Effects of A “Modified” Otago Exercise Program on the Functional Abilities and Social Participation of Older Adults Living in the Community—The AGA@4life Model
Abstract
1. Introduction
2. Materials and Methods
2.1. FallSensing Exergames
2.2. Participants and Ethics
2.3. Procedure
2.4. Outcomes
2.4.1. Handgrip Strength (HS)
2.4.2. 30 Seconds Sit-to-Stand (30s STS)
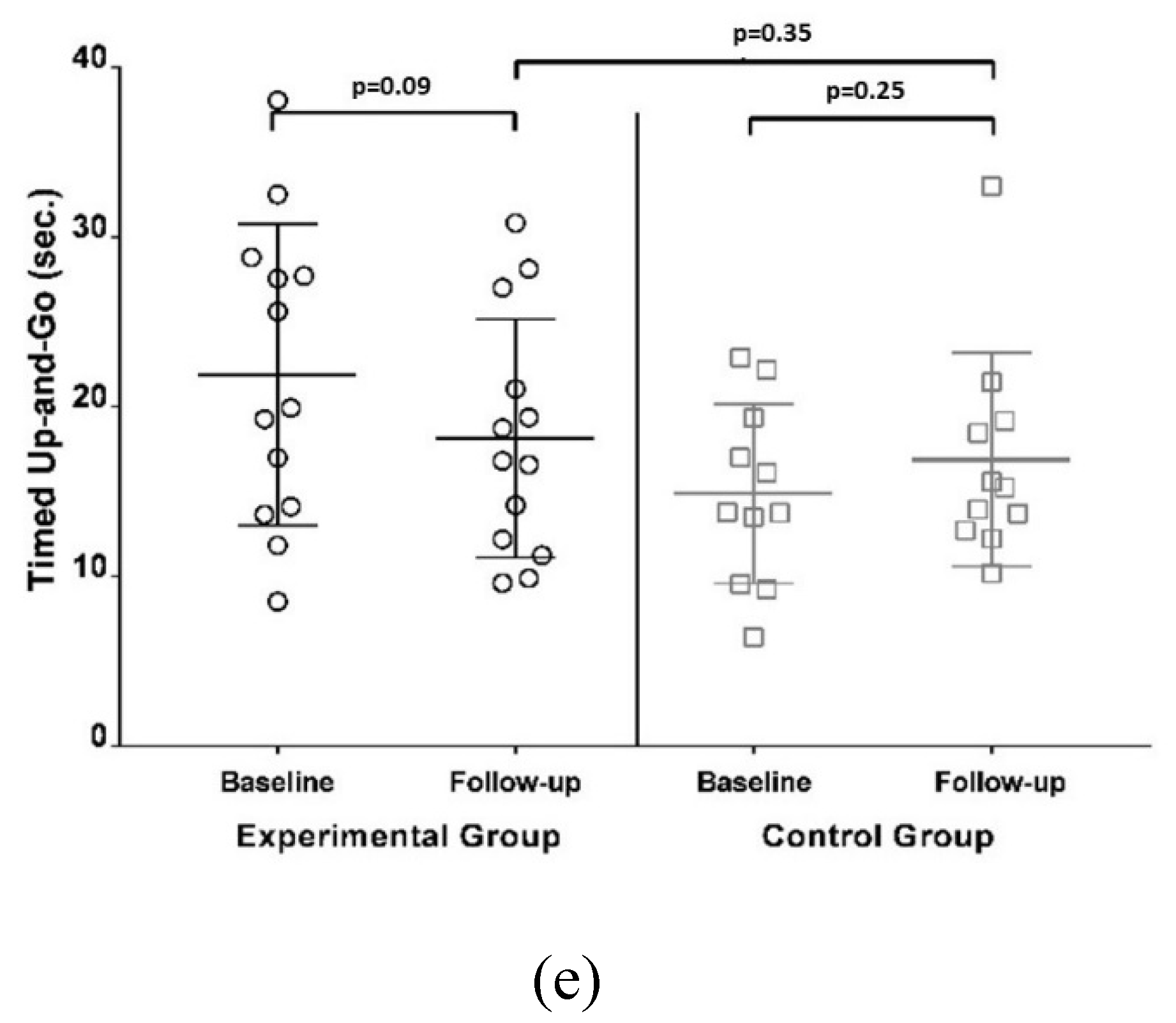
2.4.3. Timed Up and Go (TUG)
2.4.4. Step Test (ST)
2.4.5. 4 Stage Balance Test “Modified” (4StageBTM)
2.4.6. Self-Efficacy for Exercise (SEE)
2.4.7. Activities and Participation Profile related to Mobility (PAPM)
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization (WHO). Global Strategy and Action Plan on Ageing and Health; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/ageing/WHO-GSAP-2017.pdf?ua=1 (accessed on 6 June 2019).
