Melatonin-Measurement Methods and the Factors Modifying the Results. A Systematic Review of the Literature
Abstract
1. Introduction
2. Dim Light Melatonin Onset
3. Material Sampling
3.1. Blood
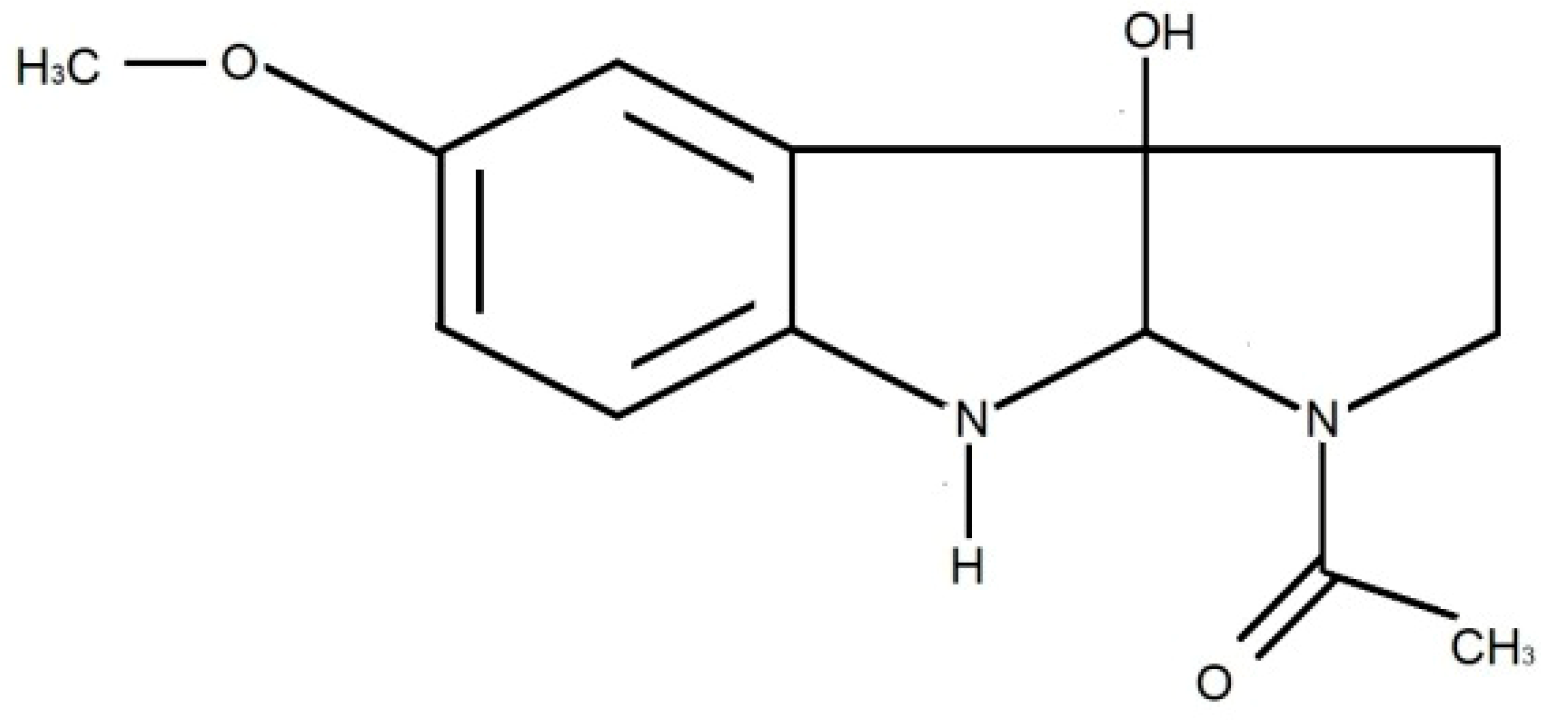
3.2. Urine
3.3. Saliva
3.4. Cerebrospinal Fluid (CSF)
4. Material Collection
5. Material Storage
5.1. Blood
5.2. Urine
5.3. Saliva
6. Analysis
6.1. Radioimmunoassay (RIA)
6.2. Elisa
6.3. High Performance Liquid Chromatography (HPLC)
6.4. Fast-Scan Cyclic Voltammetry (FSCV)
7. Factors Affecting the Measurement Results
7.1. Non-Modifiable Factors
7.1.1. Genetic factors
7.1.2. Age
7.1.3. Sex
7.2. Modifiable Factors
7.2.1. Light
7.2.2. Seasonal Changes
7.2.3. Posture During the Examination
7.2.4. Physical Activity
8. Comorbidities
8.1. Ophthalmic Diseases
8.2. Spinal Cord Injuries
8.3. Liver and Kidney Diseases
8.4. Periodontal Disease
9. Medications
10. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ostrin, L.A. Ocular and systemic melatonin and the influence of light exposure: Melatonin and light exposure. Clin. Exp. Optom. 2019, 102, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Mirick, D.K.; Davis, S. Melatonin as a biomarker of circadian dysregulation. Cancer Epidemiol. Biomark. Prev. 2008, 17, 3306–3313. [Google Scholar] [CrossRef] [PubMed]
- Hartley, S.; Dauvilliers, Y.; Quera-Salva, M.A. Circadian rhythm disturbances in the blind. Curr. Neurol. Neurosci. Rep. 2018, 18, 65. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, C.A.; Allan, J.S.; Strogatz, S.H.; Ronda, J.M.; Sánchez, R.; Ríos, C.D.; Freitag, W.O.; Richardson, G.S.; Kronauer, R.E. Bright light resets the human circadian pacemaker independent of the timing of the sleep-wake cycle. Science 1986, 233, 667–671. [Google Scholar] [CrossRef]
- Tricoire, H.; Locatelli, A.; Chemineau, P.; Malpaux, B. Melatonin enters the cerebrospinal fluid through the pineal recess. Endocrinology 2002, 143, 84–90. [Google Scholar] [CrossRef]
- Legros, C.; Chesneau, D.; Boutin, J.A.; Barc, C.; Malpaux, B. Melatonin from cerebrospinal fluid but not from blood reaches sheep cerebral tissues under physiological conditions. J. Neuroendocrinol. 2014, 26, 151–163. [Google Scholar] [CrossRef]
- Maitra, S.; Bhattacharya, D.; Das, S.; Bhattacharya, S. Melatonin and its anti-glioma functions: A comprehensive review. Rev. Neurosci. 2019, 30, 527–541. [Google Scholar] [CrossRef]
- Ikegami, T.; Azuma, K.; Nakamura, M.; Suzuki, N.; Hattori, A.; Ando, H. Diurnal expressions of four subtypes of melatonin receptor genes in the optic tectum and retina of goldfish. Comp. Biochem. Physiol. A Mol. Integr. Physiol. 2009, 152, 219–224. [Google Scholar] [CrossRef]
- Bourne, R.S.; Mills, G.H. Melatonin: Possible implications for the postoperative and critically ill patient. Intensive Care Med. 2006, 32, 371–379. [Google Scholar] [CrossRef]
- Lüdemann, P.; Zwernemann, S.; Lerchl, A. Clearance of melatonin and 6-sulfatoxymelatonin by hemodialysis in patients with end-stage renal disease. J. Pineal Res. 2001, 31, 222–227. [Google Scholar] [CrossRef]
- Cutando, A.; Gómez-Moreno, G.; Arana, C.; Acuña-Castroviejo, D.; Reiter, R.J. Melatonin: Potential functions in the oral cavity. J. Periodontol. 2007, 78, 1094–1102. [Google Scholar] [CrossRef] [PubMed]
- Nowak, R.; Mcmillen, I.C.; Redman, J.; Short, R.V. The correlation between serum and salivary melatonin concentrations and urinary 6-hydroxymelatonin sulphate excretion rates: Two non-invasive techniques for monitoring human circadian rhythmicity. Clin. Endocrinol. 1987, 27, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Claustrat, B.; Brun, J.; Chazot, G. The basic physiology and pathophysiology of melatonin. Sleep Med. Rev. 2005, 9, 11–24. [Google Scholar] [CrossRef] [PubMed]
- Paprocka, J.; Kijonka, M.; Pęcka, M.; Sokół, M. Melatonin in epilepsy: A new mathematical model of diurnal secretion. Int. J. Endocrinol. 2016, 2016, 3861461. [Google Scholar] [CrossRef]
