Creating a Multisite Perinatal Psychiatry Databank: Purpose and Development
Abstract
1. Introduction
2. Materials and Methods
2.1. Overview
2.2. Standardizing the Collection of Clinical Information
2.3. Choosing the Software
2.4. Ethical Standards
3. Results
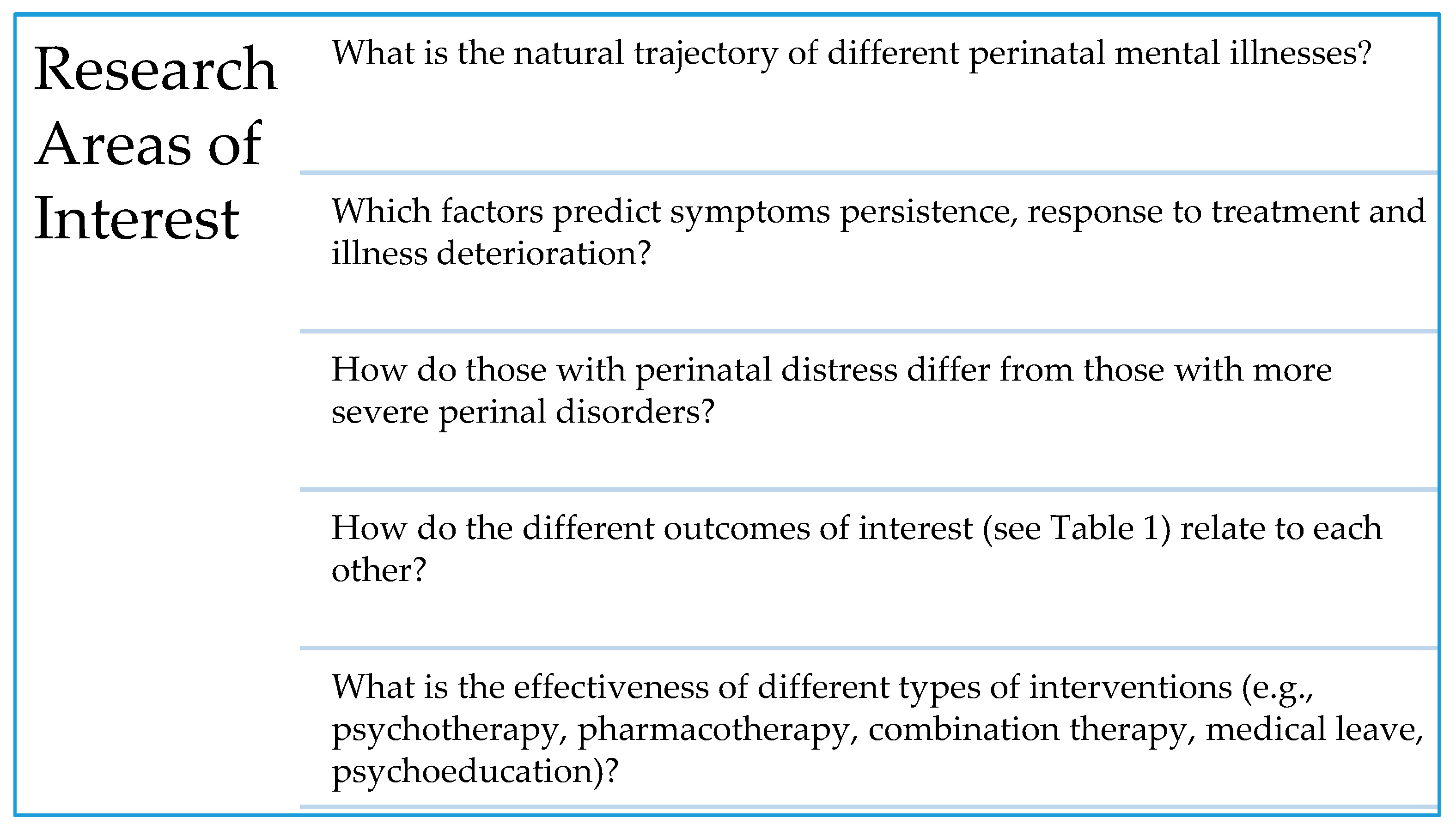
3.1. Questions
3.2. Justification of Variable Choice and Questionnaire Contents
3.3. Agreed upon Study Setting and Sample
3.4. Final Procedures
3.5. Timeline
3.6. Software
3.7. Use of the Data
4. Discussion
4.1. Summary
4.2. Databank Research Areas in Psychiatry
4.3. Perinatal Databanks
4.4. Limitations
4.5. Strengths
4.6. Challenges
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Andersson, L.; Sundström-Poromaa, I.; Wulff, M.; Aström, M.; Bixo, M. Depression and anxiety during pregnancy and six months postpartum: A follow-up study. Acta Obstet. Gynecol. Scand. 2006, 85, 937–944. [Google Scholar] [CrossRef] [PubMed]
- Barkin, J.L.; Wisner, K.L.; Bromberger, J.T.; Beach, S.R.; Wisniewski, S.R. Factors Associated with Postpartum Maternal Functioning in Women with Positive Screens for Depression. J. Womens Health 2016, 25, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Barkin, J.L.; McKeever, A.; Lian, B.; Wisniewski, S.R. Correlates of Postpartum Maternal Functioning in a Low-Income Obstetric Population. J. Am. Psychiatr. Nurses Assoc. 2017, 23, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Maina, G.; Saracco, P.; Giolito, M.R.; Danelon, D.; Bogetto, F.; Todros, T. Impact of maternal psychological distress on fetal weight, prematurity and intrauterine growth retardation. J. Affect. Disord. 2008, 111, 214–220. [Google Scholar] [CrossRef]
- Murray, L. The impact of postnatal depression on infant development. J. Child Psychol. Psychiatry 1992, 33, 543–561. [Google Scholar] [CrossRef]
- Russell, E.J.; Fawcett, J.M.; Mazmanian, D. Risk of obsessive-compulsive disorder in pregnant and postpartum women: A meta-analysis. J. Clin. Psychiatry 2013, 74, 377–385. [Google Scholar] [CrossRef]
- Vladimirova, R.; Stoyanova, V.; Milanova, V. Bipolar affective disorder, pregnancy and childbirth: Clinical characteristics and heredity. Biotechnol. Biotechnol. Equip. 2016, 30, 976–983. [Google Scholar] [CrossRef]
- Rahman, A.; Bunn, J.; Lovel, H.; Creed, F. Association between antenatal depression and low birthweight in a developing country. Acta Psychiatr. Scand. 2007, 115, 481–486. [Google Scholar] [CrossRef]
