283–297. [Google Scholar] [CrossRef] [PubMed]
- Wong, W.S.; Chen, P.P.; Yap, J.; Mak, K.H.; Tam, B.K.H.; Fielding, R. Assessing depression in patients with chronic pain: A comparison of three rating scales. J. Affect. Disord. 2011, 133, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Longbottom, J.L.; Robert Grove, J.; Dimmock, J.A. An examination of perfectionism traits and physical activity motivation. Psychol. Sport Exerc. 2010, 11, 574–581. [Google Scholar] [CrossRef]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: The process and Practice of Mindful Change; Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Suso-Ribera, C.; Camacho-Guerrero, L.; Osma, J.; Suso-Vergara, S.; Gallardo-Pujo, D. A Reduction in Pain Intensity Is More Strongly Associated with Improved Physical Functioning in Frustration Tolerant Individuals. J. Clin. Psychol. Med. Settings 2016, 23, 192–206. [Google Scholar] [CrossRef]
- Loevinger, B.L.; Shirtcliff, E.A.; Muller, D.; Alonso, C.; Coe, C.L. Delineating psychological and biomedical profiles in a heterogeneous fibromyalgia population using cluster analysis. Clin. Rheumatol. 2012, 31, 677–685. [Google Scholar] [CrossRef]
- Egan, S.; Wade, T.; Shafran, R.; Antony, M. Cognitive Behavioral Treatment of Perfectionism; Guilford Press: New York, NY, USA, 2014. [Google Scholar]
- Brooks, S.K.; Rimes, K.A.; Chalder, T. The role of acceptance in chronic fatigue syndrome. J. Psychosom. Res. 2011, 71, 411–415. [Google Scholar] [CrossRef]
- Wimberley, T.E.; Mintz, L.B.; Suh, H. Perfectionism and mindfulness: Effectiveness of a bibliotherapy intervention. Mindfulness 2016, 7, 433–444. [Google Scholar] [CrossRef]
- Lin, J.; Klatt, L.I.; McCracken, L.M.; Baumeister, H. Psychological flexibility mediates the effect of an online-based acceptance and commitment therapy for chronic pain: An investigation of change processes. Pain 2018, 159, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Esteve, R.; López-Martínez, A.E.; Peters, M.L.; Serrano-Ibáñez, E.R.; Ruíz-Párraga, G.T.; González-Gómez, H.; Ramírez-Maestre, C. Activity Pattern Profiles: Relationship with Affect, Daily Functioning, Impairment, and Variables Related to Life Goals. J. Pain 2017, 18, 546–555. [Google Scholar] [CrossRef] [PubMed]
- McCracken, L.M.; Vowles, K.E.; Zhao-O’Brien, J. Further development of an instrument to assess psychological flexibility in people with chronic pain. J. Behav. Med. 2010, 33, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Van Koulil, S.; Kraaimaat, F.W.; Van Lankveld, W.; Van Helmond, T.; Vedder, A.; Van Hoorn, H.; Donders, A.R.T.; Thieme, K.; Cats, H.; Van Riel, P.L.C.M.; et al. Cognitive-behavioral mechanisms in a pain-avoidance and a pain-persistence treatment for high-risk fibromyalgia patients. Arthritis Rheum. 2011, 63, 800–807. [Google Scholar] [CrossRef] [PubMed]
- Ong, C.W.; Lee, E.B.; Krafft, J.; Terry, C.L.; Barrett, T.S.; Levin, M.E.; Twohig, M.P. A randomized controlled trial of acceptance and commitment therapy for clinical perfectionism. J. Obs. -Compuls. Relat. Disord. 2019, 22, 100444. [Google Scholar] [CrossRef]
- Vlaeyen, J.W.S.; Crombez, G. Behavioral Conceptualization and Treatment of Chronic Pain. Annu. Rev. Clin. Psychol. 2020, 16, 187–212. [Google Scholar] [CrossRef]

| Variable | Fibromyalgia Women (n = 228) |
|---|---|
| Age, mean (SD) | 56.91 (8.94) |
| Education level, n (%) No studies Primary Secondary University | 31 (13.5) 121 (53.1) 61 (26.8) 15 (6.6) |
| Marital Status, n (%) Married Single Widowed/separated | 121 (53) 25 (11) 82 (36) |
