A Randomised Controlled Trial of a Caregiver-Facilitated Problem-Solving Based Self-Learning Program for Family Carers of People with Early Psychosis
Abstract
:1. Introduction
2. Materials and Methods
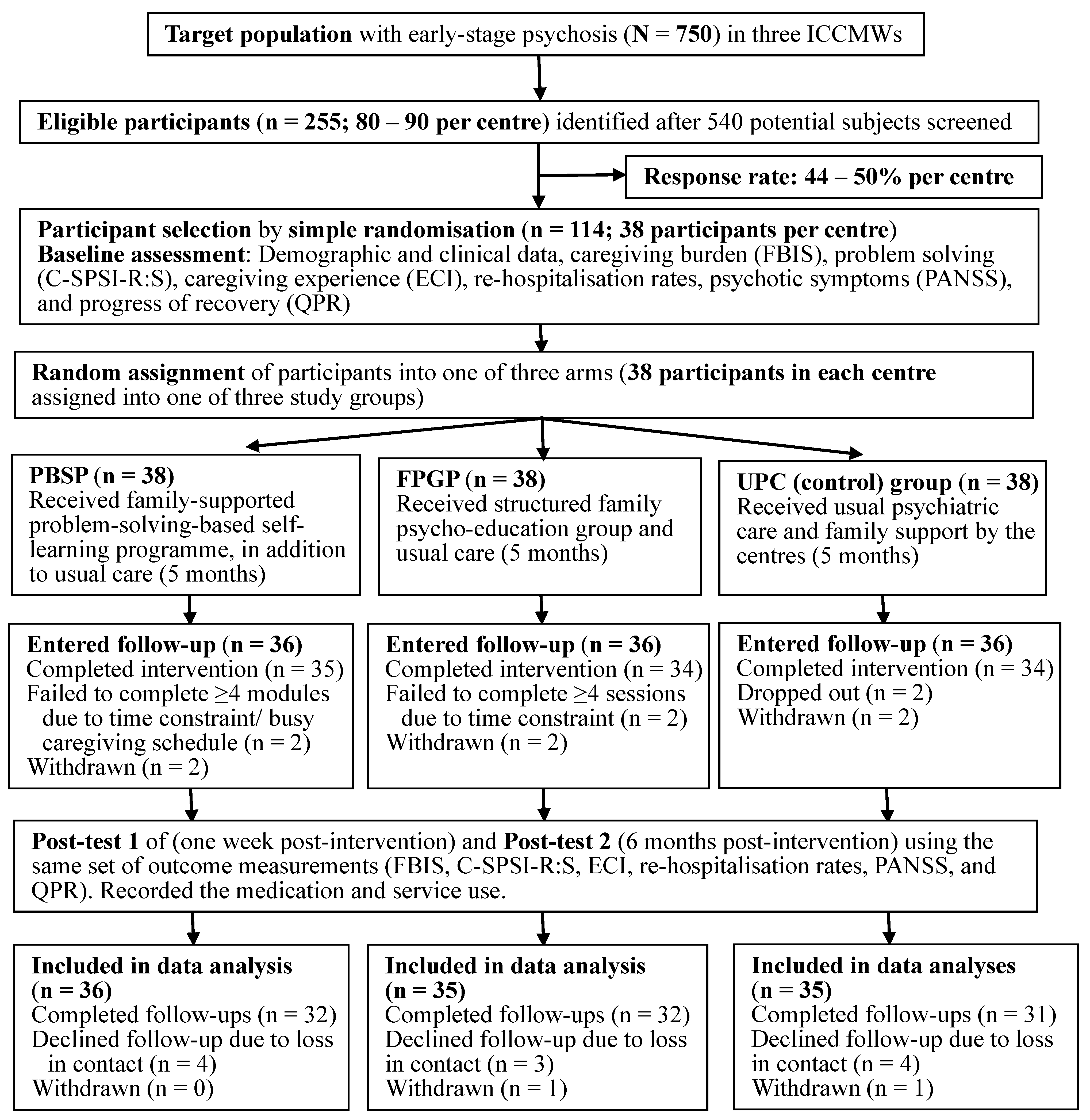
2.1. Study Design
2.2. Participants and Procedures
2.3. Measures
2.4. Interventions
2.5. Ethical Considerations
2.6. Data Collection Process
2.7. Statistical Analyses
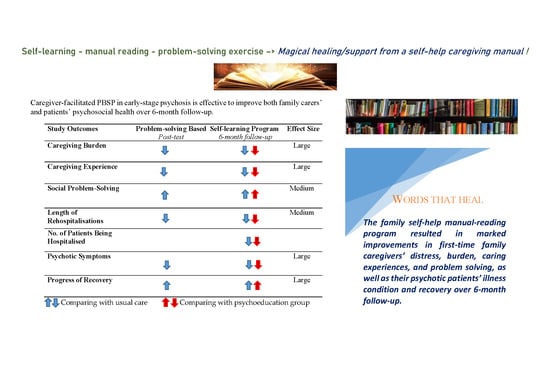
3. Results
3.1. Characteristics of Study Participants
3.2. Treatment Effects
- ▪
- Caregiving burden (FBIS) and experiences (ECI) at Time 2 (mean difference = 4.22 and 19.29, SE = 3.02 and 5.12, p = 0.01 and 0.0005, respectively) and Time 3 (MD = 9.12 and 31.97, SE = 3.91 and 8.86, p = 0.001 and 0.0001, respectively) than the UPC, and at Time 3 (MD = 3.37 and 9.69, SE = 2.98 and 5.98, both p = 0.01, respectively) than the FPGP;
- ▪
- Problem-solving ability (SPSI-R:S) at Times 2 and 3 (MD = 4.22 and 9.12, SE = 3.02 and 3.91 p = 0.01 and 0.001) than the UPC, as well as at Time 3 (MD = 3.37, SE = 2.98, p = 0.01) than the PBSP;
- ▪
- Psychotic symptoms (PANSS) and subjective recovery (QPR) at Time 2 (MD = 26.57 and 6.49, SE = 4.12 and 1.09, p = 0.005 and 0.008, respectively) and Time 3 (MD = 50.60 and 13.22, SE = 8.01 and 3.98, p = 0.0001 and 0.0003, respectively) than the UPC, and at Time 3 (MD = 15.87 and 5.74, SE = 2.98 and 1.67, p = 0.007 and 0.008) than the FPGP;
- ▪
- Average length or duration (days of hospital-stay) of re-hospitalizations at Time 3 than the UPC (MD = 7.70, SE = 3.97, p = 0.007), and FPGP (MD = 5.17, SE = 1.98, p = 0.01).
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Chien, W.T.; Leung, S.F.; Yeung, F.; Wong, W.K. Current approaches to treatments for schizophrenia spectrum disorders, part II: Psychosocial interventions and patient-focused perspectives in psychiatric care. Neuropsychiatr. Dis. Treat. 2013, 9, 1463–1481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Global Burden of Disease Study Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 743–800. [Google Scholar] [CrossRef] [Green Version]
- Owen, M.J.; Sawa, A.; Mortensen, P.B. Schizophrenia. Lancet 2016, 388, 86–97. [Google Scholar] [CrossRef] [Green Version]
- National Collaborating Centre for Mental Health and National Institute for Health and Clinical Excellence (UK). Schizophrenia: Core Interventions in the Treatment and Management of Schizophrenia in Adults in Primary and Secondary Care, updated ed.; British Psychological Society and Royal College of Psychiatrists: London, UK, 2010. [Google Scholar]
- Chien, W.T.; Yip, A.L. Current approaches to treatments for schizophrenia spectrum disorders, part I: An overview and medical treatments. Neuropsychiatr. Dis. Treat. 2013, 9, 1311–1332. [Google Scholar] [CrossRef] [Green Version]
