Sleep Disturbances Rate among Medical and Allied Health Professions Students in Iran: Implications from a Systematic Review and Meta-Analysis of the Literature
Abstract
:1. Introduction
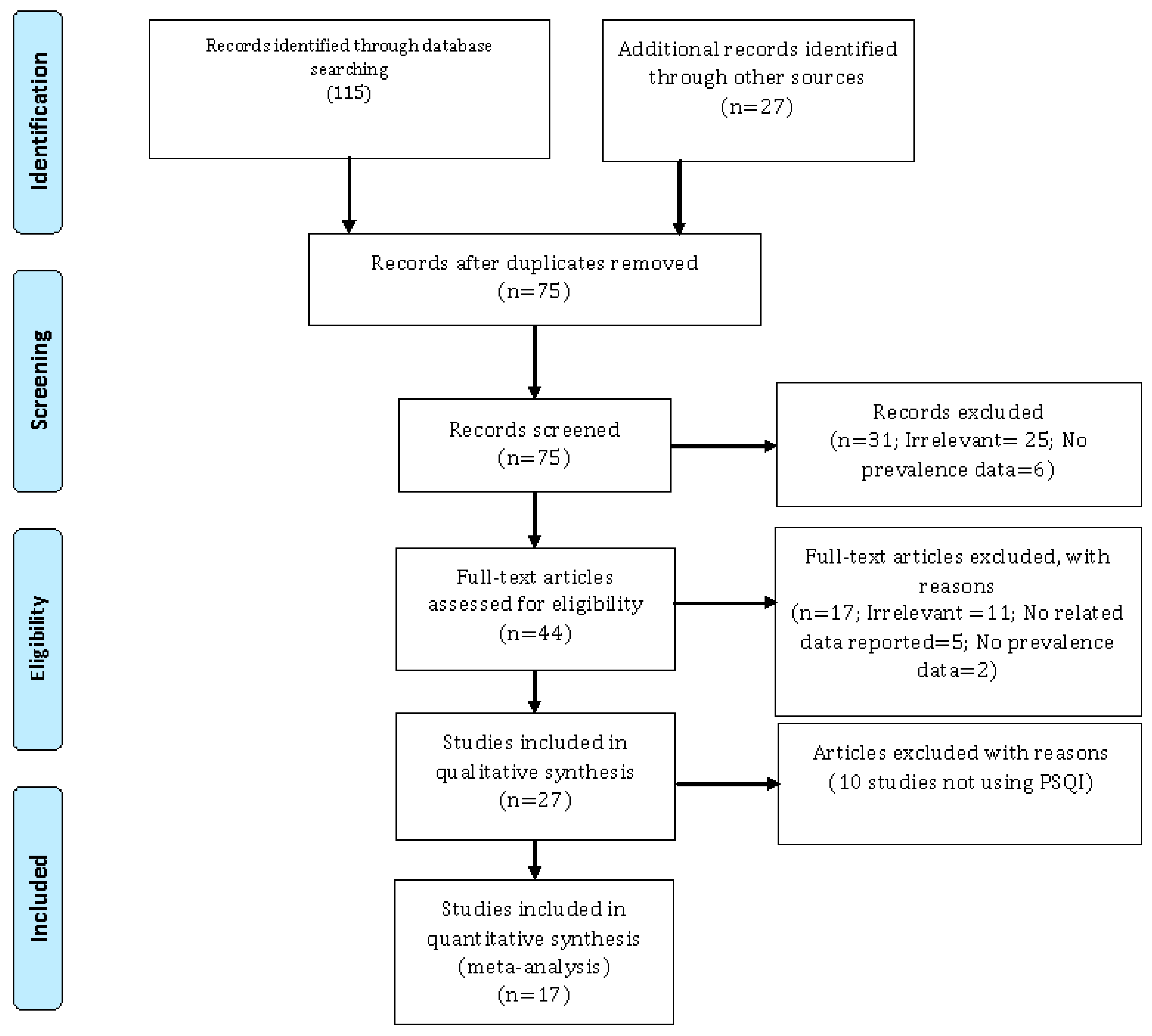
2. Materials and Methods
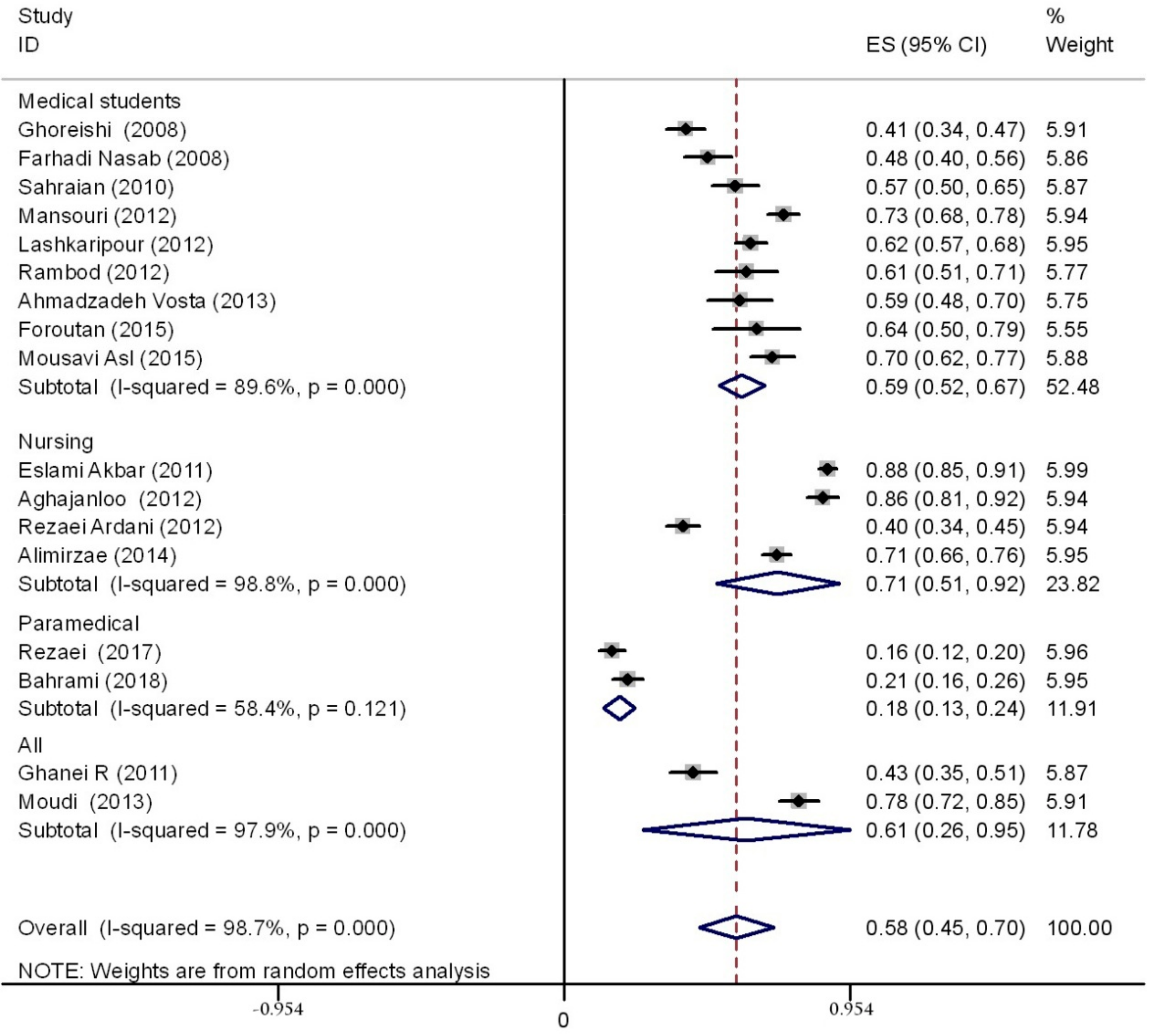
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Rich, A.; Viney, R.; Needleman, S.; Griffin, A.; Woolf, K. ‘You can’t be a person and a doctor’: The work-life balance of doctors in training-a qualitative study. BMJ. Open 2016, 6, e013897. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tafoya, S.A.; Aldrete-Cortez, V.; Ortiz, S.; Fouilloux, C.; Flores, F.; Monterrosas, A.M. Resilience, sleep quality and morningness as mediators of vulnerability to depression in medical students with sleep pattern alterations. Chronobiol. Int. 2018, in press.. [Google Scholar] [CrossRef] [PubMed]
- Norbury, R.; Evans, S. Time to think: Subjective sleep quality, trait anxiety and university start time. Psychiatry Res. 2018, 271, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Azad, M.C.; Fraser, K.; Rumana, N.; Abdullah, A.F.; Shahana, N.; Hanly, P.J.; Turin, T.C. Sleep disturbances among medical students: A global perspective. J. Clin. Sleep Med. 2015, 11, 69–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phan, D.V.; Chan, C.L.; Pan, R.H.; Yang, N.P.; Hsu, H.C.; Ting, H.W.; Lai, K.R.; Lin, K.B. Investigating the effect of daily sleep on memory capacity in college students. Technol. Health Care 2018, in press.. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Sadat, M.; Cukor, D. Sleep Knowledge and Behaviors in Medical Students: Results of a Single Center Survey. Acad. Psychiatry 2017, 41, 674–678. [Google Scholar] [CrossRef]
- Corrêa, C.C.; Oliveira, F.K.; Pizzamiglio, D.S.; Ortolan, E.V.P.; Weber, S.A.T. Sleep quality in medical students: A comparison across the various phases of the medical course. J. Bras. Pneumol. 2017, 43, 285–289. [Google Scholar] [CrossRef]
- Sateia, M.J.; Reed, V.A.; Christian Jernstedt, G. The Dartmouth sleep knowledge and attitude survey: Development and validation. Sleep Med. 2005, 6, 47–54. [Google Scholar] [CrossRef]
- Salas, R.E.; Gamaldo, A.; Collop, N.A.; Gulyani, S.; Hsu, M.; David, P.M.; Rao, A.; Gamaldo, C.E. A step out of the dark: Improving the sleep medicine knowledge of trainees. Sleep Med. 2013, 14, 105–108. [Google Scholar] [CrossRef]
