Analysis of Caesarean Section Rates Using the Robson Classification System at a University Hospital in Spain
Abstract
1. Background
2. Methods
2.1. Design, Population, and Sample
2.2. Data Collection Tools
2.3. Statistical Analysis
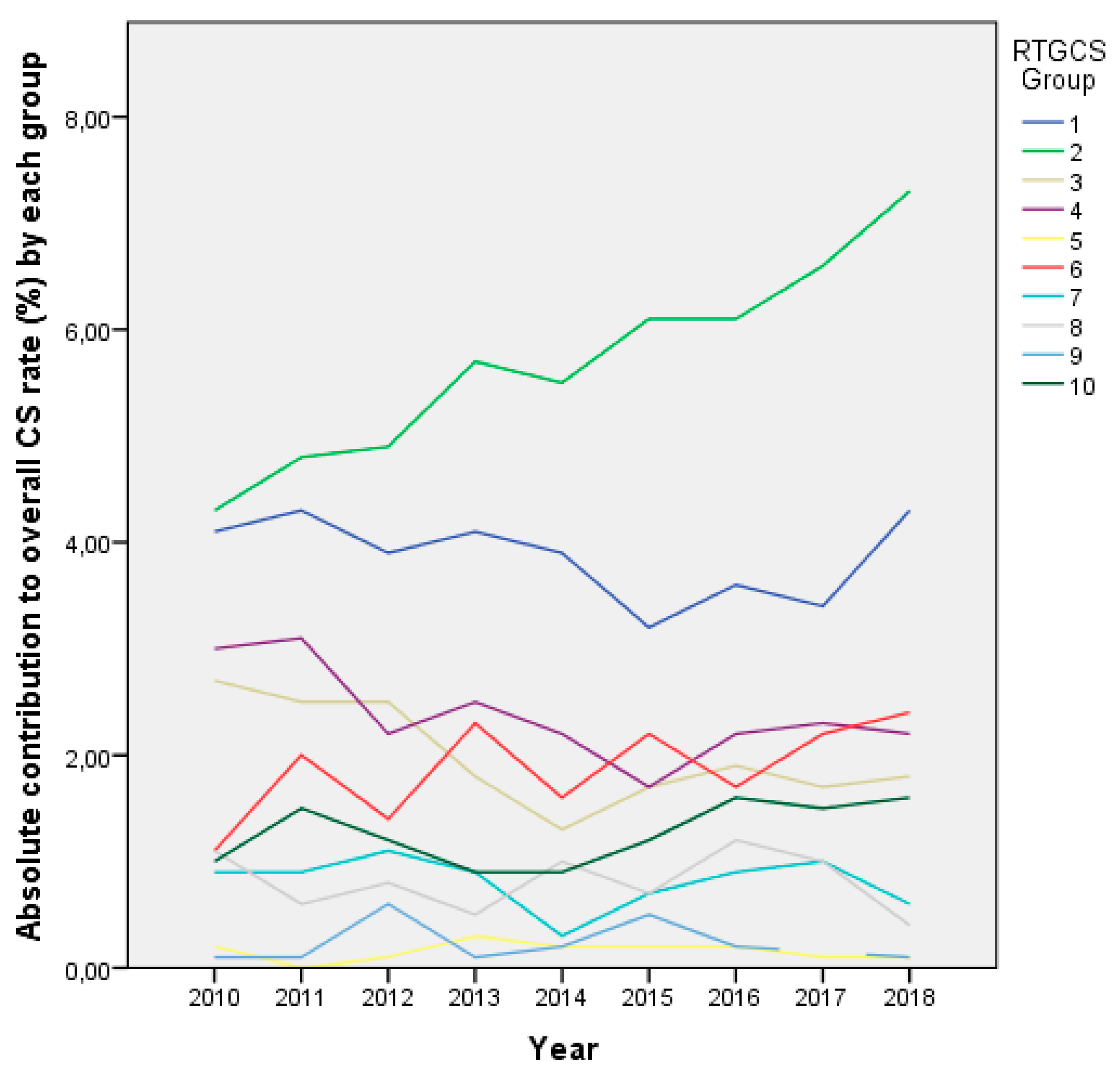
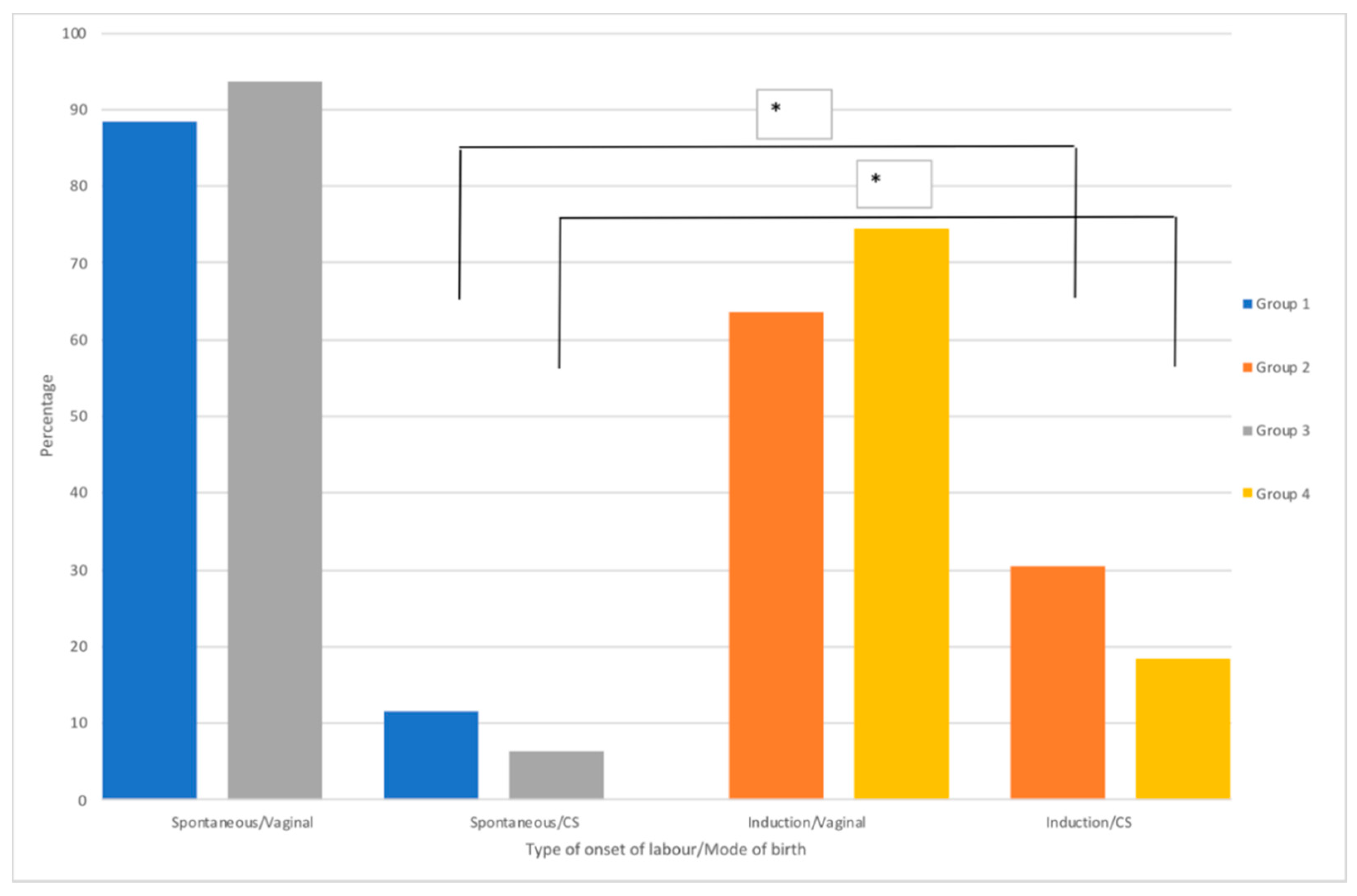
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CTG | Cardiotocographic fetal monitoring |
| CS | Caesarean Section |
| PP | Prolonged pregnancy |
| PROM | Prolonged Rupture of Membranes |
| RTGCS | Robson ten-group classification system |
| LRUH | La Ribera University Hospital |
| VBAC | Vaginal Birth After Caesarean |
| WHO | World Health Organization |
References
- Betrán, A.P.; Ye, J.; Moller, A.B.; Zhang, J.; Gülmezoglu, A.M.; Torloni, M.R. The increasing trend in caesarean section rates: Global, regional and national estimates: 1990-2014. PLoS ONE 2016, 11, e0148343. [Google Scholar] [CrossRef] [PubMed]
- Cagan, M.; Tanacan, A.; Aydin Hakli, D.; Beksac, M.S. Changing rates of the modes of delivery over the decades (1976, 1986, 1996, 2006, and 2016) based on the Robson-10 group classification system in a single tertiary health care center. J. Matern.-Fetal Neonatal. Med. 2019, 7058, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Souza, J.P.; Gülmezoglu, A.M.; Lumbiganon, P.; Laopaiboon, M.; Carroli, G.; Fawole, B.; Ruyan, P. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: The 2004–2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med. 2010, 8, 71. [Google Scholar] [CrossRef] [PubMed]
- Tura, A.K.; Pijpers, O.; De Man, M.; Cleveringa, M.; Koopmans, I.; Gure, T.; Stekelenburg, J. Analysis of caesarean sections using Robson 10-group classification system in a university hospital in eastern Ethiopia: A cross-sectional study. BMJ Open 2018, 8, e020520. [Google Scholar] [CrossRef]
- Kirchengast, S.; Hartmann, B. Recent lifestyle parameters are associated with increasing caesarean section rates among singleton term births in Austria. Int. J. Environ. Res. Public Health 2019, 16, 14. [Google Scholar] [CrossRef]
- Rodríguez-Blanco, N.; Tuells, J.; Vila-Candel, R.; Nolasco, A. Adherence and concordance of influenza and pertussis vaccination coverage in pregnant women in Spain. Int. J. Environ. Res. Public Health 2019, 16, 543. [Google Scholar] [CrossRef]
