The Association between Health Insurance and All-Cause, Cardiovascular Disease, Cancer and Cause-Specific Mortality: A Prospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Outcomes
2.3. The Definition of Insurance Status
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
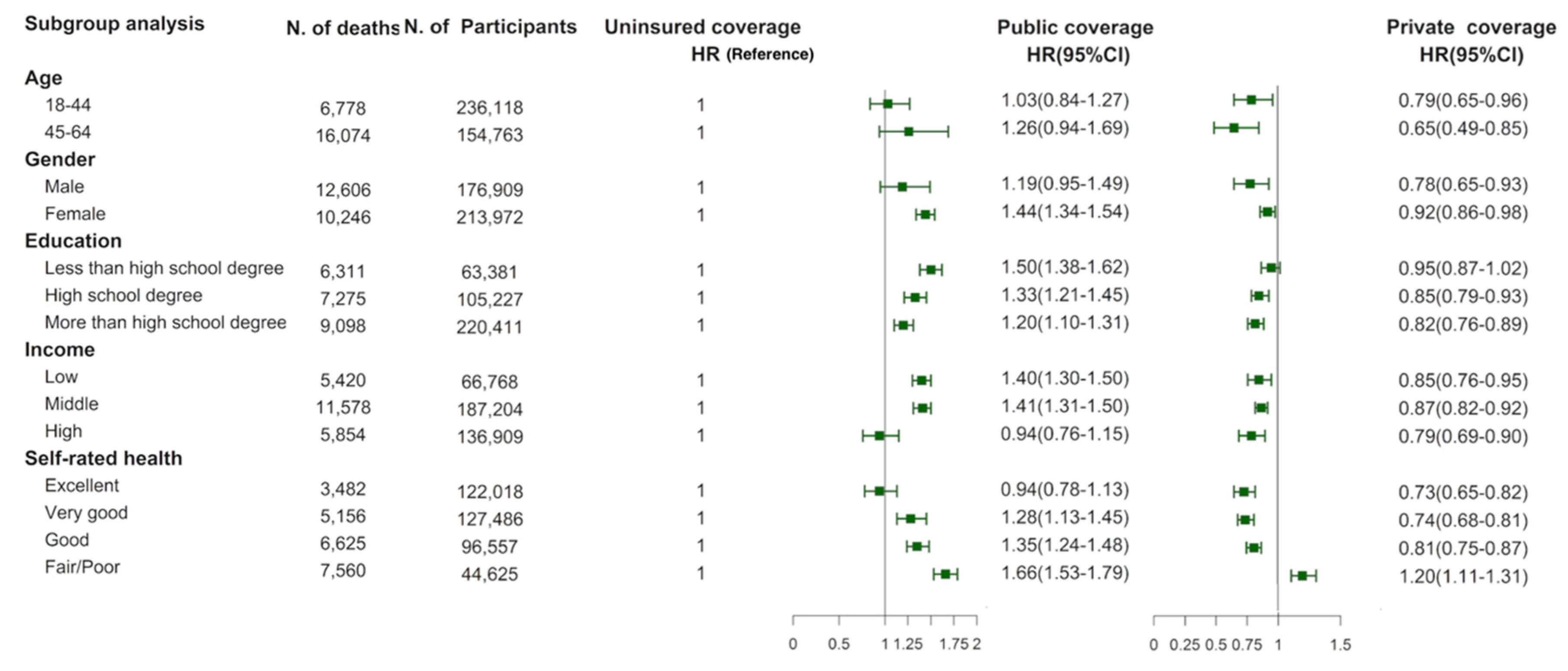
3.2. Insurance Status and All-Cause Mortality
3.3. Insurance Status and CVD, Cancer and Cause-Specific Mortality
3.4. Sensitivity Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Stone, G.S.; Tarus, T.; Shikanga, M.; Biwott, B.; Ngetich, T.; Andale, T.; Cheriro, B.; Aruasa, W. The association between insurance status and in-hospital mortality on the public medical wards of a Kenyan referral hospital. Glob. Health Action 2014, 7, 23137. [Google Scholar] [CrossRef] [PubMed]
- Cohen, R.; Terlizzi, E.; Martinez, M. Health Insurance Coverage: Early Release of Estimates from the National Health Interview Survey, 2018; National Center for Health Statistics: Hyattsville, MD, USA, 2019. [Google Scholar]
- Woolhandler, S.; Himmelstein, D.U. The Relationship of Health Insurance and Mortality: Is Lack of Insurance Deadly? Ann. Intern. Med. 2017, 167, 424–431. [Google Scholar] [CrossRef] [PubMed]
- Ayanian, J.Z.; Weissman, J.S.; Schneider, E.C.; Ginsburg, J.A.; Zaslavsky, A.M. Unmet health needs of uninsured adults in the United States. JAMA 2000, 284, 2061–2069. [Google Scholar] [CrossRef] [PubMed]
- Flocke, S.A.; Gilchrist, V. Physician and patient gender concordance and the delivery of comprehensive clinical preventive services. Med. Care 2005, 43, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Wilper, A.P.; Woolhandler, S.; Lasser, K.E.; McCormick, D.; Bor, D.H.; Himmelstein, D.U. Health insurance and mortality in US adults. Am. J. Public Health 2009, 99, 2289–2295. [Google Scholar] [CrossRef]
- Zhou, M.; Liu, S.; Kate Bundorf, M.; Eggleston, K.; Zhou, S. Mortality In Rural China Declined As Health Insurance Coverage Increased, But No Evidence The Two Are Linked. Health Aff. (Millwood) 2017, 36, 1672–1678. [Google Scholar] [CrossRef]
- Rohlfing, M.L.; Mays, A.C.; Isom, S.; Waltonen, J.D. Insurance status as a predictor of mortality in patients undergoing head and neck cancer surgery. Laryngoscope 2017, 127, 2784. [Google Scholar] [CrossRef]
- Ward, B.W.; Martinez, M.E. Health Insurance Status and Psychological Distress among US Adults Aged 18–64 Years. Stress Health 2015, 31, 324–335. [Google Scholar] [CrossRef]
- Mukamal, K.J.; Chen, C.M.; Rao, S.R.; Breslow, R.A. Alcohol Consumption and Cardiovascular Mortality Among U.S. Adults, 1987 to 2002. J. Am. Coll. Cardiol. 2010, 55, 1328–1335. [Google Scholar] [CrossRef]
- Gregg, E.W.; Cheng, Y.J.; Srinivasan, M.; Lin, J.; Imperatore, G. Trends in cause-specific mortality among adults with and without diagnosed diabetes in the USA: An epidemiological analysis of linked national survey and vital statistics data. Lancet 2018, 391, 2430–2440. [Google Scholar] [CrossRef]