- Thomas, B.D.; Chien, W.T.; Bressington, D.T. Family intervention for caregivers of people with recent-onset psychosis: A systematic review and meta-analysis. Early Interv. Psychiatry 2018, 12, 535–560. [Google Scholar] [CrossRef]
- Chien, W.T.; Yeung, F.K.K.; Chan, A.H.L. Perceived Stigma of Patients with Severe Mental Illness in Hong Kong: Relationships with Patients’ Psychosocial Conditions and Attitudes of Family Caregivers and Health Professionals. Adm. Policy Ment. Health Ment. Health Serv. Res. 2012, 41, 237–251. [Google Scholar] [CrossRef] [PubMed]
- Chien, W.T.; Ski, C.F.; Lubman, D.I.; McCann, T.V. A Randomized Controlled Trial of Clinician-Supported Problem-Solving Bibliotherapy for Family Caregivers of People with First-Episode Psychosis. Schizophr. Bull. 2016, 42, 1457–1466. [Google Scholar] [CrossRef] [Green Version]
- Chien, W.T.; Yip, A.L.; Liu, J.Y.W.; McMaster, T.W. The effectiveness of manual-guided, problem-solving-based self-learning programme for family caregivers of people with recent-onset psychosis: A randomised controlled trial with 6-month follow-up. Int. J. Nurs. Stud. 2016, 59, 141–155. [Google Scholar] [CrossRef] [Green Version]
- Kuipers, E.; Onwumere, J.; Bebbington, P. Cognitive model of caregiving in psychosis. Br. J. Psychiatry 2010, 196, 259–265. [Google Scholar] [CrossRef] [Green Version]
- Bird, V.J.; Premkumar, P.; Kendall, T.; Whittington, C.; Mitchell, J.; Kuipers, E. Early intervention services, cognitive–behavioural therapy and family intervention in early psychosis: Systematic review. Br. J. Psychiatry 2010, 197, 350–356. [Google Scholar] [CrossRef]
- Claxton, M.; Onwumere, J.; Fornells-Ambrojo, M. Do Family Interventions Improve Outcomes in Early Psychosis? A Systematic Review and Meta-Analysis. Front. Psychol. 2017, 8, 371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marshall, M.; Rathbone, J. Early intervention for psychosis. Cochrane Database Syst. Rev. 2011, 6, CD004718. [Google Scholar] [CrossRef] [Green Version]
- Chien, W.T.; Mui, J.H.C.; Cheung, E.F.C.; Gray, R. Effects of motivational interviewing-based adherence therapy for schizophrenia spectrum disorders: A randomized controlled trial. Trials 2015, 16, 270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCann, T.V.; Lubman, D.I.; Clark, E. First-Time Primary Caregivers’ Experience of Caring for Young Adults With First-Episode Psychosis. Schizophr. Bull. 2009, 37, 381–388. [Google Scholar] [CrossRef] [Green Version]
- Chan, H.Y.-L.; Chui, Y.; Chan, C.W.H.; Cheng, K.K.; Shiu, A.T.; So, W.K.W.; Ho, S.S.; Chan, M.M. Exploring the influence of Traditional Chinese Medicine on self-care among Chinese cancer patients. Eur. J. Oncol. Nurs. 2014, 18, 445–451. [Google Scholar] [CrossRef]
- McKenna, G.; Hevey, D.; Martin, E. Patients’ and providers’ perspectives on bibliotherapy in primary care. Clin. Psychol. Psychother. 2010, 17, 497–509. [Google Scholar] [CrossRef]