- OECD. Health at a Glance 2017: OECD Indicators; OECD Publishing: Paris, France, 2017; pp. 180–181. [Google Scholar]
- Aguilar Redondo, R.; Manrique Fuentes, G.; Aisa Denaroso, L.M.; Delgado Martínez, L.; González Acosta, V.; Aceituno Velasco, L. Uso de la clasificación de Robson en un Hospital Comarcal de España para reducir la tasa de cesáreas. Rev. Chil. Obstet. Ginecol. 2016, 81, 99–104. [Google Scholar] [CrossRef]
- Ye, J.; Zhang, J.; Mikolajczyk, R.; Torloni, M.R.; Gülmezoglu, A.M.; Betran, A.P. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: A worldwide population-based ecological study with longitudinal data. BJOG Int. J. Obstet. Gynaecol. 2016, 123, 745–753. [Google Scholar] [CrossRef]
- Betrán, A.P.; Vindevoghel, N.; Souza, J.P.; Gülmezoglu, A.M.; Torloni, M.R. A systematic review of the Robson classification for caesarean section: What works, doesn’t work and how to improve it. PLoS ONE 2014, 9, e97769. [Google Scholar] [CrossRef]
- Robson, M. The ten group classification system (TGCS)-a common starting point for more detailed analysis. BJOG Int. J. Obstet. Gynaecol. 2015, 122, 701. [Google Scholar] [CrossRef]
- Chen, I.; Opiyo, N.; Tavender, E.; Mortazhejri, S.; Rader, T.; Petkovic, J.; Yogasingam, S.; Taljaard, M.; Agarwal, S.; Laopaiboon, M.; et al. Non-clinical interventions for reducing unnecessary caesarean section. Cochrane Database Syst. Rev. 2018, CS005528. [Google Scholar] [CrossRef] [PubMed]
- Betran, A.P.; Torloni, M.R.; Zhang, J.J.; Gülmezoglu, A.M. WHO statement on caesarean section rates. BJOG Int. J. Obstet. Gynaecol. 2016, 123, 667–670. [Google Scholar] [CrossRef] [PubMed]
- Cabeza Vengoechea, P.J.; Calvo Pérez, A.; Betrán, A.P.; del Mar Morey, M.M.; Febles Borges, M.M.; Alcácer, P.X.; Alcover, A.R.; Campos Villamiel, E.F.; Morán Antolín, E.M.; Rehkugler, S.; et al. Clasificación de cesáreas por Grupos de Robson en dos periodos comparativos en el Hospital de Manacor. Progresos Obstet. Ginecol. 2010, 53, 385–390. [Google Scholar] [CrossRef]
- WHO. Robson Classification: Implementation Manual; WHO: Geneva, Switzerland, 2017; ISBN 978-92-4-151319-7. [Google Scholar]