- Terlizzi, E.P.; Cohen, R.A.; Martinez, M.E. National Center for Health Statistics. Health insurance coverage: Early release of estimates from the National Health Interview Survey, January–September 2018. Available online: https://www.cdc.gov/nchs/data/nhis/earlyrelease/insur201902.pdf (accessed on 1 November 2019).
- Zhao, G.; Okoro, C.A.; Li, J.; Town, M. Health Insurance Status and Clinical Cancer Screenings Among U.S. Adults. Am. J. Prev. Med. 2017, 54, e11–e19. [Google Scholar] [CrossRef] [PubMed]
- Schoen, C.; DesRoches, C. Uninsured and unstably insured: The importance of continuous insurance coverage. Health Serv. Res. 2000, 35, 187–206. [Google Scholar] [PubMed]
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report, 2008; To the Secretary of Health and Human Services. Part A: Executive Summary; US Department of Health and Human Services: Washington, DC, USA, 2009; Volume 67, pp. 114–120.
- Lau, B.; Cole, S.R.; Gange, S.J. Competing risk regression models for epidemiologic data. Am. J. Epidemiol. 2009, 170, 244–256. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, T.; Sugiyama, K.; Aida, J.; Tsuboya, T.; Osaka, K. The Contextual Effect of Area-Level Unemployment Rate on Lower Back Pain: A Multilevel Analysis of Three Consecutive Surveys of 962,586 Workers in Japan. Int. J. Environ. Res. Public Health 2019, 16, 4016. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Ding, P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann. Intern. Med. 2017, 167, 268–274. [Google Scholar] [CrossRef]
- Sorlie, P.D.; Johnson, N.J.; Backlund, E.; Bradham, D.D. Mortality in the Uninsured Compared with That in Persons with Public and Private Health Insurance. Arch. Intern. Med. 1994, 154, 2409–2416. [Google Scholar] [CrossRef]
- Kronick, R. Health insurance coverage and mortality revisited. Health Serv. Res. 2009, 44, 1211–1231. [Google Scholar] [CrossRef]
- Franks, P.; Clancy, C.M.; Gold, M.R. Health insurance and mortality. Evidence from a national cohort. JAMA 1993, 270, 737–741. [Google Scholar] [CrossRef]
- Baicker, K.; Taubman, S.L.; Allen, H.L.; Bernstein, M.; Gruber, J.H.; Newhouse, J.P.; Schneider, E.C.; Wright, B.J.; Zaslavsky, A.M.; Finkelstein, A.N.; et al. The Oregon experiment—Effects of Medicaid on clinical outcomes. N. Engl. J. Med. 2013, 368, 1713–1722. [Google Scholar] [CrossRef]
- Baicker, K.; Finkelstein, A. The effects of Medicaid coverage—Learning from the Oregon experiment. N. Engl. J. Med. 2011, 365, 683–685. [Google Scholar] [CrossRef]
- Weathers, R.R., II; Stegman, M. The effect of expanding access to health insurance on the health and mortality of Social Security Disability Insurance beneficiaries. J. Health Econ. 2012, 31, 863–875. [Google Scholar] [CrossRef] [PubMed]
- Polsky, D.; Doshi, J.A.; Escarce, J.; Manning, W.; Paddock, S.M.; Cen, L.; Rogowski, J. The health effects of Medicare for the near-elderly uninsured. Health Serv. Res. 2009, 44, 926–945. [Google Scholar] [CrossRef] [PubMed]
