Comparison of Acute Responses to Two Different Cycling Sprint Interval Exercise Protocols with Different Recovery Durations
Abstract
:1. Introduction
2. Material and Methods
2.1. Participants
2.2. Study Design
2.3. Incremental Exercise Test (IXT)
2.4. Benchmark Test (PPO10)
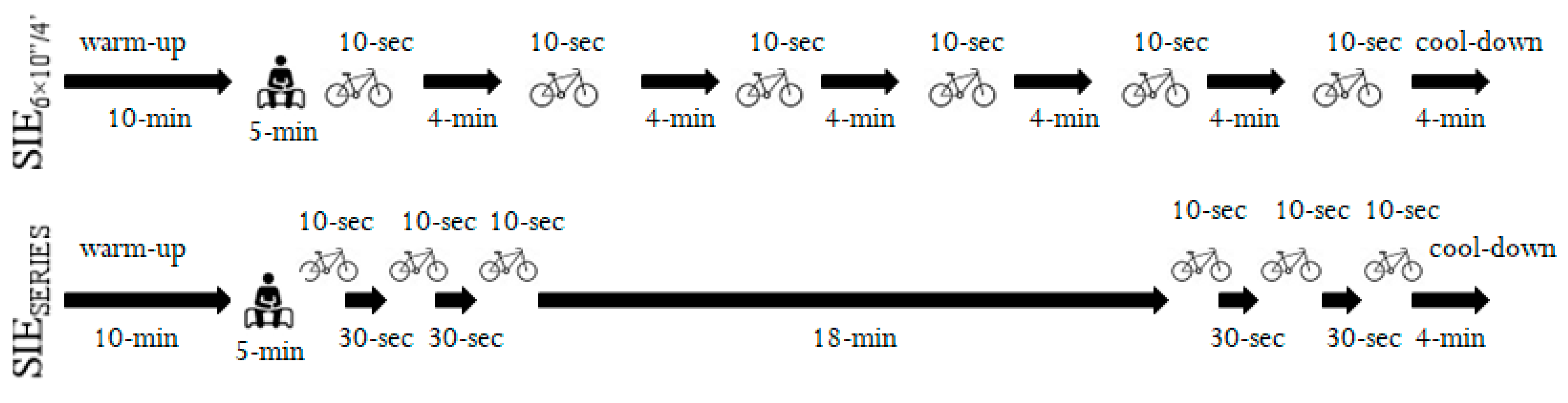
2.5. Sprint Interval Exercise (SIE) Protocols
2.6. Blood Lactate Concentrations
2.7. Rating of Perceived Exertion
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Batacan, R.B.; Duncan, M.J.; Dalbo, V.J.; Tucker, P.S.; Fenning, A.S. Effects of high-intensity interval training on cardiometabolic health: A systematic review and meta-analysis of intervention studies. Br. J. Sports Med. 2017, 51, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Gibala, M.J.; Hawley, J.A. Sprinting toward fitness. Cell Metab. 2017, 25, 988–990. [Google Scholar] [CrossRef] [PubMed]
- Vollaard, N.B.; Metcalfe, R.S. Research into the health benefits of sprint interval training should focus on protocols with fewer and shorter sprints. Sports Med. 2017, 47, 2443–2451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gist, N.H.; Fedewa, M.V.; Dishman, R.K.; Cureton, K.J. Sprint interval training effects on aerobic capacity: A systematic review and meta-analysis. Sports Med. 2014, 44, 269–279. [Google Scholar] [CrossRef] [PubMed]
- Buchheit, M.; Laursen, P.B. High-intensity interval training, solutions to the programming puzzle. Sports Med. 2013, 43, 927–954. [Google Scholar] [CrossRef]
- Hazell, T.J.; MacPherson, R.E.; Gravelle, B.M.; Lemon, P.W. 10 or 30-s sprint interval training bouts enhance both aerobic and anaerobic performance. Eur. J. Appl. Physiol. 2010, 110, 153–160. [Google Scholar] [CrossRef]
- Olek, R.A.; Kujach, S.; Ziemann, E.; Ziolkowski, W.; Waz, P.; Laskowski, R. Adaptive Changes After 2 Weeks of 10-s Sprint Interval Training with Various Recovery Times. Front. Physiol. 2018, 9, 392. [Google Scholar] [CrossRef] [Green Version]
- Kavaliauskas, M.; Aspe, R.R.; Babraj, J. High-intensity cycling training: The effect of work-to-rest intervals on running performance measures. J. Strength Cond. Res. 2015, 29, 2229–2236. [Google Scholar] [CrossRef] [Green Version]
