The Association of Active Living Environments and Mental Health: A Canadian Epidemiological Analysis
Abstract
:1. Introduction
2. Materials and Methods
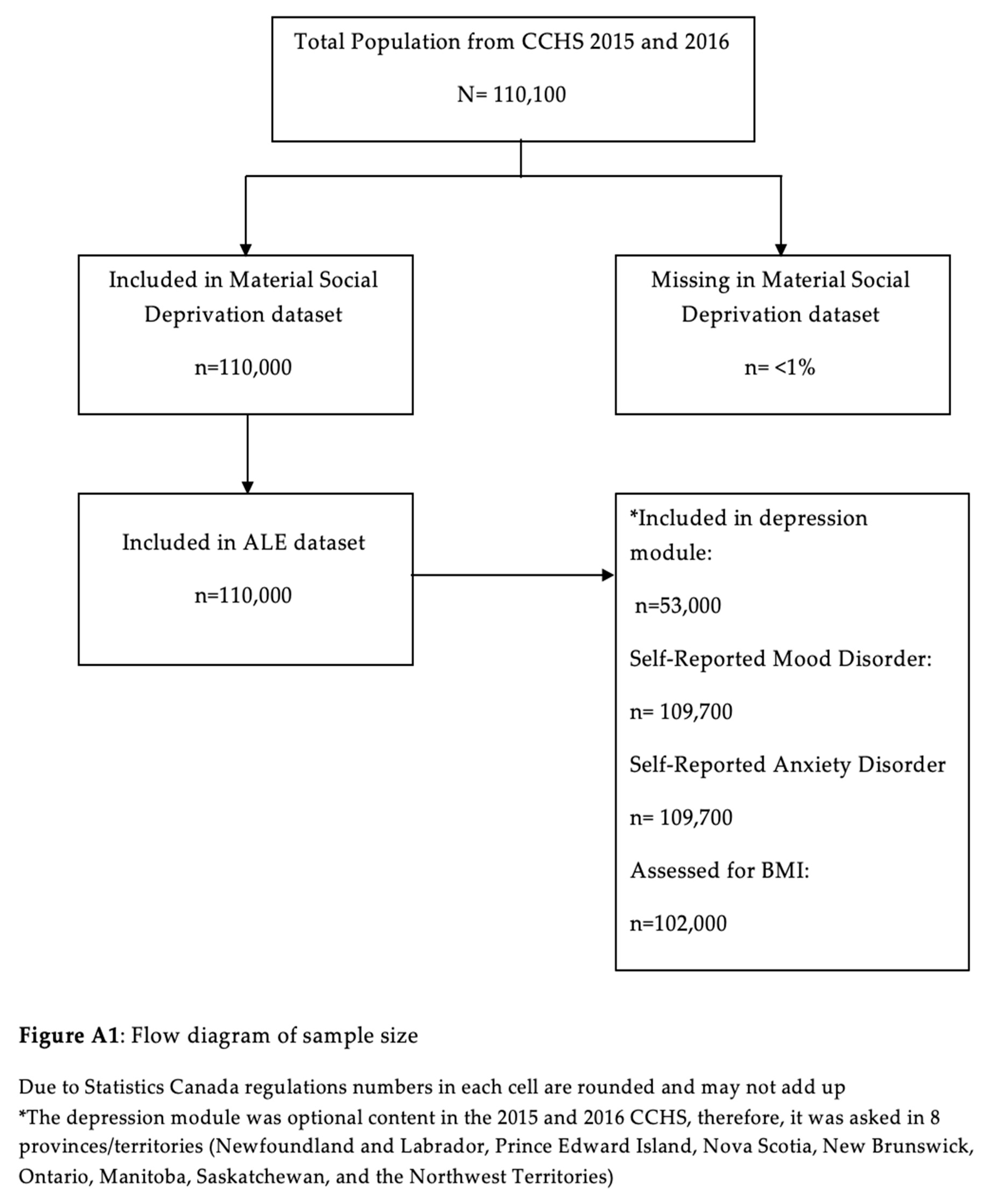
2.1. Study Population (Canadian Community Health Survey)
2.2. Health Outcomes
2.2.1. Patient Health Questionnaire-9
2.2.2. Self-Reported Mood and Anxiety Disorders
2.2.3. Social and Material Deprivation
2.2.4. Body Mass Index
2.3. Active Living Environments (Exposure)
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
References
- Canadian Urban Environmental Health Research Consortium CANUE Metadata Canadian Social and Material Deprivation. Available online: https://canue.ca/wp-content/uploads/2019/05/CANUE-Metadata-Deprivation-Index.pdf (accessed on 15 February 2020).