- Magnavita, N.; Di Stasio, E.; Capitanelli, I.; Lops, E.A.; Chirico, F.; Garbarino, S. Sleep Problems and Workplace Violence: A Systematic Review and Meta-Analysis. Front. Neurosci. 2019, 13, 997. [Google Scholar] [CrossRef]
- Manzar, M.D.; Rajput, M.M.; Zannat, W.; Hameed, U.A.; Al-Jarrah, M.D.; Spence, D.W.; Pandi-Perumal, S.R.; BaHammam, A.S.; Hussain, M.E. Association between sleep quality and inflammatory complement components in collegiate males. Sleep Breath. 2016, 20, 867–872. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Jin, H.; Shen, S.; Li, Z.; Gu, G. Influence of clinical practice on nursing students’ mental and immune-endocrine functions. Int. J. Nurs. Pract. 2015, 21, 392–400. [Google Scholar] [CrossRef]
- Matzner, P.; Hazut, O.; Naim, R.; Shaashua, L.; Sorski, L.; Levi, B.; Sadeh, A.; Wald, I.; Bar-Haim, Y.; Ben-Eliyahu, S. Resilience of the immune system in healthy young students to 30-hour sleep deprivation with psychological stress. Neuroimmunomodulation 2013, 20, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS. Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Bull. World Health Organ. 2007, 85, 867–872. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [Green Version]
- Aryankhesal, A.; Behzadifar, M.; Bragazzi, N.L.; Ghashghaee, A.; Behzadifar, M. A framework for conducting meta-analysis studies; methodological concerns and recommendations. Iran. J. Public Health 2018, 47, 773–774. [Google Scholar]
- Aghajanloo, A.; Haririan, H.; Ghafourifard, M.; Bagheri, H.; Ebrahimi, S. Sleep quality of students during final exams in Zanjan University of medical sciences. Mod. Care J. 2012, 8, 230–237. [Google Scholar]
- Ahmadzadeh Vosta, H.; Hossaini, R.; Saneei, H. The relationships between sleep habits and times with sleep quality among college students. J. Ilam Univ. Med. Sci. 2013, 21, 273–283. [Google Scholar]
- Alimirzae, R.; Azzizadeh Forouzi, M.; Abazari, F.; Haghdoost, A. Prevalence of quality of sleeping and its determinants among students of Kerman Razi School of nursing and midwifery. Asian J. Nurs. Edu. Res. 2014, 4, 76–80. [Google Scholar]
- Bahrami, M.; Dehdashti, A.; Karami, M. Sleep quality and its causes and consequences from the perspectives of students residing in the dormitories of school of health: A cross-sectional study in Semnan University of medical sciences in 2016. Koomesh 2018, 20, 96–104. [Google Scholar]
