Immediate Effects of Aquatic Therapy on Balance in Older Adults with Upper Limb Dysfunction: An Exploratory Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Subjects
2.3. Procedures for Data Collection
2.4. Intervention
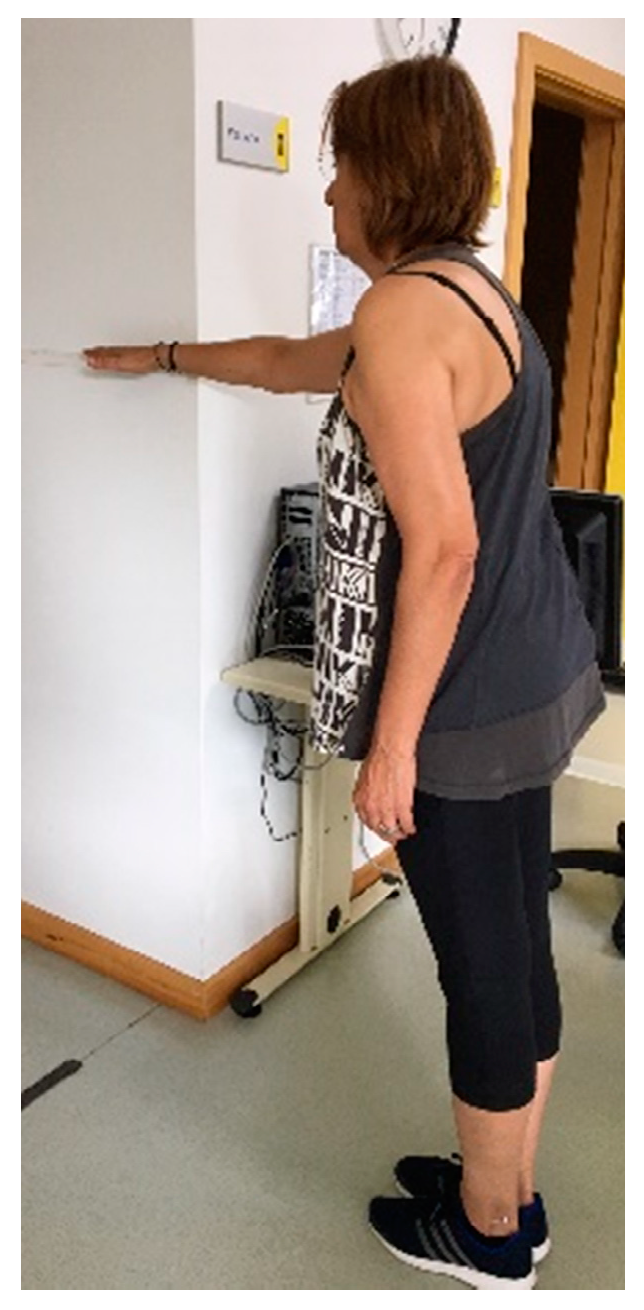
2.5. Outcomes for Data Collection
2.6. Ethical Procedures
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Turpela, M.; Häkkinen, K.; Haff, G.G.; Walker, S. Effects of different strength training frequencies on maximum strength, body composition and functional capacity in healthy older individuals. Exp. Gerontol. 2017, 98, 13–21. [Google Scholar] [CrossRef] [Green Version]
- Sherrington, C.; Tiedemann, A.; Fairhall, N.; Close, J.C.; Lord, S.R. Exercise to prevent falls in older adults: An updated meta-analysis and best practice recommendations. N. S. W. Pub. Health Bull. 2011, 22, 78–83. [Google Scholar] [CrossRef] [Green Version]
- Cadore, E.L.; Rodríguez-Mañas, L.; Sinclair, A.; Izquierdo, M. Effects of different exercise interventions on risk of falls, gait ability, and balance in physically frail older adults: A systematic review. Rejuvenation Res. 2013, 16, 105–114. [Google Scholar] [CrossRef] [Green Version]
- Freiberger, E.; Haberle, L.; Spirduso, W.W.; Zijlstra, G.A. Long-term effects of three multicomponent exercise interventions on physical performance and fall-related psychological outcomes in community-dwelling older adults: A randomized controlled trial. J. Am. Geriatr. Soc. 2012, 60, 437–446. [Google Scholar] [CrossRef]
- Hagedorn, D.K.; Holm, E. Effects of traditional physical training and visual computer feedback training in frail elderly patients. A randomized intervention study. Eur. J. Phys. Rehabil. Med. 2010, 46, 159–168. [Google Scholar] [PubMed]
- Kars Fertelli, T.; Mollaoglu, M.; Sahin, O. Aquatic exercise program for individuals with osteoarthritis: Pain, stiffness, physical function, self-efficacy. Rehabil. Nurs. J. 2018, 44, 290–299. [Google Scholar] [CrossRef]
- Adsett, J.; Morris, N.; Kuys, S.; Hwang, R.; Mullins, R.; Khatun, M.; Paratz, J.; Mudge, A. Aquatic exercise training is effective in maintaining exercise performance in trained heart failure patients: A randomised crossover pilot trial. Heart Lung Circ. 2017, 26, 572–579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alikhajeh, Y.; Hosseini, S.R.A.; Moghaddam, A. Effects of hydrotherapy in static and dynamic balance among elderly men. Procedia Soc. Behav. Sci. 2012, 46, 2220–2224. [Google Scholar] [CrossRef] [Green Version]
- Kaneda, K.; Sato, D.; Wakabayashi, H.; Hanai, A.; Nomura, T. A comparison of the effects of different water exercise programs on balance ability in elderly people. J. Aging Phys. Act. 2008, 16, 381–392. [Google Scholar] [CrossRef] [Green Version]
- Avelar, N.C.P.; Bastone, A.C.; Alcântara, M.A.; Gomes, W.F. Efetividade do treinamento de resistência à fadiga dos músculos dos membros inferiores dentro e fora d’água no equilíbrio estático e dinâmico de idosos. Braz. J. Phys. Ther. 2010, 14, 229–236. [Google Scholar] [CrossRef]
- Miyoshi, T.; Shirota, T.; Yamamoto, S.; Nakazawa, K.; Akai, M. Effect of the walking speed to the lower limb joint angular displacements, joint moments and ground reaction forces during walking in water. Disabil. Rehabil. 2004, 26, 724–732. [Google Scholar] [CrossRef]