- Paprocka, J.; Kijonka, M.; Boguszewicz, Ł.; Sokół, M. Melatonin in tuberous sclerosis complex analysis using modern mathematical modeling methods. Int. J. Endocrinol. 2017, 2017, 8234502. [Google Scholar] [CrossRef]
- Paprocka, J.; Kijonka, M.; Wojcieszek, P.; Pęcka, M.; Emich-Widera, E.; Sokół, M. Melatonin and Angelman Syndrome: Implication and mathematical model of diurnal secretion. Int. J. Endocrinol. 2017, 2017, 5853167. [Google Scholar] [CrossRef]
- Gunn, P.J.; Middleton, B.; Davies, S.K.; Revell, V.L.; Skene, D.J. Sex differences in the circadian profiles of melatonin and cortisol in plasma and urine matrices under constant routine conditions. Chronobiol. Int. 2016, 33, 39–50. [Google Scholar] [CrossRef]
- Tähkämö, L.; Partonen, T.; Pesonen, A.K. Systematic review of light exposure impact on human circadian rhythm. Chronobiol. Int. 2019, 36, 151–170. [Google Scholar] [CrossRef]
- Robillard, R.; Carpenter, J.S.; Rogers, N.L.; Fares, S.; Grierson, A.B.; Hermens, D.F.; Naismith, S.L.; Mullin, S.J.; Feilds, K.L.; Glozier, N.; et al. Circadian rhythms and psychiatric profiles in young adults with unipolar depressive disorders. Transl. Psychiatry 2018, 8, 213. [Google Scholar] [CrossRef]
- Deacon, S.; Arendt, J. Posture influences melatonin concentrations in plasma and saliva in humans. Neurosci. Lett. 1994, 167, 191–194. [Google Scholar] [CrossRef]
- Crowley, S.J.; Suh, C.; Molina, T.A.; Fogg, L.F.; Sharkey, K.M.; Carskadon, M.A. Estimating the dim light melatonin onset of adolescents within a 6-h sampling window: The impact of sampling rate and threshold method. Sleep Med. 2016, 20, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Molina, T.A.; Burgess, H.J. Calculating the dim light melatonin onset: The impact of threshold and sampling rate. Chronobiol. Int. 2011, 28, 714–718. [Google Scholar] [CrossRef] [PubMed]
- Zlotos, D.P.; Jockers, R.; Cecon, E.; Rivara, S.; Witt-Enderby, P.A. MT1 and MT2 melatonin receptors: Ligands, models, oligomers, and therapeutic potential. J. Med. Chem. 2014, 57, 3161–3185. [Google Scholar] [CrossRef] [PubMed]
- Wurtman, R.J.; Waldhauser, F.; Lieberman, H.R. The Pineal Gland and Its Endocrine Role; Springer: Boston, MA, USA, 1983; Volume 65, pp. 551–573. [Google Scholar]
- Graham, C.; Cook, M.R.; Kavet, R.; Sastre, A.; Smith, D.K. Prediction of nocturnal plasma melatonin from morning urinary measures. J. Pineal Res. 1998, 24, 230–238. [Google Scholar] [CrossRef]
- Bojkowski, C.J.; Arendt, J. Factors influencing urinary 6-sulphatoxymelatonin, a major melatonin metabolite, in normal human subjects. Clin. Endocrinol. 1990, 33, 435–444. [Google Scholar] [CrossRef]
- Crasson, M.; Kjiri, S.; Colin, A.; Kjiri, K.; L’Hermite-Baleriaux, M.; Ansseau, M.; Legros, J. Serum melatonin and urinary 6-sulfatoxymelatonin in major depression. Psychoneuroendocrinology 2004, 29, 1–12. [Google Scholar] [CrossRef]
- Arendt, J.; Bojkowski, C.; Franey, C.; Wright, J.; Marks, V. Immunoassay of 6-hydroxymelatonin sulfate in human plasma and urine: Abolition of the urinary 24-hour rhythm with atenolol. J. Clin. Endocrinol. Metab. 1985, 60, 1166–1173. [Google Scholar] [CrossRef]
- Klante, G.; Brinschwitz, T.; Secci, K.; Wollnik, F.; Steinlechner, S. Creatinine is an appropriate reference for urinary sulphatoxymelatonin of laboratory animals and humans. J. Pineal Res. 1997, 23, 191–197. [Google Scholar] [CrossRef]
- Lynch, H.J.; Wyrtman, R.J.; Moskowitz, M.A.; Archer, M.C.; Ho, M.H. Daily rhythm in human urinary melatonin. Science 1975, 187, 169–171. [Google Scholar] [CrossRef]
- Matthews, C.D.; Guerin, M.V.; Wang, X. Human plasma melatonin and urinary 6-sulphatoxy melatonin: Studies in natural annual photoperiod and in extended darkness. Clin. Endocrinol. 1991, 35, 21–27. [Google Scholar] [CrossRef]
