Associations between Intensity, Frequency, Duration, and Volume of Physical Activity and the Risk of Stroke in Middle- and Older-Aged Chinese People: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Stroke Measurements
2.3. Assessment of PA
2.4. Assessment of Covariables
2.5. Data Analysis
3. Results
3.1. Characteristics of the Participants
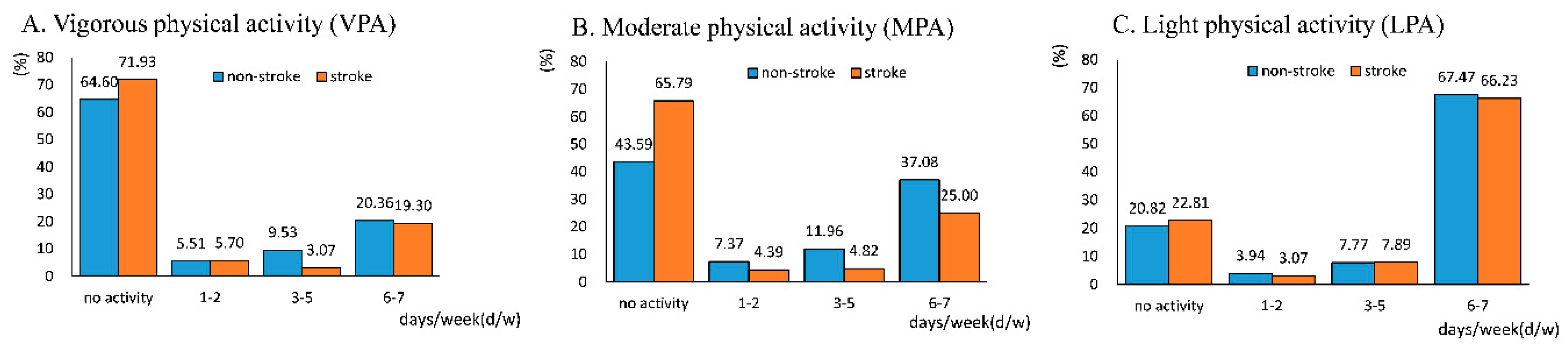
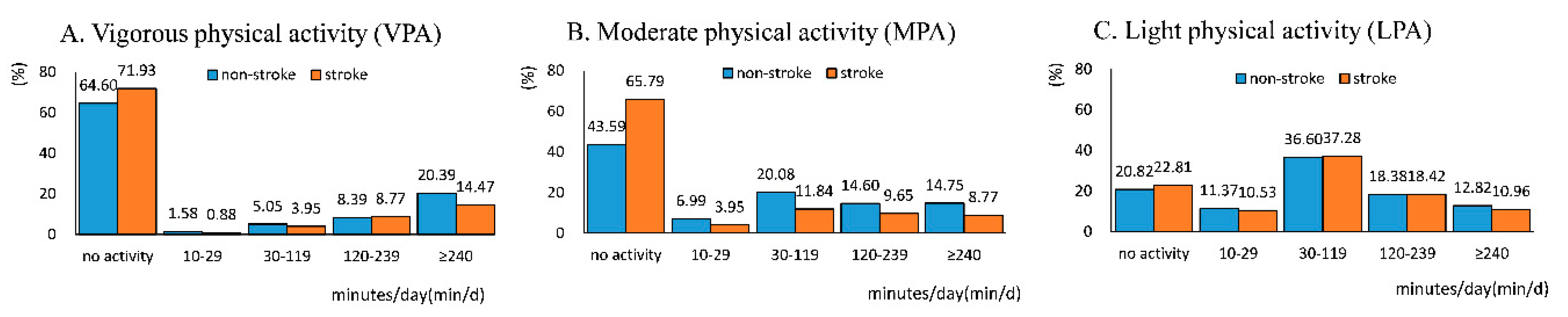
3.2. Frequency of PA and the Risk of Stroke
3.3. Duration of PA and the Risk of Stroke
3.4. Volume of PA and the Risk of Stroke
3.5. Sensitivity Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Variables | Model 4 (n = 5748) | ||
|---|---|---|---|
| OR | 95% CI | ||
| Frequency | |||
| VPA | |||
| No activity | 1.00 | ||
| 1–2 d/w | 1.30 | 0.65 | 2.63 |
| 3–5 d/w | 0.29 * | 0.10 | 0.80 |
| 6–7 d/w | 0.80 | 0.49 | 1.31 |
| MPA | |||
| No activity | 1.00 | ||
| 1–2 d/w | 0.35 * | 0.15 | 0.82 |
| 3–5 d/w | 0.26 * | 0.12 | 0.57 |
| 6–7 d/w | 0.43 * | 0.27 | 0.66 |
| LPA | |||
| No activity | 1.00 | ||
| 1–2 d/w | 0.92 | 0.33 | 2.55 |
| 3–5 d/w | 1.00 | 0.52 | 1.92 |
| 6–7 d/w | 0.94 | 0.59 | 1.49 |
| Duration | |||
| VPA | |||
| No activity | 1.00 | ||
| 10–29 min/d | 0.88 | 0.21 | 3.81 |
| 30–119 min/d | 0.57 | 0.20 | 1.57 |
| 120–239 min/d | 1.03 | 0.54 | 1.94 |
| ≥240 min/d | 0.66 | 0.39 | 1.11 |
| MPA | |||
| No activity | 1.00 | ||
| 10–29 min/d | 0.41 * | 0.19 | 0.88 |
| 30–119 min/d | 0.31 * | 0.17 | 0.55 |
| 120–239 min/d | 0.42 * | 0.23 | 0.76 |
| ≥240 min/d | 0.47 * | 0.26 | 0.85 |
| LPA | |||
| No activity | 1.00 | ||
| 10–29 min/d | 0.78 | 0.42 | 1.44 |
| 30–119 min/d | 1.07 | 0.63 | 1.80 |
| 120–239 min/d | 0.87 | 0.49 | 1.54 |
| ≥240 min/d | 0.78 | 0.41 | 1.48 |
| Volume | |||
| VPA | |||
| No activity | 1.00 | ||
| 10–74 min/w | 2.00 | 0.45 | 8.87 |
| 75–299 min/w | 0.57 | 0.15 | 2.26 |
| ≥300 min/w | 0.74 | 0.47 | 1.18 |
| MPA | |||
| No activity | 1.00 | ||
| 10–149 min/w | 0.38 * | 0.18 | 0.80 |
| 150–299 min/w | 0.20 * | 0.05 | 0.88 |
| ≥300 min/w | 0.40 * | 0.26 | 0.62 |
