The Effects of Dehydration on Metabolic and Neuromuscular Functionality during Cycling
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
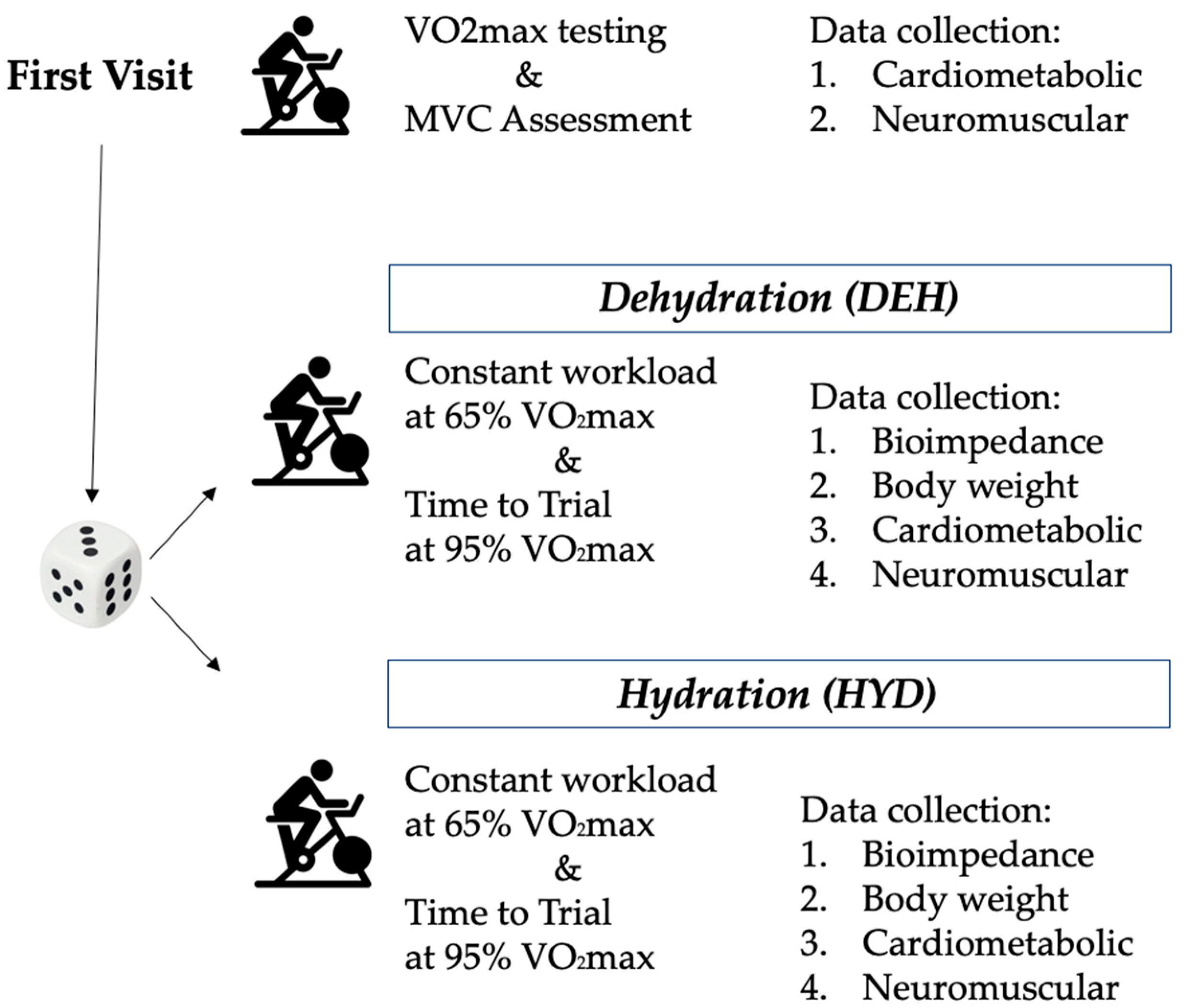
2.2. Procedures
2.3. Statistical Analysis
3. Results
3.1. Bioimpedance d-Data
3.2. Cardiometabolic Data
3.3. Neuromuscular Data
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Campa, F.; Semprini, G.; Júdice, P.B.; Messina, G.; Toselli, S. Anthropometry, Physical and Movement Features, and Repeated-sprint Ability in Soccer Players. Int. J. Sports Med. 2019, 40, 100–109. [Google Scholar] [CrossRef]
- Piras, A.; Cortesi, M.; Campa, F.; Perazzolo, M.; Gatta, G. Recovery Time Profiling After Short-, Middle- and Long-Distance Swimming Performance. J. Strength. Cond. Res. 2019, 33, 1408–1415. [Google Scholar] [CrossRef]
- Piras, A.; Gatta, G. Evaluation of the Effectiveness of Compression Garments on Autonomic Nervous System Recovery After Exercise. J. Strength Cond. Res. 2017, 31, 1636–1643. [Google Scholar] [CrossRef]
- Masento, N.A.; Golightly, M.; Field, D.T.; Butler, L.T.; van Reekum, C.M. Effects of Hydration Status on Cognitive Performance and Mood. Br. J. Nutr. 2014, 111, 1841–1852. [Google Scholar] [CrossRef] [PubMed]
- Pethick, W.A.; Murray, H.J.; McFadyen, P.; Brodie, R.; Gaul, C.A.; Stellingwerff, T. Effects of Hydration Status during Heat Acclimation on Plasma Volume and Performance. Scand. J. Med. Sci. Sports 2019, 29, 189–199. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Du, S.M.; Zhang, J.F.; Ma, G.S. Effects of Dehydration and Rehydration on Cognitive Performance and Mood among Male College Students in Cangzhou, China: A Self-Controlled Trial. Int. J. Environ. Res. Public Health 2019, 6, 1891. [Google Scholar] [CrossRef]
- Barley, O.R.; Chapman, D.W.; Blazevich, A.J.; Abbiss, C.R. Acute Dehydration Impairs Endurance Without Modulating Neuromuscular Function. Front Physiol. 2018, 9, 1562. [Google Scholar] [CrossRef] [PubMed]
- Castro-Sepulveda, M.; Cerda-Kohler, H.; Perez-Luco, C.; Monsalves, M.; Andrade, D.C.; Zbinden-Foncea, H.; Báez-San Martín, E.; Ramírez-Campillo, R. Hydration Status after Exercise Affect Resting Metabolic Rate and Heart Rate Variability. Nutr. Hosp. 2014, 31, 1273–1277. [Google Scholar]
- Georgescu, V.P.; de Souza Junior, T.P.; Behrens, C.; Barros, M.P.; Bueno, C.A.; Utter, A.C.; McAnulty, L.S.; McAnulty, S.R. Effect of Exercise-Induced Dehydration on Circulatory Markers of Oxidative Damage and Antioxidant Capacity. Appl. Physiol. Nutr. Metab. 2017, 42, 694–699. [Google Scholar] [CrossRef]