- Schisterman, E.F.; Cole, S.R.; Platt, R.W. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology 2009, 20, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zhang, Y.; Xiong, F.; Li, H.; Ding, Y.; Gao, Y.; Zhao, L.; Wan, S. Association between medical insurance type and survival in patients undergoing peritoneal dialysis. BMC Nephrol. 2015, 16, 33. [Google Scholar] [CrossRef][Green Version]
- Fan, H.; Zhao, Y.; Chen, G.D.; Sun, M.; Zhu, J.H. Health insurance status and risk factors of mortality in patients with septic acute kidney injury in Ningbo, China. J. Int. Med. Res. 2019, 47, 370–376. [Google Scholar] [CrossRef]
- Rosengren, A.; Smyth, A.; Rangarajan, S.; Ramasundarahettige, C.; Bangdiwala, S.I.; AlHabib, K.F.; Avezum, A.; Bengtsson Bostrom, K.; Chifamba, J.; Gulec, S.; et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: The Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob. Health 2019, 7, e748–e760. [Google Scholar] [CrossRef]
- Moon, S.H.; Seo, H.J.; Lee, D.Y.; Kim, S.M.; Park, J.M. Associations Among Health Insurance Type, Cardiovascular Risk Factors, and the Risk of Dementia: A Prospective Cohort Study in Korea. Int. J. Environ. Res. Public Health 2019, 16, 2616. [Google Scholar] [CrossRef]
- Kariisa, M.; Seiber, E. Distribution of cardiovascular disease and associated risk factors by county type and health insurance status: Results from the 2008 Ohio Family Health Survey. Public Health Rep. 2015, 130, 87–95. [Google Scholar] [CrossRef]
- Dalinjong, P.A.; Welaga, P.; Akazili, J.; Kwarteng, A.; Bangha, M.; Oduro, A.; Sankoh, O.; Goudge, J. The association between health insurance status and utilization of health services in rural Northern Ghana: Evidence from the introduction of the National Health Insurance Scheme. J. Health Popul. Nutr. 2017, 36, 42. [Google Scholar] [CrossRef]
- Mikhail, J.N.; Nemeth, L.S.; Mueller, M.; Pope, C.; NeSmith, E.G.; Wilson, K.L.; McCann, M.; Fakhry, S.M. The Association of Race, Socioeconomic Status, and Insurance on Trauma Mortality. J. Trauma Nurs. 2016, 23, 347–356. [Google Scholar] [CrossRef]


| Characteristics | Uninsured | Public Coverage | Private Coverage | p Value |
|---|---|---|---|---|
| No. (Weighted %) | No. (Weighted %) | No. (Weighted %) | ||
| Total population | 80449 (18.8) | 51236 (10.9) | 259196 (70.3) | |
| Age | <0.001 | |||
| 18–44 | 57215 (73) | 28833 (57.9) | 150070 (58) | |
| 45–64 | 23234 (27) | 22403 (42.1) | 109126 (42) | |
| Gender | <0.001 | |||
| Male | 39779 (54) | 17743 (40.6) | 119387 (49.3) | |
| Female | 40670 (46) | 33493 (59.4) | 139809 (50.7) | |
| Race | <0.001 | |||
| Hispanic | 30070 (29.9) | 12079 (17.4) | 32131 (8.9) | |
| Non-Hispanic White | 33481 (50.5) | 23147 (55.2) | 180642 (76.1) | |
| Non-Hispanic Black | 13419 (14.9) | 13537 (22.3) | 32279 (9.8) | |
| Non-Hispanic Other | 3479 (4.8) | 2473 (5) | 14144 (5.2) | |
| Education | <0.001 | |||
| Less than high school degree | 26074 (29.8) | 16532 (29.9) | 20775 (7.6) | |
| High school degree | 25216 (33.6) | 15679 (32) | 64332 (25.5) | |
| More than high school degree | 28548 (35.8) | 18617 (37.1) | 173246 (66.6) | |