| LPA | |||
| No activity | 1.00 | ||
| 10–149 min/w | 0.78 | 0.42 | 1.43 |
| 150–299 min/w | 0.74 | 0.20 | 2.79 |
| ≥300 min/w | 0.98 | 0.62 | 1.55 |
| Variables | Model 1 (n = 6250) | E-value | |||
|---|---|---|---|---|---|
| OR | 95% CI | Point | CI | ||
| Frequency | |||||
| VPA | |||||
| No activity | 1.00 | ||||
| 1–2 d/w | 0.92 | 0.46 | 1.81 | - | - |
| 3–5 d/w | 0.32 * | 0.14 | 0.75 | 5.70 | 2.00 |
| 6–7 d/w | 0.74 | 0.49 | 1.11 | - | - |
| MPA | |||||
| No activity | 1.00 | ||||
| 1–2 d/w | 0.35 * | 0.18 | 0.72 | 5.16 | 2.12 |
| 3–5 d/w | 0.23 * | 0.12 | 0.46 | 8.16 | 3.77 |
| 6–7 d/w | 0.40 * | 0.27 | 0.58 | 4.44 | 2.84 |
| LPA | |||||
| No activity | 1.00 | ||||
| 1–2 d/w | 0.74 | 0.29 | 1.90 | - | - |
| 3–5 d/w | 0.89 | 0.49 | 1.60 | - | - |
| 6–7 d/w | 0.92 | 0.61 | 1.39 | - | - |
| Duration | |||||
| VPA | |||||
| No activity | 1.00 | ||||
| 10–29 min/d | 0.60 | 0.14 | 2.55 | - | - |
| 30–119 min/d | 0.60 | 0.26 | 1.37 | - | - |
| 120–239 min/d | 0.82 | 0.46 | 1.45 | - | - |
| ≥240 min/d | 0.60 * | 0.38 | 0.94 | 2.72 | 1.32 |
| MPA | |||||
| No activity | 1.00 | ||||
| 10–29 min/d | 0.31 * | 0.14 | 0.65 | 5.91 | 2.45 |
| 30–119 min/d | 0.32 * | 0.20 | 0.53 | 5.70 | 3.18 |
| 120–239 min/d | 0.40 * | 0.24 | 0.67 | 4.44 | 2.35 |
| ≥240 min/d | 0.40 * | 0.23 | 0.68 | 4.44 | 2.30 |
| LPA | |||||
| No activity | 1.00 | ||||
| 10–29 min/d | 0.68 | 0.39 | 1.20 | - | - |
| 30–119 min/d | 1.05 | 0.66 | 1.66 | - | - |
| 120–239 min/d | 0.84 | 0.51 | 1.39 | - | - |
| ≥240 min/d | 0.75 | 0.43 | 1.32 | - | - |
| Volume | |||||
| VPA | |||||
| No activity | 1.00 | ||||
| 10–74 min/w | 1.30 | 0.30 | 5.58 | - | - |
| 75–299 min/w | 0.40 | 0.10 | 1.56 | - | - |
| ≥300 min/w | 0.68 * | 0.46 | 0.99 | 2.30 | 1.11 |
| MPA | |||||
| No activity | 1.00 | ||||
| 10–149 min/w | 0.34 * | 0.18 | 0.66 | 5.33 | 2.40 |
| 150–299 min/w | 0.16 * | 0.04 | 0.69 | 11.98 | 2.26 |
| ≥300 min/w | 0.38 * | 0.26 | 0.55 | 4.70 | 3.04 |
| LPA | |||||
| No activity | 1.00 | ||||
| 10–149 min/w | 0.70 | 0.41 | 1.21 | - | - |