- Deacon, S.J.; Arendt, J. Phase-shifts in melatonin, 6-sulphatoxymelatonin and alertness rhythms after treatment with moderately bright light at night. Clin. Endocrinol. 2010, 40, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Cook, M.R.; Graham, C.; Kavet, R.; Stevens, R.G.; Davis, S.; Kheifets, L. Morning urinary assessment of nocturnal melatonin secretion in older women. J. Pineal Res. 2000, 28, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Touitou, Y.; Auzéby, A.; Camus, F.; Djeridane, Y. Daily profiles of salivary and urinary melatonin and steroids in healthy prepubertal boys. J. Pediatr. Endocrinol. Metab. 2009, 22, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Vakkuri, O.; Leppäluoto, J.; Kauppila, A. Oral administration and distribution of melatonin in human serum, saliva and urine. Life Sci. 1985, 37, 489–495. [Google Scholar] [CrossRef]
- Voultsios, A.; Kennaway, D.J.; Dawson, D. Salivary melatonin as a circadian phase marker: Validation and comparison to plasma melatonin. J. Biol. Rhythm. 1997, 12, 457–466. [Google Scholar] [CrossRef] [PubMed]
- Bumb, J.M.; Enning, F.; Mueller, J.K.; van der List, T.; Rohleder, C.; Findeisen, P.; Noelte, I.; Schwarz, E.; Leweke, F.M. Differential melatonin alterations in cerebrospinal fluid and serum of patients with major depressive disorders and bipolar disorder. Compr. Psychiatry 2016, 68, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Abe, M.; Kawaguchi, H.; Miura, N.; Akioka, K.; Ushikai, M.; Oi, S.; Yukawa, A.; Yoshikawa, T.; Izumi, H.; Horiuchi, M. Diurnal variation of melatonin concentration in the cerebrospinal fluid of unanesthetized microminipig. In Vivo 2018, 32, 583–590. [Google Scholar] [CrossRef]
- Cipolla-Neto, J.; Amaral, F.G.D. Melatonin as a hormone: New physiological and clinicalinsights. Endocr. Rev. 2018, 39, 990–1028. [Google Scholar] [CrossRef]
- Weissová, K.; Škrabalová, J.; Skálová, K.; Červená, K.; Bendová, Z.; Miletínová, E.; Kopřivová, J.; Šonka, K.; Dudysová, D.; Bartoš, A.; et al. Circadian rhythms of melatonin and peripheral clock gene expression in idiopathic REM sleep behavior disorder. Sleep Med. 2018, 52, 1–6. [Google Scholar] [CrossRef]
- Ong, J.C.; Taylor, H.L.; Park, M.; Burgess, H.J.; Fox, R.S.; Snyder, S.; Rains, J.C.; Espie, C.A.; Wyatt, J.K. Can circadian dysregulation exacerbate migraines? Headache 2018, 58, 1040–1051. [Google Scholar] [CrossRef]
- Kowalczyk, P.; Manda, A.; Kościelniak, B.; Tomasik, P.; Sztefko, K. Nietypowe materiały biologiczne pobierane w sposób nieinwazyjny w diagnostyce laboratoryjnej. Diagn. Lab. 2014, 50, 255–262. [Google Scholar]
- Kozaki, T.; Lee, S.; Nishimura, T.; Katsuura, T.; Yasukouchi, A. Effects of saliva collection using cotton swabs on melatonin enzyme immunoassay. J. Circadian Rhytms 2011, 9, 1. [Google Scholar] [CrossRef]
- Kozaki, T.; Hidaka, Y. Non-cotton swab sample collection may not affect salivary melatonin assai results. J. Physiol. Anthr. 2018, 37, 17. [Google Scholar] [CrossRef] [PubMed]
- Bojkowski, C.J.; Arendt, J.; Shih, M.C.; Markey, S.P. Melatonin secretion in humans assessed by measuring its metabolite, 6-sulfatoxymelatonin. Clin. Chem. 1987, 33, 1343–1348. [Google Scholar] [CrossRef] [PubMed]
- de Almeida, E.A.; Di Mascio, P.; Harumi, T.; Spence, D.W.; Moscovitch, A.; Hardeland, R.; Cardinali, D.P.; Brown, G.M.; Pandi-Perumal, S.R. Measurement of melatonin in body fluids: Standards, protocols and procedures. Child’s Nerv. Syst. 2011, 27, 879–891. [Google Scholar] [CrossRef] [PubMed]
- Webley, G.E.; Mehl, H.; Willey, K.P. Validation of a sensitive direct assay for melatonin for investigation of circadian rhythms in different species. J. Endocrinol. 1985, 106, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Ferrua, B.; Masseyeff, R. Immunoassay of melatonin with enzyme-labeled antibodies. J. Immunoass. 1985, 6, 79–94. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, V.; Porta, C.; Moroni, M.; Scoglio, E.; Moratti, R. Determination of free and total (free plus protein-bound) melatonin in plasma and cerebrospinal fluid by high-performance liquid chromatography with fluorescence detection. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2002, 774, 17–24. [Google Scholar] [CrossRef]