- Wilcock, I.M.; Cronin, J.B.; Hing, W.A. Physiological response to water immersion: A method for sport recovery? Sports Med. 2006, 36, 747–765. [Google Scholar] [CrossRef]
- Torres-Ronda, L.; Del Alcazar, X.S. The properties of water and their applications for training. J. Hum. Kinet. 2014, 44, 237–248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verhagen, A.P.; Cardoso, J.R.; Bierma-Zeinstra, S.M. Aquatic exercise & balneotherapy in musculoskeletal conditions. Best Pract. Res. Clin. Rheumatol. 2012, 26, 335–343. [Google Scholar] [PubMed]
- Simmons, V.; Hansen, P.D. Effectiveness of water exercise on postural mobility in the well elderly: An experimental study on balance enhancement. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1996, 51, M233–M238. [Google Scholar] [CrossRef] [PubMed]
- Waller, B.; Munukka, M.; Multanen, J.; Rantalainen, T.; Poyhonen, T.; Nieminen, M.T.; Kiviranta, I.; Kautiainen, H.; Selanne, H.; Dekker, J.; et al. Effects of a progressive aquatic resistance exercise program on the biochemical composition and morphology of cartilage in women with mild knee osteoarthritis: Protocol for a randomised controlled trial. BMC Musculoskelet. Disord. 2013, 14, 82. [Google Scholar] [CrossRef] [Green Version]
- Waller, B.; Ogonowska-Slodownik, A.; Vitor, M.; Rodionova, K.; Lambeck, J.; Heinonen, A.; Daly, D. The effect of aquatic exercise on physical functioning in the older adult: A systematic review with meta-analysis. Age Ageing 2016, 45, 593–601. [Google Scholar] [CrossRef] [Green Version]
- So, B.C.L.; Kong, I.S.Y.; Lee, R.K.L.; Man, R.W.F.; Tse, W.H.K.; Fong, A.K.W.; Tsang, W.W.N. The effect of Ai Chi aquatic therapy on individuals with knee osteoarthritis: A pilot study. J. Phys. Ther. Sci. 2017, 29, 884–890. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.; Mehta, T.; Lai, B.; Motl, R.W. Immediate and sustained effects of interventions for changing physical activity in people with multiple sclerosis: Meta-analysis of randomized controlled trials. Arch. Phys. Med. Rehabil. 2020, 101, 1414–1436. [Google Scholar] [CrossRef]
- Martins, A.C.; Andrade, S.; Santos, D. Screening and assessment of the risk of fall: An initiative to prevent falls in community dwelling older adults. Physiotherapy 2015, 101, e958. [Google Scholar] [CrossRef] [Green Version]
- Linaker, C.H.; Walker-Bone, K. Shoulder disorders and occupation. Best Pr. Res. Clin. Rheumatol. 2015, 29, 405–423. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c869. [Google Scholar] [CrossRef] [Green Version]
- Graça, M. Development of an aquatic therapy group’s protocol program for older adults with upper limb disability. In Proceedings of the International Congress of Health and Well-Being Intervention (ICHWBI 2019), Viseu, Portugal, 31 May–1 June 2019; Desouzart, G., Ed.; Work Journal: Viseu, Portugal, 2019; p. 146. [Google Scholar]
- Meredith-Jones, K.; Waters, D.; Legge, M.; Jones, L. Upright water-based exercise to improve cardiovascular and metabolic health: A qualitative review. Complementary Ther. Med. 2011, 19, 93–103. [Google Scholar] [CrossRef]
- Lambeck, J.; Gamper, U. The Halliwick Concept. In Comprehensive Aquatic Therapy, 3rd ed.; Bruce, E., Becker, A.J.C., Eds.; Washington State University Press: Pullman, WA, USA, 2010. [Google Scholar]