- Cotton, S.M.; McCann, T.; Gleeson, J.; Crisp, K.; Murphy, B.; Lubman, D.I. Coping strategies in carers of young people with a first episode of psychosis. Schizophr. Res. 2013, 146, 118–124. [Google Scholar] [CrossRef]
- Chien, W.T.; Clifton, A.V.; Zhao, S.; Lui, S. Peer support for people with schizophrenia or other serious mental illness. Cochrane Database Syst. Rev. 2019, 4, CD010880. [Google Scholar] [CrossRef] [Green Version]
- McCann, T.V.; Lubman, D.I.; Cotton, S.M.; Murphy, B.; Crisp, K.; Catania, L.; Marck, C.; Gleeson, J.F.M. A Randomized Controlled Trial of Bibliotherapy for Carers of Young People with First-Episode Psychosis. Schizophr. Bull. 2013, 39, 1307–1317. [Google Scholar] [CrossRef] [Green Version]
- Stevens, J.P. Applied Multivariate Statistics for the Social Sciences, 5th ed.; Routledge: New Work, NY, USA, 2009. [Google Scholar]
- Juszczak, E.; Altman, D.G.; Hopewell, S.; Schulz, K. Reporting of Multi-Arm Parallel-Group Randomized Trials: Extension of the CONSORT 2010 Statement. JAMA 2019, 321, 1610–1620. [Google Scholar] [CrossRef] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; (DSM IV-TR); American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; (DSM 5); American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Saghaei, M.; Saghaei, S. Implementation of an open-source customizable minimization program for allocation of patients to parallel groups in clinical trials. J. Biomed. Sci. Eng. 2011, 4, 734–739. [Google Scholar] [CrossRef] [Green Version]
- Chan, S.W.-C.; Yip, B.; Tso, S.; Cheng, B.-S.; Tam, W. Evaluation of a psychoeducation program for Chinese clients with schizophrenia and their family caregivers. Patient Educ. Couns. 2009, 75, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Chien, W.T.; Leung, S.F.; Chu, C.S. A nurse-led, needs-based psycho-education intervention for Chinese patients with first-onset mental illness. Contemp. Nurse 2012, 40, 194–209. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.Y.; Chair, S.Y.; Chau, J.P. The effectiveness of caregiver psychosocial interventions on the psychosocial wellbeing, physical health and quality of life of stroke family caregivers and their stroke survivors: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2012, 10, 679–797. [Google Scholar] [CrossRef]
- Pai, S.; Kapur, R.L. Impact of treatment intervention on the relationship between dimensions of clinical psychopathology, social dysfunction and burden on the family of psychiatric patients. Psychol. Med. 1982, 12, 651–658. [Google Scholar] [CrossRef]
- Lau, D.; Pang, A. Validation of the Chinese version of experience of caregiving inventory in caregivers of persons suffering from severe mental disorders. Hong Kong J. Psychiatry 2007, 17, 24–31. Available online: https://www.easap.asia/index.php/find-issues/past-issue/item/324 (accessed on 30 November 2019).