- Howard, L.M. Fertility and pregnancy in women with psychotic disorders. Eur. J. Obstet. Gynecol. Reprod. Biol. 2005, 119, 3–10. [Google Scholar] [CrossRef]
- Stein, A.; Pearson, R.M.; Goodman, S.H.; Rapa, E.; Rahman, A.; McCallum, M.; Howard, L.M.; Pariante, C.M. Effects of perinatal mental disorders on the fetus and child. Lancet Lond. Engl. 2014, 384, 1800–1819. [Google Scholar] [CrossRef]
- Leight, K.L.; Fitelson, E.M.; Weston, C.A.; Wisner, K.L. Childbirth and mental disorders. Int. Rev. Psychiatry Abingdon Engl. 2010, 22, 453–471. [Google Scholar] [CrossRef] [PubMed]
- Dietz, P.M.; Williams, S.B.; Callaghan, W.M.; Bachman, D.J.; Whitlock, E.P.; Hornbrook, M.C. Clinically identified maternal depression before, during, and after pregnancies ending in live births. Am. J. Psychiatry 2007, 164, 1515–1520. [Google Scholar] [CrossRef] [PubMed]
- Gotlib, I.H.; Whiffen, V.E.; Mount, J.H.; Milne, K.; Cordy, N.I. Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J. Consult. Clin. Psychol. 1989, 57, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Chaudron, L.H.; Klein, M.H.; Remington, P.; Palta, M.; Allen, C.; Essex, M.J. Predictors, prodromes and incidence of postpartum depression. J. Psychosom. Obstet. Gynaecol. 2001, 22, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Murray, L.; Carothers, A.D. The validation of the Edinburgh Post-natal Depression Scale on a community sample. Br. J. Psychiatry J. Ment. Sci. 1990, 157, 288–290. [Google Scholar] [CrossRef]
- Wisner, K.L.; Sit, D.K.Y.; McShea, M.C.; Rizzo, D.M.; Zoretich, R.A.; Hughes, C.L.; Eng, H.F.; Luther, J.F.; Wisniewski, S.R.; Costantino, M.L.; et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 2013, 70, 490–498. [Google Scholar] [CrossRef]
- Weinberger, M.; Oddone, E.Z.; Henderson, W.G.; Smith, D.M.; Huey, J.; Giobbie-Hurder, A.; Feussner, J.R. Multisite randomized controlled trials in health services research: Scientific challenges and operational issues. Med. Care 2001, 39, 627–634. [Google Scholar] [CrossRef]
- Higgins, N.; Howard, L. Database use in psychiatric research: An international review. Eur. J. Psychiatry 2005, 19, 19–30. [Google Scholar] [CrossRef]
- James, A.; Costello, M. The Benefits of Incorporating Clinical Research Into Physician Practices. Available online: https://www.elligohealthresearch.com/wp-content/uploads/Elligo_PhysicianPaper_11-15-19_VF.pdf (accessed on 10 October 2020).
