Modelling Potential Geographical Access of the Population to Public Hospitals and Quality Health Care in Romania
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Methods
2.3. Data
2.3.1. Population Data
2.3.2. Hospitals and Physicians Data
2.3.3. Google Maps API Data
2.4. Accessibility Indicators
Accessibility Index (ISA)
2.5. Study Limits
3. Results and Discussion
3.1. The Hospital: A Central Role in the Delivery of Health Care in Romania
3.2. Modelling Potential Geographical Access of the Population to Public Hospitals
3.2.1. Potential Geographical Access of the Population to All Categories of Hospitals
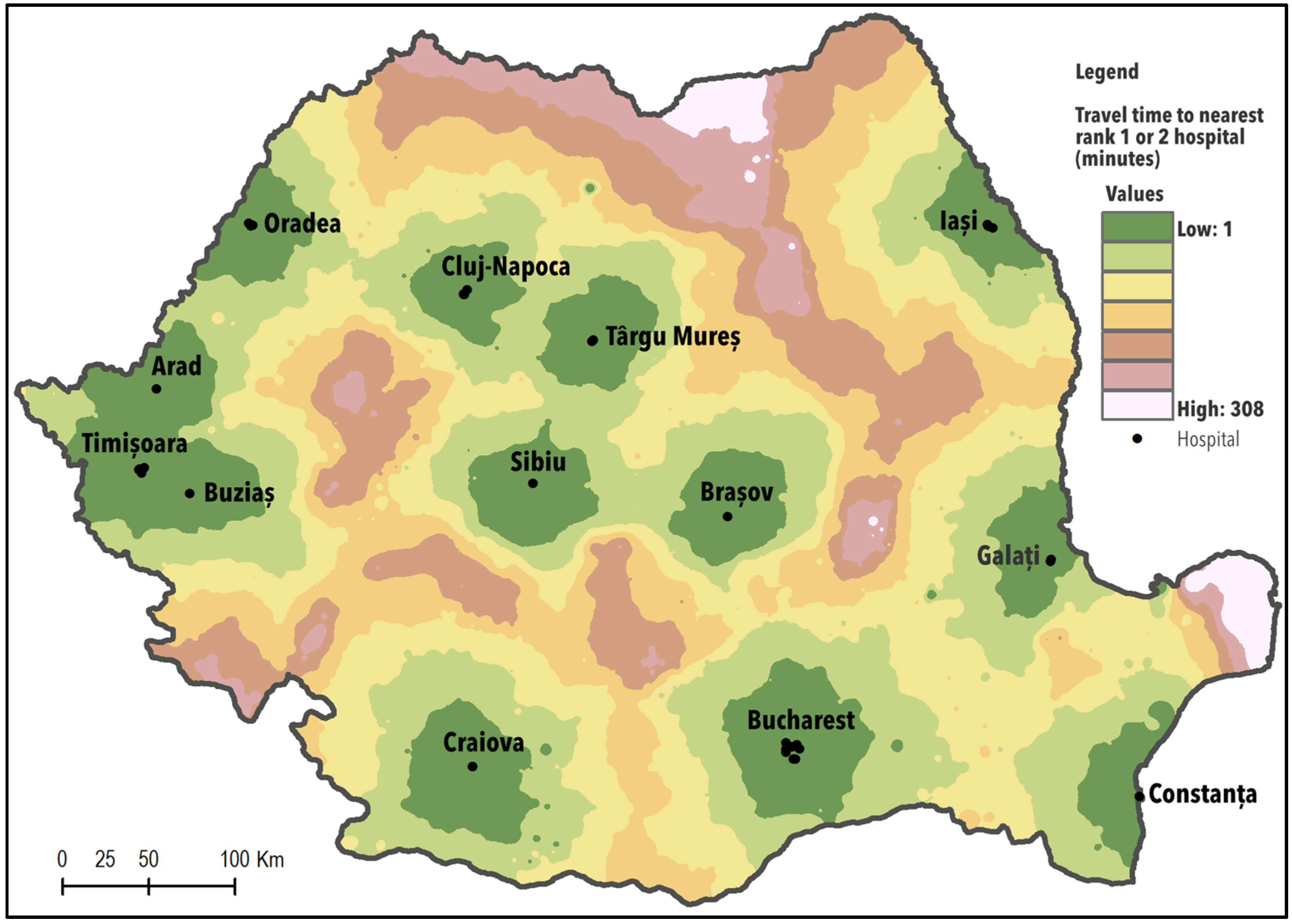
3.2.2. Potential Geographical access of the Population to Hospitals with a High Competency Level
3.2.3. Index of Spatial Accessibility
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Derose, K.P.; Gresenz, C.R.; Ringel, J.S. Understanding disparities in health care access and reducing them through a focus on public health. Health Aff. 2011, 10, 1844–1851. [Google Scholar] [CrossRef]
- World Health Organization. Draft Thirteenth General Programme of Work 2019–2023. Available online: http://apps.who.int/gb/ebwha/pdf_files/WHA71/A71_4-en.pdf?ua=1 (accessed on 19 May 2020).
- World Health Organization. Health 2020: A European Policy Framework and Strategy for the 21st Century. Available online: https://www.euro.who.int/en/publications/abstracts/health-2020.-a-european-policy-framework-and-strategy-for-the-21st-century-2013 (accessed on 15 May 2020).
- Institute of Medicine-Committee on Monitoring Access to Personal Health Care Services. Access to Health Care in America; Millman, M., Ed.; National Academies Press: Washington, DC, USA, 1993. [Google Scholar] [CrossRef]
- Andersen, R.M.; McCutcheon, A.; Aday, L.A.; Chiu, G.Y.; Bell, R. Exploring dimensions of access to medical care. Health Serv. Res. 1983, 18, 49–74. [Google Scholar] [PubMed]
- Martin, D.; Williams, H.C.W.L. Market area analysis and accessibility to primary health care centers. Environ. Plan. A 1992, 24, 1009–1019. [Google Scholar] [CrossRef]