- Lord, S.R.; Ward, J.A.; Williams, P.; Anstey, K.J. An epidemiological study of falls in older community-dwelling women: The Randwick falls and fractures study. Aust. J. Public Health 1993, 17, 240–245. [Google Scholar] [CrossRef]
- Methajarunon, P.; Eitivipart, C.; Diver, C.J.; Foongchomcheay, A. Systematic review of published studies on aquatic exercise for balance in patients with multiple sclerosis, Parkinson’s disease, and hemiplegia. Hong Kong Physiother. J. 2016, 35, 12–20. [Google Scholar] [CrossRef] [Green Version]
- Pérez-de la Cruz, S.; García Luengo, A.V.; Lambeck, J. Effects of an Ai Chi fall prevention programme for patients with Parkinson’s disease. Neurología 2016, 31, 176–182. [Google Scholar]
- Assis, M.R.; Silva, L.E.; Alves, A.M.; Pessanha, A.P.; Valim, V.; Feldman, D.; Neto, T.L.; Natour, J. A randomized controlled trial of deep water running: Clinical effectiveness of aquatic exercise to treat fibromyalgia. Arthritis Rheum. 2006, 55, 57–65. [Google Scholar] [CrossRef]
- Rewald, S.; Mesters, I.; Lenssen, A.F.; Emans, P.J.; Wijnen, W.; de Bie, R.A. Effect of aqua-cycling on pain and physical functioning compared with usual care in patients with knee osteoarthritis: Study protocol of a randomised controlled trial. BMC Musculoskelet. Disord. 2016, 17, 88. [Google Scholar] [CrossRef] [Green Version]
- Brady, B.; Redfern, J.; MacDougal, G.; Williams, J. The addition of aquatic therapy to rehabilitation following surgical rotator cuff repair: A feasibility study. Physiother. Res. Int. J. Res. Clin. Phys. Ther. 2008, 13, 153–161. [Google Scholar] [CrossRef]
- Burmaster, C.; Eckenrode, B.J.; Stiebel, M. Early incorporation of an evidence-based aquatic-assisted approach to arthroscopic rotator cuff repair rehabilitation: Prospective case study. Phys. Ther. 2016, 96, 53–61. [Google Scholar] [CrossRef] [Green Version]
- Bidonde, J.; Busch, A.J.; Webber, S.C.; Schachter, C.L.; Danyliw, A.; Overend, T.J.; Richards, R.S.; Rader, T. Aquatic exercise training for fibromyalgia. Cochrane Database Syst. Rev. 2014, 10, Cd011336. [Google Scholar] [CrossRef] [PubMed]
- Candeloro, J.; Caromano, F. Efeito de um programa de hidroterapia na flexibilidade e na força muscular de idosas. Braz. J. Phys. Ther. 2007, 11, 303–309. [Google Scholar] [CrossRef] [Green Version]
- Atroshi, I.; Gummesson, C.; Andersson, B.; Dahlgren, E.; Johansson, A. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: Reliability and validity of the Swedish version evaluated in 176 patients. Acta Orthop. Scand. 2000, 71, 613–618. [Google Scholar] [CrossRef]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual analog scale for pain (VAS Pain), numeric rating scale for pain (NRS Pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res. 2011, 63, S240–S252. [Google Scholar]
- Tashjian, R.Z.; Deloach, J.; Porucznik, C.A.; Powell, A.P. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J. Shoulder Elb. Surg. 2009, 18, 927–932. [Google Scholar] [CrossRef] [PubMed]
- Salaffi, F.; Stancati, A.; Silvestri, C.A.; Ciapetti, A.; Grassi, W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur. J. Pain 2004, 8, 283–291. [Google Scholar] [CrossRef]
- Devereux, K.; Robertson, D.; Briffa, N.K. Effects of a water-based program on women 65 years and over: A randomised controlled trial. Aust. J. Physiother. 2005, 51, 102–108. [Google Scholar] [CrossRef] [Green Version]
