Comparing Accuracy of Implant Installation with a Navigation System (NS), a Laboratory Guide (LG), NS with LG, and Freehand Drilling
Abstract
1. Introduction
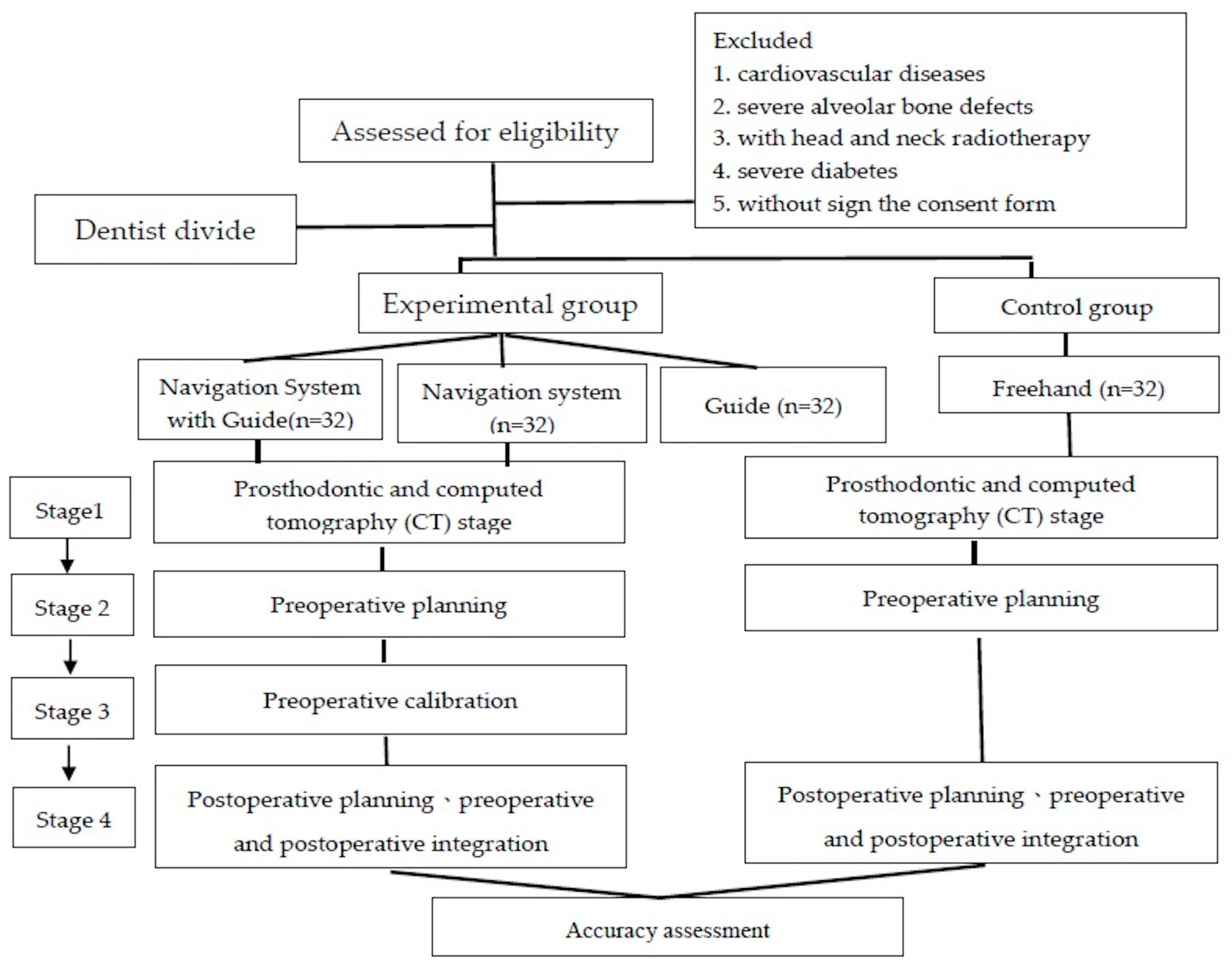
2. Materials and Methods
2.1. Main Operator
2.2. Participants Recruitment
2.3. Power Calculation
2.4. Four Dental Implant Surgery Approach
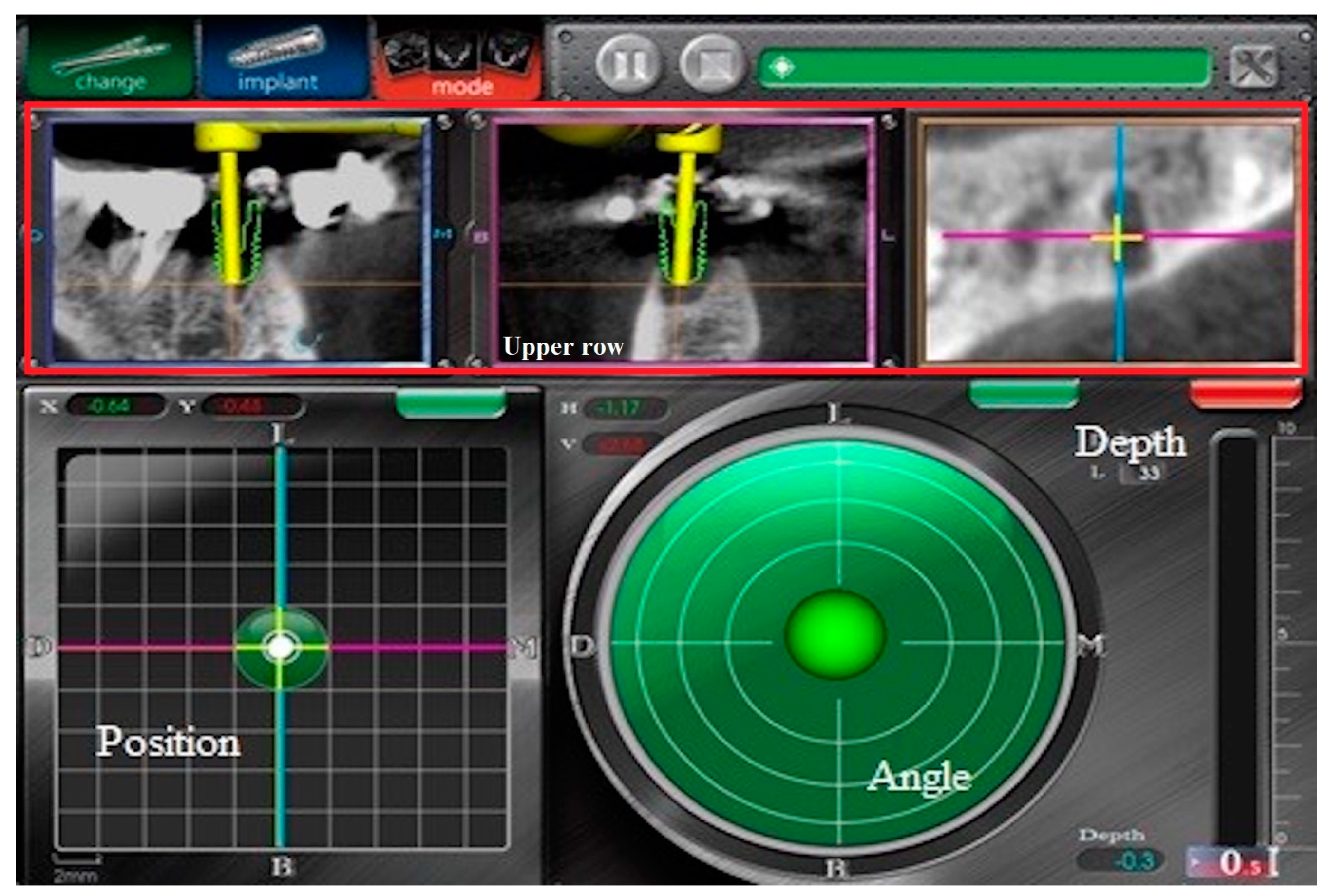
2.4.1. Navigation System
2.4.2. Computer-Guide
2.4.3. Freehand
2.5. Postsurgical Care
2.6. Operational Processes for Four Approaches
