Methods of Disinfecting Stethoscopes: Systematic Review
Abstract
1. Introduction
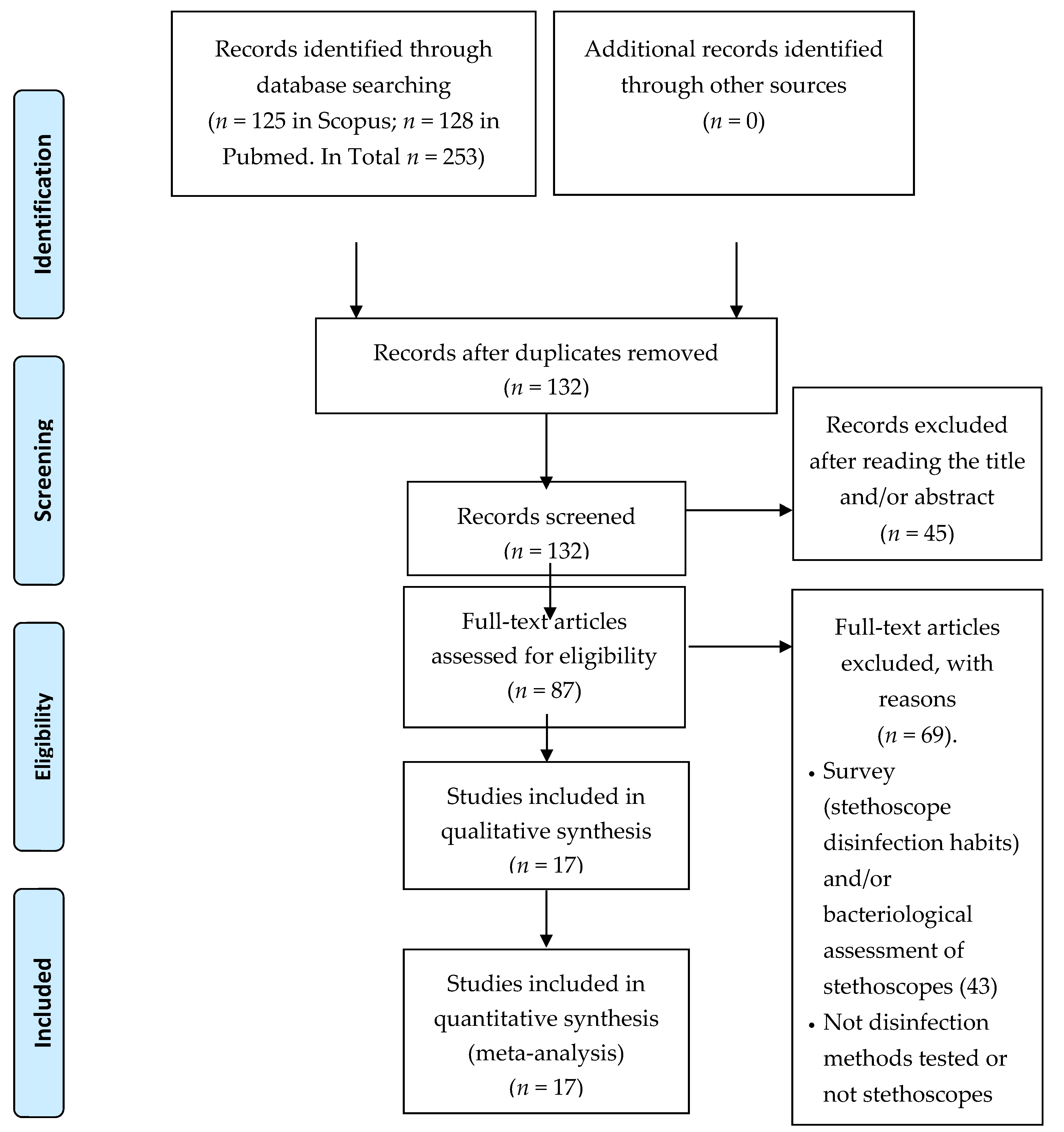
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wenzel, R.P.; Thompson, R.L.; Landry, S.M.; Russell, B.S.; Miller, P.J.; Ponce de Leon, S.; Miller, G.B., Jr. Hospital-acquired infections in intensive care unit patients: An overview with emphasis on epidemics. Infect. Control 1983, 4, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Sengupta, S.; Sirkar, A.; Shivananda, P.G. Stethoscopes and nosocomial infection. Indian J. Pediatri. 2000, 67, 197–199. [Google Scholar] [CrossRef] [PubMed]
- Messina, G.; Burgassi, S.; Messina, D.; Montagnani, V.; Cevenini, G. A new, U.V.-LED device for automatic disinfection of stethoscope membranes. Am. J. Infect. Control 2015, 43, e61–e66. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Report on the Burden of Endemic Health Care Associated Infection Worldwide. Available online: https://apps.who.int/iris/bitstream/handle/10665/80135/9789241501507_eng.pd;jsessionid=7F83155702C33EEC68AAA100F103E01B?sequence=1 (accessed on 7 February 2020).