- Zierath, J.R.; Wallberg-Henriksson, H. Looking Ahead Perspective: Where Will the Future of Exercise Biology Take Us? Cell Metab. 2015, 22, 25–30. [Google Scholar] [CrossRef] [Green Version]
- Tomlin, D.L.; Wenger, H.A. The relationship between aerobic fitness and recovery from high intensity intermittent exercise. Sports Med. 2001, 31, 1–11. [Google Scholar] [CrossRef]
- Islam, H.; Townsend, L.K.; Hazell, T.J. Modified sprint interval training protocols. Part I. Physiological responses. Appl. Physiol. Nutr. Metab. 2016, 42, 339–346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benítez-Flores, S.; de Sousa, A.F.; da Cunha Totó, E.C.; Santos Rosa, T.; Del Rosso, S.; Foster, C.; Boullosa, D. Shorter sprints elicit greater cardiorespiratory and mechanical responses with less fatigue during time-matched sprint interval training (SIT) sessions. J. Electromyogr. Kinesiol. 2018, 50, 137–148. [Google Scholar] [CrossRef]
- Freese, E.C.; Gist, N.H.; Cureton, K.J. Physiological responses to an acute bout of sprint interval cycling. J. Strength Cond. Res. 2013, 27, 2768–2773. [Google Scholar] [CrossRef] [PubMed]
- Malta, E.S.; Brisola, G.M.; Dutra, Y.M.; Franchini, E.; Zagatto, A.M. Metabolic Profile and Performance Responses During Two Consecutive Sessions of Sprint Interval Training. J. Strength Cond. Res. 2018, 1, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Townsend, L.K.; Islam, H.; Dunn, E.; Eys, M.; Robertson-Wilson, J.; Hazell, T.J. Modified sprint interval training protocols. Part II. Psychological responses. Appl. Physiol. Nutr. Metab. 2017, 42, 347–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, Q.; Tong, T.K.; Sun, S.; Kong, Z.; Chan, C.K.; Liu, W.; Nie, J. Influence of recovery duration during 6-s sprint interval exercise on time spent at high rates of oxygen uptake. J. Exerc. Sci. Fit. 2018, 16, 16–20. [Google Scholar] [CrossRef]
- Hebisz, P.; Hebisz, R.; Zatoń, M.; Borkowski, J. Dynamics of changes in power output, heart rate, and disorders of acid-base balance during interval training in mountain cyclists. Isokinet. Exerc. Sci. 2015, 23, 245–252. [Google Scholar] [CrossRef]