- Eslami Akbar, R. The prevalence of sleep disorder and its causes and effects on students residing in Jahrom University of Medical Sciences dormitories, 2008. J. Jahrom Univ. Med. Sci. 2011, 9, 14–19. [Google Scholar] [CrossRef] [Green Version]
- Farhadi Nasab, A.; Azimi, H. Study of Patterns and Subjective Quality of Sleep and Their Correlation with Personality Traits among Medical Students of Hamadan University of Medical Sciences. Avicenna J. Clin. Med. 2008, 15, 11–15. [Google Scholar]
- Foroutan, B.; Abolhassani, M.; Eftekhari, N. An investigation of the prevalence of sleep disturbances among medical students of Shahroud Islamic Azad University in 2013. J. Chem. Pharm. Res. 2015, 7, 623–626. [Google Scholar]
- Ghanei, R.; Hemmati Maslakpak, M.; Rezaei, K.; Baghi, V.; Makki, B. Nursing students quality of sleep in dormitories of Urmia university of medical sciences. J. Urmia Nurs. Midwifery. Fac. 2011, 9, 1–6. [Google Scholar]
- Ghoreishi, A.; Aghajani, A.H. Sleep quality in Zanjan university medical students. Tehran Univ. Med. J. 2008, 66, 61–67. [Google Scholar]
- Lashkaripour, K.; Bakhshani, N.M.; Mafi, S. Sleep quality assessment of medicine students and physician (medical) assistants. Interdiscip. J. Contemp. Res. Business 2012, 4, 443–450. [Google Scholar]
- Mansouri, A.; Mokhayeri, Y.; Mohammadi Farrokhran, E.; Tavakkol, Z.; Fotouhi, A. Sleep quality of students living in dormitories in Tehran university of medical sciences (TUMS) in 2011. Iranian J. Epidemiol. 2012, 8, 71–82. [Google Scholar]
- Moudi, S.; Saleh Ahangar, M.; Hosseini, S.; Khafri, S. Prevalence of sleep disturbances among medical students of Babol university of medical sciences, Iran, 2013. J. Babol Univ. Med. Sci. 2014, 16, 69–74. [Google Scholar]
- Mousavi Asl, S.E.; Alizadeh, T.; Sheikh, M. Prevalence of Sleep disturbances among medical students of Yasuj University of Medical Sciences. Aligoodarz Nurs. Coll. Anal. Res. J. 2015, 6, 55–62. [Google Scholar]
- Rambod, M.; Ghodsbin, F.; Beheshtipour, N.; Raieyatpishe, A.A.; Mohebi Noubandegani, Z.; Mohammadi-Nezhad, A. The relationship between perceived social support and quality of sleep in nursing students. Iran J. Nurs. 2012, 25, 12–23. [Google Scholar]
- Rezaei Ardani, A.; Talaei, A.; Borhani Moghani, M.; Nejati, R.; Sabouri, S.; Solooti, S.; Hosseini, S.A. Assessment the rules of demographic variables and body mass index in sleep quality among medical students. J. Fundam. Ment. Health 2012, 14, 132–139. [Google Scholar]
