Psychophysical Health Factors and Its Correlations in Elderly Wheelchair Users Who Live in Nursing Homes
Abstract
:1. Introduction
2. Materials and Methods
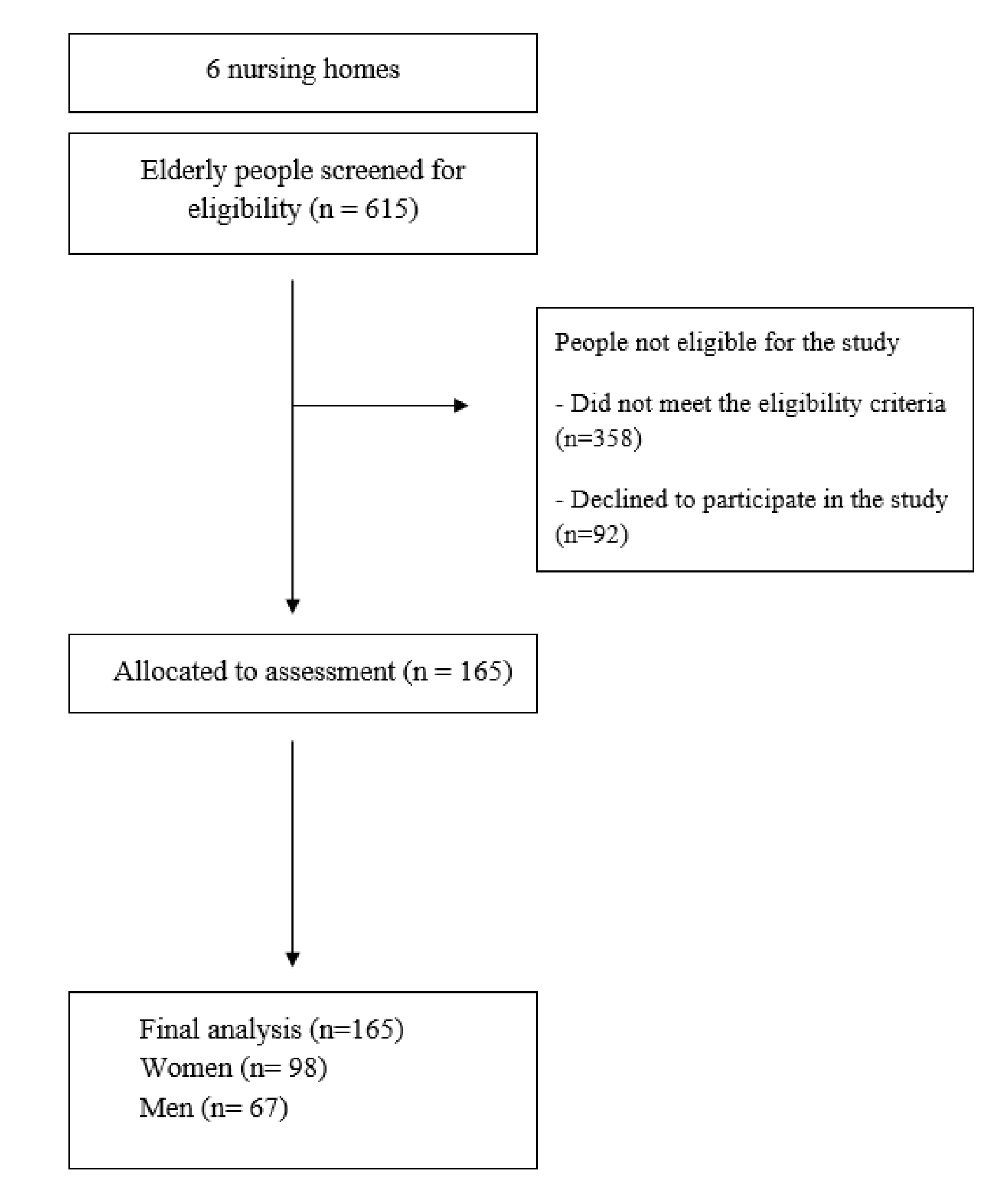
2.1. Study Participants
2.2. Sample Size
2.3. Research Procedure
2.3.1. Cognitive Functioning
2.3.2. Depression
2.3.3. Daily Functioning
2.3.4. Body Balance Assessment
2.3.5. Body Flexibility
2.3.6. Muscle Strength and Endurance
2.3.7. Joint Mobility
2.3.8. Manual Dexterity of the Upper Limb
2.3.9. Lung Capacity (PEF, FEV1)
2.4. Statistical Analysis
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Availability of Data and Materials
Ethics Approval and Consent to Participate
References
- The 2017 Revision Key Findings and Advance Tables. Available online: https://esa.un.org/unpd/wpp/Publications (accessed on 24 November 2019).
- Ministry of Family, Labour and Social Policy of the Republic of Poland. Available online: http://senior.gov.pl/materialy_i_badania/pokaz/399 (accessed on 25 November 2019).