| Employment status, n (%) Currently employed Unemployed Sick leave Retired Retired due to disability Housewife | 27 (11.8) 28 (11.9) 24 (10.5) 33 (14.5) 42 (18.8) 74 (32.5) |
| Pain, mean (SD) | 7.15 (1.52) |
| Time from fibromyalgia diagnosis, mean (SD) | 12.14 (8.45) |
| Variable | Mean (SD) | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. Activity avoidance | 7.45 (2.71) | 0.27 ** | 0.24 ** | 0.29 ** |
| 2. Perfectionism | 22.09 (7.65) | 0.03 | <0.01 | |
| 3. Pain intensity in LPS | 5.58 (2.09) | 0.48 ** | ||
| 4. Pain intensity in HPS | 8.44 (1.52) |
| Variable | R2 | F | p | Beta | t | p | 95% CI |
|---|---|---|---|---|---|---|---|
| High disease severity group | |||||||
| DV = Activity avoidance | 0.16 | 7.71 | <0.001 | ||||
| Pain intensity in HPS | 0.29 | 1.15 | 0.24 | −20, 0.78 | |||
| Perfectionism | 0.10 | 4.05 | <0.001 | 0.05, 0.15 | |||
| Interaction | −0.12 | −3.19 | 0.002 | −0.20, −0.05 | |||
| DV = Activity avoidance | 0.10 | 4.37 | 0.005 | ||||
| Pain intensity in LPS | 0.14 | 1.25 | 0.21 | −0.08, 0.37 | |||
| Perfectionism | 0.08 | 3.44 | <0.001 | 0.04, 0.14 | |||
| Interaction | <0.001 | 0.11 | 0.91 | −0.02, 0.03 | |||
| Low/moderate disease severity group | |||||||
| DV = Activity avoidance | 0.14 | 5.49 | 0.001 | ||||
| Pain intensity in HPS | 0.38 | 2.07 | 0.04 | 0.02, 0.76 | |||
| Perfectionism | 0.11 | 2.85 | 0.005 | 0.03, 0.18 | |||
| Interaction | 0.06 | 2.40 | 0.018 | 0.01, 0.11 | |||
| DV = Activity avoidance | 0.07 | 2.57 | 0.058 | ||||
| Pain intensity in LPS | 0.12 | 0.67 | 0.50 | −0.24, 0.50 | |||
| Perfectionism | 0.09 | 2.36 | 0.02 | 0.01, 0.16 | |||
| Interaction | 0.03 | 1.14 | 0.25 | −0.02, 0.08 |
| Perfectionism | Beta (Pain Intensity in HPS) | t | p | 95% CI |
|---|---|---|---|---|
| −7.78 | 1.238 | 3.127 | 0.002 | 0.454, 2.022 |
| −0.63 | 0.363 | 1.451 | 0.149 | −0.132, 0.859 |
| 8.53 | −0.756 | −1.880 | 0.062 | −1.551, 0.04 |
| Perfectionism | Beta (Pain Intensity in HPS) | t | p | 95% CI |
|---|---|---|---|---|
| −7.40 | −0.063 | −0.240 | 0.810 | −0.584, 0.458 |
| −0.40 | 0.362 | 1.942 | 0.054 | −0.008, 0.732 |
| 7.59 | 0.849 | 3.148 | 0.002 | 0.314, 1.383 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheila, B.; Octavio, L.-R.; Patricia, C.; Dolores, B.; Lilian, V.; Cecilia, P. Perfectionism and Pain Intensity in Women with Fibromyalgia: Its Influence on Activity Avoidance from The Contextual Perspective. Int. J. Environ. Res. Public Health 2020, 17, 8442. https://doi.org/10.3390/ijerph17228442
Sheila B, Octavio L-R, Patricia C, Dolores B, Lilian V, Cecilia P. Perfectionism and Pain Intensity in Women with Fibromyalgia: Its Influence on Activity Avoidance from The Contextual Perspective. International Journal of Environmental Research and Public Health. 2020; 17(22):8442. https://doi.org/10.3390/ijerph17228442
Chicago/Turabian StyleSheila, Blanco, Luque-Reca Octavio, Catala Patricia, Bedmar Dolores, Velasco Lilian, and Peñacoba Cecilia. 2020. "Perfectionism and Pain Intensity in Women with Fibromyalgia: Its Influence on Activity Avoidance from The Contextual Perspective" International Journal of Environmental Research and Public Health 17, no. 22: 8442. https://doi.org/10.3390/ijerph17228442
APA StyleSheila, B., Octavio, L.-R., Patricia, C., Dolores, B., Lilian, V., & Cecilia, P. (2020). Perfectionism and Pain Intensity in Women with Fibromyalgia: Its Influence on Activity Avoidance from The Contextual Perspective. International Journal of Environmental Research and Public Health, 17(22), 8442. https://doi.org/10.3390/ijerph17228442





