The Association of Knowledge, Attitudes and Access with Park Use before and after a Park-Prescription Intervention for Low-Income Families in the U.S.
Abstract
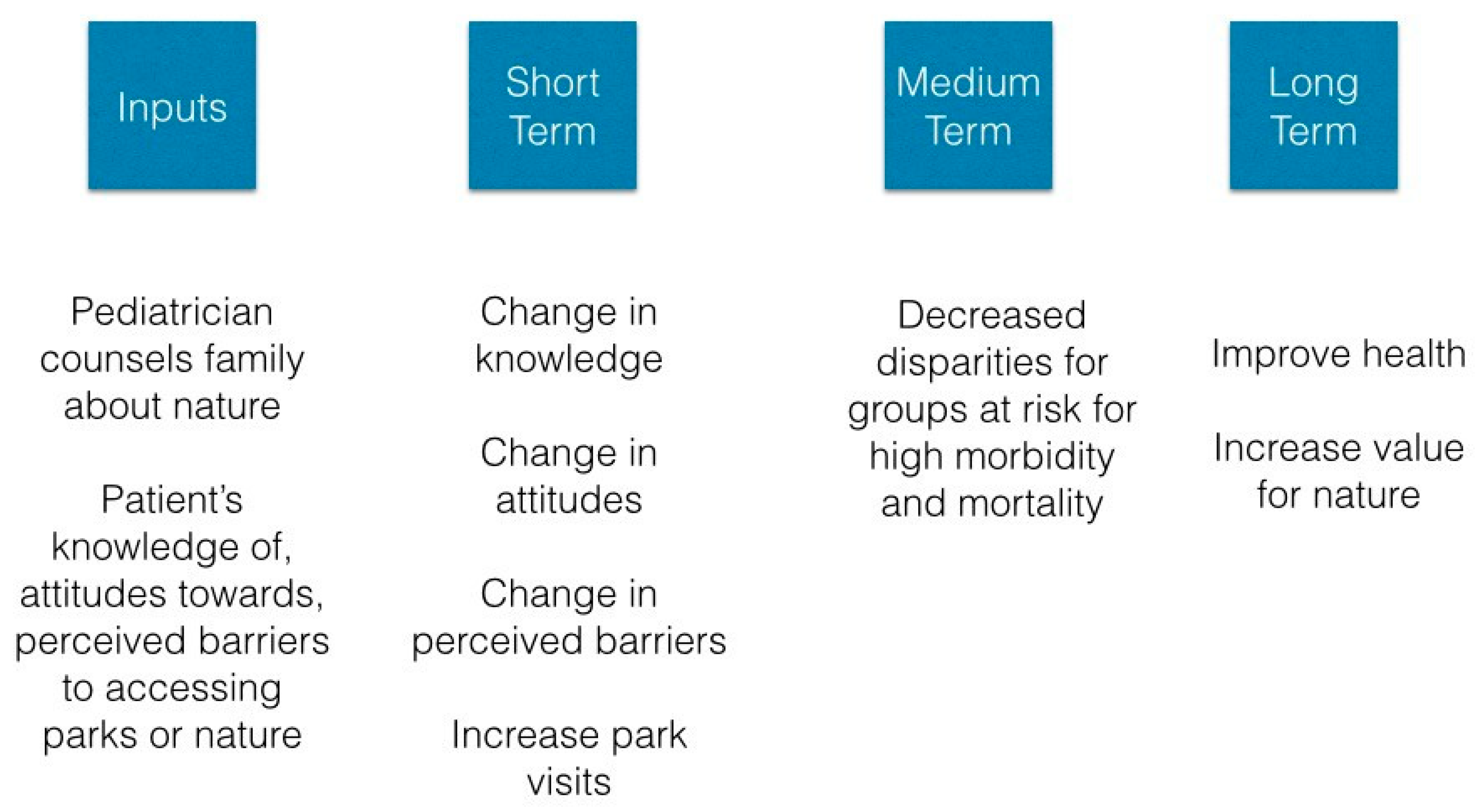
:1. Introduction
2. Materials and Methods
2.1. Outcomes
2.2. Predictors
2.3. Statistical Analysis
3. Results
3.1. Baseline Findings
3.2. How Were Baseline Demographics, Knowledge, Attitudes and Barriers Associated with Park Use at Baseline?
3.3. How Are Demographics, Knowledge, Attitudes and Barriers to Access Associated with Park Use as They Changed over Time after a Park Prescription?