- Siu, A.M.H.; Shek, D.T.L. Relations between Social Problem Solving and Indicators of Interpersonal and Family Well-Being among Chinese Adolescents in Hong Kong. In Quality-of-Life Research in Chinese, Western and Global Contexts, Social Indicators Research Series; Shek, D.T., Chan, Y.K., Lee, P.S., Eds.; Springer: Dordrecht, The Netherlands, 2005; Volume 25, pp. 517–539. [Google Scholar]
- Bell, M.; Milstein, R.; Beam-Goulet, J.; Lysaker, P.; Cicchetti, D. The Positive and Negative Syndrome Scale and the Brief Psychiatric Rating Scale. J. Nerv. Ment. Dis. 1992, 180, 723–728. [Google Scholar] [CrossRef]
- Chien, W.T.; Chan, Z. Chinese translation and validation of the questionnaire on the process of recovery in schizophrenia and other psychotic disorders. Res. Nurs. Health 2013, 36, 400–411. [Google Scholar] [CrossRef]
- Chien, W.T.; Norman, I. The Validity and Reliability of a Chinese Version of the Family Burden Interview Schedule. Nurs. Res. 2004, 53, 314–322. [Google Scholar] [CrossRef]
- McCann, T.V.; Cotton, S.M.; Lubman, D.I. Social problem solving in carers of young people with a first episode of psychosis: A randomized controlled trial. Early Interv. Psychiatry 2015, 11, 346–350. [Google Scholar] [CrossRef] [Green Version]
- D’zurilla, T.J.; Nezu, A.M. Problem-Solving Therapy: A Positive Approach to Clinical Intervention, 3rd ed.; Springer: New York, NY, USA, 2007. [Google Scholar]
- Lehman, A.F.; Buchanan, R.W.; Dickerson, F.; Dixon, L.B.; Goldberg, R.; Green-Paden, L.; Kreyenbuhl, J. Evidence-based treatment for schizophrenia. Psychiatr. Clin. N. Am. 2003, 26, 939–954. [Google Scholar] [CrossRef]
- Bellg, A.J.; Treatment Fidelity Workgroup of the NIH Behavior Change Consortium; Borrelli, B.; Resnick, B.; Hecht, J.; Minicucci, D.S.; Ory, M.G.; Ogedegbe, G.; Orwig, D.L.; Ernst, D.; et al. Enhancing Treatment Fidelity in Health Behavior Change Studies: Best Practices and Recommendations From the NIH Behavior Change Consortium. Health Psychol. 2004, 23, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Bezchlibnyk-Butler, K.Z.; Jeffries, J.J.; Procyshyn, R.M.; Virani, A. Clinical Handbook of Psychotropic Drugs, 20th ed.; Hogrefe and Huber: Boston, MA, USA, 2013. [Google Scholar]
- Tabachnick, B.; Fidell, S. Using Multivariate Statistics, 4th ed.; Allyn and Bacon: New York, NY, USA, 2001. [Google Scholar]
- Glynn, S.M.; Cohen, A.N.; Dixon, L.B.; Niv, N. The Potential Impact of the Recovery Movement on Family Interventions for Schizophrenia: Opportunities and Obstacles. Schizophr. Bull. 2006, 32, 451–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Toole, M. Self-Management. In The Art and Science of Mental Health Nursing; Norman, I., Ryrie, I., Eds.; McGraw-Hill Higher Education: London, UK, 2013; pp. 291–305. [Google Scholar]
- Oosterbaan, D.B.; Verbraak, M.J.P.M.; Terluin, B.; Hoogendoorn, A.W.; Peyrot, W.J.; Muntingh, A.; Van Balkom, A.J.L.M. Collaborative stepped care v. care as usual for common mental disorders: 8-month, cluster randomised controlled trial. Br. J. Psychiatry 2013, 203, 132–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Theme | Goals | Content | Length of Each Theme a |
|---|---|---|---|
| Group session 1 | |||
| Orientation and engagement into group | Introduction of problem-solving, self-learning, and the PBSP manual and program, treatment goals and objectives. |
| 1 session (1.5 h group session) in the first week |