- Statistics Poland. Available online: https://stat.gov.pl/obszary-tematyczne/warunki-zycia/ubostwo-pomoc-spoleczna/zaklady-stacjonarne-pomocy-spolecznej-w-2017-roku,18,2.html (accessed on 25 November 2019).
- Stineman, M.G.; Streim, J.E.; Pan, Q.; Kurichi, J.E.; Rose, S.M.; Xie, D. Establishing an Approach to Activity of Daily Living and Instrumental Activity of Daily Living Staging in the United States Adult Community-Dwelling Medicare Population. PM&R 2014, 6, 976–987. [Google Scholar]
- Myck, M.; Najsztub, M.; Oczkowska, M.; Chłoń-Domińczak, A.; Lewandowski, P.; Magda, I.; Morawski, L.; Paukszteło, W. Dane SHARE z perspektywy oceny jakości życia: Osoby w wieku 50+ w Polsce na tle Europy. In Pokolenie 50+ w Polsce na tle Europy: Aktywność, Zdrowie i jakość życia: Wyniki na Podstawie Badania SHARE; Myck, M., Oczkowska, M., Eds.; Ministerstwo Rodziny, Pracy i Polityki Społecznej: Warszawa, Poland, 2017; pp. 14–40. [Google Scholar]
- Murrock, C.J.; Graor, C.H.; Sues-Mitzel, A. Effects of dance on upper extremity activities in underserved adults. J. Am. Assoc. Nurse Pract. 2015, 10, 584–590. [Google Scholar] [CrossRef] [PubMed]
- Kingston, A.; Collerton, J.; Davies, K.; Bond, J.; Robinson, L.; Jagger, C. Losing the Ability in Activities of Daily Living in the Oldest Old: A Hierarchic Disability Scale from the Newcastle 85+ Study. PLoS ONE 2012, 7, e31665. [Google Scholar] [CrossRef] [PubMed]
- Bendayan, R.; Cooper, R.; Wloch, E.G.; Hofer, S.M.; Piccinin, A.M.; Muniz-Terrera, G. Hierarchy and Speed of Loss in Physical Functioning: A Comparison Across Older U.S. and English Men and Women. J. Gerontol. A Biomed. Sci. Med. Sci. 2017, 72, 1117–1122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wloch, E.G.; Kuh, D.; Cooper, R. Is the Hierarchy of Loss in Functional Ability Evident in Midlife? Findings from a British Birth Cohort. PLoS ONE 2016, 11, e0155815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vermeulen, J.; Neyens, J.C.; van Rossum, E.; Spreeuwenberg, M.D.; de Witte, L.P. Predicting ADL disability in community-dwelling elderly people using physical frailty indicators: A systematic review. BMC Geriatr. 2011, 11, 33. [Google Scholar] [CrossRef] [Green Version]
- Karmarkar, A.M.; Diciann, B.E.; Cooper, R.; Collins, D.M.; Matthews, J.T.; Koontz, A.; Teodorski, E.E.; Cooper, A. Demographic Profile of Older Adults Using Wheeled Mobility Devices. J. Aging Res. 2011, 2011, 560358. [Google Scholar] [CrossRef] [Green Version]
- Gell, N.M.; Wallace, R.B.; LaCroix, A.Z.; Mroz, T.M. Mobility device use in older adults and incidence of falls and worry about falling: Findings from the 2011–2012 national health and aging trends study. J. Am. Geriatr. Soc. 2015, 63, 853–859. [Google Scholar] [CrossRef]
- Chen, K.M.; Li, C.H.; Chang, Y.H.; Huang, H.T.; Cheng, Y.Y. An elastic band exercise program for older adults using wheelchairs in Taiwan nursing homes: A cluster randomized trial. Int. J. Nurs. Stud. 2015, 52, 30–38. [Google Scholar] [CrossRef]
- Jongenelis, K.; Pot, A.M.; Eisses, A.M.; Beekman, A.T.; Kluiter, H.; Ribbe, M.W. Prevalence and risk indicators of depression in elderly nursing home patients: The AGED study. J. Affect. Disord. 2004, 83, 135–142. [Google Scholar] [CrossRef]
- Chen, K.M.; Huang, H.T.; Cheng, Y.Y.; Li, C.H.; Chang, Y.H. Sleep quality and depression of nursing home older adults in wheelchairs after exercises. Nurs. Outlook 2015, 63, 357–365. [Google Scholar] [CrossRef] [PubMed]
- Jonker, C.; Geerlings, M.I.; Schmand, B. Are memory complaints predictive for dementia? A review of clinical and population-based studies. Int. J. Geriatr. Psychiatry 2000, 15, 983–991. [Google Scholar] [CrossRef]
- Drageset, J.; Eide, G.E.; Ranhoff, A.H. Depression is associated with poor functioning in activities of daily living among nursing home residents without cognitive impairment. J. Clin. Nurs. 2011, 20, 3111–3118. [Google Scholar] [CrossRef] [PubMed]