- Brauer, S.G.; Burns, Y.R.; Galley, P. A prospective study of laboratory and clinical measures of postural stability to predict community-dwelling fallers. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2000, 55, M469–M476. [Google Scholar] [CrossRef] [Green Version]
- Duncan, P.W.; Weiner, D.K.; Chandler, J.; Studenski, S. Functional reach: A new clinical measure of balance. J. Gerontol. 1990, 45, M192–M197. [Google Scholar] [CrossRef]
- Martins, A.C.; Silva, J.; Baltazar, D.; Silva, A.J.; Santos, A.; Madureira, J.; Alcobia, C.; Ferreira, L.; Mendes, P.; Tonelo, C.; et al. Fatores ambientais e prevenção de quedas_o FallSensing como solução integradora. Segurança Saúde Ocup. E Ambient. 2016. Available online: https://docplayer.com.br/51053574-Fatores-ambientais-e-prevencao-de-quedas-o-fallsensing-como-solucao-integradora.html (accessed on 15 December 2020).
- Whyatt, C.; Merriman, N.A.; Young, W.R.; Newell, F.N.; Craig, C. A Wii bit of fun: A novel platform to deliver effective balance training to older adults. Games Health J. 2015, 4, 423–433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Julious, S.A. Sample size of 12 per group rule of thumb for a pilot study. Pharm. Stat. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Blanca, M.J.; Alarcón, R.; Arnau, J.; Bono, R.; Bendayan, R. Non-normal data: Is ANOVA still a valid option? Psicothema 2017, 29, 552–557. [Google Scholar]
- Field, A. Discovering Statistics Using SPSS, 5th ed.; SAGE Publishing: Newbury Park, CA, USA, 2013. [Google Scholar]
- Dias, J.M.; Cisneros, L.; Dias, R.; Fritsch, C.; Gomes, W.; Pereira, L.; Santos, M.L.; Ferreira, P.H. Hydrotherapy improves pain and function in older women with knee osteoarthritis: A randomized controlled trial. Braz. J. Phys. Ther. 2017, 21, 449–456. [Google Scholar] [CrossRef]
- Simmerman, S.M.; Sizer, P.S.; Dedrick, G.S.; Apte, G.G.; Brismée, J.M. Immediate changes in spinal height and pain after aquatic vertical traction in patients with persistent low back symptoms: A crossover clinical trial. PM R J. Inj. Funct. Rehabil. 2011, 3, 447–457. [Google Scholar] [CrossRef]
- Moore, M.; Barker, K. The validity and reliability of the four square step test in different adult populations: A systematic review. Syst. Rev. 2017, 6, 187. [Google Scholar] [CrossRef]
- Schmitt, J.S.; Di Fabio, R.P. Reliable change and minimum important difference (MID) proportions facilitated group responsiveness comparisons using individual threshold criteria. J. Clin. Epidemiol. 2004, 57, 1008–1018. [Google Scholar] [CrossRef]
- Lord, S.; Mitchell, D.; Williams, P. Effect of water exercise on balance and related factors in older people. Aust. J. Physiother. 1993, 39, 217–222. [Google Scholar] [CrossRef] [Green Version]
- Alcalde, G.E.; Fonseca, A.C.; Bôscoa, T.F.; Gonçalves, M.R.; Bernardo, G.C.; Pianna, B.; Carnavale, B.F.; Gimenes, C.; Barrile, S.R.; Arca, E.A. Effect of aquatic physical therapy on pain perception, functional capacity and quality of life in older people with knee osteoarthritis: Study protocol for a randomized controlled trial. Trials 2017, 18, 317. [Google Scholar] [CrossRef] [Green Version]