| Understanding about the illness and its treatment/care | Understanding psychosis, early stage of the illness and its care; the illness related behaviours, and management |
| |
| Five reading modules—Improving carer’s well-being and coping skills Introduction: To increase the carer’s understanding of recent-onset psychosis and appreciate how to use the problem-solving framework. Main topics include: What is psychosis? (e.g., symptoms and causes; types and myths; stereotypes and stigma; role of a carer, family and friends; common experiences of caregiving). Introduction to problem-solving approaches and self-assessment; styles and strengths and weaknesses of each psychoeducation approach. | |||
| Module 1: Carer’s well-being | Assisting the carer to work through their emotions, reflect upon how they are currently looking after themselves, and developing good coping strategies in caregiving and family care. |
D—Define correctly the problem by writing out all the facts, identify the obstacles to solving the problem, and specify a realistic goal A—(Thinking of) Alternative ways for overcoming the problem and achieving the goal P—Predict the consequence that may occur for each alterative T—Try-out the problem-solving approach in ‘real-life’ and evaluate whether the chosen approach works | Completing the module over 3 weeks |
| Group session 2 | |||
| Problem-solving activities for carers’ well-being | Assisting carers working through their emotions and challenges in caregiving |
| 1 session (1.5 h group session) after the first module |
| Module 2: Benefitting the most from support services | Enable carers to access support services and make the most of these services |
| Completing 1 module over 3–4 weeks |
| Module 3: Well-being of the person with psychotic disorders | Enhancing carers’ understanding of how to promote their own and patients’ well-being; equipping carers to provide practical and emotional support to patients |
| Completing the module over 3 weeks |
| Group session 3 | |||
| Problem-solving for maintaining the well-being of a person with psychosis | Relapse prevention and symptom management |
| 1 session (1.5 h group session) after completing the third module |
| Module 4: Dealing with the effects of the illness, Part I | Examining effective ways of carer’s communication with patient, equip carer about how to manage a patient who is lacking motivation, socially withdrawn, or engaging in risky/unstrained behaviour |
| Completing the module over 3–4 weeks |
| Module 5: Dealing with the effects of the illness, Part II | Exploring ways for carer to respond to suicidal behaviours, depression and anxiety, suicide, and self-harm |
| Completing the module over 3–4 weeks |
| Group session 4 | |||
| Practices, review, and future plans | Behavioural rehearsals of problem solving in caregiving; establishing community resources; self-reflection of learning experiences |
| 1 session (1.5 h group session) after completing the fifth module |
| Characteristics | PBSP (n = 38) f (%) or M ± SD | FPGP (n = 38) f (%) or M ± SD | UPC (n = 38) f (%) or M ± SD | Chi-Squared or ANOVA Test # | p |
|---|---|---|---|---|---|
| Family carers | |||||
| Gender | χ2 = 1.02 | 0.48 | |||
| Male | 14 (36.8) | 12 (31.6) | 12 (31.6) | ||
| Female | 24 (63.2) | 26 (68.4) | 26 (68.4) | ||
| Age (years) | 32.2 ± 8.8 CI = 26.1–39.3 | 33.9 ± 8.3 CI = 27.6–42.6 | 35.8 ± 9.0 CI = 25.8–44.9 | F = 2.18 | 0.11 |