| Missing | 611 (0.9) | 408 (0.9) | 843 (0.3) | |
| Income | <0.001 | |||
| Low | 25599 (26.8) | 25471 (41.2) | 15698 (4.7) | |
| Middle | 47586 (61.7) | 21568 (47.6) | 118050 (43) | |
| High | 7264 (11.5) | 4197 (11.2) | 125448 (52.4) | |
| BMI (kg/m2) | <0.001 | |||
| <25 | 30780 (39.1) | 16733 (33.5) | 101702 (39.1) | |
| 25–30 | 26613 (32.2) | 15190 (29.4) | 88102 (34.3) | |
| >30 | 19822 (24.7) | 17321 (33.2) | 60848 (23.4) | |
| Missing | 3234 (4) | 1992 (3.9) | 8544 (3.2) | |
| Smoking status | <0.001 | |||
| Never cigarette | 43530 (52.6) | 25328 (49.3) | 155505 (60.1) | |
| Former cigarette | 10180 (12.5) | 8588 (17.4) | 51300 (20.2) | |
| Current cigarette | 26248 (34.2) | 16980 (32.7) | 50904 (19.1) | |
| Missing | 491 (0.6) | 340 (0.7) | 1487 (0.6) | |
| Alcohol intake | <0.001 | |||
| Lifetime abstainer | 21399 (25.7) | 15349 (30.1) | 44236 (17.2) | |
| Former drinker | 9970 (12.2) | 10569 (20.3) | 29185 (11.1) | |
| Current drinker | 47652 (60.3) | 24367 (47.8) | 181845 (70.2) | |
| Missing | 1428 (1.9) | 951 (1.9) | 3930 (1.5) | |
| Physical activity | <0.001 | |||
| Meeting guideline | 28973 (37.1) | 14718 (30.1) | 126613 (49.4) | |
| Not meeting guideline | 49154 (59.8) | 35138 (67) | 124450 (47.3) | |
| Missing | 2322 (3.2) | 1380 (2.9) | 8133 (3.3) | |
| Hypertension | <0.001 | |||
| Yes | 13390 (15.9) | 17309 (32.4) | 52292 (19.9) | |
| No | 66926 (83.9) | 33824 (67.4) | 206705 (80.1) | |
| Missing | 133 (0.2) | 103 (0.2) | 199 (0.1) | |
| Diabetes | <0.001 | |||
| Yes | 3555 (4.4) | 6522 (12.1) | 12566 (4.8) | |
| No | 76831 (95.5) | 44666 (87.8) | 246481 (95.2) | |
| Missing | 63 (0.1) | 48 (0.1) | 149 (0.1) | |
| CHD | <0.001 | |||
| Yes | 1111 (1.3) | 2871 (5.4) | 4527 (1.8) | |
| No | 79271 (98.7) | 48209 (94.6) | 254488 (98.2) | |
| Missing | 67 (0.1) | 156 (0.1) | 181 (0.1) | |
| Stroke | <0.001 | |||
| Yes | 840 (1) | 2541 (4.7) | 2182 (0.8) | |
| No | 79564 (99) | 48597 (95.1) | 256874 (99.1) | |
| Missing | 45 (0) | 98 (0.2) | 140 (0.1) | |
| Cancer | <0.001 | |||
| Yes | 2158 (2.7) | 3495 (6.7) | 12139 (4.7) | |
| No | 78223 (97.3) | 47649 (93.1) | 246889 (95.2) | |
| Missing | 68 (0.1) | 92 (0.2) | 168 (0.1) | |
| Self-rated health | <0.001 | |||
| Excellent | 21376 (27.7) | 8606 (17.7) | 92036 (36.6) | |
| Very good | 23993 (30) | 10480 (21.2) | 93013 (35.7) | |
| Good | 24453 (29.9) | 14575 (28.7) | 57529 (21.7) | |
| Fair/Poor | 10576 (12.3) | 17519 (32.2) | 16530 (6) | |
| Missing | 51 (0.1) | 56 (0.1) | 88 (0) |
| Outcomes | Uninsured | Public Coverage | Private Coverage | ||
|---|---|---|---|---|---|
| HR (95%CI) | HR (95%CI) | p Value | HR (95%CI) | p Value | |
| Excluding participants with CHD, stroke or cancer | |||||
| All-cause mortality | 1 (Reference) | 1.24 (1.18,1.31) | <0.01 | 0.80 (0.76,0.84) | <0.01 |
| Cancer mortality | 1 (Reference) | 1.08 (0.95,1.22) | 0.23 | 0.88 (0.81,0.96) | 0.01 |
| CVD mortality | 1 (Reference) | 1.10 (0.95,1.27) | 0.21 | 0.76 (0.67,0.87) | <0.01 |