- Messina, G.; Ceriale, E.; Lenzi, D.; Burgassi, S.; Azzolini, E.; Manzi, P. Environmental contaminants in hospital settings and progress in disinfecting techniques. BioMed Res. Int. 2013, 2013, 429780. [Google Scholar] [CrossRef] [PubMed]
- Messina, G.; Rosadini, D.; Burgassi, S.; Messina, D.; Nante, N.; Tani, M.; Cevenini, G. Tanning the bugs—A pilot study of an innovative approach to stethoscope disinfection. J. Hosp. Infect. 2017, 95, 228–230. [Google Scholar] [CrossRef] [PubMed]
- OߣFlaherty, N.; Fenelon, L. The stethoscope and healthcare-associated infection: A snake in the grass or innocent bystander? J. Hosp. Infect. 2015, 91, 1–7. [Google Scholar]
- Lee, Y.T.; Chen, S.C.; Lee, M.C.; Hung, H.C.; Huang, H.J.; Lin, H.C.; Wu, D.J.; Tsao, S.M. Time-series analysis of the relationship of antimicrobial use and hand hygiene promotion with the incidence of healthcare-associated infections. J. Antibiot. 2012, 65, 311–316. [Google Scholar] [CrossRef]
- Alvarez, J.A.; Ruiz, S.R.; Mosqueda, J.L.; Leon, X.; Arreguin, V.; Macias, A.E.; Macias, J.H. Decontamination of stethoscope membranes with chlorhexidine: Should it be recommended? Am. J. Infect. Control 2016, 44, e205–e209. [Google Scholar] [CrossRef]
- West, G.F.; Resendiz, M.; Lustik, M.B.; Nahid, M.A. Bacterial Contamination of Military and Civilian Uniforms in an Emergency Department. J. Emerg. Nurs. JEN Off. Publ. Emerg. Dep. Nurses Assoc. 2018, 45, 169–177.e1. [Google Scholar] [CrossRef]
- Marinella, M.A.; Pierson, C.; Chenoweth, C. The stethoscope. A potential source of nosocomial infection? Arch. Intern. Med. 1997, 157, 786–790. [Google Scholar] [CrossRef]
- Ghumman, G.W.; Ahmad, N.; Pop-Vicas, A.; Iftikhar, S. Stethoscope Cleaning During Patient Care. Rhode Isl. Med J. 2018, 101, 18–20. [Google Scholar]
- Raghubanshi, B.R.; Sapkota, S.; Adhikari, A.; Dutta, A.; Bhattarai, U.; Bhandari, R. Use of 90% ethanol to decontaminate stethoscopes in resource limited settings. Antimicrob. Resist. Infect. Control 2017, 6, 68. [Google Scholar] [CrossRef] [PubMed]
- Rutala, W.A.; Weinsten, R.A. The Healthcare Infection Control Practices Advisory Committee (HICPAC). Guideline for Disinfection and Sterilization in Healthcare Facilities. 2008. Available online: https://www.cdc.gov/infectioncontrol/pdf/guidelines/disinfection-guidelines.pdf (accessed on 13 September 2017).
- Boulee, D.; Kalra, S.; Haddock, A.; Johnson, T.D.; Peacock, W.F. Contemporary stethoscope cleaning practices: What we haven’t learned in 150 years. Am. J. Infect. Control 2019, 47, 238–242. [Google Scholar] [CrossRef] [PubMed]
- JBI Critical Appraisal Tools. Joanna Briggs Institute. Available online: https://joannabriggs.org/ebp/critical_appraisal_tools (accessed on 27 February 2020).