| 18–25 | 14 (36.8) | 12 (31.6) | 13 (34.2) | ||
| 26–30 | 14 (36.8) | 15 (39.5) | 14 (36.8) | ||
| 31–35 | 5 (13.2) | 6 (15.8) | 6 (15.8) | ||
| >35 | 4 (10.5) | 5 (13.2) | 5 (13.2) | ||
| Education level | χ2 = 1.89 | 0.23 | |||
| Primary school or below | 9 (23.7) | 8 (21.1) | 10 (26.3) | ||
| Secondary school | 20 (52.6) | 19 (50.0) | 20 (52.6) | ||
| University or above | 9 (23.7) | 11 (28.9) | 8 (21.1) | ||
| Relationship with patient | χ2 = 1.28 | 0.30 | |||
| Child | 8 (21.0) | 7 (18.4) | 7 (18.4) | ||
| Parent | 12 (31.6) | 12 (31.6) | 14 (36.9) | ||
| Spouse | 13 (34.2) | 14 (36.8) | 13 (34.2) | ||
| Others (e.g., sibling) | 5 (13.2) | 5 (13.2) | 4 (10.5) | ||
| Monthly household income (HKD) ~ | 16,481 ± 4123 CI = 11,323–21,205 | 17,912 ± 513 CI = 11,211–23,533 | 17,367 ± 4902 CI = 12,250–22,887 | F = 1.81 | 0.14 |
| 10,000 or below | 7 (18.4) | 5 (13.2) | 6 (15.8) | ||
| 10,001–20,000 | 17 (44.7) | 15 (39.5) | 16 (42.1) | ||
| 20,001–30,000 | 9 (23.7) | 11 (28.9) | 9 (23.7) | ||
| >30,000 | 5 (13.2) | 7 (18.4) | 7 (18.4) | ||
| Patients | |||||
| Gender | χ2 = 1.64 | 0.16 | |||
| Male | 22 (57.9) | 23 (60.5) | 24 (63.2) | ||
| Female | 16 (42.1) | 15 (39.5) | 14 (36.8) | ||
| Age (years) | 24.2 ± 6.8 CI = 18.0–30.3 | 26.2 ± 7.8 CI = 18.8–35.3 | 26.5 ± 7.7 CI = 28.5–36.5 | F = 1.25 | 0.24 |
| 18–24 | 17 (44.7) | 16 (42.1) | 15 (39.5) | ||
| 25–30 | 15 (39.5) | 17 (44.7) | 18 (47.4) | ||
| 31–37 | 6 (15.8) | 5 (13.2) | 5 (13.2) | ||
| Education level | χ2 = 1.65 | 0.20 | |||
| Primary school or below | 8 (21.1) | 7 (18.4) | 7 (18.4) | ||
| Secondary school | 20 (52.6) | 21 (55.3) | 19 (50.0) | ||
| University or above | 10 (26.3) | 10 (26.3) | 12 (31.6) | ||
| Duration of illness (months) | 10.1 ± 4.8, range = 4.0–19.5 CI = 4.5–15.2 | 11.9 ± 5.9, range = 3.5–19.0 CI = 7.2–18.7 | 12.8 ± 6.7, range = 4.0–21.5 CI = 4.1–21.0 | F = 1.70 | 0.23 |
| 3–6 | 8 (21.1) | 9 (23.7) | 7 (18.4) | ||
| 7–12 | 16 (42.1) | 15 (39.5) | 17 (44.7) | ||
| 13–18 | 10 (26.3) | 11 (28.9) | 11 (28.9) | ||
| 19–22 | 4 (10.5) | 3 (7.9) | 3 (7.9) | ||
| Number of family members living with patient | χ2 = 1.42 | 0.28 | |||
| One | 12 (31.6) | 14 (36.8) | 15 (39.5) | ||
| 2–3 | 20 (52.6) | 20 (52.6) | 18 (47.4) | ||
| 4–5 | 6 (15.8) | 4 (10.5) | 5 (13.1) | ||
| Types of psychotropic drugs | χ2 = 1.86 | 0.21 | |||
| Conventional antipsychotics (e.g., haloperidol) | 14 (36.8) | 12 (31.6) | 13 (34.2) | ||
| Atypical antipsychotics (e.g., risperidone) | 16 (42.1) | 15 (39.5) | 15 (39.5) | ||
| Anti-depressants (e.g., fluoxetine) | 5 (13.1) | 6 (15.8) | 4 (10.5) | ||
| Blended mode ^ | 3 (7.9) | 5 (13.1) | 6 (15.8) | ||
| Use of psychiatric services | χ2 = 1.52 | 0.28 | |||
| Medical consultation and treatment planning | 36 (94.7) | 38 (100.0) | 36 (94.7) | ||
| Nursing advice on services and brief education | 38 (100.0) | 36 (94.7) | 35 (92.1) | ||
| Social welfare and financial advices | 25 (65.8) | 20 (52.6) | 17 (44.7) | ||
| Individual/family counselling | 18 (47.4) | 20 (52.6) | 10 (26.2) | ||
| Dosage of medication + | χ2 = 1.32 | 0.26 | |||
| High | 8 (21.1) | 7 (18.4) | 6 (15.8) | ||
| Medium | 15 (39.5) | 17 (44.7) | 18 (47.4) | ||
| Low | 15 (39.5) | 14 (36.9) | 14 (36.8) |
| PBSP (n = 36) | FPGP (n = 35) | UPC (n = 35) | GEE Analysis | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Time | M ± SD | 95% CI | M ± SD | 95% CI | M ± SD | 95% CI | Group Effect | Time Effect | Group × Time Effect | |