- Levesque, J.F.; Harris, M.F.; Russell, G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int. J. Equity Health 2013, 12, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haggerty, J.L.; Levesque, J.F. Validation of a new measure of availability and accommodation of health care that is valid for rural and urban contexts. Health Expect. Int. J. Public Particip. Health Care Health Policy 2016, 20, 321–334. [Google Scholar] [CrossRef] [Green Version]
- Penchansky, R.; Thomas, J.W. The concept of access: Definition and relationships to consumer satisfaction. Med. Care 1981, 19, 127–140. [Google Scholar] [CrossRef]
- Arcury, T.A.; Gesler, W.M.; Preisser, J.S.; Sherman, J.; Spencer, J.; Perin, J. The Effects of Geography and Spatial Behavior on Health Care Utilisation among the Residents of a Rural Region. Health Serv. Res. 2005, 40, 135–156. [Google Scholar] [CrossRef] [Green Version]
- Henry, K.; Mcdonald, K. Geographic access to Health Services. In Geographic Health Data: Fundamental Techniques for Analysis; Boscoe, F.P., Ed.; CABI: Wallingford, UK, 2013; pp. 142–164. [Google Scholar]
- Guagliardo, M.F. Spatial Accessibility of Primary Care: Concepts, Methods and Challenges. Int. J. Health Geogr. 2004, 3, 3. [Google Scholar] [CrossRef] [Green Version]
- McLafferty, S.L. GIS and Health Care. Annu. Rev. Public Health 2003, 24, 25–42. [Google Scholar] [CrossRef]
- Gulliford, M.; Figueroa, J.; Morgan, M.; Hughes, D.; Gibson, B.; Beech, R.; Hudson, M. What does ‘access to health care’ mean? J. Health Serv. Res. Policy 2002, 7, 186–188. [Google Scholar] [CrossRef]
- Lovett, A.; Haynes, R.; Sünnenberg, G.; Gale, S. Car travel time and accessibility by bus to general practitioner services: A study using patient registers and GIS. Soc. Sci. Med. 2002, 55, 97–111. [Google Scholar] [CrossRef]
- Gulliford, M.; Morgan, M.; Hughes, D.; Beech, R.; Figeroa-Munoz, J.; Gibson, B.; Hudson, M.; Arumugam, C.; Connell, P.; Mohiddin, A.; et al. Access to Health Care. Report of a Scoping Exercise for the National Co-ordinating Centre for NHS Service Delivery and Organisation R & D (NCCSDO). 2011. Available online: http://www.netscc.ac.uk/netscc/hsdr/files/project/SDO_ES_08-1009-005_V01.pdf (accessed on 9 May 2020).