- Schmidt, M.G.; Tuuri, R.E.; Dharsee, A.; Attaway, H.H.; Fairey, S.E.; Borg, K.T.; Salgado, C.D.; Hirsch, B.E. Antimicrobial copper alloys decreased bacteria on stethoscope surfaces. Am. J. Infect. Control 2017, 45, 642–647. [Google Scholar] [CrossRef]
- Grandiere-Perez, L.; Bovet, J.; Beaudron, A.; Saulnier, P.; Blanchi, S.; Delemotte, M.; Ramanantsoa, C. Efficacy of an ethanol-based hand sanitizer for disinfection of stethoscopes. J. Hosp. Infect. 2015, 91, 183–184. [Google Scholar] [CrossRef]
- Mehta, A.K.; Halvosa, J.S.; Gould, C.V.; Steinberg, J.P. Efficacy of alcohol-based hand rubs in the disinfection of stethoscopes. Infect. Control Hosp. Epidemiol. 2010, 31, 870–872. [Google Scholar] [CrossRef]
- Schroeder, A.; Schroeder, M.A.; D’Amico, F. What’s growing on your stethoscope? (And what you can do about it). J. Fam. Pract. 2009, 58, 404–409. [Google Scholar]
- Hill, C.; King, T.; Day, R. A strategy to reduce, M.R.SA colonization of stethoscopes. J. Hosp. Infect. 2006, 62, 122–123. [Google Scholar] [CrossRef]
- Leprat, R.; Minary, P.; Devaux, V.; de Waziere, B.; Dupond, J.L.; Talon, D. Why, when and how to clean stethoscopes. J. Hosp. Infect. 1998, 39, 80–82. [Google Scholar] [CrossRef]
- Messina, G.; Fattorini, M.; Nante, N.; Rosadini, D.; Serafini, A.; Tani, M.; Cevenini, G. Time Effectiveness of Ultraviolet C Light (UVC) Emitted by Light Emitting Diodes (LEDs) in Reducing Stethoscope Contamination. Int. J. Environ. Res. Public Health 2016, 13, 940. [Google Scholar] [CrossRef]
- Wood, M.W.; Lund, R.C.; Stevenson, K.B. Bacterial contamination of stethoscopes with antimicrobial diaphragm covers. Am. J. Infect. Control. 2007, 35, 263–266. [Google Scholar] [CrossRef] [PubMed]
- Messina, G.; Spataro, G.; Rosadini, D.; Burgassi, S.; Mariani, L.; Tani, M.; Cevenini, G. A novel approach to stethoscope hygiene: A coat-pocket innovation. Infect. Dis. Health. 2018, 23, 211–216. [Google Scholar] [CrossRef]
- Parmar, R.C.; Valvi, C.C.; Sira, P.; Kamat, J.R. A prospective, randomised, double-blind study of comparative efficacy of immediate versus daily cleaning of stethoscope using 66% ethyl alcohol. Indian J. Med. Sci. 2004, 58, 423–430. [Google Scholar] [PubMed]
- Datta, P.; Kaur, M.; Rawat, S.; Gupta, V.; Chander, J. Stethoscope, “the friendly foe”—A study to evaluate bacterial contamination of stethoscopes and disinfection practices. J. Infect. Dev. Ctries. 2018, 12, 887–893. [Google Scholar] [CrossRef] [PubMed]
- O’Gorman, J.; Humphreys, H. Application of copper to prevent and control infection. Where are we now? J. Hosp. Infect. 2012, 81, 217–223. [Google Scholar]
- Sahiledengle, B. Stethoscope disinfection is rarely done in Ethiopia: What are the associated factors? PLoS ONE 2019, 14, e0208365. [Google Scholar] [CrossRef]
- Longtin, Y.; Schneider, A.; Tschopp, C.; Renzi, G.; Gayet-Ageron, A.; Schrenzel, J.; Pittet, D. Contamination of stethoscopes and physicians’ hands after a physical examination. Mayo Clin. Proc. 2014, 89, 291–299. [Google Scholar] [CrossRef]
- Vasudevan, R.; Shin, J.H.; Chopyk, J.; Peacock, W.F.; Torriani, F.J.; Maisel, A.S.; Pride, D.T. Aseptic Barriers Allow a Clean Contact for Contaminated Stethoscope Diaphragms. Mayo Clin. Proc. Innov. Qual. Outcomes 2020, 4, 21–30. [Google Scholar] [CrossRef]
| Author, Year | Country | Year | Setting | Study Design | Aim | Sample (N) | Sample Characteristics | Reduction (%) | Results | Findings |
|---|---|---|---|---|---|---|---|---|---|---|