- Hensley, A.L.; Colley, A.R.; Ross, A.E. Real-time detection of melatonin using Fast-Scan Cyclic Voltammetry. Anal. Chem. 2018, 90, 8642–8650. [Google Scholar] [CrossRef]
- Iinuma, F.; Hamase, K.; Matsubayashi, S.; Takahashi, M.; Watanabe, M.; Zaitsu, K. Sensitive determination of melatonin by precolumn derivatization and reversed-phase high-performance liquid chromatography. J. Chromatogr. A 1999, 835, 67–72. [Google Scholar] [CrossRef]
- Tomita, T.; Hamase, K.; Hayashi, H.; Fukuda, H.; Hirano, J.; Zaitsu, K. Determination of endogenous melatonin in the individual pineal glands of inbred mice using precolumn oxidation reversed-phase micro-high-performance liquid chromatography. Anal. Biochem. 2003, 316, 154–161. [Google Scholar] [CrossRef]
- Hirano, J.; Hamase, K.; Fukuda, H.; Tomita, T.; Zaitsu, K. Novel stable fluorophore, 6-methoxy-4-quinolone, with strong fluorescence in wide pH range of aqueous media, and its application as a fluorescent labeling reagent. J. Chromatogr. A 2004, 1059, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, K.; Ostin, A.; Levin, J.O. Quantification of melatonin in human saliva by liquid chromatography-tandem mass spectrometry using stable isotope dilution. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2003, 794, 115–123. [Google Scholar] [CrossRef]
- Khan, S.A.; George, R.; Charles, B.G.; Taylor, P.J.; Heussler, H.S.; Cooper, D.M.; McGuire, T.M.; Pache, D.; Norris, R.L. Monitoring salivary melatonin concentrations in children with sleep disorders using liquid chromatography-tandem mass spectrometry. Ther. Drug Monit. 2013, 35, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Motoyama, A.; Kanda, T.; Namba, R. Direct determination of endogenous melatonin in human saliva by column-switching semi-microcolumn liquid chromatography/mass spectrometry with on-line analyte enrichment. Rapid Commun. Mass Spectrom. 2004, 18, 1250–1258. [Google Scholar] [CrossRef] [PubMed]
- Reiter, R.J. The Mammalian Pineal Gland: Structure and Function. Am. J. Anat. 1981, 162, 287–313. [Google Scholar] [CrossRef]
- Coon, S.L.; Zarazaga, L.A.; Malpaux, B.; Ravault, J.P.; Bodin, L.; Voisin, P.; Weller, J.L.; Klein, D.C.; Chemineau, P. Genetic variability in plasma melatonin in sheep is due to pineal weight, not to variations in enzyme activities. Am. J. Physiol. 1999, 277, E792–E797. [Google Scholar] [CrossRef]
- Kunz, D.; Schmitz, S.; Mahlberg, R.; Mohr, A.; Stoter, C.; Wolf, K.J.; Herrmann, W.M. A new concept for melatonin deficit: On pineal calcification and melatonin excretion. Neuropsychopharmacology 1999, 21, 765–772. [Google Scholar] [CrossRef]
- Lushington, K.; Dawson, D.; Encel, N.; Lack, L. Urinary 6-Sulfatoxymelatonin cycle-to-cycle variability. Chronobiol. Int. 1996, 13, 411–421. [Google Scholar] [CrossRef]
- Mahlberg, R.; Tilmann, A.; Salewski, L.; Kunz, D. Normative data on the daily profile of urinary 6-Sulfatoxymelatonin in healthy subjects between the ages of 20 and 84. Psychoneuroendocrinology 2006, 31, 634–641. [Google Scholar] [CrossRef]
- Sack, R.L.; Lewy, A.J.; Erb, D.L.; Vollmer, W.M.; Singer, C.M. Human melatonin production decreases with age. J. Pineal Res. 1986, 3, 379–388. [Google Scholar] [CrossRef] [PubMed]
- Waldhauser, F.; Weiszenbacher, G.; Tatzer, E.; Gisinger, B.; Waldhauser, M.; Schemper, M.; Frisch, H. Alterations in nocturnal serum melatonin levels in humans with growth and aging. J. Clin. Endocrinol. Metab. 1988, 66, 648–652. [Google Scholar] [CrossRef] [PubMed]
- Kennaway, D.J.; Lushington, K.; Dawson, D.; Lack, L.; Heuvel, C.; Rogers, N. Urinary 6-Sulfatoxymelatonin excretion and aging: New results and a critical review of the literature. J. Pineal Res. 1999, 27, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Vakkuri, O.; Kivelä, A.; Leppäluoto, J.; Valtonen, M.; Kauppila, A. Decrease in melatonin precedes follicle-stimulating hormone increase during perimenopause. Eur. J. Endocrinol. 1996, 135, 188–192. [Google Scholar] [CrossRef]
- Hofman, M.A.; Swaab, D.F. Alterations in circadian rhythmicity of the vasopressin-producing neurons of the human suprachiasmatic nucleus (SCN) with aging. Brain Res. 1994, 651, 134–142. [Google Scholar] [CrossRef]