- Gould, J.B. The role of regional collaboratives: The California Perinatal Quality Care Collaborative model. Clin. Perinatol. 2010, 37, 71–86. [Google Scholar] [CrossRef]
- Kaplan, H.C.; Lannon, C.; Walsh, M.C.; Donovan, E.F. Ohio Perinatal Quality Collaborative Ohio statewide quality-improvement collaborative to reduce late-onset sepsis in preterm infants. Pediatrics 2011, 127, 427–435. [Google Scholar] [CrossRef]
- Frosst, G.; Hutcheon, J.; Joseph, K.S.; Kinniburgh, B.; Johnson, C.; Lee, L. Validating the British Columbia Perinatal Data Registry: A chart re-abstraction study. BMC Pregnancy Childbirth 2015, 15, 123. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, L. Partnership Expands Database Available for Autism Research. Psychiatr. News 2012, 47, 19b. [Google Scholar] [CrossRef]
- Potash, J.B.; Toolan, J.; Steele, J.; Miller, E.B.; Pearl, J.; Zandi, P.P.; Schulze, T.G.; Kassem, L.; Simpson, S.G.; Lopez, V.; et al. The bipolar disorder phenome database: A resource for genetic studies. Am. J. Psychiatry 2007, 164, 1229–1237. [Google Scholar] [CrossRef] [PubMed]
- Flynn, L. The benefits and challenges of multisite studies: Lessons learned. AACN Adv. Crit. Care 2009, 20, 388–391. [Google Scholar] [CrossRef]
- Woody, C.A.; Ferrari, A.J.; Siskind, D.J.; Whiteford, H.A.; Harris, M.G. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord. 2017, 219, 86–92. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef]
- Giardinelli, L.; Innocenti, A.; Benni, L.; Stefanini, M.C.; Lino, G.; Lunardi, C.; Svelto, V.; Afshar, S.; Bovani, R.; Castellini, G.; et al. Depression and anxiety in perinatal period: Prevalence and risk factors in an Italian sample. Arch. Womens Ment. Health 2012, 15, 21–30. [Google Scholar] [CrossRef]
- Rallis, S.; Skouteris, H.; McCabe, M.; Milgrom, J. A prospective examination of depression, anxiety and stress throughout pregnancy. Women Birth J. Aust. Coll. Midwives 2014, 27, e36–e42. [Google Scholar] [CrossRef]
- Robertson, E.; Grace, S.; Wallington, T.; Stewart, D.E. Antenatal risk factors for postpartum depression: A synthesis of recent literature. Gen. Hosp. Psychiatry 2004, 26, 289–295. [Google Scholar] [CrossRef]
- Hobel, C.J.; Goldstein, A.; Barrett, E.S. Psychosocial Stress and Pregnancy Outcome. Clin. Obstet. Gynecol. 2008, 51, 333–348. [Google Scholar] [CrossRef]
- Lobel, M.; Cannella, D.L.; Graham, J.E.; DeVincent, C.; Schneider, J.; Meyer, B.A. Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychol. 2008, 27, 604–615. [Google Scholar] [CrossRef] [PubMed]
- Meltzer-Brody, S. New insights into perinatal depression: Pathogenesis and treatment during pregnancy and postpartum. Dialogues Clin. Neurosci. 2011, 13, 89–100. [Google Scholar] [PubMed]
- Nkansah-Amankra, S.; Luchok, K.J.; Hussey, J.R.; Watkins, K.; Liu, X. Effects of maternal stress on low birth weight and preterm birth outcomes across neighborhoods of South Carolina, 2000–2003. Matern. Child Health J. 2010, 14, 215–226. [Google Scholar] [CrossRef] [PubMed]
- Lamb, M.E. Patterns of Attachment: A Psychological Study of the Strange Situation; Halsted (Wiley): New York, NY, USA, 1980; pp. 68–70. [Google Scholar]
- Dozier, M.; Stovall-McClough, K.C.; Albus, K.E. Attachment and psychopathology in adulthood. In Handbook of attachment: Theory, Research, and Clinical Applications, 2nd ed.; The Guilford Press: New York, NY, USA, 2008; pp. 718–744. ISBN 978-1-59385-874-2. [Google Scholar]
- Campbell, S.B.; Brownell, C.A.; Hungerford, A.; Spieker, S.I.; Mohan, R.; Blessing, J.S. The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Dev. Psychopathol. 2004, 16, 231–252. [Google Scholar] [CrossRef]
- Brummelte, S.; Galea, L.A.M. Postpartum depression: Etiology, treatment and consequences for maternal care. Horm. Behav. 2016, 77, 153–166. [Google Scholar] [CrossRef]