- McCormack, G.R.; Cabaj, J.; Orpana, H.; Lukic, R.; Blackstaffe, A.; Goopy, S.; Hagel, B.; Keough, N.; Martinson, R.; Chapman, J.; et al. A scoping review on the relations between urban form and health: A focus on Canadian quantitative evidence. Health Promot. Chronic Dis. Prev. Can. Res. Policy Pract. 2019, 39, 187–200. [Google Scholar] [CrossRef] [PubMed]
- Colley, R.C.; Christidis, T.; Michaud, I.; Tjepkema, M.; Ross, N.A. An examination of the associations between walkable neighbourhoods and obesity and self-rated health in Canadians. Health Rep. 2019, 30, 14–24. [Google Scholar] [PubMed]
- Malambo, P.; Kengne, A.P.; De Villiers, A.; Lambert, E.V.; Puoane, T. Built environment, selected risk factors and major cardiovascular disease outcomes: A systematic review. PLoS ONE 2016, 11, e0166846. [Google Scholar] [CrossRef] [PubMed]
- Creatore, M.I.; Glazier, R.H.; Moineddin, R.; Fazli, G.S.; Johns, A.; Gozdyra, P.; Matheson, F.I.; Kaufman-Shriqui, V.; Rosella, L.C.; Manuel, D.G. Association of neighborhood walkability with change in overweight, obesity, and diabetes. JAMA 2016, 315, 2211–2220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Global Strategy on Diet, Physical Activity and Health. Available online: https://www.who.int/dietphysicalactivity/factsheet_adults/en/ (accessed on 15 February 2020).
- Mammen, G.; Faulkner, G. Physical activity and the prevention of depression: A systematic review of prospective studies. Am. J. Prev. Med. 2013, 45, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Meyer, J.D.; Crombie, K.M.; Cook, D.B.; Hillard, C.J.; Koltyn, K.F. Serum Endocannabinoid and Mood Changes after Exercise in Major Depressive Disorder. Med. Sci. Sports Exerc. 2019, 51, 1909–1917. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gariepy, G.; Blair, A.; Kestens, Y.; Schmitz, N. Neighbourhood characteristics and 10-year risk of depression in Canadian adults with and without a chronic illness. Health Place 2014, 30, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Rebar, A.L.; Stanton, R.; Geard, D.; Short, C.; Duncan, M.J.; Vandelanotte, C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol. Rev. 2015, 9, 366–378. [Google Scholar] [CrossRef] [PubMed]
- Statistics Canada Canadian Community Health Survey—Annual Component (CCHS). Available online: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226#a2 (accessed on 15 February 2020).
- Kroenke, K.; Spitzer, R.L. The PHQ-9: A new depression diagnostic and severity measure. Psychiatr. Ann. 2002, 32, 509–515. [Google Scholar] [CrossRef] [Green Version]
- Pampalon, R.; Hamel, D.; Gamache, P.; Philibert, M.D.; Raymond, G.; Simpson, A. An area-based material and social deprivation index for public health in Québec and Canada. Can. J. Public Health Revue Canadienne de Sante’e Publique 2012, 103, S17–S22. [Google Scholar] [CrossRef]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Statistics Canada Canadian Guidelines for Body Weight Classification in Adults—Quick Reference Tool for Professionals. Available online: https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/fn-an/alt_formats/hpfb-dgpsa/pdf/nutrition/cg_quick_ref-ldc_rapide_ref-eng.pdf (accessed on 15 February 2020).