- Rezaei, O.; Mokhayeri, Y.; Haroni, J.; Rastani, M.J.; Sayadnasiri, M.; Ghisvand, H.; Noroozi, M.; Armoon, B. Association between sleep quality and quality of life among students: A cross sectional study. Int. J. Adolesc. Med. Health 2017, 20170111. [Google Scholar] [CrossRef] [PubMed]
- Sahraian, A.; Javadpour, A. Sleep disruption and its correlation to psychological distress among medical students. Shiraz E-Med. J. 2010, 11, 20378. [Google Scholar]
- Byrd, K.; Gelaye, B.; Tadessea, M.G.; Williams, M.A.; Lemma, S.; Berhanec, Y. Sleep disturbances and common mental disorders in college students. Health Behav. Policy Rev. 2014, 1, 229–237. [Google Scholar] [CrossRef]
- Hysing, M.; Harvey, A.G.; Linton, S.J.; Askeland, K.G.; Sivertsen, B. Sleep and academic performance in later adolescence: Results from a large population-based study. J. Sleep Res. 2016, 25, 318–324. [Google Scholar] [CrossRef]
- Pacheco, J.P.; Giacomin, H.T.; Tam, W.W.; Ribeiro, T.B.; Arab, C.; Bezerra, I.M.; Pinasco, G.C. Mental health problems among medical students in Brazil: A systematic review and meta-analysis. Braz. J. Psychiatr. 2017, 39, 369–378. [Google Scholar] [CrossRef] [Green Version]
- Becker, S.P.; Jarrett, M.A.; Luebbe, A.M.; Garner, A.A.; Burns, G.L.; Kofler, M.J. Sleep in a large, multi-university sample of college students: Sleep problem prevalence, sex differences, and mental health correlates. Sleep Health 2018, 4, 174–181. [Google Scholar] [CrossRef]
- Ayala, E.E.; Berry, R.; Winseman, J.S.; Mason, H.R. A Cross-Sectional Snapshot of Sleep Quality and Quantity Among US Medical Students. Acad. Psychiatry 2017, 41, 664–668. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, A.F.; Al-Musa, H.; Al-Amri, H.; Al-Qahtani, A.; Al-Shahrani, M.; Al-Qahtani, M. Sleep Patterns and Predictors of Poor Sleep Quality among Medical Students in King Khalid University, Saudi Arabia. Malays. J. Med. Sci. 2016, 23, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Lohitashwa, R.; Kadli, N.; Kisan, R.; Sindhuja, A.; Deshpande, D. Effect of stress on sleep quality in young adult medical students: A cross sectional study. Int. J. Res. Med. Sci. 2015, 3, 3519–3523. [Google Scholar] [CrossRef] [Green Version]
- Yazdi, Z.; Lookzadeh, Z.; Abbasi, M.; Ziaeeha, M.; Mahmoodi, M. Prevalence of insomnia and its relation with academic performance of medical students in Qazvin University of Medical Sciences. J. Med. Educ. Dev. 2013, 2013, 1. [Google Scholar]