| 150–299 min/w | 0.54 | 0.15 | 1.99 | - | - |
| ≥300 min/w | 0.97 | 0.64 | 1.45 | - | - |
References
- Naghavi, M.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Adetokunboh, O.; Afshin, A.; Agrawal, A.; et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1151–1210. [Google Scholar] [CrossRef]
- Avan, A.; Digaleh, H.; Di Napoli, M.; Stranges, S.; Behrouz, R.; Shojaeianbabaei, G.; Amiri, A.; Tabrizi, R.; Mokhber, N.; Spence, J.D.; et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: An ecological analysis from the Global Burden of Disease Study 2017. BMC Med. 2019, 17, 191. [Google Scholar] [CrossRef]
- Global Burden of Disease Stroke Expert Group. Global, Regional, and Country-Specific Lifetime Risks of Stroke, 1990 and 2016. N. Engl. J. Med. 2018, 379, 2429–2437. [Google Scholar] [CrossRef]
- Wang, Y.J.; Li, Z.X.; Gu, H.Q.; Zhai, Y.; Jiang, Y.; Zhao, X.Q.; Wang, Y.L.; Yang, X.; Wang, C.J.; Meng, X.; et al. China Stroke Statistics 2019: A Report From the National Center for Healthcare Quality Management in Neurological Diseases, China National Clinical Research Center for Neurological Diseases, the Chinese Stroke Association, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention and Institute for Global Neuroscience and Stroke Collaborations. Stroke Vasc. Neurol. 2020, 5, 211–239. [Google Scholar] [CrossRef]
- Wang, W.; Jiang, B.; Sun, H.; Ru, X.; Sun, D.; Wang, L.; Wang, L.; Jiang, Y.; Li, Y.; Wang, Y.; et al. Prevalence, Incidence, and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480 687 Adults. Circulation 2017, 135, 759–771. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.J.; Chin, S.L.; Rangarajan, S.; Xavier, D.; Liu, L.; Zhang, H.; Rao-Melacini, P.; Zhang, X.; Pais, P.; Agapay, S.; et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): A case-control study. Lancet 2016, 388, 761–775. [Google Scholar] [CrossRef]
- WHO Guidelines Approved by the Guidelines Review Committee. In Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010.