- Murphy, R.A.; Hagaman, A.K.; Reinders, I.; Steeves, J.A.; Newman, A.B.; Rubin, S.M.; Satterfield, S.; Kritchevsky, S.B.; Yaffe, K.; Ayonayon, H.N.; et al. Depressive Trajectories and Risk of Disability and Mortality in Older Adults: Longitudinal Findings from the Health, Aging, and Body Composition Study. J. Gerontol. A Biomed. Sci. Med. Sci. 2016, 71, 228–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakamura, T.; Michikawa, T.; Imamura, H.; Takebayashi, T.; Nishiwaki, Y. Relationship Between Depressive Symptoms and Activity of Daily Living Dependence in Older Japanese: The Kurabuchi Study. J. Am. Geriatr. Soc. 2017, 65, 2639–2645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chung, S. Residential status and depression among Korean elderly people: A comparison between residents of nursing home and those based in the community. Health Soc. Care Community 2008, 16, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Conradsson, M.; Littbrand, H.; Boström, G.; Lindelöf, N.; Gustafson, Y.; Rosendahl, E. Is a change in functional capacity or dependency in activities of daily living associated with a change in mental health among older people living in residential care facilities? Clin. Interv. Aging 2013, 8, 1561–1568. [Google Scholar] [CrossRef] [Green Version]
- Makizako, H.; Shimada, H.; Doi, T.; Tsutsumimoto, K.; Lee, S.; Hotta, R.; Nakakubo, S.; Harada, K.; Lee, S.; Bae, S.; et al. Cognitive Functioning and Walking Speed in Older Adults as Predictors of Limitations in Self-Reported Instrumental Activity of Daily Living: Prospective Findings from the Obu Study of Health Promotion for the Elderly. Int. J. Environ. Res. Public Health 2015, 12, 3002–3013. [Google Scholar] [CrossRef] [Green Version]
- Kotagal, V.; Langa, K.M.; Plassman, B.L.; Fisher, G.G.; Giordani, B.J.; Wallace, R.B.; Burke, J.R.; Steffens, D.C.; Kabeto, M.; Albin, R.L.; et al. Factors associated with cognitive evaluations in the United States. Neurology 2015, 84, 64–71. [Google Scholar] [CrossRef] [Green Version]
- Kelaiditi, E.; Cesari, M.; Canevelli, M.; van Kan, G.A.; Ousset, P.J.; Gillette-Guyonnet, S.; Ritz, P.; Duveau, F.; Soto, M.E.; Provencher, V.; et al. Cognitive frailty: Rational and definition from an (I.A.N.A./I.A.G.G.) international consensus group. J. Nutr. Health Aging 2013, 17, 726–734. [Google Scholar] [CrossRef]
- Mitnitski, A.; Fallah, N.; Rockwood, M.R.; Rockwood, K. Transitions in cognitive status in relation to frailty in older adults: A comparison of three frailty measures. J. Nutr. Health Aging 2011, 15, 863–867. [Google Scholar] [CrossRef] [PubMed]
- Raji, M.A.; Al Snih, S.; Ostir, G.V.; Markides, K.S.; Ottenbacher, K.J. Cognitive status and future risk of frailty in older Mexican Americans. J. Gerontol. A Biomed. Sci. Med. Sci. 2010, 65, 1228–1234. [Google Scholar] [CrossRef] [PubMed]
- Boyle, P.A.; Buchman, A.S.; Wilson, R.S.; Leurgans, S.E.; Bennett, D.A. Physical frailty is associated with incident mild cognitive impairment in community-based older persons. J. Am. Geriatr. Soc. 2010, 58, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Auyeung, T.W.; Lee, J.S.; Kwok, T.; Woo, J. Physical frailty predicts future cognitive decline—A four-year prospective study in 2737 cognitively normal older adults. J. Nutr. Health Aging 2011, 15, 690–694. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state” A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Albiński, R.; Kleszczewska-Albińska, A.; Bedyńska, S. Geriatryczna Skala Depresji (GDS). Trafność i rzetelność różnych wersji tego narzędzia - przegląd badań. Psychiatr. Pol. 2011, 45, 555–562. [Google Scholar]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index. Md. State. Med. J. 1965, 14, 61–65. [Google Scholar]
- Liu, T.W.; Ng, G.Y.F.; Ng, S.S.M. Effectiveness of a combination of cognitive behavioral therapy and task-oriented balance training in reducing the fear of falling in patients with chronic stroke: Study protocol for a randomized controlled trial. Trials 2018, 19, 168. [Google Scholar] [CrossRef] [Green Version]