| Instrument | β (95% CI), p | β (95% CI), p | β (95% CI), p, Wald χ2, ES | |||||||
| FBIS (0–50) $ | Time 1 | 29.20 ± 6.42 | 22.61, 35.83 | 29.92 ± 5.01 | 23.0, 38.0 | 29.82 ± 6.52 | 22.10, 37.04 | 0.62 (0.32, 0.95), 0.005 | −0.68 (−0.98, −0.38), 0.008 | −2.02 (−4.48, −0.12), 0.001 Wald χ2 = 19.43, ES = 0.20 |
| Time 2 | 25.41 ± 5.81 | 19.52, 31.14 | 27.04 ± 5.95 | 19.9, 31.5 | 29.63 ± 7.12 | 22.01, 38.05 | ||||
| Time 3 | 22.82 ± 5.02 | 17.02, 29.12 | 26.13 ± 7.12 | 19.2, 33.5 | 31.94 ± 8.01 | 23.63, 40.05 | ||||
| ECI (0–204) # | Time 1 | 130.21 ± 16.43 | 114.1, 146.92 | 133.22 ± 16.52 | 116.52, 149.83 | 133.02 ± 18.42 | 114.00, 150.54 | 0.42 (0.21, 0.63), 0.01 | −0.60 (−0.98, −0.22),0.01 | −1.41 (−2.03, −0.89), 0.005 Wald χ2 = 14.12, ES = 0.18 |
| Time 2 | 118.23 ± 21.04 | 98.23, 140.82 | 119.83 ± 20.04 | 98.82, 141.42 | 137.52 ± 22.02 | 115.20, 158.54 | ||||
| Time 3 | 109.84 ± 16.41 | 88.22, 118.43 | 119.53 ± 18.81 | 99.23, 138.05 | 141.81 ± 19.21 | 120.20, 160.42 | ||||
| SPSI-R:S (0–100) | Time 1 | 51.22 ± 8.46 | 43.12, 58.93 | 50.23 ± 7.03 | 41.11, 58.24 | 50.02 ± 8.04 | 41.78, 58.26 | 0.36 (0.18, 0.54), 0.05 | 0.40 (0.21, 0.59), 0.05 | 1.01 (0.78, 1.24), 0.05 Wald χ2 = 7.05, ES = 0.12 |
| Time 2 | 56.23 ± 9.02 | 47.24, 66.05 | 53.02 ± 9.16 | 43.80, 63.06 | 48.01 ± 8.51 | 40.20, 57.02 | ||||
| Time 3 | 54.85 ± 8.43 | 45.63, 63.44 | 50.82 ± 9.05 | 42.20, 60.24 | 47.83 ± 9.23 | 28.20, 47.26 | ||||
| Re-hospitalisations | ||||||||||
| - Average Number ~ | Time 1 | 1.72 ± 0.93 | 0.62, 2.74 | 1.62 ± 1.01 | 0.50, 2.61 | 1.60 ± 0.90 | 0.60, 2.70 | 0.21 (0.10, 0.32), 0.09 | 0.18 (0.10, 0.26), 0.14 | 0.74 (0.49, 0.99), 0.10 Wald χ2 = 2.05, ES = 0.02 |
| Time 2 | 1.43 ± 0.81 | 0.63, 2.22 | 1.53 ± 1.00 | 0.51, 2.62 | 1.82 ± 1.14 | 0.68, 3.06 | ||||
| Time 3 | 1.34 ± 0.86 | 0.54, 2.12 | 1.72 ± 1.22 | 0.52, 3.22 | 1.92 ± 1.31 | 0.61, 3.23 | ||||
| - Duration ^ | Time 1 | 16.52 ± 5.85 | 10.52, 22.51 | 17.01 ± 6.44 | 11.12, 23.84 | 15.91 ± 7.12 | 7.79, 24.03 | −0.58 (−0.78, −0.18), 0.01 | −0.49 (−0.74, −0.25), 0.04 | −1.05 (−1.65, −0.45), 0.02 Wald χ2 = 7.08, ES = 0.13 |
| Time 2 | 14.02 ± 6.21 | 6.92, 20.82 | 15.21 ± 9.02 | 6.01, 24.25 | 17.83 ± 9.51 | 8.52, 27.24 | ||||
| Time 3 | 11.85 ± 8.53 | 3.52, 21.04 | 17.02 ± 9.04 | 7.78, 26.82 | 19.55 ± 10.81 | 8.54, 30.06 | ||||
| No. of patients being hospitalised | Time 1 | (17) + | (18) | (17) | KW = 6.81 @, 0.005 | |||||
| Time 2 | (11) | (14) | (16) | |||||||
| Time 3 | (8) | (13) | (20) | |||||||
| PANSS (43–215) | Time 1 | 116.53 ± 17.82 | 98.52, 135.53 | 107.22 ± 14.71 | 96.51, 123.23 | 118.12 ± 9.81 | 109.01, 128.23 | −0.68 (−0.98, −0.38), 0.005 | −0.72 (−1.13, −0.29), 0.002 | −1.36 (−1.98, −0.73), 0.001 Wald χ2 = 21.87, ES = 0.24 |
| Time 2 | 99.64 ± 19.24 | 80.03, 119.02 | 99.81 ± 12.21 | 86.00, 112.02 | 126.21 ± 17.10 | 107.99, 142.21 | ||||
| Time 3 | 88.22 ± 17.05 | 71.03, 106.25 | 104.11 ± 19.51 | 84.20, 124.23 | 138.82 ± 19.81 | 118.81, 159.03 | ||||
| QPR (0–88) | Time 1 | 38.92 ± 9.01 | 28.83, 38.02 | 39.21 ± 9.10 | 30.01, 48.31 | 38.12 ± 8.50 | 29.58, 37.02 | 0.60 (0.23, 0.87), 0.006 | 0.58 (0.25, 0.91), 0.01 | 1.64 (1.26, 1.98), 0.005 Wald χ2 = 15.28, ES = 0.18 |
| Time 2 | 43.57 ± 9.82 | 32.42, 43.84 | 40.81 ± 8.21 | 32.20, 49.42 | 37.08 ± 9.81 | 26.07, 46.89 | ||||
| Time 3 | 48.24 ± 11.05 | 37.02, 59.53 | 42.50 ± 9.22 | 32.18, 51.73 | 35.02 ± 8.31 | 26.01, 43.63 | ||||