- Mora, S.; Cook, N.; Buring, J.E.; Ridker, P.M.; Lee, I.M. Physical activity and reduced risk of cardiovascular events: Potential mediating mechanisms. Circulation 2007, 116, 2110–2118. [Google Scholar] [CrossRef] [PubMed]
- Fiuza-Luces, C.; Santos-Lozano, A.; Joyner, M.; Carrera-Bastos, P.; Picazo, O.; Zugaza, J.L.; Izquierdo, M.; Ruilope, L.M.; Lucia, A. Exercise benefits in cardiovascular disease: Beyond attenuation of traditional risk factors. Nat. Rev. Cardiol. 2018, 15, 731–743. [Google Scholar] [CrossRef]
- Lear, S.A.; Hu, W.; Rangarajan, S.; Gasevic, D.; Leong, D.; Iqbal, R.; Casanova, A.; Swaminathan, S.; Anjana, R.M.; Kumar, R.; et al. The effect of physical activity on mortality and cardiovascular disease in 130,000 people from 17 high-income, middle-income, and low-income countries: The PURE study. Lancet 2017, 390, 2643–2654. [Google Scholar] [CrossRef]
- Kyu, H.H.; Bachman, V.F.; Alexander, L.T.; Mumford, J.E.; Afshin, A.; Estep, K.; Veerman, J.L.; Delwiche, K.; Iannarone, M.L.; Moyer, M.L.; et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: Systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ 2016, 354, i3857. [Google Scholar] [CrossRef]
- Soares-Miranda, L.; Siscovick, D.S.; Psaty, B.M.; Longstreth, W.T., Jr.; Mozaffarian, D. Physical Activity and Risk of Coronary Heart Disease and Stroke in Older Adults: The Cardiovascular Health Study. Circulation 2016, 133, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Kiely, D.K.; Wolf, P.A.; Cupples, L.A.; Beiser, A.S.; Kannel, W.B. Physical activity and stroke risk: The Framingham Study. Am. J. Epidemiol. 1994, 140, 608–620. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Liang, Q.; Zhou, W.; Huang, X.; Hu, L.; You, C.; Li, J.; Wu, Y.; Li, P.; Wu, Q.; et al. Association between physical activity and stroke in a middle-aged and elderly Chinese population. Medicine (Baltimore) 2018, 97, e13568. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, Z.; Gao, M.; Yang, R.; Li, N.; Liu, Z.; Cao, W.; Huang, T. Association of physical activity, sedentary behaviours and sleep duration with cardiovascular diseases and lipid profiles: A Mendelian randomization analysis. Lipids Health Dis. 2020, 19, 86. [Google Scholar] [CrossRef]
- Chomistek, A.K.; Henschel, B.; Eliassen, A.H.; Mukamal, K.J.; Rimm, E.B. Frequency, Type, and Volume of Leisure-Time Physical Activity and Risk of Coronary Heart Disease in Young Women. Circulation 2016, 134, 290–299. [Google Scholar] [CrossRef]
- Jeong, H.G.; Kim, D.Y.; Kang, D.W.; Kim, B.J.; Kim, C.K.; Kim, Y.; Yang, W.; Park, E.S.; Lee, S.H. Physical Activity Frequency and the Risk of Stroke: A Nationwide Cohort Study in Korea. J. Am. Heart Assoc. 2017, 6, e005671. [Google Scholar] [CrossRef]
- Zhao, Y.; Hu, Y.; Smith, J.P.; Strauss, J.; Yang, G. Cohort profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 2014, 43, 61–68. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Ding, P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann. Intern. Med. 2017, 167, 268–274. [Google Scholar] [CrossRef]