- Ho, S.C.; Woo, J.; Yuen, Y.K.; Sham, A.; Chan, S.G. Predictors of Mobility Decline: The Hong Kong Old-old Study. J. Gerontol. Med. Sci. 1997, 52, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Buchman, A.S.; Wilson, Ã.R.S.; Boyle, P.A.; Tang, Ã.Y.; Fleischman, D.A.; Bennett, D.A. Physical Activity and Leg Strength Predict Decline in Mobility. J. Am. Geriatr. Soc. 2007, 55, 1618–1623. [Google Scholar] [CrossRef] [PubMed]
- Verghese, J.; Levalley, Ã.A.; Hall, Ã.C.B.; Katz, Ã.M.J. Epidemiology of Gait Disorders in Community-Residing Older Adults. J. Am. Geriatr. Soc. 2006, 54, 255–261. [Google Scholar] [CrossRef]
- Sturnieks, L.; St George, R.; Lord, S. Balance disorders in the elderly. Neurophysiol. Clin. Neurophysiol. 2008, 38, 467–478. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO Global Report on Falls Prevention in Older Age; World Health Organization: Lyon, France, 2007. [Google Scholar]
- Coutinho, E.D.S.F.; Silva, S.D. Uso de medicamentos como fator de risco para fratura grave decorrente de queda em idosos. Cad. Saude Publica 2002, 18, 1359–1366. [Google Scholar] [CrossRef] [PubMed]
- Gardner, M.M.; Robertson, M.C.; Campbell, A.J. Exercise in preventing falls and fall related injuries in older people: A review of randomised controlled trials. Br. J. Sports Med. 2000, 34, 7–17. [Google Scholar] [CrossRef] [PubMed]
- Sachetti, A.; Vidmar, M.F.; Marinho, M.; Schneider, R.H.; Wibelinger, M. Risco de quedas em idosos com osteoporose. Rev. Bras. Ciências Saúde 2010, 24, 22–26. [Google Scholar]
- World Health Organization (WHO). Health Literacy: The Solid Facts; WHO: Copenhagen, Denmark, 2013. [Google Scholar]
- Kerrigan, D.C.; Lee, L.W.; Collins, J.J.; Riley, P.O.; Lipsitz, L.A. Reduced Hip Extension during Walking: Healthy Elderly and Fallers versus Young Adults. Arch. Phys. Med. Rehabil. 2001, 82, 26–30. [Google Scholar] [CrossRef]
- Kwon, I.S.; Oldaker, S.; Schrager, M.; Talbot, L.A.; Fozard, J.L.; Metter, E.J. Relationship between Muscle Strength and the Time Taken to Complete a Standardized Walk-Turn-Walk Test. J. Gerontol. Biol. Sci. 2001, 56, 398–404. [Google Scholar] [CrossRef]
- Ahmadiahangar, A.; Javadian, Y.; Babaei, M.; Heidari, B.; Hosseini, S.; Aminzadeh, M. The role of quadriceps muscle strength in the development of falls in the elderly people, a cross-sectional study. Chiropr. Man. Ther. 2018, 26, 31. [Google Scholar] [CrossRef]
- American Geriatrics Society/British Geriatrics Society (AGS/BGS). Summary of the Updated American Geriatrics Society/British Geriatrics Society Clinical Practice Guideline for Prevention of Falls in Older Persons. J. Am. Geriatr. Soc. 2011, 59, 148–157. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence (NICE). Falls: Assessment and Prevention of Falls in Older People; NICE Clinical Guideline 161; NICE: London, UK, 2013.