- WHO; HRP. WHO Statement on Caesarean Section Rates; WHO: Geneva, Switzerland, 2015; pp. 667–670. [Google Scholar]
- Smith, D.C.; Phillippi, J.C.; Lowe, N.K.; Breman, R.B.; Carlson, N.S.; Neal, J.L.; Gutierrez, E.; Tilden, E.L. Using the Robson 10-Group Classification System to Compare Cesarean Birth Utilization Between US Centers With and Without Midwives. J. Midwifery Women Health 2019, 65, 10–21. [Google Scholar] [CrossRef]
- Tapia, V.; Betran, A.P.; Gonzales, G.F. Caesarean section in Peru: Analysis of trends using the Robson classification system. PLoS ONE 2016, 11, e0148138. [Google Scholar] [CrossRef]
- Dunn, L.; Kumar, S.; Beckmann, M. Maternal age is a risk factor for caesarean section following induction of labor. Aust. N. Z. J. Obstet. Gynaecol. 2017, 57, 426–431. [Google Scholar] [CrossRef]
- Yoshioka-Maeda, K.; Ota, E.; Ganchimeg, T.; Kuroda, M.; Mori, R. Caesarean section by maternal age group among singleton deliveries and primiparous Japanese women: A secondary analysis of the WHO Global Survey on Maternal and Perinatal Health. BMC Pregnancy Childbirth 2016, 16, 39. [Google Scholar] [CrossRef]
- Rydahl, E.; Declercq, E.; Juhl, M.; Maimburg, R.D. Cesarean section on a rise—Does advanced maternal age explain the increase? A population register-based study. PLoS ONE 2019, 14. [Google Scholar] [CrossRef]
- Vogel, J.P.; Betrán, A.P.; Vindevoghel, N.; Souza, J.P.; Torloni, M.R.; Zhang, J.; Tunçalp, Ö.; Mori, R.; Morisaki, N.; Ortiz-Panozo, E.; et al. Use of the robson classification to assess caesarean section trends in 21 countries: A secondary analysis of two WHO multicountry surveys. Lancet Glob. Health 2015, 5, e260–e270. [Google Scholar] [CrossRef]
- Lafitte, A.S.; Dolley, P.; Le Coutour, X.; Benoist, G.; Prime, L.; Thibon, P.; Dreyfus, M. Rate of caesarean sections according to the Robson classification: Analysis in a French perinatal network—Interest and limitations of the French medico-administrative data (PMSI). J. Gynecol. Obstet. Hum. Reprod. 2018, 47, 39–44. [Google Scholar] [CrossRef]
- Assar, T.M.; Nucier, A.A.A.R.; Raziq, H.E.A.; Abd El-Azym Saad, A.S.; Megahed Amer, W.; Jadoon, B. Analysis of the caesarean section rate using the 10-Group Robson classification at Benha University Hospital, Egypt. Women Birth 2019, 33, e105–e110. [Google Scholar] [CrossRef]