- Shepherd, A.I.; Pulsford, R.; Poltawski, L.; Forster, A.; Taylor, R.S.; Spencer, A.; Hollands, L.; James, M.; Allison, R.; Norris, M.; et al. Physical activity, sleep, and fatigue in community dwelling Stroke Survivors. Sci. Rep. 2018, 8, 7900. [Google Scholar] [CrossRef]
- Bernhardt, J.; Dewey, H.; Thrift, A.; Donnan, G. Inactive and alone: Physical activity within the first 14 days of acute stroke unit care. Stroke 2004, 35, 1005–1009. [Google Scholar] [CrossRef]
- Gao, F.; Zhang, L.Q. Altered contractile properties of the gastrocnemius muscle poststroke. J. Appl. Physiol. 2008, 105, 1802–1808. [Google Scholar] [CrossRef] [PubMed]
- Lieber, R.L.; Ward, S.R. Cellular mechanisms of tissue fibrosis. 4. Structural and functional consequences of skeletal muscle fibrosis. Am. J. Physiol. Cell Physiol. 2013, 305, C241–C252. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.S.; Spear, S.; Rymer, W.Z. Quantifying changes in material properties of stroke-impaired muscle. Clin. Biomech. (Bristol Avon) 2015, 30, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Willey, J.Z.; Moon, Y.P.; Paik, M.C.; Boden-Albala, B.; Sacco, R.L.; Elkind, M.S. Physical activity and risk of ischemic stroke in the Northern Manhattan Study. Neurology 2009, 73, 1774–1779. [Google Scholar] [CrossRef] [PubMed]
- Sattelmair, J.R.; Kurth, T.; Buring, J.E.; Lee, I.M. Physical activity and risk of stroke in women. Stroke 2010, 41, 1243–1250. [Google Scholar] [CrossRef]
- Shangren, Q.; Zirui, H.; Ye, D. Income-Related Inequalities in Chronic Disease Situation Among the Chinese Population Aged Above 45 Years. Inquiry 2019, 56, 46958019860383. [Google Scholar] [CrossRef]
- Wang, Z.; Chen, Z.; Zhang, L.; Wang, X.; Hao, G.; Zhang, Z.; Shao, L.; Tian, Y.; Dong, Y.; Zheng, C.; et al. Status of Hypertension in China: Results From the China Hypertension Survey, 2012-2015. Circulation 2018, 137, 2344–2356. [Google Scholar] [CrossRef]
- Yang, L.; Shao, J.; Bian, Y.; Wu, H.; Shi, L.; Zeng, L.; Li, W.; Dong, J. Prevalence of type 2 diabetes mellitus among inland residents in China (2000-2014): A meta-analysis. J. Diabetes Investig. 2016, 7, 845–852. [Google Scholar] [CrossRef]
- Borjesson, M.; Onerup, A.; Lundqvist, S.; Dahlof, B. Physical activity and exercise lower blood pressure in individuals with hypertension: Narrative review of 27 RCTs. Br. J. Sports Med. 2016, 50, 356–361. [Google Scholar] [CrossRef]
- Smith, A.D.; Crippa, A.; Woodcock, J.; Brage, S. Physical activity and incident type 2 diabetes mellitus: A systematic review and dose-response meta-analysis of prospective cohort studies. Diabetologia 2016, 59, 2527–2545. [Google Scholar] [CrossRef]
- Zeng, Z.; Bian, Y.; Cui, Y.; Yang, D.; Wang, Y.; Yu, C. Physical Activity Dimensions and Its Association with Risk of Diabetes in Middle and Older Aged Chinese People. Int. J. Environ. Res. Public Health 2020, 17, E7803. [Google Scholar] [CrossRef] [PubMed]