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Maller, C.; Townsend, M.; Pryor, A.; Brown, P.; Leger, L.S. Healthy nature healthy people: ‘Contact with nature’ as an upstream health promotion intervention for populations. Health Promot. Int. 2006, 21, 45–54. [Google Scholar] [CrossRef] [Green Version]
- Swinburn, B.A.; Walter, L.G.; Arroll, B.; Tilyard, M.W.; Russell, D.G. The green prescription study: A randomized controlled trial of written exercise advice provided by general practitioners. Am. J. Public Health 1998, 88, 288–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andrews, M.; Sawyer, C.; Frerichs, L.; Asheley, C.S.; Hoffman, J.; Gaskin, K.; Armstrong, S. Feasibility of a clinic-community partnership to treat childhood obesity. Clin. Pediatr. 2018, 57, 783–791. [Google Scholar] [CrossRef]
- Uijtdewilligen, L.; Waters, C.N.; Aw, S.; Wong, M.L.; Sia, A.; Ramiah, A.; Wong, M.; Müller-Riemenschneider, F. The park prescription study: Development of a community-based physical activity intervention for a multi-ethnic Asian population. PLoS ONE 2019, 14, e0218247. [Google Scholar] [CrossRef] [Green Version]
- Zarr, R.; Cottrell, L.; Merrill, C. Park prescription (DC Park Rx): A new strategy to combat chronic disease in children. J. Phys. Act. Health 2017, 14, 1–2. [Google Scholar] [CrossRef]
- Messiah, S.E.; Jiang, S.; Kardys, J.; Hansen, E.; Nardi, M.; Forster, L. Reducing childhood obesity through coordinated care: Development of a park prescription program. World J. Clin. Pediatr. 2016, 5, 234–243. [Google Scholar] [CrossRef]
- Razani, N.; Kohn, M.A.; Wells, N.M.; Thompson, D.; Hamilton Flores, H.; Rutherford, G.W. Design and evaluation of a park prescription program for stress reduction and health promotion in low-income families: The stay healthy in nature everyday (SHINE) study protocol. Contemp. Clin. Trials 2016, 51, 8–14. [Google Scholar] [CrossRef]
- Seltenrich, N. Just what the doctor ordered: Using parks to improve children’s health. Environ. Health Perspect. 2015, 123, A254–A259. [Google Scholar] [CrossRef] [Green Version]
- Coffey, J.S.; Gauderer, L. When pediatric primary care providers prescribe nature engagement at a State Park, do children “fill” the prescription? Ecopsychology 2016, 8, 207–214. [Google Scholar] [CrossRef] [Green Version]
- Hoffman, J.; Frerichs, L.; Story, M.; Jones, J.; Gaskin, K.; Apple, A.; Skinner, A.; Armstrong, S. An Integrated clinic-community partnership for child obesity treatment: A randomized pilot trial. Pediatrics 2018, 141, e20171444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Razani, N.; Niknam, K.; Wells, N.M.; Thompson, D.; Hills, N.K.; Kennedy, G.; Gilgoff, R.; Rutherford, G.W. Clinic and park partnerships for childhood resilience: A prospective study of park prescriptions. Health Place 2019, 57, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Razani, N.; Morshed, S.; Kohn, M.A.; Wells, N.M.; Thompson, D.; Alqassari, M.; Agodi, A.; Rutherford, G.W. Effect of park prescriptions with and without group visits to parks on stress reduction in low-income parents: SHINE randomized trial. PLoS ONE 2018, 13, e0192921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, K.S.T.; Sia, A.; Ng, M.K.W.; Tan, C.T.Y.; Chan, H.Y.; Tan, C.H.; Rawtaer, I.; Feng, L.; Mahendran, R.; Larbi, A.; et al. Effects of horticultural therapy on Asian older adults: A randomized controlled trial—Clinical Trial. Int. J. Environ. Res. Public Health 2018, 15, 1705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolch, J.; Jerrett, M.; Reynolds, K.; McConnell, R.; Chang, R.; Dahmann, N.; Brady, K.; Gilliland, F.; Su, J.G.; Berhane, K. Childhood obesity and proximity to urban parks and recreational resources: A longitudinal cohort study. Health Place 2011, 17, 207–214. [Google Scholar] [CrossRef] [Green Version]