- Ross, N.; Wasfi, R.; Herrmann, T.; Gleckner, W. Canadian Active Living Environments Database (Can-ALE) User Manual & Technical Document; Geo-Social Determinants of Health Research Group, Department of Geography, McGill University: Montreal, QC, Canada, 2018. [Google Scholar]
- Canadian Urban Environmental Health Research Consortium. CanMap Postal Code Suite, v2016.3; Computer File; DMTI Spatial Inc.: Markham, ON, Canada, 2016. [Google Scholar]
- Canadian Urban Environmental Health Research Consortium CANUE Metadata Canadian Active Living Environments. Available online: https://canue.ca/wp-content/uploads/2019/05/CANUE-Metadata-Canadian-Active-Living-Environments.pdf (accessed on 15 February 2020).
- Frank, L.D.; Pivo, G. Impacts of mixed use and density on utilization of three modes of travel: Single-occupant vehicle, transit, and walking. Transp. Res. Rec. 1994, 1466, 44–52. [Google Scholar]
- Lee, C.; Moudon, A.V. Correlates of walking for transportation or recreation purposes. J. Phys. Act. Health 2006, 3, S77–S98. [Google Scholar] [CrossRef] [PubMed]
- Herrmann, T.; Gleckner, W.; Wasfi, R.A.; Thierry, B.; Kestens, Y.; Ross, N.A. A pan-Canadian measure of active living environments using open data. Health Rep. 2019, 30, 16–25. [Google Scholar]
- StataCorp LLC. Stata Statistical Software: Release 15; StataCorp LLC: College Station, TX, USA, 2017. [Google Scholar]
- Sugiyama, T.; Leslie, E.; Giles-Corti, B.; Owen, N. Associations of neighbourhood greenness with physical and mental health: Do walking, social coherence and local social interaction explain the relationships? J. Epidemiol. Community Health 2008, 62, e9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Srugo, S.A.; de Groh, M.; Jiang, Y.; Morrison, H.I.; Hamilton, H.A.; Villeneuve, P.J. Assessing the impact of school-based greenness on mental health among adolescent students in Ontario, Canada. Int. J. Environ. Res. Public Health 2019, 16, 4364. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, M.; Hosking, J.; Woodward, A.; Witten, K.; MacMillan, A.; Field, A.; Baas, P.; Mackie, H. Systematic literature review of built environment effects on physical activity and active transport–an update and new findings on health equity. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 158. [Google Scholar] [CrossRef] [PubMed]
| Demographic Characteristics | Overall CCHS (%) n ≈ 110,000 | Active Living Environments | |||
|---|---|---|---|---|---|
| Class 1 n ≈ 49,000 (%) (Very Low) | Class 2 n ≈ 33,000 (%) (Low) | Class 3 n ≈ 19,000 (%) (Moderate) | Class 4/5 n ≈ 8000 (%) (High/ Very High) | ||