| Messina et al. (2018) | Italy | Nov 2016–May 2017 | Four wards of a private clinic | Cross-sectional study | To test the efficacy of a device emitting UVC light for disinfecting stethoscope membranes | 272 | Stethoscopes | 94.8% (95% CI 91.3–97.7) | The mean number of CFU: Not Treated: 132.2 Treated: 6.9 (p < 0.001) | The UV-C device can efficiently and effectively disinfect stethoscope membranes, even if they are highly contaminated |
| Datta et al. (2018) | India | 2015 | Tertiary care hospital | Cross–sectional study | To determine the disinfectant efficacy of 70% IPA | 100 | Stethoscopes | 96.2% | The mean number of CFU: Before disinfection: 65 After disinfection: 2, 5 Colonization: Before disinfection: 56 After disinfection: 5 (p < 0.001) | IPA is significantly effective in disinfection |
| Schimidt. et al. (2017) | U.S.A. | Tertiary care facilities (PedsED and AICU) | Structured prospective trial; | To assess the efficacy of antimicrobial copper stethoscope surfaces to reduce the bacterial concentration | 32 | Stethoscopes | 90.8% | The mean number of CFU (PedsED) Three surfaces sampled: 11.7/cm2 Copper arm 127.1/cm2 Control arm (p < 0.001) Diaphragm: 4/cm2 Copper arm 16/cm2 Control arm (p = 0.09) The mean number of CFU (AICU) diaphragm: 5/cm2 Copper arm 10/cm2 Control arm (p < 0.01) | Copper surfaces proved to limit the concentration of bacteria on stethoscopes surface (not always statistically significant) | |
| 75% | ||||||||||
| 50% | ||||||||||
| Messina G. et al. (2017) Letter to Editor | Italy | 2015 | Laboratories of University | Pilot study pre/post design | To test the efficacy of a device emitting UVC light through a LED to reduce bacterial load on stethoscopes surface | 10 | Stethoscopes | 85.7% | The mean (±SD) number of CFU: Not Treated: 75.9 ± 125.7 Treated: 9.5 ± 18.8. The median (IQR) number of CFU: Not Treated: 38 (12,.5–68, 75) Treated: 2.5 (0–10.5). (p < 0.01) | -The device was effective and practical to use -It may be an advantage because of lack of resistance to UVC from micro-organism involved in HAI |
| Raghubanshi et al. (2017) | Nepal | Dec 2016–March 2017 | Tertiary care hospital | Randomized blinded experimental study | To determine the effectiveness of 90% ethanol compared with isopropyl alcohol pads to reduce the bacterial load | 108 | Stethoscopes | 100 | The median (IQR) number of CFU: Before disinfection: -IPA 22.5 (7–48) -Ethanol 17.5 (7–31) After disinfection: -IPA 0 (0–0) (p < 0.001) -Ethanol 0 (0–0) (p < 0.001) | Both 90% ethanol and IPA are equally effective in decontaminating the diaphragm of the stethoscope |
| Alvarez MD et al. (2016) | Mexico | 2013 | Secondary care hospital/ Tertiary care hospital | Experimental, controlled blinded trial | To determine differences in recontamination of stethoscope membranes after being cleaned with chlorhexidine, triclosan or alcohol | 370 | Stethoscopes | 100 (IPA) | Median (IQR) of CFU for study arms: baseline: 10 (3–42) IPA, at the time 0: 0(0–0) IPA, the residual effect at 4h: 8 (1–28) Triclosan, the residual effect at 4 h: 4 (0–17) Chlorhexidine, residual effect at 4h: 0 (0–1) Kruskal–Wallis Test: 133.2 (p < 0.001) | -Chlorhexidine prevented the recontamination of stethoscopes for at least 4 h after disinfection -No significant differences between the bacterial load of the chlorhexidine arm and one of the immediate effects of the isopropyl alcohol |
| Messina G. et al. (2016) | Italy | August 2015–March 2016 | Laboratories of University | Cross-sectional study pre/post design | To test if the UVC LEDs are still effective to reduce microbial contamination after a prolonged use | 1 | Stethoscopes | 85.6 | The number of CFU: Not Treated: 104 CFU Treated (LED 16):15 CFU (p < 0.001) Treated (LED 18):12 CFU (p < 0.001) | UVC LEDs were still effective in disinfection after a prolonged use |