- Bowlby, J. Attachment and loss: Retrospect and prospect. Am. J. Orthopsychiatry 1982, 52, 664–678. [Google Scholar] [CrossRef]
- Seng, J.S.; Sperlich, M.; Low, L.K.; Ronis, D.L.; Muzik, M.; Liberzon, I. Childhood Abuse History, Posttraumatic Stress Disorder, Postpartum Mental Health, and Bonding: A Prospective Cohort Study. J. Midwifery Womens Health 2013, 58, 57–68. [Google Scholar] [CrossRef]
- Barkin, J.L.; Wisner, K.L.; Wisniewski, S.R. The Psychometric Properties of the Barkin Index of Maternal Functioning. J. Obstet. Gynecol. Neonatal Nurs. 2014, 43, 792–802. [Google Scholar] [CrossRef]
- Mirghafourvand, M.; Barkin, J.L.; Jafarabadi, M.A.; Karami, F.; Ghanbari-Homayi, S. The psychometric properties of the Barkin index of maternal functioning (BIMF) for the Iranian population. BMC Womens Health 2019, 19, 166. [Google Scholar] [CrossRef]
- Aydın, R.; Kukulu, K. Adaptation of the Barkin scale of maternal functioning and examination of the psychometric properties. Health Care Women Int. 2018, 39, 50–64. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry J. Ment. Sci. 1987, 150, 782–786. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.L.; Chapman, G.; Murray, D.; Jones, P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in non-postnatal women. J. Affect. Disord. 1996, 39, 185–189. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Green, J.M.; Kafetsios, K.; Statham, H.E.; Snowdon, C.M. Factor structure, validity and reliability of the Cambridge Worry Scale in a pregnant population. J. Health Psychol. 2003, 8, 753–764. [Google Scholar] [CrossRef] [PubMed]
- Austin, M.-P.; Colton, J.; Priest, S.; Reilly, N.; Hadzi-Pavlovic, D. The antenatal risk questionnaire (ANRQ): Acceptability and use for psychosocial risk assessment in the maternity setting. Women Birth J. Aust. Coll. Midwives 2013, 26, 17–25. [Google Scholar] [CrossRef]
- Sims, D.; Christl, B.; Reilly, N.; Smith, M.; Chavasse, F.; Austin, M. Psychosocial assessment and mental health: Use of the Post Natal Risk Questionnaire (PNRQ) in an early parenting facility. Women Birth J. Aust. Coll. Midwives 2013, 26, 1–19. [Google Scholar] [CrossRef]
- Bartholomew, K.; Horowitz, L.M. Attachment styles among young adults: A test of a four-category model. J. Pers. Soc. Psychol. 1991, 61, 226–244. [Google Scholar] [CrossRef]
- Scharfe, E.; Bartholomew, K. Reliability and stability of adult attachment patterns. Pers. Relatsh. 1994, 1, 23–43. [Google Scholar] [CrossRef]
- Griffin, D.; Bartholomew, K. The metaphysics of measurement: The case of adult attachment. In Advances in Personal Relationships: Attachment Processes in Adulthood; Bartholomew, K., Perlman, D., Eds.; Jessica Kingsley Publishers: London, UK, 1994; Volume 5, pp. 17–52. [Google Scholar]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef]
- Murphy, A.; Steele, M.; Dube, S.R.; Bate, J.; Bonuck, K.; Meissner, P.; Goldman, H.; Steele, H. Adverse Childhood Experiences (ACEs) questionnaire and Adult Attachment Interview (AAI): Implications for parent child relationships. Child Abus. Negl. 2014, 38, 224–233. [Google Scholar] [CrossRef]
- Brockington, I.F.; Oates, J.; George, S.; Turner, D.; Vostanis, P.; Sullivan, M.; Loh, C.; Murdoch, C. A Screening Questionnaire for mother-infant bonding disorders. Arch. Womens Ment. Health 2001, 3, 133–140. [Google Scholar] [CrossRef]
- Brockington, I.F.; Fraser, C.; Wilson, D. The Postpartum Bonding Questionnaire: A validation. Arch. Womens Ment. Health 2006, 9, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Barkin, J.L.; Wisner, K.L.; Bromberger, J.T.; Beach, S.R.; Terry, M.A.; Wisniewski, S.R. Development of the Barkin Index of Maternal Functioning. J. Womens Health 2002 2010, 19, 2239–2246. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention Pregnancy Risk Assessment Monitoring System. Available online: https://www.cdc.gov/prams/index.htm (accessed on 10 October 2020).
