Dental Caries among Refugees in Europe: A Systematic Literature Review
Abstract
:1. Introduction
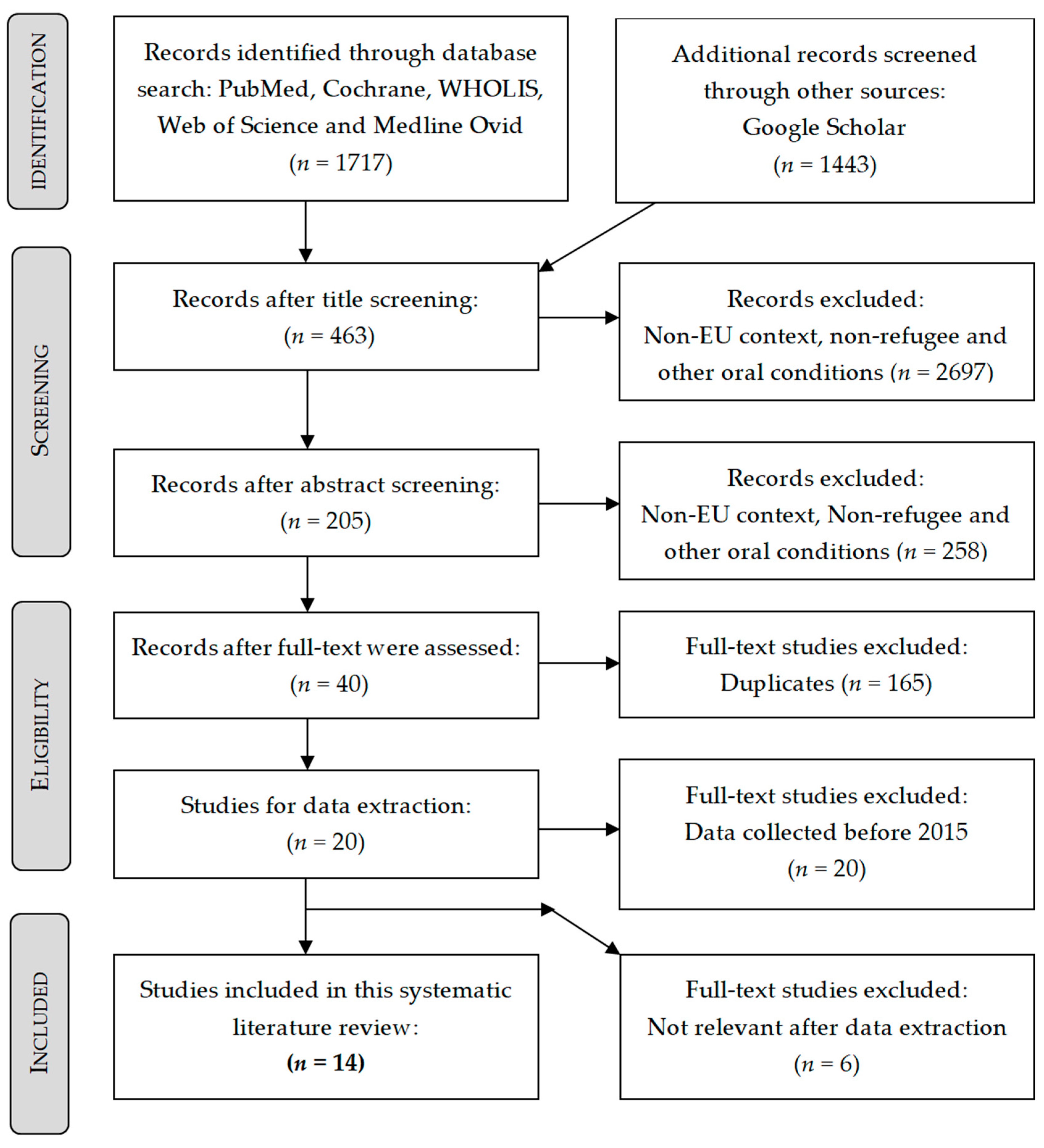
2. Materials and Methods
3. Results
Further Results
4. Discussion
5. Conclusions
Key Points
- (1)
- High prevalence of caries and limited access to dental health services are the main challenges refugees and asylum seekers face in Europe.