- Macfarlane, A.J.; Blondel, B.; Mohangoo, A.D.; Cuttini, M.; Nijhuis, J.; Novak, Z.; Ólafsdóttir, H.S.; Zeitlin, J. Wide differences in mode of delivery within Europe: Risk-stratified analyses of aggregated routine data from the Euro-Peristat study. BJOG Int. J. Obstet. Gynaecol. 2016, 123, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Kacerauskiene, J.; Bartuseviciene, E.; Railaite, D.R.; Minkauskiene, M.; Bartusevicius, A.; Kliucinskas, M.; Simoliuniene, R.; Nadisauskiene, R.J. Implementation of the Robson classification in clinical practice: Lithuania’s experience. BMC Pregnancy Childbirth 2017, 17, 432. [Google Scholar] [CrossRef] [PubMed]
- Crosby, D.A.; Murphy, M.M.; Segurado, R.; Byrne, F.; Mahony, R.; Robson, M.; McAuliffe, F.M. Cesarean delivery rates using Robson classification system in Ireland: What can we learn? Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 236, 121–126. [Google Scholar] [CrossRef]
- Rydahl, E.; Eriksen, L.; Juhl, M. Effects of induction of labor prior to post-term in low-risk pregnancies: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2019, 17, 170–208. [Google Scholar] [CrossRef]
- Grobman, W.A.; Rice, M.M.; Reddy, U.M.; Tita, A.T.N.; Silver, R.M.; Mallett, G.; Hill, K.; Thom, E.A.; El-Sayed, Y.Y.; Perez-Delboy, A.; et al. Labor induction versus expectant management in low-risk nulliparous women. N. Engl. J. Med. 2018, 379, 513–523. [Google Scholar] [CrossRef]
- Brennan, D.J.; Robson, M.S.; Murphy, M.; O’Herlihy, C. Comparative analysis of international cesarean delivery rates using 10-group classification identifies significant variation in spontaneous labor. Am. J. Obstet. Gynecol. 2009, 201, 308-e1–308.e8. [Google Scholar] [CrossRef]
- Roberge, S.; Dubé, E.; Blouin, S.; Chaillet, N. Reporting Caesarean Delivery in Quebec Using the Robson Classification System. J. Obstet. Gynaecol. Canada 2017, 39, 152–156. [Google Scholar] [CrossRef]
- RCOG Birth After Previous Caesarean Birth. Available online: https://www.rcog.org.uk/globalassets/documents/guidelines/gtg_45.pdf (accessed on 16 March 2019).