| Messina G et al. (2015) | Italy | n.r. | Laboratories of University | Cohort study | To test the efficacy of a device emitting UVC light for reducing bacterial load of E. Coli, S. Aureus, P. Aeruginosa and E. Faecalis | 28 | Stethoscopes | >85 | Median (and IQR) of CFU: S. aureus: Not Treated: 56 (51–64) Treated: 7 (5–8) p < 0.01 E. coli: Not Treated: 35 (27–43) Treated: 2 (1–3) p < 0.01 P. aeruginosa: Not Treated: 39 (38–41) Treated: 2 (2–3) < 0.01 E. faecalis: Not Treated: 228 (198–261) Treated: 33 (25–36) p < 0.01 | For all four species, statistically significant differences were found in CFU count after one UVC treatment |
| Grandiere-Perez et al. (2015) Letter to Editor | France | n.r. | Le Mans Hospital | Cross-sectional study pre/post design | To test the effectiveness of an EBHS to reduce the number of bacterial colonies on stethoscope diaphragms. | 40 | Stethoscopes | 96.3 | The mean number of CFU: Before disinfection: 29.9 per plate After disinfection: 1.1 per plate Colonization: Before disinfection: 38 out of 40 (95%); After disinfection: 22 out of 40 (55%); p < 0.001 | The EBHS was effective to significantly reduce the bacterial load on stethoscopes |
| Messina G. et al. (2013) | Italy | n.r. | Hospital of Siena | Cross-sectional study pre/post design | -To evaluate the environmental contamination in Hospital Setting and to evaluate the efficacy of a putty compound (the main components: ethanol (29%), water (51%, guar (6%), glycerine (%)) | 35 37 27 | Stethoscopes Telephone handsets Computer keyboards | >99 | CFU total count: TBC at 36°: Before disinfection: 3368 After disinfection: 1 TBC at 22°: Before disinfection: 3678 After disinfection: 0 | -Proper disinfection of medical devices is very important -The disinfecting technique used was effective in reducing bacterial load |
| Mehta et al. (2010) | U.S.A. | n.r. | Grady Memorial Hospital and Emory University Hospital Midtown | Cross-sectional study pre/post design | To test the efficacy of alcohol-based hand rubs to reduce bacterial load on stethoscope surfaces and to compare it with that of the isopropyl alcohol wipes | 84 | Stethoscopes | 90 | The median (IQR) number of CFU: Before disinfection: 34.5 (0–247) After disinfection: -Alcohol hand rub: 4 CFU (0–60) p < 0.001 no growth in 12 (20%) out of 60 - Alcohol wipe: 0 CFU (0–59) no growth in 17 (71%) out of 24 p = 0.001 | -Both methods significantly reduced bacterial contamination - the alcohol wipes were more effective but less available |
| Schroeder et al. (2009) | U.S.A. | n.r. | A community-based hospital and 1 satellite family health center | Prospective, single-blinded study Pre/post Design | To test if clinicians can simultaneously disinfect stethoscope diaphragm and their hands with alcohol-based foam | 92 | Stethoscopes | 88.7 | The mean number of CFU: Before disinfection:28.4 (95% CI, 20.2–36.6) After disinfection: 3.2 (95% CI, 1.8–4.6; p < 0.001). | The use of alcohol-based hand foam can simultaneously disinfect the hands and the stethoscope diaphragm |
| Wood M et al. (2007) | U.S.A. | 2003 | A medical/surgical/trauma intensive care unit (ICU) and a regional trauma emergency department (ED) | Cross-sectional study | To test the utility of the stethoscope covers impregnated with silver ions in preventing surface contamination | 74 (37 with cover, 37 no cover) | Stethoscopes | - | The mean number of CFU: uncovered: 71.4 cover < 1 week: 246.5 cover > week: 335.6 | The use of the cover was associated with significantly higher colony counts |