- (2)
- Further research is urgently needed to better understand the dental health needs of refugees in Europe.
- (3)
- The necessity of oral health check-up irrespective of need will help make the shift from curative to preventive oral health care.
Author Contributions
Funding
Conflicts of Interest
References
- Clayton, J. UNHCR Chief Issues Key Guidelines for Dealing with Europe’s Refugee Crisis UNHCR; The UN Refugee Agency. 2015. Available online: https://www.unhcr.org/55e9793b6.html (accessed on 13 June 2019).
- Williams, B.; Cassar, C.; Siggers, G.; Taylor, S. Medical and social issues of child refugees in Europe. Arch. Dis. Child 2016, 101, 839–842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perruchoud, R. Glossary on Migration. In International Migration Law; IOM (International Organization for Migration): Geneva, Switzerland, 2004; p. 233. [Google Scholar]
- United Nations High Commissioner for Refugees. A Handy Guide to UNHCR Emergency Standards and Indicators UNHCR2000 [updated 26 July 2019]. Available online: https://www.refworld.org/docid/3dee456c4.html (accessed on 29 July 2019).
- Efird, J.; Bith-Melander, P. Refugee Health: An Ongoing Commitment and Challenge; Multidisciplinary Digital Publishing Institute: Basel, Switzerland, 2018. [Google Scholar]
- Høyvik, A.C.; Lie, B.; Grjibovski, A.M.; Willumsen, T. Oral health challenges in refugees from the Middle East and Africa: A comparative study. J. Immigr. Minority Health 2019, 21, 443–450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rechel, B. Migration and Health in the European Union; McGraw-Hill Education: London, UK, 2011. [Google Scholar]
- World Health Organization. Oral Health WHO 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/oral-health (accessed on 23 June 2019).
- Glick, M.; Da Silva, O.M.; Seeberger, G.K.; Xu, T.; Pucca, G.; Williams, D.M.; Kess, S.; Eiselé, J.-L.; Séverin, T. FDI Vision 2020: Shaping the future of oral health. Int. Dent. J. 2012, 62, 278–291. [Google Scholar] [CrossRef] [PubMed]
- Maamari, A. Geriatric odontology. Revue Med Brux. 2018, 39, 322–324. [Google Scholar]
- Banu, A.; Șerban, C.; Pricop, M.; Urechescu, H.; Vlaicu, B. Dental health between self-perception, clinical evaluation and body image dissatisfaction—A cross-sectional study in mixed dentition pre-pubertal children. BMC Oral Health 2018, 18, 74. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E. Oral health. Int. Encycl. Public Health. 2008, 4, 677–685. [Google Scholar]
- Zaheer, K.; Sheikh, S.; Khalid, O.; Rizvi, Z. Refugees: Addressing the burden of oral disease through prevention. Br. Dent. J. 2017, 223, 121. [Google Scholar] [CrossRef]
- Petersen, P.E. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century—The approach of the WHO Global Oral Health Programme. Community Dent. Oral Epidemiol. 2003, 31, 3–24. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [Green Version]
- Shulman, J.D.; Cappelli, D.P. Epidemiology of dental caries. In Prevention in Clinical Oral Health Care; Elsevier: Amsterdam, The Netherlands, 2008; pp. 2–13. [Google Scholar]
- Ejcecada, L. Caries Process and Prevention Strategies: Epidemiology; American Dental Association: Niagara Falls, NY, USA, 2014. [Google Scholar]
- World Health Organization. Oral Health Surveys: Basic Methods; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- National Institute of Health. Study Quality Assessment Tools U.S. Department of Health & Human Services, National Heart, Lung and Blood Institute. 2019. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 12 June 2019).