- Cain, S.W.; Dennison, C.F.; Zeitzer, J.M.; Guzik, A.M.; Khalsa, S.B.; Santhi, N.; Schoen, M.W.; Czeisler, C.A.; Duffy, J.F. Sex differences in phase angle of entrainment and melatonin amplitude in humans. J. Biol. Rhythm. 2010, 25, 288–296. [Google Scholar] [CrossRef]
- Ekmekcioglu, C. Melatonin receptors in humans: Biological role and clinical relevance. Biomed. Pharm. 2006, 60, 97–108. [Google Scholar] [CrossRef]
- Luboshitzky, R.; Herer, P.; Lavie, P. Pulsatile patterns of melatonin secretion in patients with gonatotropin-releasing hormone deficiency: Effects of testosterone treatment. J. Pineal Res. 1997, 22, 95–101. [Google Scholar] [CrossRef]
- Cardinali, D.P.; Vacas, M.I. Cellular and molecular mechanisms controlling melatonin release by mammalian pineal glands. Cell. Mol. Neurobiol. 1987, 7, 323–337. [Google Scholar] [CrossRef]
- Carlson, L.A.; Pobocik, K.M.; Lawrence, M.A.; Brazeau, D.A.; Koch, A.J. Influence of exercise time of day on salivary melatonin responses. Int. J. Sports Physiol. Perform. 2019, 14, 351–353. [Google Scholar] [CrossRef]
- Lucas, R.J.; Peirson, S.N.; Berson, D.M.; Brown, T.M.; Cooper, H.M.; Czeisler, C.A.; Figueiro, M.G.; Gamlin, P.D.; Lockley, S.W.; O’Hagan, J.B.; et al. Measuring and using light in the melanopsin age. Trends Neurosci. 2014, 37, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Souman, J.L.; Borra, T.; de Goijer, I.; Schlangen, L.J.M.; Vlaskamp, B.N.S.; Lucassen, M.P. Spectral tuning of white light allows for strong reduction in melatonin suppression without changing illumination level or color temperature. J. Biol. Rhythm. 2018, 33, 420–431. [Google Scholar] [CrossRef] [PubMed]
- Chinoy, E.D.; Duffy, J.F.; Czeisler, C.A. Unrestricted evening use of light emitting tablet computers delays self-selected bedtime and disrupts circadian timing and alertness. Physiol. Rep. 2018, 6, e13692. [Google Scholar] [CrossRef] [PubMed]
- Zeitzer, J.M.; Dijk, D.-J.; Kronauer, R.E.; Brown, E.N.; Czeisler, C.A. Sensitivity of the human circadian pacemaker to nocturnal light: Melatonin phase resetting and suppression. J. Physiol. 2000, 526, 695–702. [Google Scholar] [CrossRef]
- Thapan, K.; Arendt, J.; Skene, D.J. An action spectrum for melatonin suppression: Evidence for a novel non-rod, non-cone photoreceptor system in humans. J. Physiol. 2001, 535, 261–267. [Google Scholar] [CrossRef]
- Kozaki, T.; Hidaka, Y.; Takakura, J.; Kusano, Y. Suppression of salivary melatonin secretion under 100-Hz flickering and non-flickering blue light. J. Physiol. Anthr. 2018, 37, 23. [Google Scholar] [CrossRef]
- Bojkowski, C.J.; Arendt, J. Annual changes in 6-sulphatoxymelatonin excretion in man. Acta Endocrinol. 1988, 117, 470–476. [Google Scholar] [CrossRef]
- Wehr, T.A. The durations of human melatonin secretion and sleep respond to changes in daylength (photoperiod). J. Clin. Endocrinol. Metab. 1991, 73, 1276–1280. [Google Scholar] [CrossRef]
- Buxton, O.M.; Lee, C.W.; L’Hermite-Balériaux, M.; Turek, F.W.; Van Cauter, E. Exercise elicits phase shifts and acute alterations of melatonin that vary with circadian phase. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2003, 284, R714–R724. [Google Scholar] [CrossRef]
- Buxton, O.M.; Frank, S.A.; L’Hermite-Balériaux, M.; Leproult, R.; Turek, F.W.; Van Cauter, E. Roles of intensity and duration of nocturnal exercise in causing phase delays of human circadian rhythms. Am. J. Physiol. 1997, 273, E536–E542. [Google Scholar] [CrossRef]
- Monteleone, P.; Maj, M.; Fusco, M.; Orazzo, C.; Kemali, D. Physical Exercise at night blunts the nocturnal increase of plasma melatonin levels in healthy humans. Life Sci. 1990, 47, 1989–1995. [Google Scholar] [CrossRef]
- Marrin, K.; Drust, B.; Gregson, W.; Morris, C.J.; Chester, N.; Atkinson, G. Diurnal variation in the salivary melatonin responses to exercise: Relation to exercise-mediated tachycardia. Eur. J. Appl. Physiol. 2011, 111, 2707–2714. [Google Scholar] [CrossRef] [PubMed]