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2009, 2, CD007146. [Google Scholar]
- Silva, T.O.; Freitas, R.S.D.F.; Monteiro, M.R.; Borges, S.D.M. Avaliação da capacidade física e quedas em idosos ativos e sedentários da comunidade. Rev. Bras. Clin. Med. 2010, 8, 392–398. [Google Scholar]
- Matsudo, S.M.; Keihan, V.; Matsudo, R.; Barros, L. Atividade física e envelhecimento: Aspectos epidemiológicos. Rev. Bras. Med. Esporte 2001, 7, 2–13. [Google Scholar] [CrossRef]
- Bjerk, M.; Brovold, T.; Skelton, D.A.; Bergland, A. A falls prevention programme to improve quality of life, physical function and falls efficacy in older people receiving home help services: Study protocol for a randomised controlled trial. BMC Health Serv. Res. 2017, 17, 559. [Google Scholar] [CrossRef]
- Accident Compensation Corporation (ACC). Otago Exercise Programme to Prevent Falls in Older Adults: A Home-Based, Individually Tailored Strength and Balance Retraining Programme; University of Otago: Dunedin, New Zealand, 2007. [Google Scholar]
- Patel, N.N. The Effects of Otago Exercise Programme for Fall Prevention in Elderly People. Int. J. Physiother. 2015, 2, 633–639. [Google Scholar] [CrossRef]
- Alhasan, H.; Hood, V.; Mainwaring, F. The effect of visual biofeedback on balance in elderly population: A systematic review. Clin. Interv. Aging 2017, 12, 487–497. [Google Scholar] [CrossRef]
- Silva, J.; Moreira, D.; Madureira, J.; Pereira, E.; Dias, A.; Sousa, I. A thecnological solution for supporting fall prevention exercises at the physiotherapy clinic. In Proceedings of the IEEE International Symposium on Medical Measurements & Applications, Rome, Italy, 11–13 June 2018. [Google Scholar]
- Sousa, I.; Silva, J.; Moreira, D.; Madureira, J.; Tonelo, C.; Dias, A. FallSensing—Tecnological solution for fall risk screening and falls prevention. In Proceedings of the EU Falls Festival, Manchester, UK, 2–3 July 2018. [Google Scholar]
- Silva, J.; Oliveira, E.; Moreira, D.; Nunes, F.; Caic, M.; Madureira, J.; Pereira, E. Design and evaluation of fall prevention multiplayer game for senior care centers. In Proceedings of the International Conference on Entertainment Computing (IFIP-ICEC’18), Poznan, Poland, 17–20 September 2018. [Google Scholar]
- Silva, J.; Oliveira, E.; Moreira, D.; Nunes, F.; Caic, M.; Madureira, J.; Pereira, E. Design and Evaluation of a Fall Prevention Multiplayer Game for Senior Care Centres. In Entertainment Computing—ICEC 2018; Lecture Notes in Computer Science; Clua, E., Roque, L., Lugmayr, A., Tuomi, P., Eds.; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Rantanen, T.; Volpato, S.; Ferrucci, L.; Heikkinen, E.; Fried, L.P.; Guralnik, J.M. Handgrip strength and cause-specific and total mortality in older disabled women: Exploring the mechanism. J. Am. Geriatr. Soc. 2003, 51, 636–641. [Google Scholar] [CrossRef]
- Aadahl, M.; Beyer, N.; Linneberg, A.; Thuesen, B.H.; Jørgensen, T. Grip strength and lower limb extension power in 19–72-year-old Danish men and women: The Health 2006 study. BMJ Open 2011, 1, e000192. [Google Scholar] [CrossRef]
- Bastiaanse, L.P.; Hilgenkamp, T.I.M.; Echteld, M.A.; Evenhuis, H.M. Prevalence and associated factors of sarcopenia in older adults with intellectual disabilities. Res. Dev. Disabil. 2012, 33, 2004–2012. [Google Scholar] [CrossRef]
- Campbell, T.M.; Vallis, L.A. Predicting fat-freemass index and sarcopenia in assisted-living older adults. Age 2014, 36, 9674. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.C.; Moreira, J.; Silva, C.; Silva, J.; Tonelo, C.; Baltazar, D.; Rocha, C.; Pereira, T.; Sousa, I. Multifactorial Screening Tool for Determining Fall Risk in Community-Dwelling Adults Aged 50 Years or Over (FallSensing): Protocol for a Prospective Study. JMIR Res. Protoc. 2018, 7, e10304. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.J.; Rikli, R.E.; Beam, W.C. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res. Q. Exerc. Sport 1999, 70, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Cadore, E.L.; Rodríguez-Mañas, L.; Sinclair, A.; Izquierdo, M. Effects of Different Exercise Interventions on Risk of Falls, Gait Ability, and Balance in Physically Frail Older Adults: A Systematic Review. Rejuvenation Res. 2013, 16, 105–114. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The Timed “Up and Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Siggeirsdóttir, K.; Jónsson, B.Y.; Jónsson, H.; Iwarsson, S. The timed ‘Up & Go’ is dependent on chair type. Clin. Rehabil. 2002, 16, 609–616. [Google Scholar]
- Rehabilitation Measures Database. Available online: https://www.sralab.org/rehabilitation-measures/hand-held-dynamometergrip-strength (accessed on 22 February 2019).