- Aigner, A.; Grittner, U.; Rolfs, A.; Norrving, B.; Siegerink, B.; Busch, M.A. Contribution of Established Stroke Risk Factors to the Burden of Stroke in Young Adults. Stroke 2017, 48, 1744–1751. [Google Scholar] [CrossRef] [PubMed]
- Kubota, Y.; Iso, H.; Yamagishi, K.; Sawada, N.; Tsugane, S.; Group, J.S. Daily Total Physical Activity and Incident Stroke: The Japan Public Health Center-Based Prospective Study. Stroke 2017, 48, 1730–1736. [Google Scholar] [CrossRef] [PubMed]
- Wendel-Vos, G.C.; Schuit, A.J.; Feskens, E.J.; Boshuizen, H.C.; Verschuren, W.M.; Saris, W.H.; Kromhout, D. Physical activity and stroke. A meta-analysis of observational data. Int. J. Epidemiol. 2004, 33, 787–798. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Dai, Y.; Zheng, J.; Xie, Y.; Guo, R.; Guo, X.; Sun, G.; Sun, Z.; Sun, Y.; Zheng, L. Sex difference in the incidence of stroke and its corresponding influence factors: Results from a follow-up 8.4 years of rural China hypertensive prospective cohort study. Lipids Health Dis. 2019, 18, 72. [Google Scholar] [CrossRef]
- Starmer, A.J.; Frintner, M.P.; Matos, K.; Somberg, C.; Freed, G.; Byrne, B.J. Gender Discrepancies Related to Pediatrician Work-Life Balance and Household Responsibilities. Pediatrics 2019, 144, e20182926. [Google Scholar] [CrossRef]
- Adjei, N.K.; Brand, T. Investigating the associations between productive housework activities, sleep hours and self-reported health among elderly men and women in western industrialised countries. BMC Public Health 2018, 18, 110. [Google Scholar] [CrossRef]
- Cao, X.L.; Wang, S.B.; Zhong, B.L.; Zhang, L.; Ungvari, G.S.; Ng, C.H.; Li, L.; Chiu, H.F.; Lok, G.K.; Lu, J.P.; et al. The prevalence of insomnia in the general population in China: A meta-analysis. PLoS ONE 2017, 12, e0170772. [Google Scholar] [CrossRef]
- Wang, Y.; Huang, W.; O’Neil, A.; Lan, Y.; Aune, D.; Wang, W.; Yu, C.; Chen, X. Association between sleep duration and mortality risk among adults with type 2 diabetes: A prospective cohort study. Diabetologia 2020, 63, 2292–2304. [Google Scholar] [CrossRef]
- Dohrn, I.M.; Welmer, A.K.; Hagstromer, M. Accelerometry-assessed physical activity and sedentary time and associations with chronic disease and hospital visits - a prospective cohort study with 15 years follow-up. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 125. [Google Scholar] [CrossRef]
- LaCroix, A.Z.; Bellettiere, J.; Rillamas-Sun, E.; Di, C.; Evenson, K.R.; Lewis, C.E.; Buchner, D.M.; Stefanick, M.L.; Lee, I.M.; Rosenberg, D.E.; et al. Association of Light Physical Activity Measured by Accelerometry and Incidence of Coronary Heart Disease and Cardiovascular Disease in Older Women. JAMA Netw. Open 2019, 2, e190419. [Google Scholar] [CrossRef] [PubMed]