- Skene, D.J.; Lockley, S.W.; Arendt, J. Melatonin in circadian sleep disorders in the bind. Biol. Signals Recept. 1999, 8, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Lockley, S.W.; Arendt, J.; Skene, D.J. Visual impairment and circadian rhythm disorders. Dialogues Clin. Neurosci. 2007, 9, 301–314. [Google Scholar] [PubMed]
- Thøfner Hultén, V.D.; Biering-Sørensen, F.; Jørgensen, N.R.; Jennum, P.J. Melatonin and cortisol in individuals with spinal cord injury. Sleep Med. 2018, 51, 92–98. [Google Scholar] [CrossRef]
- Verheggen, R.J.; Jones, H.; Nyakayiru, J.; Thompson, A.; Groothuis, J.T.; Atkinson, G.; Hopman, M.T.; Thijssen, D.H. Complete absence of evening melatonin increase in tetraplegics. FASEB J. 2012, 26, 3059–3064. [Google Scholar] [CrossRef]
- Iguchi, H.; Kato, K.I.; Ibayashi, H. Melatonin serum levels and metabolic clearance rate in patients with liver cirrhosis. J. Clin. Endocrinol. Metab. 1982, 54, 1025–1027. [Google Scholar] [CrossRef]
- Scheer, F.A.; Van Montfrans, G.A.; van Someren, E.J.; Mairuhu, G.; Buijs, R.M. Daily nightime melatonin reduces blond pressure in male patients with essential hypertension. Hypertension 2004, 43, 192–197. [Google Scholar] [CrossRef]
- Ulfberg, J.; Micic, S.; Strøm, J. Afternoon serum-melatonin in sleep disordered breathing. J. Intern. Med. 1998, 244, 163–168. [Google Scholar] [CrossRef]
- Hanly, P.J.; Gabor, J.Y.; Chan, C.; Pierratos, A. Daytime sleepiness in patients with CRF: Impact of nocturnal hemodialysis. Am. J. Kidney Dis. 2003, 41, 403–410. [Google Scholar] [CrossRef]
- Vaziri, N.D.; Oveisi, F.; Reyes, G.A.; Zhou, X.J. Dysregulation of melatonin metabolizm in chronic renal insufficiency: Role of erythropoietin-deficiency anemia. Kidney Int. 1996, 50, 653–656. [Google Scholar] [CrossRef] [PubMed]
- Koch, B.C.; van der Putten, K.; Van Someren, E.J.; Wielders, J.P.; Ter Wee, P.M.; Nagtegaal, J.E.; Gaillard, C.A. Impairment of endogenous melatonin rhythm is related to the degree of chronic kidney disease (CREAM study). Nephrol. Dial. Transpl. 2010, 25, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Ishigaki, S.; Ohashi, N.; Isobe, S.; Tsuji, N.; Iwakura, T.; Ono, M.; Sakao, Y.; Tsuji, T.; Kato, A.; Miyajima, H.; et al. Impaired endogenous nighttime melatonin secretion relates to intrarenal renin–angiotensin system activation and renal damage in patients with chronic kidney disease. Clin. Exp. Nephrol. 2016, 20, 878–884. [Google Scholar] [CrossRef] [PubMed]
- Almughrabi, O.M.; Marzouk, K.M.; Hasanato, R.M.; Shafik, S.S. Melatonin levels in periodontal health and disease. J. Periodontal Res. 2013, 48, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Srinath, R.; Acharya, A.B.; Thakur, S.L. Salivary and gingival crevicular fluid melatonin in periodontal health and disease. J. Periodontol. 2010, 81, 277–283. [Google Scholar] [CrossRef]
- Balaji, T.M.; Vasanthi, H.R.; Rao, S.R. Gingival, plasma and salivary levels of melatonin in periodontally healthy individuals and chronic periodontitis patients: A pilot study. J. Clin. Diagn. Res. 2015, 9. [Google Scholar] [CrossRef]
- Virto, L.; Haugen, H.J.; Fernandez-Mateos, P.; Cano, P.; Gonzalez, J.; Jimenez-Ortega, V.; Esquifino, A.I.; Sanz, M. Melatonin expression in periodontitis and obesity: An experimental in vivo investigation. J. Periodontal Res. 2018, 53, 825–831. [Google Scholar] [CrossRef]
- Cowen, P.J.; Bevan, J.S.; Gosden, B.; Elliott, S.A. Treatment with beta-adrenoceptor blockers reduces plasma melatonin concentration. Br. J. Clin. Pharm. 1985, 19, 258–260. [Google Scholar] [CrossRef]
- Brismar, K.; Mogensen, L.; Wetterberg, L. Depressed melatonin secretion in patients with nightmares due to beta-adrenoceptor blocking drugs. Acta Med. Scand. 1987, 221, 155–158. [Google Scholar] [CrossRef]
- Rommel, T.; Demisch, L. Influence of chronic b-adrenoreceptor blocker treatment on melatonin secretion and sleep quality in patients with essential hypertension. J. Neural Transm. Gen. Sect. 1994, 95, 39–48. [Google Scholar] [CrossRef]