- Nuccio, R.P.; Barnes, K.A.; Carter, J.M.; Baker, L.B. Fluid Balance in Team Sport Athletes and the Effect of Hypohydration on Cognitive, Technical, and Physical Performance. Sports Med. 2017, 47, 1951–1982. [Google Scholar] [CrossRef]
- McDermott, B.P.; Anderson, S.A.; Armstrong, L.; Casa, D.G.; Cheuvront, S.N.; Cooper, L.; Kenney, W.L.; O’Connor, F.G.; Roberts, W.O. National Athletic Trainers’ Association Position Statement: Fluid Replacement for the Physically Active. J. Athl. Train. 2017, 2017 52, 877–895. [Google Scholar] [CrossRef]
- Logan-Sprenger, H.M.; Heigenhauser, G.F.; Jones, G.L.; Spriet, L.L. The Effect of Dehydration on Muscle Metabolism and Time Trial Performance during Prolonged Cycling in Males. Physiol. Rep. 2015, 3, e12483. [Google Scholar] [CrossRef] [PubMed]
- Campa, F.; Silva, A.M.; Iannuzzi, V.; Mascherini, G.; Benedetti, L.; Toselli, S. The role of somatic maturation on bioimpedance patterns and body composition in male elite youth soccer players. Int. J. Environ. Res. Public Health 2019, 16, 4711. [Google Scholar] [CrossRef] [PubMed]
- Campa, F.; Silva, A.M.; Toselli, S. Changes in Phase Angle and Handgrip Strength Induced by Suspension Training in Older Women. Int. J. Sports Med. 2018, 39, 442–449. [Google Scholar] [CrossRef]
- Campa, F.; Toselli, S. Bioimpedance Vector Analysis of Elite, Subelite, and Low-Level Male Volleyball Players. Int. J. Sports Physiol. Perform. 2018, 13, 1250–1253. [Google Scholar] [CrossRef]
- Gatterer, H.; Schenk, K.; Laninschegg, L.; Lukaski, H.; Burtscher, M. Bioimpedance Identifies Body Fluid Loss after Exercise in the Heat: A Pilot Study with Body Cooling. PLoS ONE 2014, 9, e109729. [Google Scholar] [CrossRef]
- Piccoli, A.; Rossi, B.; Pillon, L.; Bucciante, G. A New Method for Monitoring Body Fluid Variation by Bioimpedance Analysis: The RXc Graph. Kidney Int. 1994, 46, 534–539. [Google Scholar] [CrossRef]
- Campa, F.; Matias, C.N.; Marini, E.; Heymsfield, S.B.; Toselli, S.; Sardinha, L.B.; Silva, A.M. Identifying Athlete Body-Fluid Changes During a Competitive Season With Bioelectrical Impedance Vector Analysis. Int. J. Sports Physiol. Perform. 2019. [Google Scholar] [CrossRef]
- Marini, E.; Campa, F.; Buffa, R.; Stagi, S.; Matias, C.N.; Toselli, S.; Sardinha, L.B.; Silva, A.M. Phase angle and bioelectrical impedance vector analysis in the evaluation of body composition in athletes. Clin. Nutr. 2020, 39, 447–454. [Google Scholar] [CrossRef]