| Hill et al. (2005) Letter to editor | U.K. | n.r. | Elderly care department | Prospective, cross-sectional study pre/post design | To evaluate the effectiveness of both the sensitization campaign and of the increased availability of alcohol wipes | n.r. | Stethoscopes | - | The mean total colony count: baseline: 70, one month: 59, three months: 41 (↓ 41%) MRSA colonies fell from 0.42 per stethoscopes to 0.08 per stethoscopes at one month (↓83%). No MRSA colonies at three months (↓100%) | -The awareness campaign was effective -the alcohol wipes decrease the bacterial load - No MRSA colonies at three months |
| Parmar et al. (2004) | India | n.r. | Tertiary care hospital | Prospective randomized, double blind study | To determine the effectiveness of disinfection with 66% ethyl alcohol | 100 | Stethoscopes | 94.8 (Group B) | Before cleaning: 90% stethoscopes contaminated - Immediately after cleaning: 28% stethoscopes contaminated after five days without cleaning: 95% stethoscopes contaminated -Five days after cleaning once a day: 25% stethoscopes contaminated | 66% ethyl alcohol was an effective disinfectant |
| Leprat et al. (1998) Letter to editor | France | n.r. | Service d’Higiene Hospitaliere | Cross-sectional study pre/post design | To assess: - The efficacy of wipes impregnated with benzalkonium to clean stethoscopes -The rate of recontamination after use | 105 | Stethoscopes | 100 | Before disinfection: 97 stethoscopes contaminatedAfter disinfection: No stethoscopes contaminated The rate recontamination: after five uses ->100% recontaminated stethoscopes | -The reduction of the bacterial load was remarkable -The rate of recontamination increases with increasing the use |
| Marinella M et al. (1997) | U.S.A. | n.r. | Intensive care unit | Cross-sectional study pre/post design | To compare the effectiveness of various cleaning agents | 40 (10 for each method tested) | Stethoscopes | ≥80.6 (IPA, NaOCl, BAK) | The mean (±SE) of CFU and: Before disinfection diaphragm 158 ± 33 rim 289 ± 54 After disinfection:diaphragm: 0.2( ± 0.2) (p = 0.2) IPA 0.1(±0.1) (p = 0.2) NaOCl 0.6(±0.4) (p = 0.02) BAK 47(±28) (p = 0.11) Soap and water Rim: 2.2(±1.5) (p = 0.01) IPA 50(±29) (p = 0.04) NaOCl 56 ± 49 (p = 0.04) BAK 95 ± 48 (p = 0.11) Soap and water | -The most cleaning agent was IPA. -In addition, sodium hypochlorite and benzalkonium chloride significantly decreased colony counts. Soap and water did not do it significantly |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Napolitani, M.; Bezzini, D.; Moirano, F.; Bedogni, C.; Messina, G. Methods of Disinfecting Stethoscopes: Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 1856. https://doi.org/10.3390/ijerph17061856
Napolitani M, Bezzini D, Moirano F, Bedogni C, Messina G. Methods of Disinfecting Stethoscopes: Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(6):1856. https://doi.org/10.3390/ijerph17061856
Chicago/Turabian StyleNapolitani, Margherita, Daiana Bezzini, Fulvio Moirano, Corrado Bedogni, and Gabriele Messina. 2020. "Methods of Disinfecting Stethoscopes: Systematic Review" International Journal of Environmental Research and Public Health 17, no. 6: 1856. https://doi.org/10.3390/ijerph17061856
APA StyleNapolitani, M., Bezzini, D., Moirano, F., Bedogni, C., & Messina, G. (2020). Methods of Disinfecting Stethoscopes: Systematic Review. International Journal of Environmental Research and Public Health, 17(6), 1856. https://doi.org/10.3390/ijerph17061856