- Hupin, D.; Raffin, J.; Barth, N.; Berger, M.; Garet, M.; Stampone, K.; Celle, S.; Pichot, V.; Bongue, B.; Barthelemy, J.C.; et al. Even a Previous Light-Active Physical Activity at Work Still Reduces Late Myocardial Infarction and Stroke in Retired Adults Aged>65 Years by 32%: The PROOF Cohort Study. Front. Public Health 2019, 7, 51. [Google Scholar] [CrossRef] [PubMed]
- LaMonte, M.J.; Buchner, D.M.; Rillamas-Sun, E.; Di, C.; Evenson, K.R.; Bellettiere, J.; Lewis, C.E.; Lee, I.M.; Tinker, L.F.; Seguin, R.; et al. Accelerometer-Measured Physical Activity and Mortality in Women Aged 63 to 99. J. Am. Geriatr. Soc. 2018, 66, 886–894. [Google Scholar] [CrossRef] [PubMed]

| Variables | Total (n = 6250) | Non-Stroke (n = 6022) | Stroke (n = 228) |
|---|---|---|---|
| Age, year (mean ± SD) | 61.0 ± 9.2 | 60.9 ± 9.2 | 63.9 ± 9.4 |
| BMI, kg/m2 (mean ± SD) | 23.9 ± 3.9 | 23.9 ± 3.9 | 24.1 ± 3.8 |
| Sex (%) | |||
| Male | 47.0 | 46.6 | 57.9 |
| Female | 53.0 | 53.4 | 42.1 |
| Educational status (%) | |||
| Junior high school or below | 88.9 | 88.9 | 91.2 |
| Senior high school or vocational school | 10.6 | 10.7 | 7.9 |
| College or above | 0.5 | 0.5 | 0.9 |
| Marital status (%) | |||
| Married or partnered | 87.5 | 87.7 | 80.7 |
| Separated, divorced, or widowed | 12.1 | 11.8 | 18.4 |
| Never married | 0.5 | 0.4 | 0.9 |
| Drinking (%) | |||
| Never | 54.5 | 54.7 | 50.9 |
| Former | 11.0 | 10.7 | 20.6 |
| Current | 34.5 | 34.7 | 28.5 |
| Smoking (%) | |||
| Never | 56.1 | 56.6 | 45.2 |
| Former | 15.9 | 15.5 | 26.3 |
| Current | 28.0 | 28.0 | 28.5 |
| Variables | Model 1 (n = 6250) | Model 2 (n = 2936) | Model 3 (n = 3314) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||||
| Frequency | |||||||||
| VPA | |||||||||
| No activity | 1.00 | 1.00 | 1.00 | ||||||
| 1–2 d/w | 0.92 | 0.46 | 1.81 | 0.68 | 0.29 | 1.6 | 1.56 | 0.54 | 4.54 |
| 3–5 d/w | 0.32 * | 0.14 | 0.75 | 0.43 | 0.18 | 1.05 | N/A | ||
| 6–7 d/w | 0.74 | 0.49 | 1.11 | 0.61 | 0.36 | 1.02 | 1.06 | 0.59 | 1.90 |
| MPA | |||||||||
| No activity | 1.00 | 1.00 | 1.00 | ||||||
| 1–2 d/w | 0.35 * | 0.18 | 0.72 | 0.26 * | 0.09 | 0.78 | 0.53 | 0.21 | 1.32 |
| 3–5 d/w | 0.23 * | 0.12 | 0.46 | 0.28 * | 0.12 | 0.63 | 0.14 * | 0.04 | 0.46 |
| 6–7 d/w | 0.40 * | 0.27 | 0.58 | 0.34 * | 0.20 | 0.60 | 0.46 * | 0.28 | 0.78 |
| LPA | |||||||||
| No activity | 1.00 | 1.00 | 1.00 | ||||||
| 1–2 d/w | 0.74 | 0.29 | 1.90 | 0.49 | 0.10 | 2.45 | 1.30 | 0.44 | 3.81 |
| 3–5 d/w | 0.89 | 0.49 | 1.60 | 0.89 | 0.43 | 1.84 | 0.76 | 0.27 | 2.18 |
| 6–7 d/w | 0.92 | 0.61 | 1.39 | 0.79 | 0.45 | 1.38 | 1.13 | 0.63 | 2.03 |
| Duration | |||||||||
| VPA | |||||||||
| No activity | 1.00 | 1.00 | 1.00 | ||||||
| 10–29 min/d | 0.60 | 0.14 | 2.55 | 0.82 | 0.18 | 3.64 | N/A | ||
| 30–119 min/d | 0.60 | 0.26 | 1.37 | 0.46 | 0.18 | 1.21 | 1.06 | 0.26 | 4.26 |
| 120–239 min/d | 0.82 | 0.46 | 1.45 | 0.71 | 0.34 | 1.51 | 1.05 | 0.46 | 2.4 |
| ≥240 min/d | 0.60 * | 0.38 | 0.94 | 0.53 * | 0.30 | 0.93 | 0.80 | 0.40 | 1.57 |
| MPA | |||||||||
| No activity | 1.00 | 1.00 | 1.00 | ||||||