- Goldsby, T.U.; George, B.J.; Yeager, V.A.; Sen, B.P.; Ferdinand, A.; Sims, D.M.; Manzella, B.; Cockrell Skinner, A.; Allison, D.B.; Menachemi, N. Urban park development and pediatric obesity rates: A quasi-experiment using electronic health record data. Int. J. Environ. Res. Public Health 2016, 13, 411. [Google Scholar] [CrossRef] [Green Version]
- Feng, X.; Astell-Burt, T. The Relationship between neighbourhood green space and child mental wellbeing depends upon whom you ask: Multilevel evidence from 3083 children aged 12–13 years. Int. J. Environ. Res. Public Health 2017, 14, 543. [Google Scholar] [CrossRef] [Green Version]
- Cohen, D.A.; Ashwood, J.S.; Scott, M.M.; Overton, A.; Evenson, K.R.; Staten, L.K.; Porter, D.; McKenzie, T.L.; Catellier, D. Public parks and physical activity among adolescent girls. Pediatrics 2006, 118, e1381-9. [Google Scholar] [CrossRef] [Green Version]
- Giles-Corti, B.; Broomhall, M.H.; Knuiman, M.; Collins, C.; Douglas, K.; Ng, K.; Lange, A.; Donovan, R.J. Increasing walking: How important is distance to, attractiveness, and size of public open space? Am. J. Prev. Med. 2005, 28, 169–176. [Google Scholar] [CrossRef]
- Hartig, T.; Mitchell, R.; de Vries, S.; Frumkin, H. Nature and health. Annu. Rev. Public Health 2014, 35, 207–228. [Google Scholar] [CrossRef] [Green Version]
- Dadvand, P.; Sunyer, J.; Basagaña, X.; Ballester, F.; Lertxundi, A.; Fernández-Somoano, A.; Estarlich, M.; García-Esteban, R.; Mendez, M.A.; Nieuwenhuijsen, M.J. Surrounding greenness and pregnancy outcomes in four Spanish birth cohorts. Environ. Health Perspect. 2012, 120, 1481–1487. [Google Scholar] [CrossRef]
- Mitchell, R.; Popham, F. Effect of exposure to natural environment on health inequalities: An observational population study. Lancet 2008, 372, 1655–1660. [Google Scholar] [CrossRef] [Green Version]
- Ulrich, R.S. View through a window may influence recovery from surgery. Science 1984, 224, 420. [Google Scholar] [CrossRef] [Green Version]
- Yu, J. Prefrontal cortical activation while viewing urban and garden scenes: A pilot fNIRS study. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Seogwipo, Korea, 11–15 July 2017; pp. 2546–2549. [Google Scholar]
- Van Dyck, D.; Sallis, J.F.; Cardon, G.; Deforche, B.; Adams, M.A.; Geremia, C.; De Bourdeaudhuij, I. Associations of neighborhood characteristics with active park use: An observational study in two cities in the USA and Belgium. Int. J. Health Geogr. 2013, 12, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, D.A.; Han, B.; Nagel, C.J.; Harnik, P.; McKenzie, T.L.; Evenson, K.R.; Marsh, T.; Williamson, S.; Vaughan, C.; Katta, S. The first national study of neighborhood parks: Implications for physical activity. Am. J. Prev. Med. 2016, 51, 419–426. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunton, G.F.; Almanza, E.; Jerrett, M.; Wolch, J.; Pentz, M.A. Neighborhood park use by children: Use of accelerometry and global positioning systems. Am. J. Prev. Med. 2014, 46, 136–142. [Google Scholar] [CrossRef] [Green Version]
- Casey, J.A.; James, P.; Cushing, L.; Jesdale, B.M.; Morello-Frosch, R. Race, ethnicity, income concentration and 10-year change in urban greenness in the United States. Int. J. Environ. Res. Public Health 2017, 14, 1546. [Google Scholar] [CrossRef] [Green Version]