- Weisgrau, S. Issues in rural health: Access, hospitals, and reform. Health Care Financ. Rev. 1995, 17, 1–14. [Google Scholar]
- Zamfir, D.; Dumitrache, L.; Stoica, I.V.; Vârdol, D. Spatial inequalities in health care provision in Romania: Milestones for territorial sustainable development. Carpathian J. Earth Environ. Sci. 2015, 10, 177–188. [Google Scholar]
- Damian, N.; Mocanu, I.; Mitrică, B. Education and health care provision in the Romanian Danube Valley: Territorial disparities. Area 2019, 51, 360–370. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Assuring the Health of the Public in the 21st Century. The Health Care Delivery System. In The Future of the Public’s Health in the 21st Century; National Academies Press: Washington, DC, USA, 2002. [Google Scholar]
- Wang, J.; Dua, F.; Huang, J.; Liu, Y. Access to hospitals: Potential vs. observed. Cities 2020, 100. [Google Scholar] [CrossRef]
- Cheng, L.; Yang, M.; De Vos, J.; Witlox, F. Examining geographical accessibility to multi-tier hospital care services for the elderly: A focus on spatial equity. J. Transp. Health 2020, 19. [Google Scholar] [CrossRef]
- Parmelee, D.; Henderson, G.; Cohen, M. Medicine under socialism. Some observations on Yugoslavia and China. Soc. Sci. Med. 1982, 16, 1389–1396. [Google Scholar] [CrossRef] [PubMed]
- McKee, M.; Healy, J. Hospitals in a Changing Europe. European Observatory on Health Care Systems Series. 2002. Available online: https://www.euro.who.int/data/assets/pdf_file/0004/98401/E74486.pdf (accessed on 4 February 2020).
- Vlădescu, C.; Scântee, S.G.; Olsavszky, V.; Hernaández-Quevedo, C.; Sagan, A. Romania: Health system review. Health Syst. Transit. 2016, 18, 1–170. [Google Scholar] [PubMed]
- OECD/European Observatory on Health Systems and Policies. Romania: Country Health Profile 2019, State of Health in the EU; OECD Publishing: Paris, France; European Observatory on Health Systems and Policies: Brussels, Belgium, 2019. [Google Scholar]
- Dumitrache, L. Défis, incohérences et échecs de la réforme sanitaire en Roumanie. In Migration en Blanc. Medecins D’est en Ouest; Krasteva, A., Vasilcu, D., Eds.; Edition L’Harmattan, Collection Global et Local: Paris, France, 2014; pp. 21–40. [Google Scholar]
- National Institute of Statistics. Tempo Online Statistics. 2018. Available online: http://statistici.insse.ro:8077/tempo-online/#/pages/tables/insse-table (accessed on 13 April 2020).