| Used Active Transport a | 46.9 (46.3, 47.4) | 36.0 (35.2, 36.8) | 44.4 (43.3, 45.5) | 49.89 (48.7, 51.1) | 68.87 (67.2, 70.6) |
| Active Transport a,b (mean minutes) | 96.8 (94.58, 98.3) | 73.2 (70.2, 76.1) | 85.7 (82.5, 88.9) | 99.9 (95.3, 104.6) | 162.4 (153.3, 171.5) |
| Recreational Activity a (mean minutes) | 111.1 (108.5, 113.7) | 110.2 (106.5, 114.0) | 118.2 (113.4, 122.9) | 102.7 (98.0, 107.4) | 111.9 (102.1, 121.7) |
| Hours spent sedentary | |||||
| 0–14 | 26.0 (25.3, 26.8) | 28.4 (27.2, 29.6) | 24.8 (23.6, 26.0) | 25.5 (24.0, 27.0) | 25.8(23.6, 27.9) |
| 15–24 | 25.5 (24.8, 26.2) | 26.2 (25.0, 27.3) | 25.7 (24.4, 26.9) | 25.5 (24.2, 26.9) | 24.0 (22.0, 26.0) |
| 23–34 | 18.6 (18.0, 19.2) | 18.1 (17.2, 19.0) | 18.7 (17.6, 19.6) | 18.4 (17.1, 19.7) | 19.6 (17.8, 21.4) |
| 32+ | 29.9 (29.2, 30.7) | 27.4 (26.2, 28.5) | 30.9 (29.7, 32.1) | 30.6 (29.1, 32.1) | 30.6 (28.4, 32.9) |
| Material Deprivation | |||||
| 1 (Lowest) | 20.9 (20.0, 21.8) | 15.0 (13.5, 16.5) | 23.9 (22.0, 25.8) | 17.4 (15.3, 19.4) | 32.9 (29.6, 36.1) |
| 2 | 20.3 (19.3, 21.3) | 22.9 (21.3, 24.4) | 25.5 (23.4, 27.5) | 14.8 (12.8, 16.7) | 13.0 (10.2, 15.9) |
| 3 | 20.6 (19.5, 21.3) | 22.9 (21.3, 24.5) | 21.3 (19.4, 23.1) | 21.5 (19.1, 24.0) | 12.8 (9.9, 15.7) |
| 4 | 19.8 (18.8, 20.8) | 21.8 (20.3, 23.3) | 17.7 (16.0, 19.5) | 21.5 (19.1, 23.9) | 17.5 (14.4, 20.5) |
| 5 (Highest) | 18.4 (17.5, 19.3) | 17.4 (16.1, 18.7) | 11.7 (10.2, 13.2) | 24.9 (22.5, 27.3) | 23.8 (20.5, 27.1) |
| Social Deprivation | |||||
| 1 (Lowest) | 18.3 (17.4, 19.2) | 19.2 (17.8, 20.7) | 23.0 (21.1, 25.0) | 19.8 (17.4, 22.2) | 3.4 (2.0, 4.8) |
| 2 | 18.5 (17.5, 19.4) | 26.3 (24.6, 27.9) | 19.2 (17.4, 21.0) | 14.4 (12.3, 16.5) | 7.4 (5.1, 9.7) |
| 3 | 19.6 (18.6, 20.6) | 27.2 (25.5, 28.9) | 19.2 (17.4, 21.0) | 14.3 (12.3, 16.3) | 13.4 (10.6, 16.2) |
| 4 | 21.3 (20.3, 22.4) | 19.4 (17.9, 20.8) | 19.8 (18.0, 21.5) | 21.3 (19.0, 23.6) | 28.7(25.0, 32.5) |
| 5 (Highest) | 22.4 (21.4, 23.3) | 7.9 (7.0, 8.9) | 18.8 (17.3, 20.4) | 30.2 (28.0, 32.5) | 47.0 (43.1, 50.9) |
| Age (Mean) | 45.3 (45.2, 45.4) | 46.8 (46.5, 47.1) | 45.2 (44.9, 45.50) | 44.4 (44.0, 44.8) | 42.0 (43.4, 44.5) |
| Sex | |||||
| Female | 50.7 (50.6, 50.7) | 49.9 (49.3, 50.4) | 50.0 (49.3, 50.8) | 51.7 (50.7, 52.6) | 52.1 (51.0, 53.1) |
| Marital status | |||||
| Married/Common Law | 57.8 (57.3, 58.3) | 63.6 (62.9, 64.3) | 59.6 (58.7, 60.6) | 53.4 (52.3, 54.6) | 48.9 (47.1, 50.8) |
| Single | 30.1 (29.7, 30.5) | 25.3 (24.7, 25.9) | 28.7 (27.9, 29.6) | 33.2 (32.1, 34.2) | 37.6 (36.0, 39.2) |
| Widowed/ separated/ divorced | 12.2 (11.8, 12.5) | 11.1 (10.7, 11.6) | 11.7 (11.1, 12.2) | 13.4 (12.7, 14.1) | 13.5 (12.4, 14.6) |
| Highest Level of Education | |||||