- Wen, M.; Zhang, X.; Harris, C.D.; Holt, J.B.; Croft, J.B. Spatial disparities in the distribution of parks and green spaces in the USA. Ann. Behav. Med. 2013, 45, S18–S27. [Google Scholar] [CrossRef] [Green Version]
- Godbey, G.C.; Caldwell, L.L.; Floyd, M.; Payne, L.L. Contributions of leisure studies and recreation and park management research to the active living agenda. Am. J. Prev. Med. 2005, 28, 150–158. [Google Scholar] [CrossRef]
- Glanz, K.; Bishop, D.B. The role of behavioral science theory in development and implementation of public health interventions. Annu. Rev. Public Health 2010, 31, 399–418. [Google Scholar] [CrossRef] [Green Version]
- Groshong, L.; Stanis, S.A.; Kaczynski, A.T.; Hipp, J.A.; Besenyi, G.M. Exploring attitudes, perceived norms, and personal agency: Insights into theory-based messages to encourage park-based physical activity in low-income urban neighborhoods. J. Phys. Act. Health 2017, 14, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Wen, F.; Golinelli, D.; Rodriguez, D.A.; Cohen, D.A. Measurement properties of a park use questionnaire. Environ. Behav. 2013, 45, 526–547. [Google Scholar] [CrossRef] [PubMed]
- Bedimo-Rung, A.L.; Mowen, A.J.; Cohen, D.A. The significance of parks to physical activity and public health: A conceptual model. Am. J. Prev. Med. 2005, 28, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Parks. Available online: https://www.tpl.org/parks (accessed on 27 December 2019).
- U.S. Federal Poverty Guidelines Used to Determine Financial Eligibility for Certain Federal Programs. Available online: https://aspe.hhs.gov/poverty-guidelines (accessed on 23 October 2019).
- Perkins, H.E. Measuring love and care for nature. J. Environ. Psychol. 2010, 30, 455–463. [Google Scholar] [CrossRef] [Green Version]
- Shores, K.; Scott, D.; Floyd, M. Constraints to outdoor recreation: A multiple hierarchy stratification perspective. Leis. Sci. 2007, 29, 227–246. [Google Scholar] [CrossRef]
- Floyd, M.F.; Crespo, C.J.; Sallis, J.F. Active living research in diverse and disadvantaged communities. Am. J. Prev. Med. 2008, 34, 271–274. [Google Scholar] [CrossRef] [PubMed]
- Zeger, S.L.; Liang, K.Y.; Albert, P.S. Models for longitudinal data: A generalized estimating equation approach. Biometrics 1988, 44, 1049–1060. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Department of Housing Authority and Development. Median Family Income Documentation System 2015. Available online: https://www.huduser.gov/portal/datasets/il/il2019/2019MedCalc.odn (accessed on 24 October 2019).
- Weiss, C.C.; Purciel, M.; Bader, M.; Quinn, J.W.; Lovasi, G.; Neckerman, K.M.; Rundle, A.G. Reconsidering access: Park facilities and neighborhood disamenities in New York City. Urban Health 2011, 88, 297–310. [Google Scholar] [CrossRef] [Green Version]
- Yoshino, A.; Wilson, J.; Velazquez, E.J.; Johnson, E.; Márquez-Magaña, L. Healthy parks healthy people as an upstream stress reduction strategy. Recreat. Park Tour Public Health 2018, 2, 35–56. [Google Scholar] [CrossRef]
- Wells, N.M.; Lekies, K.S. Nature and the life course: Pathways from childhood nature experiences to adult environmentalism. Chil. Youth Environ. 2006, 16, 1–24. [Google Scholar]
- Edwards, N.; Hooper, P.; Knuiman, M.; Foster, S.; Giles-Corti, B. Associations between park features and adolescent park use for physical activity. Int. J. Behav. Nutr. Phys. Act. 2015, 12. [Google Scholar] [CrossRef] [Green Version]
- Vaughan, C.A.; Colabianchi, N.; Hunter, G.P.; Beckman, R.; Dubowitz, T. Park use in low-income urban neighborhoods: Who uses the parks and why? Urban Health 2018, 95, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Greer, A.E.; Castrogivanni, B.; Marcello, R. Park use and physical activity among mostly low-to-middle income, minority parents and their children. J. Phys. Act. Health 2017, 14, 83–87. [Google Scholar] [CrossRef]