- Hehir, M.P.; Ananth, C.V.; Siddiq, Z.; Flood, K.; Friedman, A.M.; D’Alton, M.E. Cesarean delivery in the United States 2005 through 2014: A population-based analysis using the Robson 10-Group Classification System. Am. J. Obstet. Gynecol. 2018, 219, 105-e1–105.e11. [Google Scholar] [CrossRef]
- Zeitlin, J.; Szamotulska, K.; Drewniak, N.; Mohangoo, A.D.; Chalmers, J.; Sakkeus, L.; Irgens, L.; Gatt, M.; Gissler, M.; Blondel, B. Preterm birth time trends in Europe: A study of 19 countries. BJOG Int. J. Obstet. Gynaecol. 2013, 120, 1356–1365. [Google Scholar] [CrossRef]
- Robson, M.S. Classification of caesarean sections. Fetal Matern. Med. Rev. 2001, 12, 23–39. [Google Scholar] [CrossRef]
- Souza, J.P.; Betran, A.P.; Dumont, A.; De Mucio, B.; Gibbs Pickens, C.M.; Deneux-Tharaux, C.; Ortiz-Panozo, E.; Sullivan, E.; Ota, E.; Togoobaatar, G.; et al. A global reference for caesarean section rates (C-Model): A multicountry cross-sectional study. BJOG Int. J. Obstet. Gynaecol. 2016, 123, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Seijmonsbergen-Schermers, A.; De Jonge, A.; Van Den Akker, T.; Beeckman, K.; Bogaerts, A.; Barros, M.; Janssen, P.; Binfa, L.; Rydahl, E.; Frith, L.; et al. Variations in childbirth interventions in high-income countries: Protocol for a multinational cross-sectional study. BMJ Open 2018, 8, e017993. [Google Scholar] [CrossRef]
- The Lancet Stemming the global caesarean section epidemic. Lancet 2018, 392, 1279. [CrossRef]
- Renfrew, M.J.; McFadden, A.; Bastos, M.H.; Campbell, J.; Channon, A.A.; Cheung, N.F.; Silva, D.R.A.D.; Downe, S.; Kennedy, H.P.; Malata, A.; et al. Midwifery and quality care: Findings from a new evidence-informed framework for maternal and newborn care. Lancet 2014, 384, 1129–1145. [Google Scholar] [CrossRef]
- Sandall, J.; Soltani, H.; Gates, S.; Shennan, A.; Devane, D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst. Rev. 2016, 4, CD004667. [Google Scholar] [CrossRef]
- Betrán, A.P.; Temmerman, M.; Kingdon, C.; Mohiddin, A.; Opiyo, N.; Torloni, M.R.; Zhang, J.; Musana, O.; Wanyonyi, S.Z.; Gülmezoglu, A.M.; et al. Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet 2018, 392, 1358–1368. [Google Scholar] [CrossRef]