- Hosanei, S.H.; Mosavy, M.H. The comparative study of health status of medical students and para-medical students trainee. J. Gorgan Univ. Med. Sci. 2004, 6, 101–107. [Google Scholar]
- James, B.O.; Omoaregba, J.O.; Igberase, O.O. Prevalence and correlates of poor sleep quality among medical students at a Nigerian university. Ann. Nigerian Med. 2011, 5, 1–5. [Google Scholar] [CrossRef]
- Giri, P.A.; Baviskar, M.P.; Phalke, D.B. Study of Sleep Habits and Sleep Problems Among Medical Students of Pravara Institute of Medical Sciences Loni, Western Maharashtra, India. Ann. Med. Health Sci. Res. 2013, 3, 51–54. [Google Scholar] [CrossRef] [Green Version]
- Surani, A.A.; Zahid, S.; Surani, A.; Ali, S.; Mubeen, M.; Khan, R.H. Sleep quality among medical students of Karachi, Pakistan. J. Pak. Med. Assoc. 2015, 65, 380–382. [Google Scholar]
- Alsaggaf, M.A.; Wali, S.O.; Merdad, R.A.; Merdad, L.A. Sleep quantity, quality, and insomnia symptoms of medical students during clinical years. Saudi Med. J. 2016, 37, 173–182. [Google Scholar] [CrossRef]
- Li, L.; Wang, Y.Y.; Wang, S.B.; Zhang, L.; Li, L.; Xu, D.D.; Ng, C.H.; Ungvari, G.S.; Cui, X.; Liu, Z.M.; et al. Prevalence of sleep disturbances in Chinese university students: A comprehensive meta-analysis. J. Sleep Res. 2018, 27, e12648. [Google Scholar] [CrossRef]
- Abdulghani, H.M.; AlKanhal, A.A.; Mahmoud, E.S.; Ponnamperuma, G.G.; Alfaris, E.A. Stress and its effects on medical students: A cross-sectional study at a college of medicine in Saudi Arabia. J. Health Popul. Nutr. 2011, 29, 516–522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrer, M.; Adam, S.H.; Baumeister, H.; Cuijpers, P.; Karyotaki, E.; Auerbach, R.P.; Kessler, R.C.; Bruffaerts, R.; Berking, M.; Ebert, D.D. Internet interventions for mental health in university students: A systematic review and meta-analysis. Int. J. Methods Psychiatr. Res. 2018, in press.. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morgenthaler, T.I.; Hashmi, S.; Croft, J.B.; Dort, L.; Heald, J.L.; Mullington, J. High School Start Times and the Impact on High School Students: What We Know, and What We Hope to Learn. J. Clin. Sleep Med. 2016, 12, 1681–1689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tabrizi, R.; Moosazadeh, M.; Razzaghi, A.; Akbari, M.; Heydari, S.T.; Kavari, S.H.; Mani, A.; Kazemi, M.; Bagheri Lankarani, K. Prevalence of sleep quality disorder among Iranian drivers: A systematic review and meta-analysis. J. Inj. Violence Res. 2018, 10, 53–59. [Google Scholar] [PubMed]