- Healy, J.; McKee, M. Hospitals in transition in central and eastern Europe and central Asia. Eur. Obs. Health Care Syst. 2001, 7, 1–90. [Google Scholar]
- Joseph, A.E.; Bantock, P.R. Measuring potential physical accessibility to general practitioners in rural areas: A method and case study. Soc. Sci. Med. 1982, 16, 85–90. [Google Scholar] [CrossRef]
- Rosenberg, M.W. Accessibility to health care: A North American perspective. Prog. Hum. Geogr. 1983, 7, 78–87. [Google Scholar] [CrossRef]
- Higgs, G. A literature review of the use of GIS based measures of access to health care services. Health Serv. Outcomes Resour. Methodol. 2004, 5, 119–139. [Google Scholar] [CrossRef]
- Ray, N.; Ebner, S. AccessMod 3.0: Computing geographic coverage and accessibility to health care services using anisotropic movement of patients. Int. J. Health Geogr. 2008, 7, 63. [Google Scholar] [CrossRef] [PubMed]
- Peters, D.H.; Garg, A.; Bloom, G.; Walker, D.G.; Brieger, W.R.; Rahman, M.H. Poverty and Access to Health Care in Developing Countries. Ann. N. Y. Acad. Sci. 2008, 1136, 161–171. [Google Scholar] [CrossRef]
- Cromley, E.K.; McLafferty, S.L. Analyzing Access to Health Services. In GIS and Public Health; Guildord Press: New York, NY, USA, 2002; pp. 232–258. [Google Scholar]
- Morrill, R.L.; Schultz, R. The transportation problem and patient travel to physicians and hospitals. Ann. Reg. Sci. 1971, 5, 11–24. [Google Scholar] [CrossRef]
- Newhouse, J.P. Geographic Access to Physician Services. Annu. Rev. Public Health 1990, 11, 207–230. [Google Scholar] [CrossRef]
- Rosenthal, M.; Zaslavsky, A.; Newhouse, J. The geographic distribution of physicians revisited. Health Serv. Res. 2005, 40, 1931–1952. [Google Scholar] [CrossRef] [Green Version]
- Goodman, D.C.; Fisher, E.; Stukel, T.A.; Chang, C. The distance to community medicare and the likehood of hospitalization: Is closer always better? Am. J. Public Health 1997, 87, 1144–1150. [Google Scholar]
- Haynes, R.; Jones, A.; Sauerzapf, V.; Zhao, H. Validation of travel times to hospital estimates by GIS. Int. J. Health Geogr. 2006, 5, 40. [Google Scholar] [CrossRef] [Green Version]
- Fone, D.; Christie, S.; Lester, N. Comparison of perceived and modelled geographical access to accident and emergency departments: A cross-sectional analysis from the Caerphilly Health and Social Needs Study. Int. J. Health Geogr. 2006, 5, 16. [Google Scholar] [CrossRef] [Green Version]
- Luo, W.; Wang, F.H. Measures of spatial accessibility to health care in GIS environment: Synthesis and a case study in Chicago region. Environ. Plan. B Plan. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef] [Green Version]
- Roovali, L.; Kiivet, R.L. Geographical variations in hospital use in Estonia. Health Place 2006, 12, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Delamater, P.L.; Messina, J.P.; Shortridge, A.M.; Crady, S.C. Measuring geographic access to health care: Raster and network-based methods. Int. J. Health Geogr. 2012, 11, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, F.H.; Luo, W. Assessing spatial and non-spatial factors for health care access: Towards an integrated approach to defining health professional shortage areas. Health Place 2005, 11, 131–146. [Google Scholar] [CrossRef] [PubMed]
- Burkey, M. Decomposing geographic accessibility into component parts: Methods and an application to hospitals. Ann. Reg. Sci. 2012, 48, 783–800. [Google Scholar] [CrossRef]
- Apparicio, P.; Abdelmajid, M.; Riva, M.; Sheamur, R. Comparing alternative approaches to measuring the geographical accessibility of urban health services: Distance types and aggregation-error issues. Int. J. Health Geogr. 2008, 7, 7. [Google Scholar] [CrossRef] [Green Version]