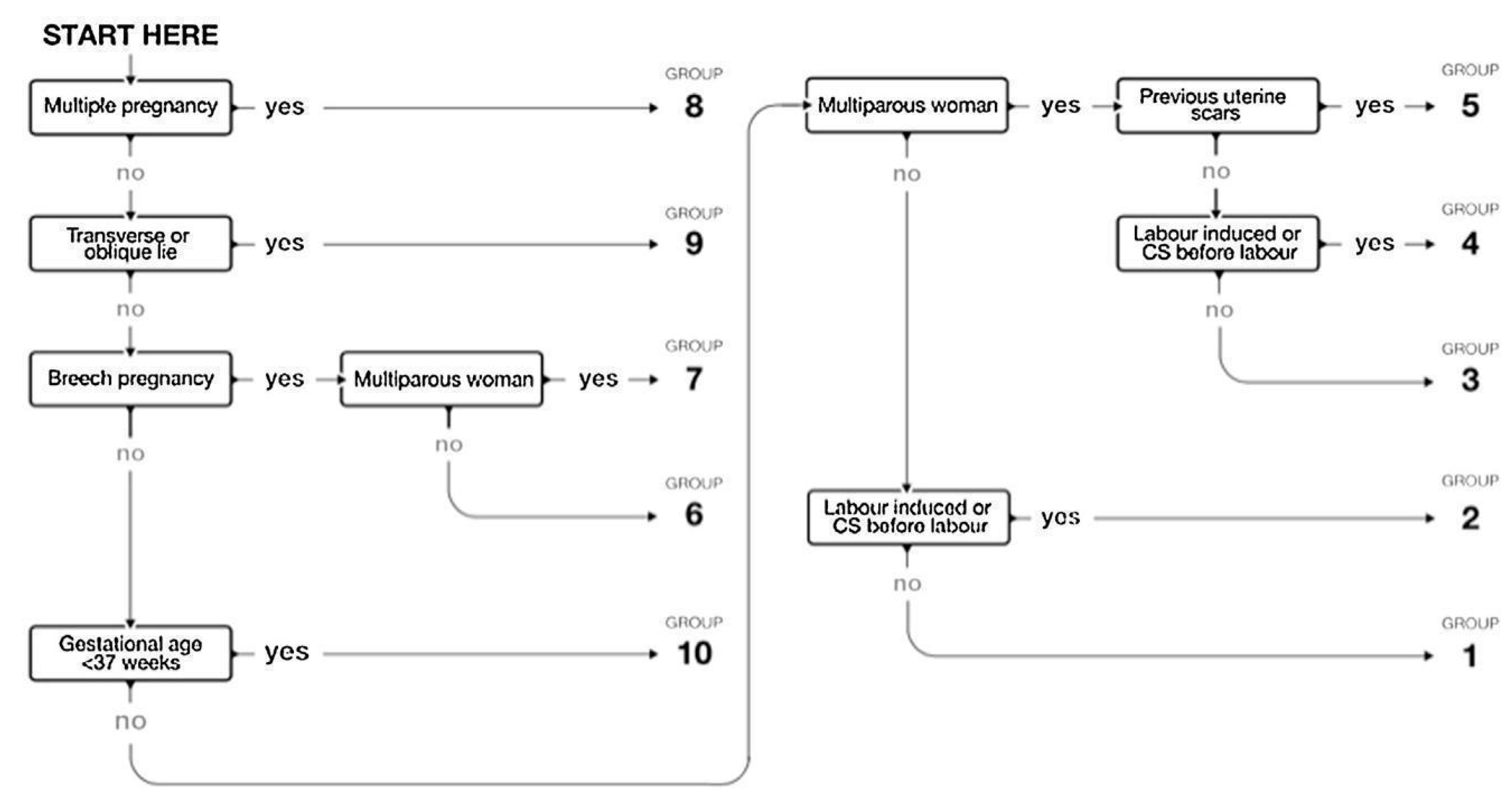
| 1 Nulliparous, singleton cephalic, ≥37 weeks, spontaneous labor. 2a Nulliparous, singleton cephalic, ≥37 weeks, induced labor. 2b Nulliparous, singleton cephalic, ≥37 weeks, or caesarean delivery before labor. 3 Multiparous, singleton cephalic, ≥37 weeks, spontaneous labor. 4a Multiparous, singleton cephalic, ≥37 weeks, induced labor. 4b Multiparous, singleton cephalic, ≥37 weeks, caesarean delivery before labor. 5 Previous caesarean delivery, singleton cephalic, ≥37 weeks, spontaneous labor or induced labor or caesarean delivery before labor. 6 All nulliparous singleton breeches, spontaneous labor or induced labor or caesarean delivery before labor. 7 All multiparous singleton breeches (including previous caesarean delivery), spontaneous labor or induced labor or caesarean delivery before labor. 8 All multiple pregnancies, spontaneous labor or induced labor or caesarean delivery before labor. 9 All abnormal singleton lies (including previous caesarean delivery but excluding breech), spontaneous labor or induced labor or caesarean delivery before labor. 10 All singleton cephalic, ≤36 weeks (including previous caesarean delivery), spontaneous labor or induced labor or caesarean delivery before labor. |
| University Hospital of la Ribera | Period: January 2010 to December 2018 | |||||
|---|---|---|---|---|---|---|
| Group | Total Number of CS in Each Group | Total Number of Women in Each Group | Group Size | Group CS Rate | Absolute Group Contribution to Overall CS Rate | Relative Contribution of the Group to Overall CS Rate |
| 1 | 638 | 5529 | 33.5% | 11.5% | 3.9% | 20.4% |
| 2 | 921 | 2527 | 15.3% | 36.4% | 5.6% | 29.4% |
| 2a | 768 | 2374 | 14.4% | 32.4% | 4.7% | 24.5% |
| 2b | 153 | 153 | 0.9% | 100.0% | 0.9% | 4.9% |
| 3 | 338 | 5283 | 32.0% | 6.4% | 2.0% | 10.8% |
| 4 | 402 | 1578 | 9.6% | 25.5% | 2.4% | 12.8% |
| 4a | 290 | 1466 | 8.9% | 19.8% | 1.8% | 9.3% |
| 4b | 112 | 112 | 0.7% | 100.0% | 0.7% | 3.6% |
| 5 | 23 | 118 | 0.7% | 19.5% | 0.1% | 0.7% |
| 6 | 304 | 320 | 1.9% | 95.0% | 1.8% | 9.7% |
| 7 | 136 | 158 | 1.0% | 86.1% | 0.8% | 4.3% |
| 8 | 133 | 229 | 1.4% | 82.1% | 0.8% | 4.2% |