| Less Than Secondary School | 18.5 (18.2, 18.8) | 22.2 (21.5, 22.8) | 17.3 (16.7, 18.0) | 18.1 (17.2, 19.0) | 13.6 (12.5, 14.7) |
| No Post-Secondary | 23.2 (22.8, 23.7) | 24.4 (23.7, 25.1) | 23.4 (22.6, 24.2) | 23.8 (22.8, 24.7) | 19.5 (18.0, 21.0) |
| Certificate, Diploma, or University Degree | 58.3 (57.8, 58.8) | 53.4 (52.6, 54.3) | 59.3 (58.3, 60.3) | 58.1 (57.0, 59.3) | 66.9 (65.1, 68.6) |
| Employment Status (last week) | |||||
| Worked | 61.9 (61.4, 62.4) | 60.3 (59.7, 61.0) | 62.8 (61.8, 63.7) | 61.8 (60.6, 63.0) | 63.4 (61.6, 65.1) |
| Absent from job | 4.9 (4.6, 5.2) | 5.3 (4.9, 5.7) | 5.3 (4.8, 5.7) | 4.3 (3.8, 4.8) | 4.2 (3.4, 5.0) |
| No job | 33.2 (32.7, 33.7) | 34.4 (33.7, 35.1) | 31.9 (31.0, 32.9) | 33.9 (32.7, 35.0) | 32.5 (30.7, 34.2) |
| Adjusted Household Income (Ratio to Low Income Cut-off) | |||||
| Quartile 1 (Highest) | 26.0 (25.6, 26.5) | 19.5 (19.0, 20.1) | 24.0 (23.1, 24.8) | 30.7 (29.6, 31.8) | 36.1 (34.5, 37.8) |
| Quartile 2 | 25.2 (24.8, 25.7) | 25.6 (25.0, 26.2) | 25.9 (25.1, 26.7) | 24.7(23.6, 25.7) | 24.1 (22.6, 25.5) |
| Quartile 3 | 24.2 (23.7, 24.6) | 25.6 (25.0, 26.2) | 23.3 (22.6, 24.1) | 23.9 (23.0, 24.8) | 23.6 (22.2, 25.0) |
| Quartile 4 (Lowest) | 24.6 (24.2, 25.0) | 29.3 (28.7, 29.9) | 26.8 (26.0, 27.6) | 20.7 (19.8, 21.7) | 16.2 (14.9, 17.6) |
| Landed immigrant, non-permanent resident | 25.7 (25.2, 26.3) | 9.9 (9.3, 10.6) | 23.0 (21.7, 24.2) | 37.3 (35.8, 38.9) | 45.7 (43.65, 47.8) |
| Current Smoker | 17.4 (16.9, 17.8) | 18.2 (17.6, 18.8) | 16.4 (15.7, 17.1) | 17.1 (16.2, 18.0) | 17.7 (16.3, 19.1) |
| Binge Drinker c | 25.0 (24.4, 25.5) | 27.0 (26.3, 27.8) | 23.5 (22.6, 24.4) | 23.9 (22.7, 25.0) | 25.5 (23.6, 27.5) |
| BMI- Standard International | |||||
| Obese | 19.1 (18.7,19.6) | 22.2 (21.5, 22.8) | 19.8 (19.0, 20.6) | 17.8 (16.9, 18.7) | 13.4 (12.0, 14.5) |
| Chronic Conditions | |||||
| Has at least 1 of 10 chronic conditions d | 50.7 (50.1, 51.2) | 53.4 (52.6, 54.2) | 51.2 (50.2, 52.1) | 49.9 (48.8, 51.0) | 45.1 (43.4, 46.9) |
| Exposure | PHQ-9 10+ | Mood Disorder | Anxiety Disorder | Obesity | ||||
|---|---|---|---|---|---|---|---|---|
| ALE | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value |
| Class 1 | 0.82 (0.64–1.05) | 0.12 | 0.94 (0.82, 1.07) | 0.36 | 1.08 (0.95, 1.23) | 0.24 | 1.86 (1.66–2.08) | <0.01 |
| Class 2 | 0.80 (0.62–1.04) | 0.10 | 1.00 (0.88, 1.51) | 0.90 | 1.08 (0.95, 1.23) | 0.25 | 1.61 (1.44–1.82) | <0.01 |
| Class 3 | 0.97 (0.74–1.27) | 0.81 | 1.02 (0.89, 1.17) | 0.78 | 1.14 (0.99, 1.30) | 0.06 | 1.42 (1.26–2.61) | <0.01 |
| Class 4/5 | ref | ref | ref | ref | ||||
| PHQ-9 10+ | Mood Disorder | Anxiety Disorder | Obesity | |||||
|---|---|---|---|---|---|---|---|---|