- Hebisz, R.; Hebisz, P.; Zatoń, M.; Michalik, K. Peak oxygen uptake in a sprint interval testing protocol vs. maximal oxygen uptake in an incremental testing protocol and their relationship with cross-country mountain biking performance. Appl. Physiol. Nutr. Metab. 2017, 42, 371–376. [Google Scholar] [CrossRef]
- Michalik, K.; Danek, N.; Zatoń, M. Assessment of the physical fitness of road cyclists in the step and ramp protocols of the incremental test. J. Sports Med. Phys. Fit. 2019, 59, 1285–1291. [Google Scholar] [CrossRef]
- Bar-Or, O. The Wingate anaerobic test an update on methodology, reliability and validity. J. Sports Med. 1987, 4, 381–394. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; LEA: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Vollaard, N.; Metcalfe, R.; Williams, S. Effect of number of sprints in a SIT session on change in VO2max: A meta-analysis. Med. Sci. Sports Exerc. 2017, 49, 1147–1156. [Google Scholar] [CrossRef] [PubMed]
- Hebisz, R.; Hebisz, P.; Borkowski, J.; Zatoń, M. Differences in physiological responses to interval training in cyclists with and without interval training experience. J. Hum. Kinet. 2016, 50, 93–101. [Google Scholar] [CrossRef]
- Bogdanis, G.C.; Nevill, M.E.; Lakomy, H.K.A.; Boobis, L.H. Power output and muscle metabolism during and following recovery from 10 and 20 s of maximal sprint exercise in humans. Acta Physiol. Scand. 1998, 163, 261–272. [Google Scholar] [CrossRef]
- Mendez-Villanueva, A.; Hamer, P.; Bishop, D. Fatigue inrepeated-sprint exercise is related to muscle powerfactors and reduced neuromuscular activity. Eur. J. Appl. Physiol. 2008, 9, 103–411. [Google Scholar]
- McCartney, N.; Spriet, L.L.; Heigenhauser, G.J.; Kowalchuk, J.M.; Sutton, J.R.; Jones, N.L. Muscle power and metabolism in maximal intermittent exercise. J. Appl. Physiol. 1986, 60, 1164–1169. [Google Scholar] [CrossRef]
- Spriet, L.L.; Lindinger, M.I.; McKelvie, R.S.; Heigenhauser, G.J.; Jones, N.L. Muscle glycogenolysis and H+ concentration during maximal intermittent cycling. J. Appl. Physiol. 1989, 66, 8–13. [Google Scholar] [CrossRef]