| 9 | 35 | 35 | 0.2% | 100.0% | 0.2% | 1.1% |
| 10 | 222 | 729 | 4.4% | 27.7% | 1.2% | 6.4% |
| Total | 3132 | 16,506 | 100.0% | 19.0% | 19.0% | 100.0% |
| Group | Change in Overall % Per Year | 95% CI | p-Value |
|---|---|---|---|
| 1 | −0.56 | −0.58, −0.55 | 0.001 |
| 2 | 1.50 | 1.48–1.53 | 0.001 |
| 3 | −0.72 | −0.74, −0.71 | 0.001 |
| 4 | −0.69 | −0.71, −0.66 | 0.001 |
| 5 | −0.81 | −1.13, −0.50 | 0.001 |
| 6 | 0.12 | 0.11–0.22 | 0.031 |
| 7 | −0.19 | −0.25, −0.13 | 0.001 |
| 8 | −0.24 | −0.31, −0.17 | 0.001 |
| 9 | 0.87 | 0.24–0.97 | 0.269 |
| 10 | 0.24 | 0.21–0.27 | 0.001 |
| Induction of Labor Indication | Group (n = 3840) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2a (n = 2374) | 4a (n = 1466) | ||||||||||
| CS (n = 768) | Vaginal (n = 1606) | CS (n = 290) | Vaginal (n = 1176) | ||||||||
| n | % Total Row | n | % col | n | % col | n | % col | n | % col | p-Value | |
| Anomalies on the CTG | 193 | 5.0% | 63 | 8.2% | 54 | 3.4% | 23 | 7.9% | 53 | 4.5% | 0.001 |
| Prolonged pregnancy | 812 | 21.1% | 177 | 23.0% | 341 | 21.2% | 57 | 19.7% | 237 | 20.2% | <0.001 |
| Polyhydramnios | 72 | 1.9% | 17 | 2.2% | 19 | 1.2% | 10 | 3.4% | 26 | 2.2% | 0.088 |
| Pregnancy-induced hypertension | 189 | 4.9% | 68 | 8.8% | 66 | 4.1% | 16 | 5.5% | 39 | 3.3% | 0.007 |
| Antepartum hemorrhage in the 3rd trimester | 16 | 0.4% | 2 | 0.3% | 12 | 0.7% | 1 | 0.3% | 1 | 0.1% | 0.226 |
| Not recorded | 303 | 7.9% | 26 | 3.4% | 133 | 8.3% | 13 | 4.5% | 131 | 11.1% | 0.057 |
| Oligohydramnios | 305 | 7.9% | 69 | 9.0% | 130 | 8.1% | 19 | 6.6% | 87 | 7.4% | 0.002 |
| Fetal pathology | 4 | 0.1% | 3 | 0.4% | 0 | 0,0% | 0 | 0.0% | 1 | 0.1% | 0.046 |
| Maternal pathology | 52 | 1.4% | 6 | 0.8% | 20 | 1.2% | 4 | 1.4% | 22 | 1.9% | 0.482 |
| Anhydramnios | 22 | 0.6% | 0 | 0,0% | 15 | 0.9% | 0 | 0.0% | 7 | 0.6% | - |
| Favorable cervix | 145 | 3.8% | 14 | 1.8% | 57 | 3.5% | 8 | 2.8% | 66 | 5.6% | 0.135 |
| Small for gestational age | 113 | 2.9% | 21 | 2.7% | 59 | 3.7% | 7 | 2.4% | 26 | 2.2% | 0.573 |
| Latent phase | 14 | 0.4% | 3 | 0.4% | 5 | 0.3% | 1 | 0.3% | 5 | 0.4% | 0.393 |
| PROM not described | 355 | 9.2% | 55 | 7.2% | 164 | 10.2% | 28 | 9.7% | 108 | 9.2% | 0.327 |