- Lukaski, H.C.; Piccoli, A. Bioelectrical impedance vector analysis for assessment of hydration in physiological states and clinical conditions. In Handbook of Anthropometry; Preedy, V., Ed.; Springer: Berlin, Germany, 2012; pp. 287–305. [Google Scholar]
- Muth, T.; Pritchett, R.; Pritchett, K.; Depaepe, J.; Blank, R. Hydration Status and Perception of Fluid Loss in Male and Female University Rugby Union Players. Int. J. Exerc. Sci. 2019, 12, 859–870. [Google Scholar]
- Piras, A.; Persiani, M.; Damiani, N.; Perazzolo, M.; RaffI, M. Peripheral heart action (PHA) training as a valid substitute to high intensity interval training to improve resting cardiovascular changes and autonomic adaptation. Eur. J. Appl. Physiol. 2015, 11, 763–773. [Google Scholar] [CrossRef] [PubMed]
- Astorino, T.A.; Willey, J.; Kinnahan, J.; Larsson, S.M.; Welch, H.; Dalleck, L.C. Elucidating determinants of the plateau in oxygen consumption at VO2max. Br. J. Sports Med. 2005, 39, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Holland, J.; Skinner, T.L.; Irwin, C.G.; Leveritt, M.D.; Goulet, E.D.B. The Influence of Drinking Fluid on Endurance Cycling Performance: A Meta-Analysis. Sports Med. 2017, 47, 2269–2284. [Google Scholar] [CrossRef]
- Backes, T.P.; Fitzgerald, K. Fluid Consumption, Exercise, and Cognitive Performance. Biol. Sport 2016, 33, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Campa, F.; Gatterer, H.; Lukaski, H.; Toselli, S. Stabilizing Bioimpedance-Vector-Analysis Measures With a 10-Minute Cold Shower After Running Exercise to Enable Assessment of Body Hydration. Int. J. Sports Physiol. Perform. 2019, 14, 1006–1009. [Google Scholar] [CrossRef]
- Lee, T.Q.; Yang, B.Y.; Sandusky, M.D.; McMahon, P.J. The effects of tibial rotation on the patellofemoral joint: assessment of the changes in in situ strain in the peripatellar retinaculum and the patellofemoral contact pressures and areas. J. Rehabil. Res. Dev. 2001, 38, 463–469. [Google Scholar]
- Kamen, G.; Gabriel, D.A. EMG signal processing. In Essentials of Electromyography; Human Kinetics: Champaign, IL, USA, 2010; pp. 105–154. [Google Scholar]
- Piras, A.; Campa, F.; Toselli, S.; Di Michele, R.; Raffi, M. Physiological responses to partial-body cryotherapy performed during a concurrent strength and endurance session. Appl. Physiol. Nutr. Metab. 2019, 44, 59–65. [Google Scholar] [CrossRef]