- Jones, C.J.; Rikli, R.E. Measuring functional fitness of older adults. J. Act. Aging 2002, 3, 24–30. [Google Scholar]
- Trampisch, U.S.; Franke, J.; Jedamzik, N.; Hinrichs, T.; Platen, P. Optimal Jamar dynamometer handle position to assess maximal isometric hand grip strength in epidemiological studies. J. Hand. Surg. Am. 2012, 37, 2368–2373. [Google Scholar] [CrossRef]
- van Bladel, A.; Lambrecht, G.; Oostra, K.M.; Vanderstraeten, G.; Cambier, D.A. randomized controlled trial on the immediate and long-term effects of arm slings on shoulder subluxation in stroke patients. Eur. J. Phys. Rehabil. Med. 2017, 53, 400–409. [Google Scholar] [PubMed]
- Platz, T.; Pinkowski, C.; van Wijck, F.; Kimm, I.H.; di Bella, P.; Johnson, G. Reliability and validity of arm function assessment with standardized guidelines for the Fugl-Meyer Test, Action Research Arm Test and Box and Block Test: A multicentre study. Clin. Rehabil. 2005, 19, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Crittenden, C.N.; Pressman, S.D.; Cohen, S.; Janicki-Deverts, D.; Smith, B.W.; Seeman, T.E. Social integration and pulmonary function in the elderly. Health Psychol. 2014, 33, 535–543. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kvæl, L.A.H.; Bergland, A.; Telenius, E.W. Associations between physical function and depression in nursing home residents with mild and moderate dementia: A cross-sectional study. BMJ Open 2017, 7, e016875. [Google Scholar] [CrossRef] [Green Version]
- Fukukawa, Y.; Nakashima, C.; Tsuboi, S.; Kozakai, R.; Doyo, W.; Niino, N.; Ando, F.; Shimokata, H. Age differences in the effect of physical activity on depressive symptoms. Psychol. Aging 2004, 19, 346–351. [Google Scholar] [CrossRef] [Green Version]
- Ćwirlej-Sozańska, A.; Wilmowska-Pietruszyńska, A.; Sozański, B.; Wiśniowska-Szurlej, A. Analysis of Chronic Illnesses and Disability in a Community-Based Sample of Elderly People in South-Eastern Poland. Med. Sci. Monit. 2018, 24, 1387–1396. [Google Scholar] [CrossRef]
- Sung, K. The effects of 16-week group exercise program on physical function and mental health of elderly Korean women in long-term assisted living facility. J. Cardiovasc. Nurs. 2009, 24, 344–351. [Google Scholar] [CrossRef]
- Welmer, A.K.; Kåreholt, I.; Angleman, S.; Rydwik, E.; Fratiglioni, L. Can chronic multimorbidity explain the age-related differences in strength, speed and balance in older adults? Aging Clin. Exp. Res. 2012, 24, 480–489. [Google Scholar]
- Chang, C.L.; Chen, K.M. Physical and mental health status and their correlations among older wheelchair users with dementia in long-term care facilities. Qual. Life Res. 2018, 27, 793–800. [Google Scholar] [CrossRef]
- Van Ness, P.H.; MacNeil Vroomen, J.; Leo-Summers, L.; Vander Wyk, B.; Allore, H.G. Chronic Conditions, Medically Supportive Care Partners, And Functional Disability Among Cognitively Impaired Adults. Innov. Aging 2019, 3, 1–9. [Google Scholar] [CrossRef]
- Park, D.G.; Lee, S.; Moon, Y.M.; Na, D.L.; Jeong, J.H.; Park, K.W.; Lee, Y.H.; Lim, T.S.; Choi, S.H.; Moon, S.Y. Predictors of Institutionalization in Patients with Alzheimer’s Disease in South Korea. J. Clin. Neurol. 2018, 14, 191–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Snowden, M.B.; Steinman, L.E.; Bryant, L.L.; Cherrier, M.M.; Greenlund, K.J.; Leith, K.H.; Levy, C.; Logsdon, R.G.; Copeland, C.; Vogel, M.; et al. Dementia and co-occurring chronic conditions: A systematic literature review to identify what is known and where are the gaps in the evidence? Int. J. Geriatr. Psychiatry 2017, 32, 357–371. [Google Scholar] [CrossRef] [PubMed]
- Choi, N.G.; Sirey, J.A.; Bruce, M.L. Depression in Homebound Older Adults: Recent Advances in Screening and Psychosocial Interventions. Curr. Transl. Geriatr. Exp. Gerontol. Rep. 2013, 2, 16–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drageset, J.; Eide, G.E.; Ranhoff, A.H. Anxiety and depression among nursing home residents without cognitive impairment. Scand. J. Caring Sci. 2013, 27, 872–881. [Google Scholar] [CrossRef] [PubMed]