| PROM < 12H | 14 | 0.4% | 2 | 0.3% | 6 | 0.4% | 0 | 0.0% | 6 | 0.5% | 0.186 |
| PROM > 12H < 18H | 127 | 3.3% | 23 | 3.0% | 46 | 2.9% | 8 | 2.8% | 50 | 4.3% | 0.011 |
| PROM > 18H < 24H | 131 | 3.4% | 20 | 2.6% | 62 | 3.9% | 9 | 3.1% | 40 | 3.4% | 0.422 |
| PROM > 24H | 390 | 10.2% | 83 | 10.8% | 178 | 11.1% | 31 | 10.7% | 98 | 8.3% | 0.112 |
| Meconium stained liquor | 272 | 7.1% | 48 | 6.3% | 110 | 6.8% | 24 | 8.3% | 90 | 7.7% | 0.085 |
| Suspected macrosomia | 62 | 1.6% | 10 | 1.3% | 22 | 1.4% | 7 | 2.4% | 23 | 2.0% | 0.485 |
| Intrauterine growth restriction | 153 | 4.0% | 34 | 4.4% | 69 | 4.3% | 15 | 5.2% | 35 | 3.0% | 0.708 |
| Gestational diabetes | 79 | 2.1% | 21 | 2.7% | 30 | 1.9% | 7 | 2.4% | 21 | 1.8% | 0.150 |
| Abnormal dopplers | 17 | 0.4% | 3 | 0.4% | 8 | 0.5% | 2 | 0.7% | 4 | 0.3% | 0.793 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vila-Candel, R.; Martín, A.; Escuriet, R.; Castro-Sánchez, E.; Soriano-Vidal, F.J. Analysis of Caesarean Section Rates Using the Robson Classification System at a University Hospital in Spain. Int. J. Environ. Res. Public Health 2020, 17, 1575. https://doi.org/10.3390/ijerph17051575
Vila-Candel R, Martín A, Escuriet R, Castro-Sánchez E, Soriano-Vidal FJ. Analysis of Caesarean Section Rates Using the Robson Classification System at a University Hospital in Spain. International Journal of Environmental Research and Public Health. 2020; 17(5):1575. https://doi.org/10.3390/ijerph17051575
Chicago/Turabian StyleVila-Candel, Rafael, Anna Martín, Ramón Escuriet, Enrique Castro-Sánchez, and Francisco Javier Soriano-Vidal. 2020. "Analysis of Caesarean Section Rates Using the Robson Classification System at a University Hospital in Spain" International Journal of Environmental Research and Public Health 17, no. 5: 1575. https://doi.org/10.3390/ijerph17051575
APA StyleVila-Candel, R., Martín, A., Escuriet, R., Castro-Sánchez, E., & Soriano-Vidal, F. J. (2020). Analysis of Caesarean Section Rates Using the Robson Classification System at a University Hospital in Spain. International Journal of Environmental Research and Public Health, 17(5), 1575. https://doi.org/10.3390/ijerph17051575