- Stoschitzky, K.; Sakotnik, A.; Lercher, P.; Zweiker, R.; Maier, R.; Liebmann, P.; Linder, W. Influence of beta-blockers on melatonin release. Eur. J. Clin. Pharm. 1999, 55, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Muñóz-Hoyos, A.; Fernández-García, J.M.; Molina-Carballo, A.; Macías, M.; Escames, G.; Ruiz-Cosano, C.; Acuña-Castroviejo, D. Effect of clonidine on plasma ACTH, cortisol and melatonin in children. J. Pineal Res. 2000, 29, 48–53. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, I.M.; Burrows, G.D.; Norman, T.R. Suppression of plasma melatonin by a single dose of the benzodiazepine alprazolam in humans. Biol. Psychiatry 1988, 24, 108–112. [Google Scholar] [CrossRef]
- Copinschi, G.; Van Onderbergen, A.; L’Hermite-Balériaux, M.; Szyper, M.; Caufriez, A.; Bosson, D.; L’Hermite, M.; Robyn, C.; Turek, F.W.; Van Cauter, E. Effects of the short-acting benzodiazepine triazolam, taken at bedtime, on circadian and sleep-related hormonal profiles in normal men. Sleep 1990, 13, 232–244. [Google Scholar]
- Gupta, M.; Kohli, K.; Gupta, Y.K. Modulation of serum concentrations of melatonin by carbamazepine and valproate. Indian J. Physiol. Pharmacol. 2006, 50, 79–82. [Google Scholar]
- Praninskiene, R.; Dumalakiene, I.; Kemezys, R.; Mauricas, M.; Jucaite, A. Melatonin secretion in children with epilepsy. Epilepsy Behav. 2012, 25, 315–322. [Google Scholar] [CrossRef]
- Dabak, O.; Altun, D.; Arslan, M.; Yaman, H.; Vurucu, S.; Yesilkaya, E.; Unay, B. Evaluation of Plasma Melatonin Levels in Children With Afebrile and Febrile Seizures. Pediatr. Neurol. 2016, 57, 51–55. [Google Scholar] [CrossRef]
- Takaesu, Y.; Futenma, K.; Kobayashi, M.; Komada, Y.; Tanaka, N.; Yamashina, A.; Inoue, Y. A preliminary study on the relationships between diurnal melatonin secretion profile and sleep variables in patients emergently admitted to the coronary care unit. Chronobiol. Int. 2015, 32, 875–879. [Google Scholar] [CrossRef]
- Murphy, P.J.; Myers, B.L.; Badia, P. Nonsteroidal anti-inflammatory drugs alter body temperature and suppress melatonin in humans. Physiol. Behav. 1996, 59, 133–139. [Google Scholar] [CrossRef]
- Monteleone, P.; Forziati, D.; Orazzo, C.; Maj, M. Preliminary observations on the suppression of nocturnal plasma melatonin levels by short-term administration of diazepam in humans. J. Pineal Res. 1989, 6, 253–258. [Google Scholar] [CrossRef]
- Monteleone, P.; Tortorella, A.; Borriello, R.; Natale, M.; Cassandro, P.; Maj, M. Suppression of nocturnal plasma melatonin levels by evening administration of sodium valproate in healthy humans. Biol. Psychiatry 1997, 41, 336–341. [Google Scholar] [CrossRef]
- Skene, D.J.; Bojkowski, C.J.; Arendt, J. Comparison of the effects of acute fluvoxamine and desipramine administration on melatonin and cortisol production in humans. Br. J. Clin. Pharmacol. 1994, 37, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Kostoglou-Athanassiou, I.; Athanassiou, P.; Treacher, D.F.; Wheeler, M.J.; Forsling, M.L. Neurohypophysial hormone and melatonin secretion over the natural and suppressed menstrual cycle in premenopausal women. Clin. Endocrinol. 1998, 49, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Burgess, H.J.; Fogg, L.F. Individual differences in the amount and timing of salivary melatonin secretion. PLoS ONE 2008, 3, e3055. [Google Scholar] [CrossRef]
- Benluocif, S.; Burgess, H.J.; Klerman, E.B.; Lewy, A.J.; Middleton, B.; Murphy, P.J.; Parry, B.L.; Revell, V.L. Measuring Melatonin in Humans. J. Clin. Sleep Med. 2008, 4, 66–69. [Google Scholar] [CrossRef]


| References | Drug | Effects on Melatonin Secretion |
|---|---|---|
| Cowen PJ et al., 1985 [99] | beta-blockers (propranolol, atenolol) | lower mean melatonin concentration |
| Brismar K et al., 1987 [100] | beta-blockers | decreased night-time melatonin secretion |
| Rommel T et al., 1994 [101] | beta-blockers (propranolol, ridazolol) | decreased melatonin secretion |