| Contrast Tests of Mean Scores of Study Outcomes between Groups by Post-Tests | ||||||||
| Outcomes | Groups | Comparison | Mean Difference | Standard Error | 95% Confidence Intervel | Slope | p-Value | |
| Upper | Lower | |||||||
| FBIS | PBSP vs. UPC | T2 | −4.22 | 3.02 | −7.22 | −1.81 | −4.89 | 0.01 |
| T3 | −9.12 | 3.91 | −13.05 | −5.88 | −8.12 | 0.001 | ||
| PBSP vs. FPGP | T2 | −1.63 | 2.21 | −3.84 | 0.58 | 1.01 | 0.08 | |
| T3 | −3.37 | 2.98 | −6.35 | −0.39 | −3.07 | 0.01 | ||
| ECI | PBSP vs. UPC | T2 | −19.29 | 5.12 | −2.41 | −14.16 | −10.13 | 0.0005 |
| T3 | −31.97 | 8.86 | −40.83 | −23.11 | −18.12 | 0.0001 | ||
| PBSP vs. FPGP | T2 | −1.60 | 3.01 | −4.61 | 1.41 | −0.13 | 0.12 | |
| T3 | −9.69 | 5.98 | −14.67 | −3.71 | −4.15 | 0.01 | ||
| SPSI-R:S | PBSP vs. UPC | T2 | 8.22 | 3.45 | 11.66 | 4.77 | 7.01 | 0.005 |
| T3 | 7.02 | 2.02 | 9.05 | 4.98 | 5.98 | 0.008 | ||
| PBSP vs. FPGP | T2 | 3.21 | 0.87 | 4.10 | 2.35 | 2.71 | 0.07 | |
| T3 | 4.03 | 1.02 | 5.06 | 3.00 | 3.58 | 0.04 | ||
| Post-Hoc Comparisons of Study Outcomes (Continued) | ||||||||
| Outcomes | Groups | Comparison | Mean Difference | Standard Error | 95% Confidence Intervel | Slope | p-Value | |
| Upper | Lower | |||||||
| Duration of Re-hospitalisations ^ | PBSP vs. UPC | T2 | −3.81 | 2.90 | −6.71 | −0.88 | −1.01 | 0.06 |
| T3 | −7.70 | 3.97 | −11.66 | −3.74 | −6.08 | 0.007 | ||
| PBSP vs. FPGP | T2 | −1.19 | 1.09 | −2.20 | −0.10 | −0.91 | 0.07 | |
| T3 | −5.17 | 1.98 | −7.16 | −3.18 | −4.01 | 0.01 | ||
| PANSS | PBSP vs. UPC | T2 | −26.57 | 4.12 | −30.70 | −22.45 | −9.89 | 0.0005 |
| T3 | −50.60 | 8.01 | −58.60 | −42.48 | −13.43 | 0.0001 | ||
| PBSP vs. FPGP | T2 | −0.17 | 1.02 | −1.20 | 0.85 | −0.90 | 0.19 | |
| T3 | −15.89 | 2.98 | −18.88 | −12.93 | −5.76 | 0.007 | ||
| QPR | PBSP vs. UPC | T2 | 6.49 | 1.09 | 7.59 | 5.39 | 6.01 | 0.008 |
| T3 | 13.22 | 3.98 | 16.21 | 9.30 | 10.89 | 0.0003 | ||
| PBSP vs. FPGP | T2 | 2.76 | 0.91 | 3.68 | 1.83 | 3.12 | 0.06 | |
| T3 | 5.74 | 1.67 | 7.42 | 4.08 | 5.70 | 0.008 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chien, W.T.; Bressington, D.; Lubman, D.I.; Karatzias, T. A Randomised Controlled Trial of a Caregiver-Facilitated Problem-Solving Based Self-Learning Program for Family Carers of People with Early Psychosis. Int. J. Environ. Res. Public Health 2020, 17, 9343. https://doi.org/10.3390/ijerph17249343
Chien WT, Bressington D, Lubman DI, Karatzias T. A Randomised Controlled Trial of a Caregiver-Facilitated Problem-Solving Based Self-Learning Program for Family Carers of People with Early Psychosis. International Journal of Environmental Research and Public Health. 2020; 17(24):9343. https://doi.org/10.3390/ijerph17249343
Chicago/Turabian StyleChien, Wai Tong, Daniel Bressington, Dan I. Lubman, and Thanos Karatzias. 2020. "A Randomised Controlled Trial of a Caregiver-Facilitated Problem-Solving Based Self-Learning Program for Family Carers of People with Early Psychosis" International Journal of Environmental Research and Public Health 17, no. 24: 9343. https://doi.org/10.3390/ijerph17249343
APA StyleChien, W. T., Bressington, D., Lubman, D. I., & Karatzias, T. (2020). A Randomised Controlled Trial of a Caregiver-Facilitated Problem-Solving Based Self-Learning Program for Family Carers of People with Early Psychosis. International Journal of Environmental Research and Public Health, 17(24), 9343. https://doi.org/10.3390/ijerph17249343