- Partridge, E.F.; Bardyn, T.P. Research Electronic Data Capture (REDCap). J. Med. Libr. Assoc. 2018, 106, 142–144. [Google Scholar] [CrossRef]
- Simon, G.E.; Unützer, J.; Young, B.E.; Pincus, H.A. Large medical databases, population-based research, and patient confidentiality. Am. J. Psychiatry 2000, 157, 1731–1737. [Google Scholar] [CrossRef]
- The Center for Women’s Mental Health at Massachusetts General Hospital Perinatal Information Resource Center. Available online: https://womensmentalhealth.org/about/ (accessed on 10 October 2020).
- Stewart, R.; Davis, K. “Big data” in mental health research: Current status and emerging possibilities. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 1055–1072. [Google Scholar] [CrossRef]
| Variable | Measure/Tool | Reliability | Validity |
|---|---|---|---|
| Demographic characteristics | Demographic form (Tool created by QRPN) | N/A | N/A |
| Medical, obstetric and psychiatric history | Physician Form (Tool created by QRPN) | N/A | N/A |
| Depression | Edinburgh Postnatal Depression Scale [44,45] | Internal consistency: α = 0.88 [44] | Sensitivity: 63–93% Specificity: 88–99% [15] |
| Anxiety | Generalized Anxiety Disorder-7 [46] | Internal consistency: α = 0.92 [46] | Sensitivity: 89% Specificity: 82% [46] |
| Cambridge Worry Scale [47] | Internal consistency: α = 0.79 | Correlation between trait anxiety and total worry scores (r = 0.45–0.56) | |
| Psychosocial risk | Antenatal Risk Questionnaire [48] | N/A | Sensitivity: 62% Specificity: 64% |
| Postnatal Risk Questionnaire [49] | N/A | N/A | |
| Adult peer relationship style | Relationship Questionnaire [50] | Test–retest: r = 0.39 to 0.58 [51] | Convergent validity with interview attachment ratings: r = 0.22 to 0.50 [52] |
| Childhood adversity | Adverse Childhood Experiences Questionnaire [53] | Internal consistency: α = 0.88 [54] | Convergent validity with adult attachment interview: chi sq = 17.50, df = 4, p = 0.002 [54] |
| Bonding | The Postpartum Bonding Questionnaire [55] | Test–retest: Scale 1, r = 0.95 Scale 2, r = 0.95 Scale 3, r = 0.93 Scale 4, r = 0.77 [55] | * Sensitivity: Scale 1 = 82% Scale 2 = 67 to 88% [56] |
| Maternal Functioning | Barkin Index of Maternal Functioning [3,41,57] | Internal consistency: α = 0.87 [57] | Construct validity: Significant correlations found with three relevant measures [57] |
| Pregnancy Risk Assessment Monitoring System Questionnaire (PRAMS) [58] | N/A | N/A |
| Measure | Intake | ~6 Weeks Post-Partum | 4–6 Months Post-Partum |
|---|---|---|---|
| Contact information and demographics—full version | ✓ | ||
| Exercise | ✓ | ✓ | ✓ |
| Complementary alternative medicine (CAM) | ✓ | ||
| Newborn and birth information | ✓ | ||
| Demographics—update | ✓ | ✓ | |
| The Edinburgh Postnatal Depression Scale (EPDS) | ✓ | ✓ | ✓ |
| The Generalized Anxiety Disorder (GAD)-7 | ✓ | ✓ | ✓ |
| The Antenatal Risk Questionnaire (ANRQ)—full version | ✓ | ||
| Postnatal Risk Questionnaire (PNRQ) | Last 3 questions ✓ | Full version ✓ | |
| The Cambridge Worry Scale (CWS) | ✓ | ||
| The Relationship Questionnaire (RQ) | ✓ | ||