| Stoschitzky K et al., 1999 [102] | beta-blockers (atenolol) | decreased melatonin secretion |
| Takaesu Y et al., 2015 [109] | beta-blockers | no significant differences |
| Muñóz-Hoyos A et al., 2000 [103] | α2 adrenergic agonist (clonidine) | decreased melatonin secretion |
| Murphy PJ et al., 1996 [110] | nonsteroidal anti-inflammatory drug (NSAIDs) (aspirin or ibuprofen) | decreased nightly melatonin secretion |
| Monteleone P et al., 1989 [111] | GABAergic drug (diazepam) | decreased night-time melatonin secretion |
| Monteleone P et al., 1997 [112] | GABAergic drug (sodium valproate) | decreased melatonin secretion |
| Gupta M et al., 2006 [106] | carbamazepine+melatonin (CBZ+MLT) valproate+melatonin (VPA+MLT) | melatonin levels in patients receiving CBZ+MLT were higher than those of the VPA+MLT recipient group The observed difference in melatonin levels could be attributed to the difference in antiepileptic drugs |
| Praninskiene R et al., 2012 [107] | antiepilepticdrugs | no significant differences |
| Dabak O et al., 2015 [108] | antiepilepticdrugs | no significant differences |
| McIntyre IM et al., 1988 [104] | benzodiazepines (alprazolam ) | decreased night-time melatonin secretion |
| Copinschi G et al., 1990 [105] | short-acting benzodiazepine (triazolam) | no significant differences |
| Claustrat B et al., 2005 [13] | monoamine oxidase inhibitors (MAO) | increased melatonin secretion |
| Claustrat B et al., 2005 [13] | tricyclic antidepressants | increased melatonin secretion |
| Skene DJ et al., 1994 [113] | the specific serotonin uptake inhibitor (fluvoxamine) | increased nocturnal plasma melatonin concentrations |
| Skene DJ et al., 1994 [113] | the noradrenaline uptake inhibitor (desipramine) | increased evening plasma melatonin concentrations |
| References | Participants | Effects on Melatonin Secretion |
|---|---|---|
| Kostoglou-Athanassiou I et al., 1998 [114] |
| overall melatonin secretion was augmented |
| Cook MR et al., 2000 [33] |
| no effect observed |
| Burgess HJ et al., 2008 [115] |
| longer duration time of melatonin secretion |
| Gunn PJ et al., 2016 [17] |
| significantly elevated plasma melatonin levels in women, no significant differences in aMT6 levels |
| Material | Determined Substances | Sampling Periods | Lighting | Body Posture | Basis for Evaluating the Circadian Rhythm Phase |
|---|---|---|---|---|---|
| urine | aMT6s | every 2 to 8 h for 24 to 48 h or the first morning urine sample | not applicable | restriction of motor activity and change of body position before and during sampling | the timing of the acrophase |
| saliva | melatonin | every 30 to 60 min starting at least one hour before and throughout the expected increase in melatonin levels | <30 lux | DLMO | |
| blood | melatonin | frequent sampling with a catheter inserted at least 2 h before the expected increase in melatonin levels | <30 lux | DLMO |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rzepka-Migut, B.; Paprocka, J. Melatonin-Measurement Methods and the Factors Modifying the Results. A Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2020, 17, 1916. https://doi.org/10.3390/ijerph17061916
Rzepka-Migut B, Paprocka J. Melatonin-Measurement Methods and the Factors Modifying the Results. A Systematic Review of the Literature. International Journal of Environmental Research and Public Health. 2020; 17(6):1916. https://doi.org/10.3390/ijerph17061916
Chicago/Turabian StyleRzepka-Migut, Beata, and Justyna Paprocka. 2020. "Melatonin-Measurement Methods and the Factors Modifying the Results. A Systematic Review of the Literature" International Journal of Environmental Research and Public Health 17, no. 6: 1916. https://doi.org/10.3390/ijerph17061916
APA StyleRzepka-Migut, B., & Paprocka, J. (2020). Melatonin-Measurement Methods and the Factors Modifying the Results. A Systematic Review of the Literature. International Journal of Environmental Research and Public Health, 17(6), 1916. https://doi.org/10.3390/ijerph17061916