- Mattila, A.; Ghaderi, P.; Tervonen, L.; Niskanen, L.; Pesonen, P.; Anttonen, V.; Laitala, M. Self-reported oral health and use of dental services among asylum seekers and immigrants in Finland—A pilot study. Eur. J. Public Health 2016, 26, 1006–1010. [Google Scholar] [CrossRef]
- Solyman, M.; Schmidt-Westhausen, A.-M. Oral health status among newly arrived refugees in Germany: A cross-sectional study. BMC Oral Health 2018, 18, 132. [Google Scholar] [CrossRef] [PubMed]
- Kakalou, E.; Riza, E.; Chalikias, M.; Voudouri, N.; Vetsika, A.; Tsiamis, C.; Choursoglou, S.; Terzidis, A.; Karamagioli, E.; Antypas, T.; et al. Demographic and clinical characteristics of refugees seeking primary healthcare services in Greece in the period 2015–2016: A descriptive study. Int. Health 2018, 10, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Goetz, K.; Winkelmann, W.; Steinhäuser, J. Assessment of oral health and cost of care for a group of refugees in Germany: A cross-sectional study. BMC Oral Health. 2018, 18, 69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riatto, S.G.; Montero, J.; Pérez, D.R.; Castaño-Séiquer, A.; Dib, A. Oral Health Status of Syrian Children in the Refugee Center of Melilla, Spain. Int. J. Dent. 2018, 2018, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Pavlopoulou, I.D.; Tanaka, M.; Dikalioti, S.; Samoli, E.; Nisianakis, P.; Boleti, O.D.; Tsoumakas, K. Clinical and laboratory evaluation of new immigrant and refugee children arriving in Greece. BMC Pediatr. 2017, 17, 132. [Google Scholar] [CrossRef]
- Van Berlaer, G.; Carbonell, F.B.; Manantsoa, S.; De Béthune, X.; Buyl, R.; Debacker, M.; Hubloue, I. A refugee camp in the centre of Europe: Clinical characteristics of asylum seekers arriving in Brussels. BMJ Open 2016, 6, e013963. [Google Scholar] [CrossRef] [Green Version]
- Al-Ani, A.; Takriti, M.; Schmoeckel, J.; Alkilzy, M.; Splieth, C.J.C.O.I. National oral health survey on refugees in Germany 2016/2017: Caries and subsequent complications. Clin. Oral Investig. 2020, 1–7. [Google Scholar] [CrossRef]
- Freiberg, A.; Wienke, A.; Bauer, L.; Niedermaier, A.; Führer, A.J. Dental Care for Asylum-Seekers in Germany: A Retrospective Hospital-Based Study. Int. J. Environ. Res. Public Health 2020, 17, 2672. [Google Scholar] [CrossRef]
- Hjern, A.; Kling, S. Health Care Needs in School-Age Refugee Children. Int. J. Environ. Res. Public Health 2019, 16, 4255. [Google Scholar] [CrossRef] [Green Version]
- Hermans, M.P.; Kooistra, J.; Cannegieter, S.C.; Rosendaal, F.R.; Mook-Kanamori, D.O.; Nemeth, B. Healthcare and disease burden among refugees in long-stay refugee camps at Lesbos, Greece. Eur. J. Epidemiol. 2017, 32, 851–854. [Google Scholar] [CrossRef]
- Geltman, P.L.; Adams, J.H.; Cochran, J.; Doros, G.; Rybin, D.; Henshaw, M.; Barnes, L.L.; Paasche-Orlow, M. The impact of functional health literacy and acculturation on the oral health status of Somali refugees living in Massachusetts. Am. J. Public Health 2013, 103, 1516–1523. [Google Scholar] [CrossRef] [PubMed]