- Harms, C.A.; Babcock, M.A.; McClaran, S.R.; Pegelow, D.F.; Nickele, G.A.; Nelson, W.B.; Dempsey, J.A. Respiratory muscle work compromises leg blood flow during maximal exercise. J. Appl. Physiol. 1997, 82, 1573–1583. [Google Scholar] [CrossRef] [Green Version]
- Astrand, I.; Astrand, P.O.; Christensen, E.H.; Hedman, R. Myohemoglobin as an oxygen-store in man. Acta Physiol. Scand. 1960, 60, 48–454. [Google Scholar] [CrossRef]
- Hazell, T.J.; Olver, T.D.; Macpherson, R.E.; Hamilton, C.D.; Lemon, P.W. Sprint interval exercise elicits near maximal peak VO2 during repeated bouts with a rapid recovery within 2 minutes. J. Sports Med. Phys. Fit. 2014, 54, 750–756. [Google Scholar]
- Iaia, F.M.; Fiorenza, M.; Larghi, L.; Alberti, G.; Millet, G.P.; Girard, O. Short-or long-rest intervals during repeated-sprint training in soccer? PLoS ONE 2017, 12, e0171462. [Google Scholar] [CrossRef] [PubMed]
- Little, T.; Williams, A.G. Effects of sprint duration and exercise: Rest ratio on repeated sprint performance and physiological responses in professional soccer players. J. Strength Cond. Res. 2007, 21, 646–648. [Google Scholar] [CrossRef] [PubMed]
- Gaesser, G.A.; Poole, D.C. The slow component of oxygen uptakekinetics in humans. Exerc. Sport Sci. Rev. 1996, 24, 35–71. [Google Scholar] [CrossRef] [PubMed]
- Gibson, A.S.C.; Noakes, T.D. Evidence for complex system integration and dynamic neural regulation of skeletal muscle recruitment during exercise in humans. Br. J. Sports Med. 2004, 38, 797–806. [Google Scholar] [CrossRef]
- Gist, N.H.; Freese, E.C.; Cureton, K.J. Comparison of responses to two high-intensity intermittent exercise protocols. J. Strength Cond. Res. 2014, 28, 3033–3040. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P.; Med, A.C.S. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Gibala, M. Molecular responses to high-intensity interval exercise. Appl. Physiol. Nutr. Metab. 2009, 34, 428–432. [Google Scholar] [CrossRef]
- Metcalfe, R.S.; Koumanov, F.; Ruffino, J.S.; Stokes, K.A.; Holman, G.D.; Thompson, D.; Vollaard, N.B.J. Physiological and molecular responses to an acute bout of reduced-exertion high-intensity interval training (REHIT). Eur. J. Appl. Physiol. 2015, 115, 2321–2334. [Google Scholar] [CrossRef] [Green Version]