- Dewulf, B.; Neutens, T.; De Weert, Y.; Van de Weghe, N. Accessibility to primary health care in Belgium: An evaluation of policies awarding financial assistance in shortage area. BMC Fam. Pract. 2013, 14, 122. [Google Scholar] [CrossRef] [Green Version]
- Kalogiru, S.; Foley, R. Health, place and Hanly: Modelling accessibility to hospitals in Ireland. Ir. Geogr. 2010, 39, 52–68. [Google Scholar] [CrossRef] [Green Version]
- Wang, F.H. Measurement, optimization, and impact of health care accessibility: A methodological review. Ann. Assoc. Am. Geogr. 2012, 102, 1104–1112. [Google Scholar] [CrossRef] [Green Version]
- Xia, N.; Cheng, L.; Chen, S.; Wei, X.; Zong, W.; Li, M. Accessibility based on Gravity-Radiation model and Google Maps API: A case study in Australia. J. Transp. Geogr. 2018, 72, 178–190. [Google Scholar] [CrossRef]
- Wang, F.; Xu, Y. Estimating OD travel time matrix by Google Maps API: Implementation, advantages, and implications. Geogr. Inf. Sci. 2011, 17, 199–209. [Google Scholar]
- Merciu, C.; Stoian, D.; Merciu, G.; Saghin, I. Using GIS for calculating the accessibility to hospitals in the city of Bucharest and its metropolitan area (Romania). Geogr. Pannonica 2013, 17, 106–113. [Google Scholar] [CrossRef]
- Ciutan, M.; Sasu, C. Aspecte ale furnizării serviciilor medicale, în mediul rural, din punct de vedere al accesibilității geografice. Manag. Health 2008, 12, 26–33. [Google Scholar] [CrossRef]
- Eva, M.; Iațu, C. Modelling spatial accessibility to medical care. Case study of the North-Eastern Region of Romania. Hum. Geogr. J. Stud. Res. Hum. Geogr. 2015, 9, 151–164. [Google Scholar]
- World Bank. Romania Regional Hospital Analysis Study. Regional Referral Networks in Romania. 2018. Available online: https://documents.worldbank.org/en/publication/documents-reports/documentdetail/798931530245678590/romania-regional-hospital-analysis-study-regional-referral-networks (accessed on 20 March 2020).
- Barbieri, S.; Jorm, L. Travel times to hospitals in Australia. Sci. Data 2019, 6, 248. [Google Scholar] [CrossRef] [PubMed]
- Nelson, A.; Weiss, D.J.; van Etten, J.; Cattaneo, A.; McMenomy, T.S.; Koo, J. A suite of global accessibility indicators. Sci. Data 2019, 6, 266. [Google Scholar] [CrossRef] [Green Version]
- Weiss, D.J.; Nelson, A.; Vargas-Ruiz, C.A.; Gligorić, K.; Bavadekar, S.; Gabrilovich, E.; Bertozzi-Villa, A.; Rozier, J.; Gibson, H.S.; Shekel, T.; et al. Global maps of travel time to health care facilities. Nat. Med. 2020. [Google Scholar] [CrossRef]
- Thiessen, A.H. Precipitation averages for large areas. Mon. Weather Rev. 1911, 39, 1082–1084. [Google Scholar] [CrossRef]
- Jin, C.; Cheng, J.; Lu, Y.; Huang, Z.; Cao, F. Spatial inequity in access to health care facilities at a county level in a developing country: A case study of Deqing County, Zhejiang. China Int. J. Equity Health 2015, 14, 67. [Google Scholar] [CrossRef] [Green Version]
- Brabyn, L.; Skelly, C. Modeling Population Access to New Zealand Public Hospitals. Int. J. Health Geogr. 2002, 1, 3. [Google Scholar] [CrossRef] [Green Version]
- Kobayashi, S.; Fujouka, T.; Tanaka, Y.; Inoue, M.; Niho, Y.; Miyoshi, A. A geographical information system using Google Map API for guidance to referral hospital. J. Med. Syst. 2010, 34, 1157–1160. [Google Scholar] [CrossRef]
- Google Maps. Guides for Directions API. 2018. Available online: https://developers.google.com/maps/documentation/directions/ (accessed on 3 September 2020).