- Cote, S.; Geltman, P.; Nunn, M.; Lituri, K.; Henshaw, M.; Garcia, R.I. Dental caries of refugee children compared with US children. AAP News J. Pediatr. 2004, 114, e733–e740. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willis, M.S.; Bothun, R.M. Oral hygiene knowledge and practice among Dinka and Nuer from Sudan to the US. J. Am. Dent. Hyg. Assoc. 2011, 85, 306–315. [Google Scholar]
- Ghiabi, E.; Matthews, D.C.; Brillant, M.S. The oral health status of recent immigrants and refugees in Nova Scotia, Canada. J. Immigr. Minority Health 2014, 16, 95–101. [Google Scholar] [CrossRef]
- Davidson, N.; Skull, S.; Calache, H.; Murray, S.; Chalmers, J. Holes a plenty: Oral health status a major issue for newly arrived refugees in Australia. Aust. Dent. J. 2006, 51, 306–311. [Google Scholar] [CrossRef]
- Marino, R.; Wright, F.; Minas, I. Oral health among Vietnamese using a community health centre in Richmond, Victoria. Aust. Dent. J. 2001, 46, 208–215. [Google Scholar] [CrossRef]
- Widström, E.; Eaton, K.A. Oral healthcare systems in the extended European Union. J. Oral Health Prev. Dent. 2004, 2, 155–194. [Google Scholar]
- Kitamoto, S.; Nagao-Kitamoto, H.; Hein, R.; Schmidt, T.; Kamada, N. The Bacterial Connection between the Oral Cavity and the Gut Diseases. J. Dent. Res. 2020, 99, 1021–1029. [Google Scholar] [CrossRef]
- Patini, R. Oral Microbiota: Discovering and Facing the New Associations with Systemic Diseases; Multidisciplinary Digital Publishing Institute: Basel, Switzerland, 2020. [Google Scholar]
- Monteiro, J.; Tanday, A.; Ashley, P.F.; Parekh, S.; Alamri, H. Interventions for increasing acceptance of local anaesthetic in children and adolescents having dental treatment. Cochrane Database Syst. Rev. 2020, 2, CD011024. [Google Scholar] [CrossRef]
- Patini, R.; Staderini, E.; Cantiani, M.; Camodeca, A.; Guglielmi, F.; Gallenzi, P. Dental anaesthesia for children—Effects of a computer-controlled delivery system on pain and heart rate: A randomised clinical trial. Br. J. Oral Maxillofac. Surg. 2018, 56, 744–749. [Google Scholar] [CrossRef]
- Akmal, N.; Ganapathy, D.; Visalakshi, R. Pain perception in children toward dental anesthesia–A survey. Drug Invent. Today. 2019, 12, 1475–1481. [Google Scholar]
- Pottie, K.; Greenaway, C.; Feightner, J.; Welch, V.; Swinkels, H.; Rashid, M.; Narasiah, L.; Kirmayer, L.J.; Ueffing, E.; Macdonald, N.E.; et al. Evidence-based clinical guidelines for immigrants and refugees. Can. Med. Assoc. J. 2011, 183, E824–E925. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Population | Refugee and Asylum seeker | Migration, migrant, immigrant |
| Indicator | European region | Other regions |
| Comparison | No specific comparators set | No specific comparators set |
| Outcome | Caries, Decay, DMF, Dental health | Other oral conditions of periodontium or oral mucosa |