- Piras, A.; Raffi, M.; Atmatzidis, C.; Merni, F.; Di Michele, R. The energy cost of running with the ball in soccer. Int. J. Sports Med. 2017, 38, 877-822. [Google Scholar] [CrossRef]
- Piccoli, A.; Pastori, G. BIVA Software. 2002. Available online: www.renalgate.it/formule_calcolatori/BIVAguide.pdf (accessed on 30 December 2019).
- Campa, F.; Matias, C.; Gatterer, H.; Toselli, S.; Koury, J.C.; Andreoli, A.; Melchiorri, G.; Sardinha, L.B.; Silva, A.M. Classic Bioelectrical Impedance Vector Reference Values for Assessing Body Composition in Male and Female Athletes. Int. J. Environ. Res. Public Health 2019, 16, 5066. [Google Scholar] [CrossRef]
- Gonzalez, M.C.; Barbosa-Silva, T.G.; Bielemann, R.M.; Gallagher, D.; Heymsfield, S.B. Phase angle and its determinants in healthy subjects: influence of body composition. Am. J Clin. Nutr. 2016, 103, 712e6. [Google Scholar] [CrossRef]
- Francisco, R.; Matias, C.N.; Santos, D.A.; Campa, F.; Minderico, C.S.; Rocha, P.; Heymsfield, S.B.; Lukaski, H.; Sardinha, L.B.; Silva, A.M. The Predictive Role of Raw Bioelectrical Impedance Parameters in Water Compartments and Fluid Distribution Assessed by Dilution Techniques in Athletes. Int. J. Environ. Res. Public. Health 2020, 17, 759. [Google Scholar] [CrossRef]
- Toselli, S.; Marini, E.; Maietta Latessa, P.; Benedetti, L.; Campa, F. Maturity Related Differences in Body Composition Assessed by Classic and Specific Bioimpedance Vector Analysis among Male Elite Youth Soccer Players. Int. J. Environ. Res. Public Health 2020, 17, 729. [Google Scholar] [CrossRef]
- Bowtell, J.L.; Avenell, G.; Hunter, S.P.; Mileva, K.N. Effect of Hypohydration on Peripheral and Corticospinal Excitability and Voluntary Activation. PLoS ONE 2013, 8, e77004. [Google Scholar] [CrossRef] [PubMed]
- Minshull, C.; James, L. The Effects of Hypohydration and Fatigue on Neuromuscular Activation Performance. Appl. Physiol. Nutr. Metab. 2013, 38, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Pallares, J.G.; Martinez-Abellan, A.; Lopez-Gullon, J.M.; Morán-Navarro, R.; De la Cruz-Sánchez, E.; Mora-Rodríguez, R. Muscle Contraction Velocity, Strength and Power Output Changes Following Different Degrees of Hypohydration in Competitive Olympic Combat Sports. J. Int. Soc. Sports Nutr. 2016, 13, 10. [Google Scholar] [CrossRef] [PubMed]
- Schoffstall, J.E.; Branch, J.D.; Leutholtz, B.C.; Swain, D.E. Effects of Dehydration and Rehydration on the One-Repetition Maximum Bench Press of Weight-Trained Males. J. Strength Cond. Res. 2001, 15, 102–108. [Google Scholar] [PubMed]