- Magder, S.A. The ups and downs of heart rate. Crit. Care Med. 2012, 40, 239–245. [Google Scholar] [CrossRef]
- Hebisz, P.; Hebisz, R.; Bakońska-Pacoń, E.; Zatoń, M. Acute hematological response to a single dose of sprint interval training in competitive cyclists. Sci. Sports 2017, 32, 369–375. [Google Scholar] [CrossRef]
- Tucker, R. The anticipatory regulation of performance: The physiological basis for pacing strategies and the development of a perception-based model for exercise performance. Br. J. Sports Med. 2009, 43, 392–400. [Google Scholar] [CrossRef] [PubMed]
- Bouchard, C.; An, P.; Rice, T.; Skinner, J.S.; Wilmore, J.H.; Gagnon, J. Familial aggregation of VO2max response to exercise training: Results from the HERITAGE Family Study. J. Appl. Physiol. 1997, 87, 1003–1008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bentley, D.J.; Wilson, G.J.; Davie, A.J.; Zhou, S. Correlations between peak power output, muscular strength and cycle time trial performance in triathletes. J. Sports Med. Phys. Fit. 1998, 38, 201–207. [Google Scholar]
- Thompson, W.R. Worldwide survey of fitness trends for 2018: The CREP edition. ACSMs Health Fit. J. 2017, 21, 10–19. [Google Scholar] [CrossRef]


| Variables | Values |
|---|---|
| Age (years) | 24.9 ± 4.1 |
| Body height (cm) | 181.3 ± 7.7 |
| Body mass (kg) | 77.8 ± 10.6 |
| Physical activity (h per week) | 7.7 ± 1.6 |
| Systolic blood pressure (mmHg) | 123 ± 10 |
| Diastolic blood pressure (mmHg) | 70 ± 8 |
| MAP (W) | 341.0 ± 41.4 |
| VEmax (L·min−1) | 148.7 ± 21.1 |
| VO2max (mL·kg−1·min−1) | 52.4 ± 7.8 |
| HRmax (b·min−1) | 193 ± 7 |
| [La−] (mmol·L−1) | 12.8 ± 1.8 |
| SIE6×10”/4’ | SIESERIES | SIESERIES | ||
|---|---|---|---|---|
| SERIES I | SERIES II | |||
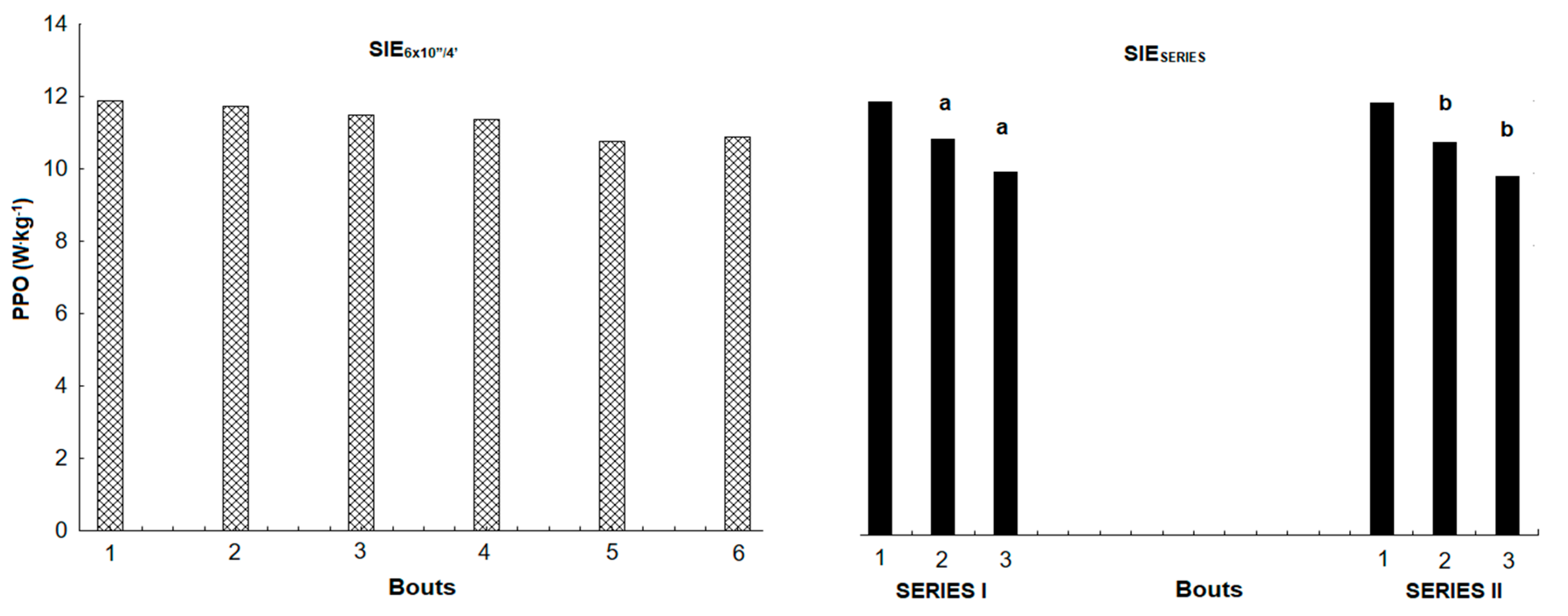
| PPO (W) | 935.7 ± 161.7 | 944.5 ± 161.1 | 936.5 ± 166.0 | 931.6 ± 149.1 |
| PPO (W·kg−1) | 12.0 ± 0.9 | 12.0 ± 0.8 | 12.1 ± 0.8 | 12.0 ± 0.9 |
| MPO (W) | 771.7 ± 139.3 | 748.2 ± 123.3 * | 754.8 ± 128.3 | 741.5 ± 118.6 # |
| MPO (W·kg−1) | 9.9 ± 1.0 | 9.6 ± 0.6 * | 9.7 ± 0.7 | 9.5 ± 0.6 # |