| First Author | Study Year | City | Mean Age (± Standard Deviation; Minimum–Maximum) | Sample Size | Prevalence Rate (%) |
|---|---|---|---|---|---|
| Ghoreishi | 2008 | Zanjan | 23 ± 2.81 | 224 | 40.6 |
| Farhadi Nasab | 2008 | Hamadan | 21.73 ± 3.5 | 150 | 48.0 |
| Sahraian | 2010 | Shiraz | 21.5 ± 2.67 | 159 | 57.2 |
| Eslami Akbar | 2011 | Jahrom | 17–27 * | 418 | NA |
| Ghanei | 2011 | Urmia | 21 | 160 | 43.1 |
| Mansouri | 2012 | Tehran | 23.4 ± 2.7 | 277 | 73.3 |
| Aghajanloo | 2012 | Zanjan | 20.62 ± 1.26 | 162 | 86.4 |
| Rezaei Ardani | 2012 | Mashhad | 22.7 ± 2.6 | 310 | 39.8 |
| Rambod | 2012 | Shiraz | NA | 87 | 61.0 |
| Lashkaripour | 2012 | Zahedan | NA | 340 | 62.4 |
| Moudi | 2013 | Babol | 20–35 * | 153 | 78.8 |
| Ahmadzadeh Vosta | 2013 | Tehran | 26.1 ± 5.1 | 80 | 58.8 |
| Alimirzae | 2014 | Kerman | NA | 349 | 71.0 |
| Mousavi Asl | 2015 | Yasuj | 18–31 * | 151 | 69.95 |
| Foroutan | 2015 | Shahroud | 22.66 ± 0.90 | 42 | 64.3 |
| Rezaei | 2017 | Tehran | 22.1 ± 3.6 | 275 | NA |
| Bahrami | 2018 | Semnan | 21.78 ± 2.91 | 249 | NA |
| Variables | Coefficient | Standard Error | Statistical Significance (p-Value) | Lower 95% CI | Upper 95% CI |
|---|---|---|---|---|---|
| Sample size | 0.0000155 | 0.0005143 | 0.976 | −0.0010808 | 0.0011118 |
| Year of publication | −0.0201732 | 0.0191123 | 0.308 | −0.0609101 | 0.0205636 |
| Average age of students | 0.0375554 | 0.0314417 | 0.260 | −0.032501 | 0.1076119 |
| Variables | Number of Studies | Number of Participants | Prevalence Rate and 95%CI | I2 | Statistical Significance (p-Value) |
|---|---|---|---|---|---|
| Methodological quality of the studies included | |||||
| 1–8 (weak quality) | 3 | 397 | 50% (41–60) | 73.3% | 0.000 |
| 9–16 (moderate quality) | 5 | 1219 | 59% (30–88) | 99.44% | 0.000 |
| 17–22 (good quality) | 9 | 1970 | 59% (43–75) | 98.4% | 0.000 |
| Sample sizes of the studies included | |||||
| Less than 200 participants | 9 | 1144 | 63% (52–74) | 94% | 0.000 |
| More than 200 participants | 8 | 2442 | 52% (31–72) | 99.3% | 0.000 |
| Region where the studies included were conducted | |||||
| North | 4 | 785 | 75% (22–91) | 99.2% | 0.000 |
| West | 6 | 1006 | 58% (41–74) | 97% | 0.000 |
| East | 5 | 1290 | 52% (32–71) | 98.3% | 0.000 |
| South | 2 | 505 | 75% (48–93) | 95.9% | 0.000 |
| Determinants | Number of Studies per Determinant | Number of Studies Reporting a Significant Impact of Determinants on Sleep Disturbances |
|---|---|---|