- Ćwirlej-Sozańska, A.; Sozański, B.; Wiśniowska-Szurlej, A.; Wilmowska-Pietruszyńska, A.; Kujawa, J. Assessment of Disability and Factors Determining Disability among Inhabitants of South-Eastern Poland Aged 71–80 Years. BioMed. Res. Int. 2018, 2018, 3872753. [Google Scholar] [CrossRef] [Green Version]
- Crimmins, E.M.; Kim, J.K.; Solé-Auró, A. Gender differences in health: Results from SHARE, ELSA and HRS. Eur. J. Public Health 2011, 21, 81–91. [Google Scholar] [CrossRef] [Green Version]
- Lane, N.E.; Stukel, T.A.; Boyd, C.M.; Wodchis, W.P. Long-Term Care Residents’ Geriatric Syndromes at Admission and Disablement Over Time: An Observational Cohort Study. J. Gerontol. A Biomed. Sci. Med. Sci. 2019, 74, 917–923. [Google Scholar] [CrossRef] [Green Version]
- Jerez-Roig, J.; de Brito Macedo Ferreira, L.M.; Torres de Araújo, J.R.; Costa Lima, K. Functional decline in nursing home residents: A prognostic study. PLoS ONE 2017, 12, e0177353. [Google Scholar] [CrossRef]
- Serrano-Urrea, R.; Gómez-Rubio, V.; Palacios-Ceña, D.; Fernández-de-Las-Peñas, C.; García-Meseguer, M.J. Individual and institutional factors associated with functional disability in nursing home residents: An observational study with multilevel analysis. PLoS ONE 2017, 12, e0183945. [Google Scholar] [CrossRef] [Green Version]
- Carlson, C.; Merel, S.E.; Yukawa, M. Geriatric syndromes and geriatric assessment for the generalist. Med. Clin. N. Am. 2015, 99, 263–279. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist 2013, 53, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Heiland, E.G.; Welmer, A.K.; Wang, R.; Santoni, G.; Angleman, S.; Fratiglioni, L.; Qiu, C. Association of mobility limitations with incident disability among older adults: A population-based study. Age Ageing 2016, 45, 812–819. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mortenson, W.B.; Miller, W.C.; Backman, C.L.; Oliffe, J.L. Association between mobility, participation, and wheelchair-related factors in long-term care residents who use wheelchairs as their primary means of mobility. J. Am. Geriatr. Soc. 2012, 60, 1310–1315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramnath, U.; Rauch, L.; Lambert, E.V.; Kolbe-Alexander, T.L. performance in physically active older adults: A pilot study. PLoS ONE 2018, 9, e0194918. [Google Scholar]
- Clouston, S.A.; Brewster, P.; Kuh, D.; Richards, M.; Cooper, R.; Hardy, R.; Rubin, M.S.; Hofer, S.M. The dynamic relationship between physical function and cognition in longitudinal aging cohorts. Epidemiol. Rev. 2013, 35, 33–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, Y.; Yang, M.; Yan, Y.; Wang, L.; Gong, J. Sex differentials in relationships between functional fitness and cognitive performance in older adults: A canonical correlation analysis. Sci. Rep. 2018, 7, 4146. [Google Scholar] [CrossRef]
- Arrieta, H.; Rezola-Pardo, C.; Echeverria, I.; Iturburu, M.; Gil, S.M.; Yanguas, J.J.; Irazusta, J.; Rodriguez-Larrad, A. Physical activity and fitness are associated with verbal memory, quality of life and depression among nursing home residents: Preliminary data of a randomized controlled trial. BMC Geriatr. 2018, 18, 80. [Google Scholar] [CrossRef] [Green Version]
- Jiang, J.; Tang, Z.; Futatsuka, M.; Zhang, K. Exploring the influence of depressive symptoms on physical disability: A cohort study of elderly in Beijing, China. Qual. Life Res. 2004, 13, 1337–1346. [Google Scholar] [CrossRef]
- Kaup, B.A.; Loreck, D.; Gruber-Baldini, A.L.; German, P.; Menon, A.S.; Zimmerman, S.; Burton, L.; Magaziner, J. Depression and its relationship to function and medical status, by dementia status, in nursing home admissions. Am. J. Geriatr. Psychiatry 2007, 15, 438–442. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Inouye, S.K.; Gill, T.M.; Doucette, J.T. Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes. JAMA 1995, 273, 1348–1353. [Google Scholar] [CrossRef]