- Judelson, D.A.; Maresh, C.M.; Anderson, J.M.; Adams, W.M.; Armstrong, L.E.; Baker, L.B.; Burke, L.; Cheuvront, S.; Chiampas, G.; González-Alonso, J.; et al. Hydration and muscular performance: does fluid balance affect strength, power and high-intensity endurance? Sports Med. 2007, 37, 907–921. [Google Scholar] [CrossRef]
- Crandall, C.G.; Gonzalez-Alonso, J. Cardiovascular Function. In the Heat-Stressed Human. Acta Physiol. 2010, 199, 407–423. [Google Scholar] [CrossRef]
- Goulet, E. Effect of Exercise-Induced Dehydration on Endurance Performance: Evaluating the Impact of Exercise Protocols on Outcomes Using a Meta-Analytic Procedure. Br. J. Sports Med. 2013, 47, 679–686. [Google Scholar] [CrossRef]
- Berkulo, M.A.; Bol, S.; Levels, K.; Lamberts, R.P.; Daanen, H.A.M.; Noakes, T.D. Ad-Libitum Drinking and Performance during a 40-Km Cycling Time Trial in the Heat. European. J. Sports Sci. 2016, 16, 213–220. [Google Scholar]
- Buono, M.J.; Wall, A.J. Effect of Hypohydration on Core Temperature during Exercise in Temperate and Hot Environments. Eur. J. Appl. Physiol. 2000, 440, 476–480. [Google Scholar] [CrossRef] [PubMed]
- Laitano, O.; Kalsi, K.K.; Pearson, J.; Lotlikar, M.; Reischak-Oliveira, A.; González-Alonso, J. Effects of Graded Exercise-Induced Dehydration and Rehydration on Circulatory Markers of Oxidative Stress across the Resting and Exercising Human Leg. European. J. Appl. Physiol. 2012, 112, 1937–1944. [Google Scholar] [CrossRef] [PubMed]

| T1 | T2 | ANOVA | |||
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Time Effect | Time x Condition | ||
| R/H (Ω/m) | HYD | 259.9 ± 36.4 | 260.4 ± 36.9 | F = 79.1; p = <0.001; η2p= 0.82 | F = 67.8; p = <0.001; η2p = 0.79 |
| DEH | 255.6 ± 35.8 | 267.4 ± 36.1 * | |||
| Xc/H (Ω/m) | HYD | 35.2 ± 5.4 | 35.3 ± 5.4 | F = 56.3; p = <0.001; η2p= 0.76 | F = 50.1; p = <0.001; η2p = 0.73 |
| DEH | 34.7 ± 6.9 | 36.9 ± 4.9 * | |||
| Vector length (Ω/m) | HYD | 262.3 ± 36.7 | 262.8 ± 37.2 | F = 82.8; p = <0.001; η2p = 0.82 | F = 71.1; p= <0.001; η2p = 0.79 |
| DEH | 257.9 ± 36.1 | 269.9 ± 36.4 * | |||
| Phase angle (°) | HYD | 7.7 ± 0.5 | 7.8 ± 0.4 | F = 3.7; p = 0.07; η2p = 0.17 | F = 3.8; p = 0.67; η2p = 0.17 |
| DEH | 7.7 ± 0.4 | 7.9 ± 0.4 | |||
| Variable | Constant Workload (65% VO2max) | Time-to-Trial (95% VO2max) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HYD | DEH | Mean Diff | p | d | HYD | DEH | Mean Diff | p | d | |