| Poor student dormitories | 11 (64.7%) | 10 (90.9%) |
| Age | 9 (52.9%) | 6 (66.7%) |
| Family avoidance | 9 (52.9%) | 8 (88.9%) |
| Hospital-related activities | 8 (47.1%) | 8 (100.0%) |
| Fatigue | 7 (41.2%) | 4 (57.1%) |
| High workload and volume of college lessons | 7 (41.2%) | 5 (71.4%) |
| Marriage | 7 (41.2%) | 5 (71.4%) |
| Depression | 6 (35.3%) | 3 (50.0%) |
| Family problems | 5 (29.4%) | 3 (60.0%) |
| Sex | 5 (29.4%) | 3 (60.0%) |
| Economic problems | 4 (23.5%) | 2 (50.0%) |
| Drug use | 3 (17.6%) | 1 (33.3%) |
| Anxiety | 2 (11.8%) | 1 (50.0%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khaksarian, M.; Behzadifar, M.; Behzadifar, M.; Jahanpanah, F.; Guglielmi, O.; Garbarino, S.; Lanteri, P.; Re, T.S.; Zerbetto, R.; Maldonado Briegas, J.J.; et al. Sleep Disturbances Rate among Medical and Allied Health Professions Students in Iran: Implications from a Systematic Review and Meta-Analysis of the Literature. Int. J. Environ. Res. Public Health 2020, 17, 1011. https://doi.org/10.3390/ijerph17031011
Khaksarian M, Behzadifar M, Behzadifar M, Jahanpanah F, Guglielmi O, Garbarino S, Lanteri P, Re TS, Zerbetto R, Maldonado Briegas JJ, et al. Sleep Disturbances Rate among Medical and Allied Health Professions Students in Iran: Implications from a Systematic Review and Meta-Analysis of the Literature. International Journal of Environmental Research and Public Health. 2020; 17(3):1011. https://doi.org/10.3390/ijerph17031011
Chicago/Turabian StyleKhaksarian, Mojtaba, Masoud Behzadifar, Meysam Behzadifar, Firuzeh Jahanpanah, Ottavia Guglielmi, Sergio Garbarino, Paola Lanteri, Tania Simona Re, Riccardo Zerbetto, Juan José Maldonado Briegas, and et al. 2020. "Sleep Disturbances Rate among Medical and Allied Health Professions Students in Iran: Implications from a Systematic Review and Meta-Analysis of the Literature" International Journal of Environmental Research and Public Health 17, no. 3: 1011. https://doi.org/10.3390/ijerph17031011
APA StyleKhaksarian, M., Behzadifar, M., Behzadifar, M., Jahanpanah, F., Guglielmi, O., Garbarino, S., Lanteri, P., Re, T. S., Zerbetto, R., Maldonado Briegas, J. J., Riccò, M., & Bragazzi, N. L. (2020). Sleep Disturbances Rate among Medical and Allied Health Professions Students in Iran: Implications from a Systematic Review and Meta-Analysis of the Literature. International Journal of Environmental Research and Public Health, 17(3), 1011. https://doi.org/10.3390/ijerph17031011