| Exposure | aOR (95% CI) | p-value | aOR (95% CI) | p-value | aOR (95% CI) | p-value | aOR (95% CI) | p-value |
| Active Living Environment | ||||||||
| Class 1 | 0.98 (0.71–1.35) | 0.90 | 0.88 (0.74, 1.05) | 0.16 | 0.95 (0.80, 1.13) | 0.56 | 1.65 (1.43–2.03) | <0.01 |
| Class 2 | 0.92 (0.67–1.25) | 0.59 | 0.93 (0.79, 1.09) | 0.36 | 0.98 (0.84, 1.16) | 0.84 | 1.47 (1.20–1.81) | <0.01 |
| Class 3 | 1.11 (0.80–1.54) | 0.53 | 0.95 (0.80, 1.12) | 0.51 | 1.01 (0.85, 1.19) | 0.94 | 1.21 (0.97–1.50) | 0.09 |
| Class 4/5 | ref | ref | ref | ref | ||||
| Material Deprivation | ||||||||
| Quintile 1 | ref | ref | ref | ref | ||||
| Quintile 2 | 0.93 (0.72–1.19) | 0.56 | 0.89 (0.78, 1.01) | 0.07 | 1.07 (0.93, 1.22) | 0.34 | 1.32 (1.14–1.53) | <0.01 |
| Quintile 3 | 0.85 (0.67–1.07) | 0.15 | 1.04 (0.92, 1.19) | 0.52 | 1.17 (1.02, 1.34) | 0.02 | 1.32 (1.15–1.52) | <0.01 |
| Quintile 4 | 0.95 (0.74–1.22) | 0.71 | 1.01 (0.89, 1.15) | 0.82 | 1.30 (1.13, 1.49) | <0.01 | 1.68 (1.45–1.94) | <0.01 |
| Quintile 5 | 1.00 (0.78–1.28) | 1.00 | 0.93 (0.82, 1.07) | 0.32 | 1.39 (1.22, 1.59) | <0.01 | 1.83 (1.57–2.13) | <0.01 |
| Social Deprivation | ||||||||
| Quintile 1 | ref | ref | ref | ref | ||||
| Quintile 2 | 1.37 (1.07–1.77) | 0.01 | 1.15 (0.99, 1.34) | 0.07 | 1.16 (0.98, 1.37) | 0.08 | 1.20 (1.05–1.37) | <0.01 |
| Quintile 3 | 1.51 (1.17–1.93) | <0.01 | 1.14 (0.98, 1.33) | 0.09 | 1.22 (1.04, 1.43) | 0.02 | 1.26 (1.11–1.44) | <0.01 |
| Quintile 4 | 1.61 (1.29–2.01) | <0.01 | 1.25 (1.08, 1.45) | <0.01 | 1.20 (1.03, 1.40) | 0.02 | 1.25 (1.10–1.42) | <0.01 |
| Quintile 5 | 2.05 (1.61–2.59) | <0.01 | 1.50 (1.29, 1.75) | <0.01 | 1.45 (1.24, 1.69) | <0.01 | 1.23 (1.07–1.40) | <0.01 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lukmanji, A.; Williams, J.V.A.; Bulloch, A.G.M.; Dores, A.K.; Patten, S.B. The Association of Active Living Environments and Mental Health: A Canadian Epidemiological Analysis. Int. J. Environ. Res. Public Health 2020, 17, 1910. https://doi.org/10.3390/ijerph17061910
Lukmanji A, Williams JVA, Bulloch AGM, Dores AK, Patten SB. The Association of Active Living Environments and Mental Health: A Canadian Epidemiological Analysis. International Journal of Environmental Research and Public Health. 2020; 17(6):1910. https://doi.org/10.3390/ijerph17061910
Chicago/Turabian StyleLukmanji, Aysha, Jeanne V.A. Williams, Andrew G.M. Bulloch, Ashley K. Dores, and Scott B. Patten. 2020. "The Association of Active Living Environments and Mental Health: A Canadian Epidemiological Analysis" International Journal of Environmental Research and Public Health 17, no. 6: 1910. https://doi.org/10.3390/ijerph17061910