| Author | Year | Study Type | Sample Size | Age in Years | Host Country | Country of Origin |
|---|---|---|---|---|---|---|
| [30] Hermans et al. | 2017 | Dynamic cohort | 2291 | 18–38 | Greece | Afghanistan, Pakistan and Syria |
| [21] Solyman and Schmidt-Westhausen | 2018 | Cross-sectional | 386 | 18–60 | Germany | Iraq and Syria |
| [22] Kakalou et al. | 2018 | Cross-sectional: Descriptive | 6688 | 0–75+ | Greece | Afghanistan, Iraq and Syria, other regions: Africa, Asia and the Middle East |
| [6] Høyvik et al. | 2019 | Cross-sectional: Comparative | 132 | 18–47 | Norway | Africa and The Middle East |
| [23] Goetz et al. | 2018 | Cross-sectional: Pilot | 102 | 16–64 | Germany | Afghanistan, Armenia, Chechnya, Eritrea, Iran, Iraq, Somalia, Syria and Yemen |
| [24] Riatto et al. | 2018 | Cross-sectional | 156 | 5–13 | Spain | Syria |
| [25] Pavlopoulou et al. | 2017 | Cross-sectional: Prospective | 300 | 0–14 | Greece | Afghanistan, Bangladesh, DR Congo, Eritrea, Iran, Kenya, Lebanon, Pakistan, Somalia and Sudan |
| [26] van Berlaer et al. | 2016 | Cross-sectional: Descriptive | 3907 | 0–75+ | Belgium | Afghanistan Iraq, Morocco, Palestine and Syria |
| [20] Mattila et al. | 2016 | Cross-sectional: Pilot | 38 | 17–53 | Finland | Afghanistan, Hungary, Iran, Iraq, Morocco, Russia, Slovakia, China, Somalia, South Sudan, Sweden, Syria, Thailand, Turkey and Vietnam |
| [27] Al-Ani et al. | 2020 | Cross-sectional | 544 | 3–75+ | Germany | Mainly from Afghanistan, Iraq and Syria, Others nationalities: African countries, Arabian countries, Asia and Eastern Europe |
| [29] Hjern and Kling | 2019 | Cross-sectional | 639 | 6–15 | Sweden | Afghanistan and Syria |
| [28] Freiberg et al. | 2020 | Retrospective observational | 568 | 20–34 | Germany | Afghanistan, Iran, Somalia and Syria |
| [13] Zaheer et al. | 2017 | Case report | NS | NS | Greece | Afghanistan, Kurdistan, Iraq and Syria |
| [2] Williams et al. | 2016 | Case report | NS | NS | European mainland and the UK | Afghanistan, Albania, Eritrea, Iran, Iraq and Syria |
| Study | Focus | Dentist Involved | Instruments Mentioned | DMF | Prevalence of Caries % | Reliability Tested | Guideline |
|---|---|---|---|---|---|---|---|
| [30] Hermans et al. | GH | NR | NR | NR | 2.9 * | NR | SPHERE |
| [21] Solyman and Schmidt-Westhausen | OH | Yes | Yes | Yes a | 87.5 | Yes | WHO |
| [22] Kakalou et al. | GH | NR | NR | NR | 4.6 | NR | ICD-10 |
| [6] Høyvik et al. | OH | Yes | Yes | Yes a | 89.4 | Yes | astdd |
| [23] Goetz et al. | OH | Yes | Yes | Yes a | NR | 1 Dentist | ICDAS (STROBE) |
| [24] Riatto et al. | OH | Yes | Yes | Yes b | (50–75) | Yes | WHO |
| [25] Pavlopoulou et al. | GH | NR | NR | NR | 24.7 | NR | NR |
| [26] van Berlaer et al. | GH | NR | NR | NR | 8.1 | NR | ICD-10 |
| [20] Mattila et al. | OH | Yes | NR | NR | AS 57 | NR | NR |
| [27] Al-Ani et al. | OH | Yes | Yes | Yes c | Age groups: | Yes | WHO |