- Kelly, C.; Hulme, C.; Farragher, T.; Clarke, G. Are differences in travel time or distance to health care for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open 2016, 6, 30–59. [Google Scholar] [CrossRef] [PubMed]
- Monitorul Oficial al României no. 490 and 652/2015. Law 95/2006 on Health Care Reform (Republished); Monitorul Oficial Publishing House: Bucharest, Romania, 2015. [Google Scholar]
- Monitorul Oficial al României no.274/2011. Ministry of Health Order no.323/2011; Monitorul Oficial Publishing House: Bucharest, Romania, 2011. [Google Scholar]
- Eurostat, Health Care Staff: Physicians by Medical Specialty. Available online: http://appsso.eurostat.ec.europa.eu/nui/submitViewTableAction.do (accessed on 24 February 2020).
- Dumitrache, L.; Nae, M.; Dumbrăveanu, D.; Simion, G.; Suditu, B. Contrasting Clustering in Health Care Provision in Romania: Spatial and Aspatial Limitations. Procedia Environ. Sci. 2016, 32, 290–299. [Google Scholar] [CrossRef] [Green Version]
- World Bank. Romania-Functional Review: Health Sector; World Bank: Washington, DC, USA, 2011; Available online: https://openknowledge.worldbank.org/handle/10986/12290 (accessed on 10 May 2020).
- Ciutan, M.; Scîntee, S.G.; Dosius, M.; Mototolea, C.; Vlădescu, C. Geographical Distribution of Avoidable Hospital Conditions in Romania. Procedia Environ. Sci. 2016, 32, 318–326. [Google Scholar] [CrossRef] [Green Version]
- McPherson, K. International differences in medical care practices. Health Care Financ. Rev. 1989, 1989, 9–20. [Google Scholar]
- Diagnostic Related Groups (DRG). Available online: http://www.drg.ro/index (accessed on 5 November 2019).
- European Commission. European Core Health Indicators. Available online: https://ec.europa.eu/health/indicators (accessed on 3 December 2019).
- Monitorul Oficial al României, no 337/2020. Ministry of Health Order No 355/2020 on National Bed Plan for the Period 2020–2022; Monitorul Oficial Publishing House: Bucharest, Romania, 2020. [Google Scholar]
- Alper, E.; O’Malley, T.A.; Greenwald, J. Hospital Discharge and Readmission. 2020. Available online: https://www.uptodate.com/contents/hospital-discharge-and-readmission/contributors (accessed on 21 January 2020).
- Kuo, Y.F.; Goodwin, J.S. Association of hospitalist care with medical utilization after discharge: Evidence of cost shift from a cohort study. Ann. Intern. Med. 2011, 155, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Garg, N.; Husk, G.; Nguyen, T.; Onyile, A.; Echezona, S.; Kuperman, G.; Shapiro, J.S. Hospital closure and insights into patient dispersion: The closure of Saint Vincent’s Catholic Medical Center in New York City. Appl. Clin. Inform. 2015, 6, 185–199. [Google Scholar] [CrossRef] [Green Version]
- Preda, M.; Mareci, A.; Tudoricu, A.; Taloș, A.M.; Bogan, E.; Lequeux-Dincă, A.I.; Vijulie, I. Defining the Concept of Family through the Lens of Fertile-Aged Women in Bucharest, Romania—Between Traditionalism and Inclusion. Sustainability 2020, 12, 2691. [Google Scholar] [CrossRef] [Green Version]
- European Union. Statistics on Income and Living Conditions. 2018. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php/EU_statistics_on_income_and_living_conditions_EU-SILC)_methodology (accessed on 24 February 2020).