- Beauchet, O.; Fantino, B.; Allali, G.; Muir, S.; Montero-Odasso, M.; Annweiler, C. Timed Up and Go test and risk of falls in older adults: A systematic review. J. Nutr. Health Aging 2011, 15, 933–938. [Google Scholar] [CrossRef]
- Hill, K.D.; Bernhardt, J.; McGann, A.M.; Maltese, D.; Berkovits, D. A New Test of Dynamic Standing Balance for Stroke Patients: Reliability, Validity and Comparison with Healthy Elderly. Physiother. Can. 1996, 48, 257–262. [Google Scholar] [CrossRef]
- Grimmer-Somers, K.; Hillier, S.; Young, A.; Sutton, M.; Lizarondo, L. CAHE Neurological Outcomes Calculator User Manual: Monitoring Patient Status over Time Using Common Neurological Outcome Measures; University of South Australia—Centre for Allied Health Evidence: Adelaide, Australia, 2009. [Google Scholar]
- Isles, R.; Choy, N.; Steer, M.; Nitz, J. Normal values of balance tests in women aged 20–80. J. Am. Geriatr. Soc. 2004, 52, 1367–1372. [Google Scholar] [CrossRef]
- Rossiter-Fornoff, J.E.; Wolf, S.L.; Wolfson, L.I.; Buchner, D.M. A cross-sectional validation study of the FICSIT common data base static balance measures. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J. Gerontol. A Biol. Sci. Med. Sci. 1995, 50, M291–M297. [Google Scholar] [CrossRef]
- Thomas, J.C.; Odonkor, C.; Griffith, L.; Holt, N.; Percac-Lima, S.; Leveille, S.; Ni, P.; Latham, N.K.; Jette, A.M.; Bean, J.F. Reconceptualizing balance: Attributes associated with balance performance. Exp. Gerontol. 2014, 57, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.C.; Silva, C.; Moreira, J.; Rocha, C.; Gonçalves, A. Escala de autoeficácia para o exercício: Validação para a população portuguesa. In Conversas de Psicologia e do Envelhecimento Ativo; Pocinho, R., Ferreira, S.M., Anjos, V.N., Eds.; Associação Portuguesa Conversas de Psicologia: Coimbra, Portugal, 2017; pp. 126–141. [Google Scholar]
- Martins, A.C. Development and initial validation of the Activities and Participation Profile related to Mobility (APPM). BMC Health Serv. Res. 2016, 16, 78–79. [Google Scholar]
- Schoene, D.; Lord, S.R.; Delbaere, K.; Severino, C.; Davies, T.A.; Smith, S.T. A Randomized Controlled Pilot Study of Home-Based Step Training in Older People Using Videogame Technology. PLoS ONE 2013, 8, e57734. [Google Scholar] [CrossRef] [PubMed]
- Martins, A.C.; Silva, J.; Santos, A.; Madureira, J.; Alcobia, J.; Ferreira, L.; Mendes, P.; Tonelo, C.; Silva, C.; Baltazar, D.; et al. Case-based study of metrics derived from instrumented fall risk assessment tests. Gerontechnology 2016, 15, 106. [Google Scholar] [CrossRef]
- Rose, D.J.; Jones, C.J.; Lucchese, N. Predicting the Probability of Falls in Community-Residing Older Adults Using the 8-Foot Up-and-Go: A New Measure of Functional Mobility. J. Aging Phys. Act. 2002, 10, 466–475. [Google Scholar] [CrossRef]
- Lanziotti, S.; Gomes, V.; Máximo, L.S.; Marcos, J.; Dias, D.; Dias, R.C. Comparação entre diferentes pontos de corte na classificação do perfil de fragilidade de idosos comunitários. Geriatr. Gerontol. 2011, 5, 130–135. [Google Scholar]
- Murphy, M.A.; Olson, S.L.; Protas, E.J.; Overby, A.R. Screening for Falls in Community-Dwelling Elderly. J. Aging Phys. Activ. 2003, 11, 66–80. [Google Scholar] [CrossRef][Green Version]
- Shubert, T.E.; Schrodt, L.A.; Mercer, V.S.; Busby-Whitehead, J.; Giuliani, C.A. Are scores on balance screening tests associated with mobility in older adults? J. Geriatr. Phys. Ther. 2006, 29, 35–39. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention. ASSESSMENT: 30-Second Chair Stand. 2017. Available online: https://www.cdc.gov/steadi/pdf/STEADI-Assessment-30Sec-508.pdf (accessed on 18 December 2019).