- Twenge, J.M.; Campbell, W.K. Associations between screen time and lower psychological well-being among children and adolescents: Evidence from a population-based study. Prev. Med. Rep. 2018, 12, 271–283. [Google Scholar] [CrossRef] [PubMed]
- Derose, K.P.; Han, B.; Williamson, S.; Cohen, D.A. Gender disparities in park use and physical activity among residents of high-poverty neighborhoods in Los Angeles. Women’s Health Issues 2018, 28, 6–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Das, K.V.; Fan, Y.; French, S.A. Park-use behavior and perceptions by race, hispanic origin, and immigrant status in Minneapolis, MN: Implications on park strategies for addressing health disparities. J. Immigr. Minor Health 2017, 19, 318–327. [Google Scholar] [CrossRef]
- Floyd, M.F. Race, Ethnicity and Use of the National Parks System. Soc. Sci. Res. Rev. 1999, 1, 1–22. [Google Scholar]
- Roberts, N.S.; Chitewere, T. Speaking of justice: Exploring ethnic minority perspectives of the Golden Gate National recreation area. Environ. Pract. 2017, 13, 354–369. [Google Scholar] [CrossRef]
- Fan, Y.; French, S.A.; Das, K.V. Family structure and park use among parents. Am. J. Prev. Med. 2012, 43, 520–526. [Google Scholar] [CrossRef]
- Lin, B.B.; Fuller, R.A.; Bush, R.; Gaston, K.J.; Shanahan, D.F. Opportunity or orientation? Who uses urban parks and why. PLoS ONE 2014, 9, e87422. [Google Scholar] [CrossRef] [Green Version]
- Piccininni, C.; Michaelson, V.; Janssen, I.; Pickett, W. Outdoor play and nature connectedness as potential correlates of internalized mental health symptoms among Canadian adolescents. Prev. Med. 2018, 112, 168–175. [Google Scholar] [CrossRef]
- Cleland, V.; Timperio, A.; Salmon, J.; Hume, C.; Baur, L.A.; Crawford, D. Predictors of time spent outdoors among children: 5-year longitudinal findings. J. Epidemiol. Community Health 2010, 64, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Remmers, T.; Broeren, S.M.; Renders, C.M.; Hirasing, R.A.; van Grieken, A.; Raat, H. A longitudinal study of children’s outside play using family environment and perceived physical environment as predictors. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Razani, N.; Stookey, J.; Brainin-Rodriguez, L.; Rutherford, G.W.; Chan, C. Surmounting barriers to public health/park agency partnerships: Insights from a county public health department. J. Park Recreat. Ad. 2016, 34, 53–67. [Google Scholar]

| Characteristic | Total (n = 78) | (%) a | No Park Visits in Prior Week (n = 29) | Any Park Visits in Prior Week (n = 49) | p-Value c | ||
|---|---|---|---|---|---|---|---|
| n | (%) b | n | (%) b | ||||
| Demographics | |||||||
| Child’s age (y), median (IQR) | 8 (4, 15) | 29 | 8.6 (3.1) | 49 | 8.9 (3.1) | 0.7487 | |
| Female child | 38 | (49) | 13 | (34) | 25 | (66) | 0.60 d |
| Caregiver’s age, mean (SD) | 73 | 38.5 (11) | 26 | 36.8 (11) | 47 | 39 (11) | 0.35 d |
| Female caregiver | 68 | (87) | 25 | (37) | 43 | (63) | 0.55 |
| Race/ethnicity of caregiver | 0.03 * | ||||||
| African American | 52 | (67) | 20 | (39) | 32 | (62) | |
| Non-Latino White | 8 | (10) | 0 | (0) | 8 | (100) | |
| Latino | 12 | (15) | 5 | (42) | 7 | (58) | |
| Other f | 5 | (6) | 4 | (80) | 1 | (20) | |
| Born in the US | 64 | (83) | 26 | (41) | 38 | (59) | 0.085 |
| % of the federal poverty level | 0.07 | ||||||
| <100% | 11 | (14) | 5 | (46) | 6 | (55) | |
| 100–199 | 42 | (54) | 18 | (43) | 24 | (57) | |
| 200–399 | 12 | (15) | 4 | (33) | 8 | (67) | |