| Heart disease mortality | 1 (Reference) | 1.17 (0.99,1.38) | 0.07 | 0.78 (0.67,0.91) | <0.01 |
| Stroke mortality | 1 (Reference) | 0.87 (0.64,1.19) | 0.38 | 0.69 (0.53,0.89) | <0.01 |
| Influenza and pneumonia mortality | 1 (Reference) | 1.34 (0.84,2.14) | 0.22 | 0.99 (0.64,1.52) | 0.95 |
| Kidney disease mortality | 1 (Reference) | 2.08 (1.24,3.49) | 0.01 | 0.89 (0.60,1.33) | 0.58 |
| Alzheimer mortality | 1 (Reference) | 0.42 (0.13,1.36) | 0.15 | 1.05 (0.38,2.90) | 0.92 |
| CLRD mortality | 1 (Reference) | 1.84 (1.38,2.46) | <0.01 | 0.89 (0.67,1.18) | 0.43 |
| Diabetes mortality | 1 (Reference) | 1.37 (1.01,1.86) | 0.05 | 0.91 (0.69,1.20) | 0.51 |
| Excluding participants who died >2 year after the interview | |||||
| All-cause mortality | 1 (Reference) | 1.32 (1.26,1.39) | <0.01 | 0.85 (0.82,0.89) | <0.01 |
| Cancer mortality | 1 (Reference) | 1.13 (1.02,1.25) | 0.02 | 0.97 (0.90,1.06) | 0.52 |
| CVD mortality | 1 (Reference) | 1.25 (1.10,1.42) | <0.01 | 0.82 (0.73,0.93) | <0.01 |
| Heart disease mortality | 1 (Reference) | 1.31 (1.14,1.51) | <0.01 | 0.85 (0.74,0.98) | 0.02 |
| Stroke mortality | 1 (Reference) | 1.02 (0.79,1.31) | 0.90 | 0.73 (0.57,0.93) | <0.01 |
| Influenza and pneumonia mortality | 1 (Reference) | 1.40 (0.91,2.14) | 0.12 | 1.07 (0.70,1.62) | 0.76 |
| Kidney disease mortality | 1 (Reference) | 2.19 (1.48,3.24) | <0.01 | 0.79 (0.56,1.12) | 0.19 |
| Alzheimer mortality | 1 (Reference) | 0.99 (0.37,2.65) | 0.99 | 1.24 (0.47,3.26) | 0.67 |
| CLRD mortality | 1 (Reference) | 1.77 (1.38,2.29) | <0.01 | 0.96 (0.74,1.24) | 0.74 |
| Diabetes mortality | 1 (Reference) | 1.58 (1.22,2.06) | <0.01 | 0.86 (0.66,1.11) | 0.24 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, L.; Wang, Y.; Chen, B.; Yang, T.; Zhang, W.; Wang, Y. The Association between Health Insurance and All-Cause, Cardiovascular Disease, Cancer and Cause-Specific Mortality: A Prospective Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 1525. https://doi.org/10.3390/ijerph17051525
Song L, Wang Y, Chen B, Yang T, Zhang W, Wang Y. The Association between Health Insurance and All-Cause, Cardiovascular Disease, Cancer and Cause-Specific Mortality: A Prospective Cohort Study. International Journal of Environmental Research and Public Health. 2020; 17(5):1525. https://doi.org/10.3390/ijerph17051525
Chicago/Turabian StyleSong, Liying, Yan Wang, Baodong Chen, Tan Yang, Weiliang Zhang, and Yafeng Wang. 2020. "The Association between Health Insurance and All-Cause, Cardiovascular Disease, Cancer and Cause-Specific Mortality: A Prospective Cohort Study" International Journal of Environmental Research and Public Health 17, no. 5: 1525. https://doi.org/10.3390/ijerph17051525
APA StyleSong, L., Wang, Y., Chen, B., Yang, T., Zhang, W., & Wang, Y. (2020). The Association between Health Insurance and All-Cause, Cardiovascular Disease, Cancer and Cause-Specific Mortality: A Prospective Cohort Study. International Journal of Environmental Research and Public Health, 17(5), 1525. https://doi.org/10.3390/ijerph17051525