- Konopack, J.F.; Marquez, D.X.; Hu, L.; Elavsky, S.; McAuley, E.; Kramer, A.F. Correlates of functional fitness in older adults. Int. J. Behav. Med. 2008, 15, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Alexandre, T.S.; Corona, L.P.; Nunes, D.P.; Santos, J.L.; Duarte, Y.A.; Lebrão, M.L. Gender differences in incidence and determinants of disability in activities of daily living among elderly individuals: SABE study. Arch. Gerontol. Geriatr. 2012, 55, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.T.; Liu, L.F.; Chen, C.K.; Hwang, S.J.; Chen, L.K.; Lu, F.H. Correlates of institutionalized senior veterans’ quality of life in Taiwan. Health Qual. Life Outcomes 2010, 8, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, M.; Sinacore, D.R.; Binder, E.F.; Kohrt, W.M. Physical and performance measures for the identification of mild to moderate frailty. J. Gerontol. A Biomed. Sci. Med. Sci. 2000, 55, 350–355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Foldvari, M.; Clark, M.; Laviolette, L.C.; Bernstein, M.A.; Kaliton, D.; Castaneda, C.; Pu, C.T.; Hausdorff, J.M.; Fielding, R.A.; Singh, M.A. Association of muscle power with functional status in community-dwelling elderly women. J. Gerontol. A Biomed. Sci. Med. Sci. 2000, 55, 192–199. [Google Scholar] [CrossRef]
- Kolanowski, A.; Buettner, L.; Litaker, M.; Yu, F. Factors that relate to activity engagement in nursing home residents. Am. J. Alzheimers Dis. Other Demen. 2006, 21, 15–22. [Google Scholar] [CrossRef]
- Wang, H.; Chen, K.; Pan, Y.; Jing, F.; Liu, H. Associations and Impact Factors between Living Arrangements and Functional Disability among Older Chinese Adults. PLoS ONE 2013, 8, e53879. [Google Scholar] [CrossRef]
- Berryman, N.; Bherer, L.; Nadeau, S.; Lauzière, S.; Lehr, L.; Bobeuf, F.; Kergoat, M.J.; Vu, T.T.; Bosquet, L. Executive functions, physical fitness and mobility in well-functioning older adults. Exp. Gerontol. 2013, 48, 1402–1409. [Google Scholar] [CrossRef]
- Lok, N.; Lok, S.; Canbaz, M. The effect of physical activity on depressive symptoms and quality of life among elderly nursing home residents: Randomized controlled trial. Arch. Gerontol. Geriatr. 2017, 70, 92–98. [Google Scholar] [CrossRef]
- Vankova, H.; Holmerova, I.; Machacova, K.; Volicer, L.; Veleta, P.; Celko, A.M. The effect of dance on depressive symptoms in nursing home residents. J. Am. Med. Dir. Assoc. 2014, 15, 582–587. [Google Scholar] [CrossRef]
- Chun, A.; Reinhardt, J.P.; Ramirez, M.; Ellis, J.M.; Silver, S.; Burack, O.; Eimicke, J.P.; Cimarolli, V.; Teresi, J.A. Depression recognition and capacity for self-report among ethnically diverse nursing homes residents: Evidence of disparities in screening. J. Clin. Nurs. 2017, 26, 4915–4926. [Google Scholar] [CrossRef]
- Carrière, I.; Gutierrez, L.A.; Pérès, K.; Berr, C.; Barberger-Gateau, P.; Ritchie, K.; Ancelin, M.L. Late life depression and incident activity limitations: Influence of gender and symptom severity. J. Affect. Disord. 2011, 133, 42–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, Y.; George, L.K. Functional disability, disability transitions, and depressive symptoms in late life. J. Aging Health 2005, 17, 263–292. [Google Scholar] [CrossRef]
- Ruscello, B.; D’Ottavio, S.; Padua, E.; Tonelli, C.; Pantanella, L. The influence of music on exercise in a group of sedentary elderly women: An important tool to help the elderly to stay active. J. Sports Med. Phys. Fit. 2014, 54, 536–544. [Google Scholar]