| 0–3 (49) | |||||||
| 6–11 (14) | |||||||
| 13–17 (28) | |||||||
| 18–34 (10) | |||||||
| 35–44 (16) | |||||||
| 45–64 (21) | |||||||
| [29] Hjern and Kling | GH | NR | Yes | NR | 48.1 | NR | NR |
| [28] Freiberg et al. | OH | Yes | NR | NR | 98.7 | NR | (BEMA) |
| [13] Zaheer et al. | OH | Yes | NR | NR | 100 | NR | NR |
| [2] Williams et al. | GH | NR | NR | NR | 65 | NR | NR |
| Study | Average/Mean | |||||||
|---|---|---|---|---|---|---|---|---|
| DMFT | DT | MT | FT | |||||
| [21] Solyman and Schmidt-Westhausen, 2018 | 6.4 | 4.0 | 1.5 | 0.9 | ||||
| [6] Høyvik et al., 2019 | 7.4 | 4.3 | 1.4 | 1.7 | ||||
| ME | A | ME | A | ME | A | ME | A | |
| 10.7 | 5.7 | 5.2 | 3.9 | 1.6 | 1.3 | 3.9 | 0.5 | |
| [23] Goetz et al., 2018 | 6.9 | 2.9 | 3.9 | 3.8 | ||||
| DMF/Dmf for Different Age Groups: All Participants Were Children | ||||||
|---|---|---|---|---|---|---|
| DMF-dmf/Age | 5–7 | 8–10 | 11–13 | 6 | 12 | 5–13 |
| DMFT | 0.1 | 0.7 | 1.8 | 0.1 | 1.6 | 0.8 |
| DT | 0.1 | 0.7 | 1.5 | 0.1 | 1.4 | 0.7 |
| MT | 0 | 0 | 0.1 | 0 | 0 | 0 |
| MT | 0 | 0 | 0.2 | 0 | 0.2 | 0.1 |
| dft | 3.2 | 2.2 | 0.9 | 3.2 | 0 | 2.2 |
| Detailed DMF Index: Participants Were Children and Adult | ||||||||
|---|---|---|---|---|---|---|---|---|
| Age group | d | m | f | dmf | D | M | F | DMF |
| 3 | 2.54 | 0.05 | 0.03 | 2.62 | - | - | - | - |
| 6–7 | 4.21 | 0.47 | 0.55 | 5.22 | 0.12 | 0 | 0.02 | 0.13 |
| 8–11 | 2.50 | 0.53 | 0.57 | 3.60 | 0.42 | 0.02 | 0.26 | 0.70 |
| 12 | 0.62 | 0.08 | 0.15 | 0.85 | 1.12 | 0.06 | 0.82 | 2 |
| 13–17 | - | - | - | - | 1.93 | 0.23 | 0.72 | 2.87 |
| 18–34 | - | - | - | - | 3.72 | 1.46 | 2.24 | 7.43 |
| 35–44 | - | - | - | - | 3.13 | 3.22 | 4.21 | 10.55 |
| 45–64 | - | - | - | - | 3.64 | 7.63 | 3.64 | 14.92 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bhusari, S.; Ilechukwu, C.; Elwishahy, A.; Horstick, O.; Winkler, V.; Antia, K. Dental Caries among Refugees in Europe: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2020, 17, 9510. https://doi.org/10.3390/ijerph17249510
Bhusari S, Ilechukwu C, Elwishahy A, Horstick O, Winkler V, Antia K. Dental Caries among Refugees in Europe: A Systematic Literature Review. International Journal of Environmental Research and Public Health. 2020; 17(24):9510. https://doi.org/10.3390/ijerph17249510
Chicago/Turabian StyleBhusari, Sneha, Chiamaka Ilechukwu, Abdelrahman Elwishahy, Olaf Horstick, Volker Winkler, and Khatia Antia. 2020. "Dental Caries among Refugees in Europe: A Systematic Literature Review" International Journal of Environmental Research and Public Health 17, no. 24: 9510. https://doi.org/10.3390/ijerph17249510
APA StyleBhusari, S., Ilechukwu, C., Elwishahy, A., Horstick, O., Winkler, V., & Antia, K. (2020). Dental Caries among Refugees in Europe: A Systematic Literature Review. International Journal of Environmental Research and Public Health, 17(24), 9510. https://doi.org/10.3390/ijerph17249510