| Duration (min) | - | - | - | - | - | 3.19 ± 0.60 | 2.39 ± 0.61 | 0.80 | * 0.027 | 1.32 |
| VO2 (ml/Kg/min) | 31.41 ± 4.28 | 31.70 ± 4.88 | −0.29 | 0.616 | −0.06 | 43.79 ± 6.51 | 43.59 ± 8.89 | 0.21 | 0.904 | 0.03 |
| RER | 0.93 ± 0.06 | 0.94 ± 0.04 | −0.01 | 0.400 | −0.26 | 1.10 ± 0.10 | 1.07 ± 0.07 | 0.04 | 0.344 | 0.43 |
| EC (W/Kg) | 9.55 ± 1.40 | 9.68 ± 1.64 | −0.14 | 0.436 | −0.09 | 14.26 ± 2.41 | 14.21 ± 3.11 | 0.05 | 0.925 | 0.02 |
| HR (bpm) | 136.22 ± 8.75 | 139.53 ± 8.12 | −3.31 | * 0.005 | −0.39 | 166.56 ± 8.91 | 171.65 ± 7.89 | −5.09 | * 0.002 | −0.60 |
| Power (Watt) | 147.56 ± 29.64 | 147.56 ± 29.64 | 0.00 | - | - | 280.67 ± 56.24 | 280.67 ± 56.24 | 0.00 | - | - |
| Constant Workload (65% VO2max) | Time-to-Trial (95% VO2max) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HYD | DEH | Mean Diff | p | d | HYD | DEH | Mean Diff | p | d | |
| RVM-RMS (%MVC) | 41.96 ± 10.39 | 34.92 ± 6.53 | 7.4 | 0.011 * | 0.81 | 57.30 ± 10.98 | 48.29 ± 6.13 | 9.00 | 0.014 * | 1.01 |
| RBF-RMS (% MVC) | 20.40 ± 3.88 | 14.91 ± 2.55 | 5.49 | 0.003 * | 1.67 | 26.97 ± 4.41 | 22.05 ± 4.04 | 4.92 | 0.021 * | 1.16 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campa, F.; Piras, A.; Raffi, M.; Trofè, A.; Perazzolo, M.; Mascherini, G.; Toselli, S. The Effects of Dehydration on Metabolic and Neuromuscular Functionality during Cycling. Int. J. Environ. Res. Public Health 2020, 17, 1161. https://doi.org/10.3390/ijerph17041161
Campa F, Piras A, Raffi M, Trofè A, Perazzolo M, Mascherini G, Toselli S. The Effects of Dehydration on Metabolic and Neuromuscular Functionality during Cycling. International Journal of Environmental Research and Public Health. 2020; 17(4):1161. https://doi.org/10.3390/ijerph17041161
Chicago/Turabian StyleCampa, Francesco, Alessandro Piras, Milena Raffi, Aurelio Trofè, Monica Perazzolo, Gabriele Mascherini, and Stefania Toselli. 2020. "The Effects of Dehydration on Metabolic and Neuromuscular Functionality during Cycling" International Journal of Environmental Research and Public Health 17, no. 4: 1161. https://doi.org/10.3390/ijerph17041161
APA StyleCampa, F., Piras, A., Raffi, M., Trofè, A., Perazzolo, M., Mascherini, G., & Toselli, S. (2020). The Effects of Dehydration on Metabolic and Neuromuscular Functionality during Cycling. International Journal of Environmental Research and Public Health, 17(4), 1161. https://doi.org/10.3390/ijerph17041161