- Lim, J.; Cho, J.J.; Kim, J.; Kim, Y.; Yoon, B.C. Design of virtual reality training program for prevention of falling in the elderly: A pilot study on complex versus balance exercises. Eur. J. Integr. Med. 2017, 15, 64–67. [Google Scholar] [CrossRef]
- Yoo, H.N.; Chung, E.; Lee, B.H. The Effects of Augmented Reality-based Otago Exercise on Balance, Gait, and Falls Efficacy of Elderly Women. J. Phys. Ther. Sci. 2013, 25, 797–801. [Google Scholar] [CrossRef]
- Davis, J.C.; Hsu, C.L.; Cheung, W.; Brasher, P.M.A.; Li, L.C.; Khan, K.M.; Sykes, J.; Skelton, D.A.; Liu-Ambrose, T. Can the Otago falls prevention program be delivered by video? A feasibility study. BMJ Open Sport Exerc. Med. 2016, 2, e000059. [Google Scholar] [CrossRef]
- Fu, A.S.; Gao, K.L.; Tung, A.K.; Tsang, W.W.; Kwan, M.M. Effectiveness of Exergaming Training in Reducing Risk and Incidence of Falls in Frail Older Adults with a History of Falls. Arch. Phys. Med. Rehabil. 2015, 96, 2096–2102. [Google Scholar] [CrossRef] [PubMed]
- Duque, G.; Boersma, D.; Loza-Diaz, G.; Hassan, S.; Suarez, H.; Geisinger, D.; Suriyaarachchi, P.; Sharma, A.; Demontiero, O. Effects of balance training using a virtual-reality system in older fallers. Clin. Interv. Aging 2013, 8, 257–263. [Google Scholar] [CrossRef]
- Rodrigues, E.V.; Valderramas, S.R.; Rossetin, L.L.; Gomes, A.R.S. Effects of Video Game Training on the Musculoskeletal Function of Older Adults. A Systematic Review and Meta-analysis. Top. Geriatr. Rehabil. 2014, 30, 238–245. [Google Scholar] [CrossRef]
- Prata, M.G.; Scheicher, M.E. Effects of strength and balance training on the mobility, fear of falling and grip strength of elderly female fallers. J. Bodyw. Mov. Ther. 2015, 19, 646–650. [Google Scholar] [CrossRef] [PubMed]
- Park, E.C.; Kim, S.G.; Lee, C.W. The effects of virtual reality game exercise on balance and gait of the elderly. J. Phys. Ther. Sci. 2015, 27, 1157–1159. [Google Scholar] [CrossRef] [PubMed]
- Thibaud, M.; Bloch, F.; Tournoux-Facon, C.; Brèque, C.; Rigaud, A.S.; Dugué, B.; Kemoun, G. Impact of physical activity and sedentary behaviour on fall risks in older people: A systematic review and meta-analysis of observational studies. Eur. Rev. Aging Phys. Activ. 2012, 9, 5–15. [Google Scholar] [CrossRef]
- Molina, K.I.; Ricci, N.A.; Moraes, S.A.; Perracini, M.R. Virtual reality using games for improving physical functioning in older adults: A systematic review. J. Neuroeng. Rehabil. 2014, 11, 156. [Google Scholar] [CrossRef]
- Li, J.; Erdt, M.; Chen, L.; Cao, Y.; Lee, S. The Social Effects of Exergames on Older Adults: Systematic Review and Metric Analysis. J. Med. Internet Res. 2018, 20, e10486. [Google Scholar] [CrossRef]
- Jessup, J.V.; Horne, C.; Vishen, R.K.; Wheeler, D. Effects of exercise on bone density, balance, and self-efficacy in older women. Biol. Res. Nurs. 2003, 4, 171–180. [Google Scholar] [CrossRef]