- Cheng, G.; Zeng, X.; Duan, L.; Lu, X.; Sun, H.; Jiang, T.; Li, Y. Spatial difference analysis for accessibility to high level hospitals based on travel time in Shenzhen, China. Habitat Int. 2016, 53, 485–494. [Google Scholar] [CrossRef] [Green Version]
- Gibson, R.; Lazenby, H.; Levit, K.R.; Waldo, D.R. Health Care Financing Review; U.S. Government Printing Office: Washington, DC, USA, 1984.
- Monitorul Oficial. Partea I, No 988/2016, Order No. 1376/2016; Monitorul Oficial Publishing House: Bucharest, Romania, 2016. [Google Scholar]



| Medical Personnel | Total | Urban Areas | Rural Areas | Romania Average Inhabitants/Medical Personnel | EU Average Inhabitants/ Medical Personnel |
|---|---|---|---|---|---|
| Doctors | 60,585 | 54,870 | 5715 | 322.4 | 262.4 |
| out of which: GPs | 12,027 | 7584 | 4443 | 1623.9 | 1088.0 |
| Dentists | 16,457 | 14,425 | 2032 | 1186.8 | 343.2 |
| Pharmacists | 17,611 | 14,199 | 3412 | 1109.0 | 1115.2 |
| Nurses | 145,317 | 129,424 | 15,893 | 134.4 | 135.6 |
| All Hospital Categories | Rank I and II Hospitals | |||
|---|---|---|---|---|
| Population | % Total Population | Population | % Total Population | |
| Less than 30 min | 17,538,668 | 82.7 | 6,183,014 | 29.2 |
| 30–90 min | 3,611,485 | 17.0 | 7,738,097 | 36.5 |
| 90–120 min | 42,265 | 0.2 | 3,742,540 | 17.7 |
| Over 120 min | 3,528,767 | 16.6 | ||
| No roads access | 10,728 | 0.1 | 10,728 | 0.1 |
| ISA Values | Accessibility Level | Population (Millions) | % |
|---|---|---|---|
| Less than 0.06 | Very low | 3,940,118 | 18.6 |
| 0.06–0.08 | Low | 2,884,692.0 | 13.6 |
| 0.08–0.11 | Medium | 4,444,386 | 21.0 |
| 0.11–0.15 | Relatively high | 3,136,227 | 14.8 |
| 0.15–0.89 | High | 6,797,723 | 32.1 |
| Total population | 21,203,146 | 100.0 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dumitrache, L.; Nae, M.; Simion, G.; Taloș, A.-M. Modelling Potential Geographical Access of the Population to Public Hospitals and Quality Health Care in Romania. Int. J. Environ. Res. Public Health 2020, 17, 8487. https://doi.org/10.3390/ijerph17228487
Dumitrache L, Nae M, Simion G, Taloș A-M. Modelling Potential Geographical Access of the Population to Public Hospitals and Quality Health Care in Romania. International Journal of Environmental Research and Public Health. 2020; 17(22):8487. https://doi.org/10.3390/ijerph17228487
Chicago/Turabian StyleDumitrache, Liliana, Mariana Nae, Gabriel Simion, and Ana-Maria Taloș. 2020. "Modelling Potential Geographical Access of the Population to Public Hospitals and Quality Health Care in Romania" International Journal of Environmental Research and Public Health 17, no. 22: 8487. https://doi.org/10.3390/ijerph17228487
APA StyleDumitrache, L., Nae, M., Simion, G., & Taloș, A.-M. (2020). Modelling Potential Geographical Access of the Population to Public Hospitals and Quality Health Care in Romania. International Journal of Environmental Research and Public Health, 17(22), 8487. https://doi.org/10.3390/ijerph17228487