- Barbour, K.A.; Edenfield, T.M.; Blumenthal, J.A. Exercise as a treatment for depression and other psychiatric disorders: A review. J. Cardiopulm. Rehabil. Prev. 2007, 27, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Onder, G.; Penninx, B.W.; Ferrucci, L.; Fried, L.P.; Guralnik, J.M.; Pahor, M. Measures of physical performance and risk for progressive and catastrophic disability: Results from the Women’s Health and Aging Study. J. Gerontol. A Biomed. Sci. Med. Sci. 2005, 60, 74–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Legrand, D.; Vaes, B.; Matheï, C.; Adriaensen, W.; Van Pottelbergh, G.; Degryse, J.M. Muscle strength and physical performance as predictors of mortality, hospitalization, and disability in the oldest old. J. Am. Geriatr. Soc. 2014, 62, 1030–1038. [Google Scholar] [CrossRef]
| Variable | Total (n = 165) | Women (n = 98) | Men (n = 67) | p-Value | |
|---|---|---|---|---|---|
| Number (%) | |||||
| Sociodemographic and clinical | Mean (SD) | ||||
| Age | 74.35 (7.33) | 75.87 (7.03) | 72.12 (7.25) | 0.001 * | |
| BMI (kg/m2) | 27.02 (4.44) | 26.21 (4.40) | 28.21 (4.26) | 0.004 * | |
| Education | |||||
| Basic | 50 (30.3) | 29 (29.59) | 21 (31.34) | 0.171 | |
| Secondary | 99 (60.0) | 56 (57.14) | 43 (64.17) | ||
| Higher | 16 (9.7) | 13 (13.26) | 3 (4.48) | ||
| Marital status | |||||
| Married | 17 (10.3) | 9 (9.18) | 8 (11.94) | 0.007 * | |
| Widow/Widower | 73 (44.2) | 54 (55.10) | 19 (28.36) | ||
| Divorced | 28 (17.0) | 14 (14.29) | 14 (20.90) | ||
| Single | 47 (28.5) | 21 (21.43) | 26 (38.81) | ||
| Length of NH residency | |||||
| >12 moths | 14 (8.5) | 7 (10.45) | 7 (7.14) | 0.639 | |
| 1–5 years | 5 (27.3) | 19 (28.36) | 26 (26.53) | ||
| 6–10 years | 77 (46.7) | 32 (47.76) | 45 (45.92) | ||
| over 10 years | 29 (17.6) | 9 (13.43) | 20 (20.41) | ||
| Length of wheelchair dependence | |||||
| >12 months | 3 (1.8) | 2 (2.04) | 1 (1.49) | 0.891 | |
| 1–5 years | 76 (46.1) | 46 (46.94) | 30 (44.78) | ||
| 6–10 years | 72 (43.6) | 29 (43.28) | 43 (43.87) | ||
| over 10 years | 14 (8.5) | 7 (10.45) | 7 (7.14) | ||
| Chronic disease | |||||
| Cardiovascular | 117 (70.9) | 71 (72.45) | 46 (68.66) | 0.598 | |
| Pulmonary | 31 (18.8) | 19 (19.39) | 12 (17.91) | 0.811 | |
| Neurological | 113 (68.5) | 70 (71.43) | 43 (64.18) | 0.325 | |
| Urinary system | 42 (25.5) | 25 (25.51) | 17 (25.37) | 0.984 | |
| Digestive system | 25 (15.2) | 18 (18.37) | 7 (10.45) | 0.164 | |
| Muscoskeletal | 83 (50.3) | 49 (50.00) | 34 (50.75) | 0.925 | |
| Ophtamological | 58 (35.2) | 37 (37.76) | 21 (31.34) | 0.397 | |
| Otological | 52 (31.5) | 29 (29.59) | 23 (34.33) | 0.520 | |
| Dominant limb | |||||
| Right | 138 (83.6) | 81 (82.65) | 57 (85.07) | 0.680 | |
| Left | 27 (16.4) | 17 (17.35) | 10 (14.93) | 0.680 | |
| Mental status | |||||
| MMSE | 24.94 (3.37) | 24.70 (3.33) | 25.28 (3.42) | 0.265 | |
| Normal cognition | 59 (35.76) | 33 (33.67) | 26 (38.81) | 0.774 | |
| Cognitive impairment without dementia | 45 (27.27) | 27 (27.55) | 18 (26.87) | ||
| Moderate dementia | 61 (36.97) | 38 (38.76) | 23 (34.33) | ||
| GDS | 5.52 (2.72) | 5.67 (2.87) | 5.30 (2.49) | 0.269 | |
| No depression | 73 (44.24) | 40 (40.82) | 33 (49.25) | 0.284 | |
| Moderate depression | 92 (55.76) | 58 (59.18) | 34 (50.75) | ||
| Daily Functioning BI | 54.36 (11.78) | 52.74(11.11) | 56.72 (12.42) | 0.027 * | |
| Complete dependence | 0 | 0 | 0 | ||
| Severe dependence | 113 (68.48) | 75 (76.53) | 38 (56.72) | 0.007 * | |
| Moderate dependence | 52 (31.51) | 23 (23.47) | 29 (43.28) | ||
| Body balance | |||||
| BBS total | 15.52 (5.56) | 15.44 (5.53) | 15.63 (5.64) | 0.895 | |
| Body flexibility | |||||
| BS (cm) | −38.85 (22.84) | −37.64 (20.35) | −40.63 (25.43) | 0.550 | |
| CSR (cm) | −12.42 (19.54) | −10.86 (15.62) | −14.70 (21.82) | 0.459 | |
| Muscle strength and endurance | |||||
| ACT (repetitions) | 9.94 (5.33) | 8.94 (4.81) | 11.40 (5.73) | 0.005 * | |
| HGS (kg) | 17.18 (15.00) | 13.02 (6.35) | 23.28 (11.44) | <0.001 * | |
| Joint mobility | |||||
| Shoulder flexion (degree) | 131.13 (20.61) | 127.66(18.41) | 136.19 (22.67) | 0.007 * | |
| Shoulder extension (degree) | 43.95 (9.99) | 43.91 (10.26) | 44.01 (9.67) | 0.979 | |