| The Adverse Childhood Experiences Questionnaire (ACE) | ✓ | ||
| The Postpartum Bonding Questionnaire (PBQ) | ✓ | ✓ | |
| Pregnancy Risk Assessment Monitoring System Questionnaire (PRAMS)—14 questions | ✓ | ✓ | |
| The Barkin Index of Maternal Functioning (BIMF) | ✓ | ✓ | |
| Physician history-taking form | ✓ | ||
| Compliance with recommendations | ✓ | ✓ | |
| COVID-19 module | ✓ |
| Measure | Intake | 4–6 Months Post-Partum |
|---|---|---|
| Contact information and demographics—full version | ✓ | |
| Exercise | ✓ | ✓ |
| Complementary alternative medicine (CAM) | ✓ | |
| Newborn and birth information | ✓ | |
| Demographics—update | ✓ | |
| The Edinburgh Postnatal Depression Scale (EPDS) | ✓ | ✓ |
| The Generalized Anxiety Disorder (GAD)-7 | ✓ | ✓ |
| Postnatal Risk Questionnaire (PNRQ)—full | ✓ | ✓ |
| The Relationship Questionnaire (RQ) | ✓ | |
| The Adverse Childhood Experiences Questionnaire (ACE) | ✓ | |
| The Postpartum Bonding Questionnaire (PBQ) | ✓ | ✓ |
| Pregnancy Risk Assessment Monitoring System Questionnaire (PRAMS)—14 questions only | ✓ | ✓ |
| The Barkin Index of Maternal Functioning (BIMF) | ✓ | ✓ |
| Physician history-taking form | ✓ | |
| Compliance with recommendations | ✓ | |
| COVID-19 module | ✓ |
| Demographic Features | Number (Percentage) | |
|---|---|---|
| Single (never married) | 18 (10.2) | 176 (Missing = 0) |
| Married | 76 (43.2) | |
| Living with your partner | 78 (44.3) | |
| Divorced/separated | 4 (2.3) | |
| Widow | 0 (0.0) | |
| Unemployed | 110 (62.9) | 175 (Missing = 1) |
| Employed | 65 (37.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kattan, W.; Avigan, L.; Hayton, B.; Barkin, J.L.; St-André, M.; Nguyen, T.-V.; Schwartz, H.; Poulin, M.-J.; Stikarovska, I.; Wolde-Giorghis, R.; et al. Creating a Multisite Perinatal Psychiatry Databank: Purpose and Development. Int. J. Environ. Res. Public Health 2020, 17, 9352. https://doi.org/10.3390/ijerph17249352
Kattan W, Avigan L, Hayton B, Barkin JL, St-André M, Nguyen T-V, Schwartz H, Poulin M-J, Stikarovska I, Wolde-Giorghis R, et al. Creating a Multisite Perinatal Psychiatry Databank: Purpose and Development. International Journal of Environmental Research and Public Health. 2020; 17(24):9352. https://doi.org/10.3390/ijerph17249352
Chicago/Turabian StyleKattan, Wid, Laura Avigan, Barbara Hayton, Jennifer L. Barkin, Martin St-André, Tuong-Vi Nguyen, Hannah Schwartz, Marie-Josée Poulin, Irena Stikarovska, Rahel Wolde-Giorghis, and et al. 2020. "Creating a Multisite Perinatal Psychiatry Databank: Purpose and Development" International Journal of Environmental Research and Public Health 17, no. 24: 9352. https://doi.org/10.3390/ijerph17249352
APA StyleKattan, W., Avigan, L., Hayton, B., Barkin, J. L., St-André, M., Nguyen, T.-V., Schwartz, H., Poulin, M.-J., Stikarovska, I., Wolde-Giorghis, R., Arafah, M., & Zelkowitz, P. (2020). Creating a Multisite Perinatal Psychiatry Databank: Purpose and Development. International Journal of Environmental Research and Public Health, 17(24), 9352. https://doi.org/10.3390/ijerph17249352