| 10–29 min/d | 0.31 * | 0.14 | 0.65 | 0.35 | 0.12 | 1.03 | 0.27 * | 0.10 | 0.75 |
| 30–119 min/d | 0.32 * | 0.20 | 0.53 | 0.27 * | 0.13 | 0.56 | 0.38 * | 0.19 | 0.75 |
| 120–239 min/d | 0.40 * | 0.24 | 0.67 | 0.35 * | 0.17 | 0.72 | 0.49 * | 0.25 | 0.99 |
| ≥240 min/d | 0.40 * | 0.23 | 0.68 | 0.34 * | 0.17 | 0.68 | 0.51 | 0.23 | 1.15 |
| LPA | |||||||||
| No activity | 1.00 | 1.00 | 1.00 | ||||||
| 10–29 min/d | 0.68 | 0.39 | 1.20 | 0.50 | 0.23 | 1.07 | 1.03 | 0.45 | 2.34 |
| 30–119 min/d | 1.05 | 0.66 | 1.66 | 0.92 | 0.49 | 1.75 | 1.25 | 0.68 | 2.31 |
| 120–239 min/d | 0.84 | 0.51 | 1.39 | 0.78 | 0.41 | 1.50 | 0.91 | 0.42 | 1.95 |
| ≥240 min/d | 0.75 | 0.43 | 1.32 | 0.61 | 0.29 | 1.26 | 1.02 | 0.42 | 2.44 |
| Volume | |||||||||
| VPA | |||||||||
| No activity | 1.00 | 1.00 | 1.00 | ||||||
| 10–74 min/w | 1.30 | 0.30 | 5.58 | 1.86 | 0.40 | 8.62 | N/A | ||
| 75–299 min/w | 0.40 | 0.10 | 1.56 | 0.14 | 0.02 | 1.08 | 1.34 | 0.26 | 6.95 |
| ≥300 min/w | 0.68 * | 0.46 | 0.99 | 0.61 * | 0.38 | 0.99 | 0.84 | 0.49 | 1.44 |
| MPA | |||||||||
| No activity | 1.00 | 1.00 | 1.00 | ||||||
| 10–149 min/w | 0.34 * | 0.18 | 0.66 | 0.34 * | 0.12 | 0.92 | 0.35 * | 0.15 | 0.84 |
| 150–299 min/w | 0.16 * | 0.04 | 0.69 | 0.26 | 0.06 | 1.17 | N/A | ||
| ≥300 min/w | 0.38 * | 0.26 | 0.55 | 0.32 * | 0.19 | 0.54 | 0.47 * | 0.29 | 0.78 |
| LPA | |||||||||
| No activity | 1.00 | 1.00 | 1.00 | ||||||
| <150 min/w | 0.70 | 0.41 | 1.21 | 0.47 | 0.22 | 1.01 | 1.15 | 0.53 | 2.50 |
| 150–299 min/w | 0.54 | 0.15 | 1.99 | 0.63 | 0.13 | 3.15 | 0.37 | 0.05 | 2.85 |
| ≥300 min/w | 0.97 | 0.64 | 1.45 | 0.86 | 0.50 | 1.48 | 1.13 | 0.63 | 2.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, D.; Bian, Y.; Zeng, Z.; Cui, Y.; Wang, Y.; Yu, C. Associations between Intensity, Frequency, Duration, and Volume of Physical Activity and the Risk of Stroke in Middle- and Older-Aged Chinese People: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 8628. https://doi.org/10.3390/ijerph17228628
Yang D, Bian Y, Zeng Z, Cui Y, Wang Y, Yu C. Associations between Intensity, Frequency, Duration, and Volume of Physical Activity and the Risk of Stroke in Middle- and Older-Aged Chinese People: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2020; 17(22):8628. https://doi.org/10.3390/ijerph17228628
Chicago/Turabian StyleYang, Donghui, Yuqian Bian, Zixin Zeng, Yiran Cui, Yafeng Wang, and Chuanhua Yu. 2020. "Associations between Intensity, Frequency, Duration, and Volume of Physical Activity and the Risk of Stroke in Middle- and Older-Aged Chinese People: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 17, no. 22: 8628. https://doi.org/10.3390/ijerph17228628
APA StyleYang, D., Bian, Y., Zeng, Z., Cui, Y., Wang, Y., & Yu, C. (2020). Associations between Intensity, Frequency, Duration, and Volume of Physical Activity and the Risk of Stroke in Middle- and Older-Aged Chinese People: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 17(22), 8628. https://doi.org/10.3390/ijerph17228628