- McAuley, E.; Mihalko, S.L.; Rosengren, K. Self-efficacy and balance correlates of fear of falling in the elderly. J. Aging Phys. Activ. 1997, 5, 329–340. [Google Scholar] [CrossRef]
- Martins, A.C.; Santos, C.; Silva, C.; Baltazar, D.; Moreira, J.; Tavares, N. Does modified Otago Exercise Program improves balance in older people? A systematic review. Prev. Med. Rep. 2018, 11, 231–239. [Google Scholar] [CrossRef] [PubMed]



| Variables | Total Sample (n = 34) | Control Group (n = 16) | Intervention Group (n = 18) | p-Value |
|---|---|---|---|---|
| Age, years | 83.24 ± 6.89 | 84.88 ± 7.27 | 83.06 ± 8.52 | 0.763 |
| Gender | ||||
| Female, % (n) | 23.53 (8) | 81.25 (13) | 72.22(13) | 0.690 |
| Male, % (n) | 76.47(26) | 18.75 (3) | 27.78 (5) | |
| History of falls in the last 12 months | ||||
| Yes, % (n) | 41.18 (14) | 31.25 (5) | 50.00 (9) | 0.320 |
| No, % (n) | 58.82 (20) | 68.75 (11) | 50.00 (9) | |
| Fear of falling | ||||
| Yes, % (n) | 85.29 (29) | 81.25 (13) | 88.89 (16) | 0.650 |
| No, % (n) | 14.71 (5) | 18.75 (3) | 11.11 (2) | |
| Sedentary lifestyle | ||||
| Yes, % (n) | 76.47 (26) | 75.00 (12) | 77.78 (14) | 1.00 |
| No, % (n) | 23.53 (8) | 25.00 (4) | 22.22 (4) | |
| Upper extremities assistance to stand from a chair | ||||
| Yes, % (n) | 73.53 (25) | 62.50 (10) | 83.33 (15) | 0.250 |
| No, % (n) | 26.47 (9) | 37.50 (6) | 16.67 (3) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martins, A.C.; Guia, D.; Saraiva, M.; Pereira, T. Effects of A “Modified” Otago Exercise Program on the Functional Abilities and Social Participation of Older Adults Living in the Community—The AGA@4life Model. Int. J. Environ. Res. Public Health 2020, 17, 1258. https://doi.org/10.3390/ijerph17041258
Martins AC, Guia D, Saraiva M, Pereira T. Effects of A “Modified” Otago Exercise Program on the Functional Abilities and Social Participation of Older Adults Living in the Community—The AGA@4life Model. International Journal of Environmental Research and Public Health. 2020; 17(4):1258. https://doi.org/10.3390/ijerph17041258
Chicago/Turabian StyleMartins, Anabela Correia, Daniela Guia, Marina Saraiva, and Telmo Pereira. 2020. "Effects of A “Modified” Otago Exercise Program on the Functional Abilities and Social Participation of Older Adults Living in the Community—The AGA@4life Model" International Journal of Environmental Research and Public Health 17, no. 4: 1258. https://doi.org/10.3390/ijerph17041258
APA StyleMartins, A. C., Guia, D., Saraiva, M., & Pereira, T. (2020). Effects of A “Modified” Otago Exercise Program on the Functional Abilities and Social Participation of Older Adults Living in the Community—The AGA@4life Model. International Journal of Environmental Research and Public Health, 17(4), 1258. https://doi.org/10.3390/ijerph17041258