| Shoulder abduction (degree) | 128.39 (23.14) | 125.32 (24.13) | 132.90 (20.98) | 0.057 | |
| Manual dexterity of the upper limb | |||||
| BBT | 26.89(11.15) | 24.65 (10.25) | 30.16 (11.66) | 0.002 * | |
| Lung capacity | |||||
| PEF l/min | 169.74 (69.06) | 150.22 (49.69) | 198.28 (82.64) | <0.001 * | |
| FEV1 0,01 l | 1.26 (0.59) | 1.06 (0.42) | 1.54 (0.70) | <0.001 * | |
| Variable | Cognitive Functioning | Depression | Daily Functioning | ||||||
|---|---|---|---|---|---|---|---|---|---|
| rho | rho | rho | |||||||
| Total (n = 165) | Women (n = 98) | Men (n = 67) | Total (n = 165) | Women (n = 98) | Men (n = 67) | Total (n = 165) | Women (n = 98) | Men (n = 67) | |
| BI | 0.263 ** | 0.136 | 0.377 ** | −0.408 ** | −0.443 ** | −0.357 ** | - | - | - |
| BBS | 0.298 ** | 0.281 ** | 0.311 * | −0.261 ** | −0.205 * | −0.353 ** | 0.450 ** | 0.352 ** | 0.583 ** |
| BP | 0.168 * | 0.140 | 0.231 | −0.115 | −0.027 | −0.269 * | 0.431 ** | 0.331 ** | 0.571 ** |
| CSR | 0.132 | 0.167 | 0.087 | −0.047 | −0.084 | 0.005 | 0.314 ** | 0.207 * | 0.477 ** |
| HGS | 0.256 ** | 0.203 * | 0.295 * | −0.087 | −0.150 | −0.031 | 0.393 ** | 0.315 ** | 0.382 ** |
| ACT | 0.259 ** | 0.211 * | 0.265 * | −0.318** | −0.353 ** | −0.181 | 0.316 ** | 0.269 ** | 0.275 * |
| Shoulder flexion | 0.278 ** | 0.179 | 0.384 ** | −0.189* | −0.163 | −0.132 | 0.395 ** | 0.240 * | 0.480 ** |
| Shoulder extension | 0.12 | 0.021 | 0.270 * | −0.10 | −0.106 | −0.089 | 0.310 ** | 0.342 ** | 0.276 * |
| Shoulder abduction | 0.221 ** | 0.228 * | 0.167 | −0.13 | −0.146 | −0.032 | 0.203 ** | 0.071 | 0.269 * |
| BBT | 0.282 ** | 0.225 * | 0.252 * | −0.237 ** | −0.224 * | −0.130 | 0.380 ** | 0.227 * | 0.435 ** |
| PEF l/min | 0.156 * | 0.056 | 0.261 * | −0.15 | −0.095 | −0.179 | 0.14 | 0.113 | 0.089 |
| FEV1(l) | 0.12 | 0.035 | 0.126 | −0.11 | −0.107 | −0.038 | 0.186 * | 0.091 | 0.211 |
| Variable | Cognitive Functioning | Depression | Daily Functioning | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R2 = 0.114, R2adj = 0.103, F = 10.383 | R2 = 0.191, R2adj = 0.181, F = 21.327 | R2 = 0.348, R2adj = 0.331, F = 19.161 | |||||||||||||
| β | B | (95 CI) | p-Value | β | B | (95 CI) | p-Value | β | B | (95 CI) | p-Value | ||||
| Constant | - | 18.14 | 14.84 | 21.44 | <0.001 | - | 10.82 | 9.02 | 12.63 | <0.001 | - | 32.56 | 20.29 | 44.84 | <0.001 |
| BI | - | - | - | - | - | 0.35 | 0.08 | 0.16 | 0.05 | <0.001 | - | - | - | - | - |
| BBS | 0.22 | 0.14 | 0.05 | 0.23 | 0.003 | - | - | - | - | - | 0.29 | 0.62 | 0.33 | 0.91 | <0.001 |
| BS | - | - | - | - | - | - | - | - | - | - | 0.22 | 0.11 | 0.04 | 0.19 | 0.003 |
| ACT | - | - | - | - | - | 0.18 | 0.09 | 0.17 | 0.02 | 0.018 | - | - | - | - | - |
| HGS | - | - | - | - | - | - | - | - | - | - | 0.17 | 0.20 | 0.04 | 0.37 | 0.018 |
| Shoulder flexion | 0.23 | 0.04 | 0.01 | 0.06 | 0.004 | - | - | - | - | - | 0.18 | 0.10 | 0.02 | 0.18 | 0.015 |
| Women | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Men | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wołoszyn, N.; Grzegorczyk, J.; Wiśniowska-Szurlej, A.; Kilian, J.; Kwolek, A. Psychophysical Health Factors and Its Correlations in Elderly Wheelchair Users Who Live in Nursing Homes. Int. J. Environ. Res. Public Health 2020, 17, 1706. https://doi.org/10.3390/ijerph17051706
Wołoszyn N, Grzegorczyk J, Wiśniowska-Szurlej A, Kilian J, Kwolek A. Psychophysical Health Factors and Its Correlations in Elderly Wheelchair Users Who Live in Nursing Homes. International Journal of Environmental Research and Public Health. 2020; 17(5):1706. https://doi.org/10.3390/ijerph17051706
Chicago/Turabian StyleWołoszyn, Natalia, Joanna Grzegorczyk, Agnieszka Wiśniowska-Szurlej, Justyna Kilian, and Andrzej Kwolek. 2020. "Psychophysical Health Factors and Its Correlations in Elderly Wheelchair Users Who Live in Nursing Homes" International Journal of Environmental Research and Public Health 17, no. 5: 1706. https://doi.org/10.3390/ijerph17051706