| 400% or more | 9 | (12) | 0 | (0) | 9 | (100) | |
| Knowledge | |||||||
| I know park locations | 41 | (53) | 9 | (22) | 32 | (78) | 0.01 * |
| Attitudes | |||||||
| Nature affinity, median (IQR) | 4.1 | (3.5, 4.7) | 3.8 | (3.4, 4.2) | 4.1 | (3.9, 4.3) | 0.18 e |
| I value visiting parks | 63 | (81) | 19 | (30) | 44 | (70) | 0.007 * |
| Barriers to Access | |||||||
| There is a park in my neighborhood | 55 | (71) | 18 | (33) | 37 | (67) | 0.225 |
| I have access to nature in daily life | 53 | (68) | 19 | (36) | 34 | (64) | 0.715 |
| I feel welcome in parks | 65 | (83) | 25 | (39) | 40 | (62) | 0.88 |
| I feel safe in parks (one missing) | 59 | (76) | 20 | (34) | 39 | (66) | 0.44 |
| I have money to visit parks | 37 | (47) | 12 | (32) | 25 | (68) | 0.45 |
| I have transportation to visit parks | 51 | (65) | 19 | (37) | 32 | (63) | 1.00 |
| I have time to visit parks | 43 | (55) | 12 | (28) | 31 | (72) | 0.09 |
| My neighborhood is safe for my child to play outside | 39 | (50) | 9 | (23) | 30 | (77) | 0.01 * |
| Behaviors | |||||||
| I spend a lot of time in nature now | 17 | (22) | 0 | (0) | 17 | (100) | <0.001 |
| I spent a lot of time in nature as a child | 51 | (65) | 18 | (35) | 33 | (65) | 0.87 |
| Characteristic | Univariate Analysis | Multivariable Analysis | ||||
|---|---|---|---|---|---|---|
| Coeff | 95% CI | p-Value | Coeff | 95% CI | p-Value | |
| Change in knowledge and attitudes | ||||||
| Park in neighborhood | 0.26 | (0.03, 0.50) | 0.03 | |||
| Access to nature | 0.47 | (0.24, 0.71) | <0.001 | |||
| Value visiting parks | 0.53 | (0.22, 0.84) | 0.001 | |||
| Feel welcome in parks | 0.49 | (0.15, 0.82) | 0.005 | |||
| Feel safe in parks | 0.54 | (0.30, 0.78) | <0.001 | |||
| Know park locations | 0.53 | (0.30, 0.76) | <0.001 | 0.27 | (0.05, 0.50) | 0.016 |
| Have transportation to parks | 0.33 | (0.08, 0.58) | 0.01 | |||
| Have time to visit parks | 0.67 | (0.43, 0.90) | <0.001 | 0.48 | (0.28, 0.69) | <0.001 |
| Have money to visit parks | 0.43 | (0.19, 0.66) | <0.001 | 0.24 | (0.05, 0.42) | 0.013 |
| Change in nature affinity | 0.65 | (0.35, 0.94) | <0.001 | 0.34 | (0.09, 0.59) | 0.007 |
| Change in neighborhood safety | 0.35 | (0.02, 0.70) | 0.049 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Razani, N.; Hills, N.K.; Thompson, D.; Rutherford, G.W. The Association of Knowledge, Attitudes and Access with Park Use before and after a Park-Prescription Intervention for Low-Income Families in the U.S. Int. J. Environ. Res. Public Health 2020, 17, 701. https://doi.org/10.3390/ijerph17030701
Razani N, Hills NK, Thompson D, Rutherford GW. The Association of Knowledge, Attitudes and Access with Park Use before and after a Park-Prescription Intervention for Low-Income Families in the U.S. International Journal of Environmental Research and Public Health. 2020; 17(3):701. https://doi.org/10.3390/ijerph17030701
Chicago/Turabian StyleRazani, Nooshin, Nancy K. Hills, Doug Thompson, and George W. Rutherford. 2020. "The Association of Knowledge, Attitudes and Access with Park Use before and after a Park-Prescription Intervention for Low-Income Families in the U.S." International Journal of Environmental Research and Public Health 17, no. 3: 701. https://doi.org/10.3390/ijerph17030701
APA StyleRazani, N., Hills, N. K., Thompson, D., & Rutherford, G. W. (2020). The Association of Knowledge, Attitudes and Access with Park Use before and after a Park-Prescription Intervention for Low-Income Families in the U.S. International Journal of Environmental Research and Public Health, 17(3), 701. https://doi.org/10.3390/ijerph17030701