| TW (kJ) | 46.3 ± 8.4 | 44.9 ± 7.4 * | 22.6 ± 3.8 | 22.3 ± 3.6 # |
| TW (J·kg−1) | 593.0 ± 57.5 | 575.9 ± 38.6 * | 290.3 ± 19.6 | 285.6 ± 19.3 # |
| FI (%) | 11.9 ± 8.0 | x | 15.9 ± 3.9 | 16.7 ± 5.3 |
| SIE6×10”/4’ | SIESERIES | SIESERIES | ||
|---|---|---|---|---|
| SERIES I | SERIES II | |||
| VEpeak (L∙min−1) | 118.2 ± 18.9 | 141.7 ± 18.5 * | 137.0 ± 17.7 | 138.7 ± 19.9 |
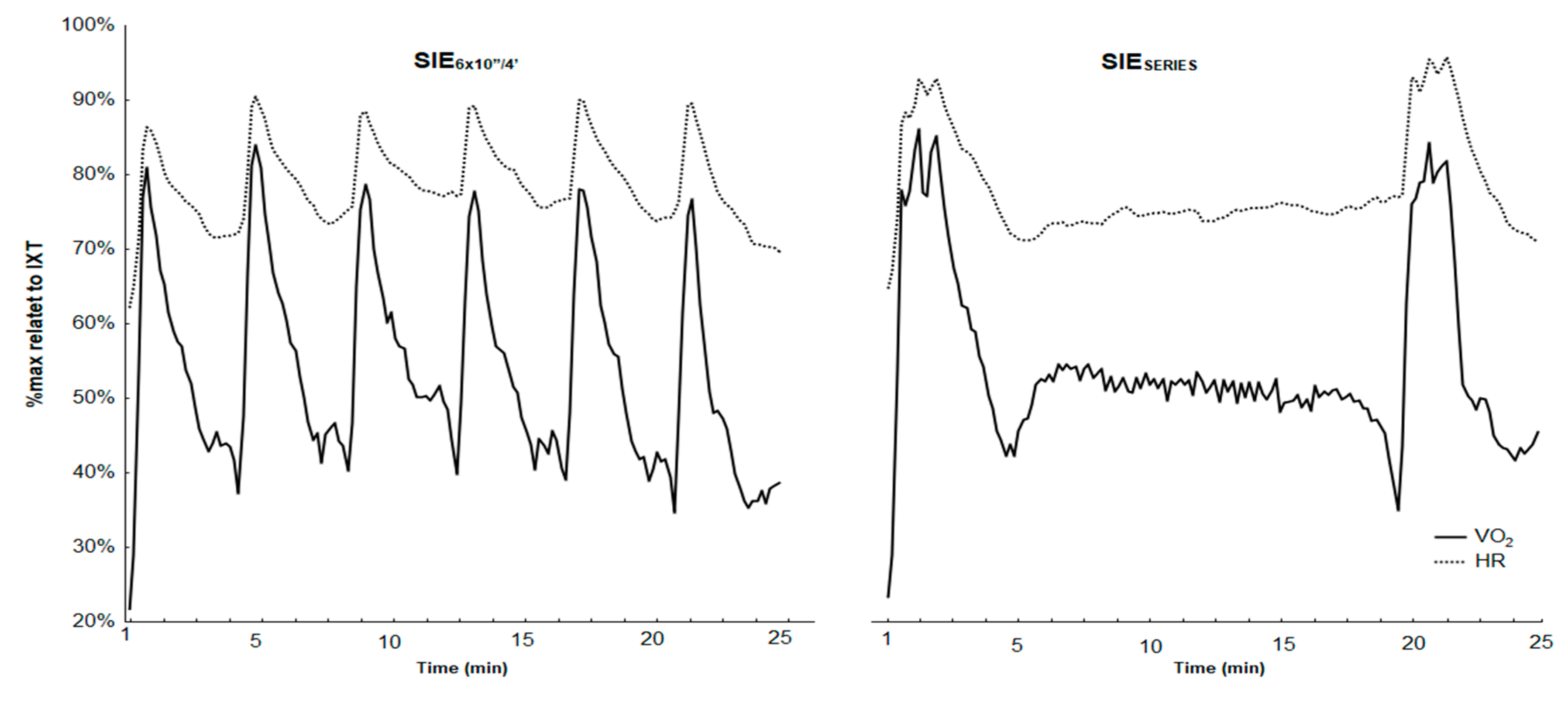
| VO2peak (mL∙kg−1∙min−1) | 43.0 ± 4.6 | 45.0 ± 4.7 * | 44.5 ± 4.5 | 44.3 ± 3.8 |
| VO2mean (mL∙kg−1∙min−1) | 28.2 ± 2.5 | 28.6 ± 2.3 | 38.7 ± 3.8 | 39.3 ± 3.5 |
| HRpeak (beats·min−1) | 178 ± 8.0 | 184 ± 7 * | 180 ± 6 | 184 ± 7 |
| HRmean (beats·min−1) | 154 ± 10 | 151 ± 11 | 170 ± 8 | 177 ± 9 # |
| [La−]peak (mmol·L−1) | 13.9 ± 1.8 | 13.4 ± 2.3 | 11.8 ± 1.0 | 13.3 ± 2.3 |
| RPEmean (6–20) | 15.2 ± 0.9 | 15.9 ± 1.4 | 15.6 ± 2.0 | 16.6 ± 1.2 # |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Danek, N.; Smolarek, M.; Michalik, K.; Zatoń, M. Comparison of Acute Responses to Two Different Cycling Sprint Interval Exercise Protocols with Different Recovery Durations. Int. J. Environ. Res. Public Health 2020, 17, 1026. https://doi.org/10.3390/ijerph17031026
Danek N, Smolarek M, Michalik K, Zatoń M. Comparison of Acute Responses to Two Different Cycling Sprint Interval Exercise Protocols with Different Recovery Durations. International Journal of Environmental Research and Public Health. 2020; 17(3):1026. https://doi.org/10.3390/ijerph17031026
Chicago/Turabian StyleDanek, Natalia, Marcin Smolarek, Kamil Michalik, and Marek Zatoń. 2020. "Comparison of Acute Responses to Two Different Cycling Sprint Interval Exercise Protocols with Different Recovery Durations" International Journal of Environmental Research and Public Health 17, no. 3: 1026. https://doi.org/10.3390/ijerph17031026
APA StyleDanek, N., Smolarek, M., Michalik, K., & Zatoń, M. (2020). Comparison of Acute Responses to Two Different Cycling Sprint Interval Exercise Protocols with Different Recovery Durations. International Journal of Environmental Research and Public Health, 17(3), 1026. https://doi.org/10.3390/ijerph17031026