- Bocalini, D.S.; Serra, A.J.; Rica, R.L.; Dos Santos, L. Repercussions of training and detraining by water-based exercise on functional fitness and quality of life: A short-term follow-up in healthy older women. Clinics 2010, 65, 1305–1309. [Google Scholar] [CrossRef] [Green Version]
- Cronin, N.J.; Valtonen, A.M.; Waller, B.; Pöyhönen, T.; Avela, J. Effects of short term water immersion on peripheral reflex excitability in hemiplegic and healthy individuals: A preliminary study. J. Musculoskelet. Neuronal. Interact. 2016, 16, 58–62. [Google Scholar] [PubMed]



| Characteristics | Intervention | Control | ||
|---|---|---|---|---|
| Female | Male | Female | Male | |
| Gender/n | 11 | 1 | 7 | 3 |
| Age (years)/mean (SD) | 62.9 (5.9) | 58 | 61.9 (5.6) | 75 (8.7) |
| Height (m)/mean (SD) | 1.6 (0.1) | 1.7 | 1.7 (0.8) | 1.7 (0.7) |
| Weight (Kg)/mean (SD) | 70.6 (12.4) | 100 | 65.9 (11.2) | 72.0 (11.8) |
| BMI (kg/m2)/mean (SD) | 27.8 (4.1) | 35 | 27.0 (4) | 25.0 (2) |
| Health condition * (yes/no)/n | 11/0 | 1/0 | 4/3 | 1/2 |
| Medication (yes/no)/n | 7/4 | 0/1 | 1/6 | 0/3 |
| Osteoarthritis (yes/no)/n | 10/1 | 1/0 | 1/6 | 0/3 |
| DASH Score/mean (SD) | 54 (13.8) | 67 | 28.7 (21.8) | 6.11 (5.9) |
| Outcomes | Before Mean (SD) | After Mean (SD) | |||
|---|---|---|---|---|---|
| VAS_Pain (cm) | Intervention (n = 12) | 6.2 (1.9) | 5.2 (2.3) | Time: F (1.20) = 4.31 | p < 0.05 |
| Time*group: F (1.20) = 3.86 | p = 0.06 | ||||
| Control (n = 10) | 0.9 (1.9) | 0.9 (1.9) | Group*inter subjects: F (1.20) = 97.60 | p < 0.01 | |
| ST (n) | Intervention (n = 12) | 7.0 (2.0) | 7.4 (1.8) | Time: F (1.20) = 11.20 | p < 0.01 |
| Time*group: F (1.20) = 0.39 | p = 0.54 | ||||
| Control (n = 10) | 11.23 (3.1) | 11.80 (3.3) | Group*inter subjects: F (1.20) = 297.04 | p < 0.01 | |
| FRT (cm) | Intervention (n = 12) | 9.1 (2.8) | 10.4 (3.8) | Time: F (1.20) = 4.67 | p < 0.05 |
| Time*group: F (1.20) = 1.31 | p = 0.27 | ||||
| Control (n = 10) | 20.41 (5.9) | 20.91 (5.5) | Group*inter subjects: F (1.20) = 270.43 | p < 0.01 | |
| GBST (% T in balance) | Intervention (n = 12) | 61.7 (5.9) | 71.3 (18.2) | Time: F (1.20) = 2.24 | p = 0.15 |
| Time*group: F (1.20) = 3.34 | p = 0.08 | ||||
| Control (n = 10) | 73.24 (24.3) | 72.24 (22.9) | Group*inter subjects: F (1.20) = 237.80 | p < 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Graça, M.; Alvarelhão, J.; Costa, R.; Fernandes, R.J.; Ribeiro, A.; Daly, D.; Vilas-Boas, J.P. Immediate Effects of Aquatic Therapy on Balance in Older Adults with Upper Limb Dysfunction: An Exploratory Study. Int. J. Environ. Res. Public Health 2020, 17, 9434. https://doi.org/10.3390/ijerph17249434
Graça M, Alvarelhão J, Costa R, Fernandes RJ, Ribeiro A, Daly D, Vilas-Boas JP. Immediate Effects of Aquatic Therapy on Balance in Older Adults with Upper Limb Dysfunction: An Exploratory Study. International Journal of Environmental Research and Public Health. 2020; 17(24):9434. https://doi.org/10.3390/ijerph17249434
Chicago/Turabian StyleGraça, Maria, José Alvarelhão, Rui Costa, Ricardo J. Fernandes, Andrea Ribeiro, Daniel Daly, and João Paulo Vilas-Boas. 2020. "Immediate Effects of Aquatic Therapy on Balance in Older Adults with Upper Limb Dysfunction: An Exploratory Study" International Journal of Environmental Research and Public Health 17, no. 24: 9434. https://doi.org/10.3390/ijerph17249434