2.6.1. First Step: Prosthodontic and Computed Tomography (CT) Stage
2.6.2. Second Step: Preoperative Planning
2.6.3. Third Step: Preoperative Calibration for Navigation System and Navi with Guide
2.6.4. Fourth Step: Postoperative Planning and Preoperative and Postoperative Integration
2.7. Surgery Process
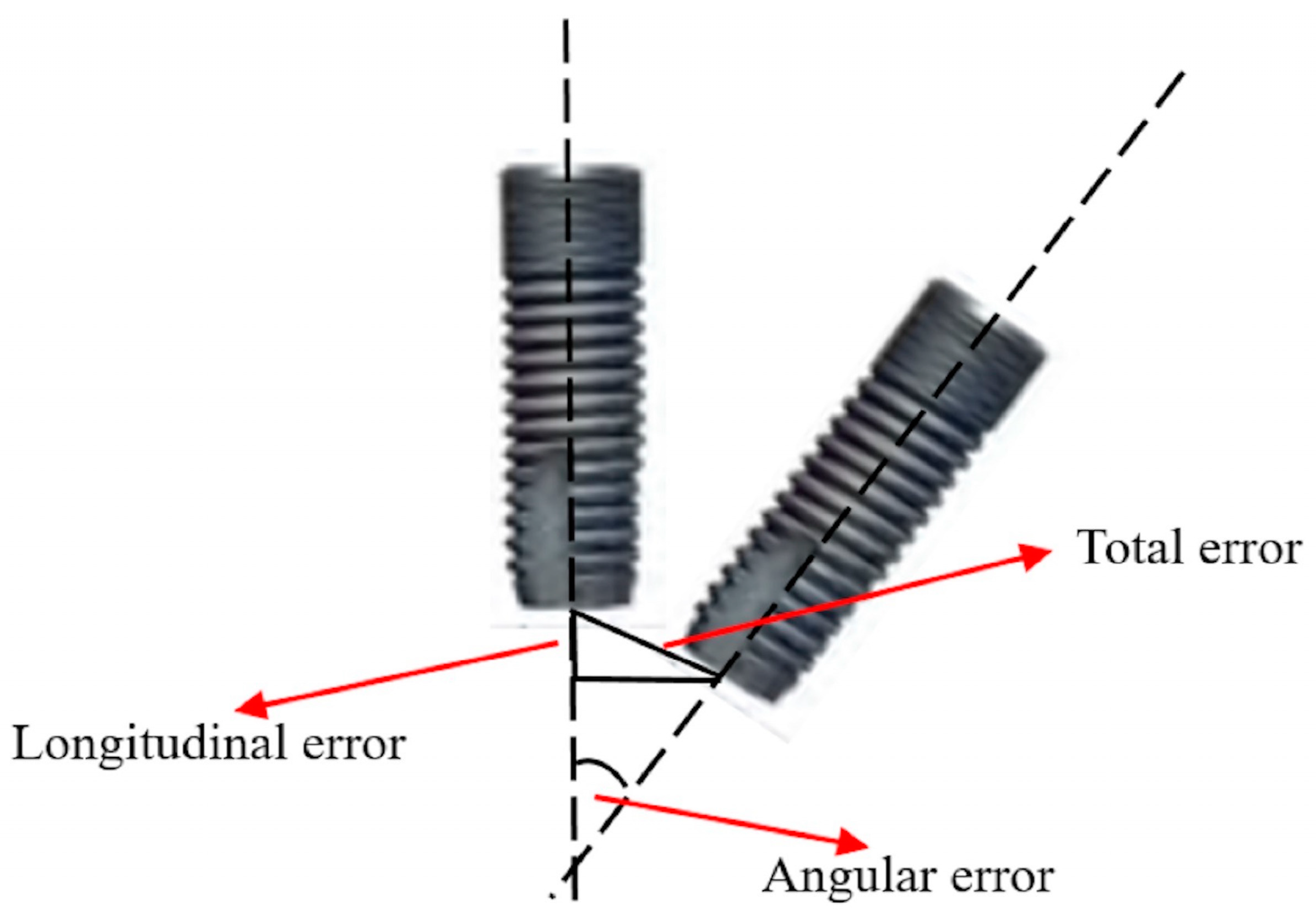
2.8. Deviation Definition
- Total Error: Point A1 was set as the origin, and vector A () was the Z-axis in space. The Pythagorean theorem was applied to obtain the 2-dimensional error between vector B () and vector A.
- Longitudinal Error: Point A1 was set as the origin, and vector A () was the Z-axis in space. The coordinate difference of the 2 points along the Z-axis was the longitudinal error.
- Angular Error (ø): The product of spatial vectors used to obtain the angle between vector A () and vector B () was the angular error.
2.9. Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Luo, Z.; Zeng, R.; Luo, Z.; Chen, Z. Single implants in the esthetic zone: Analysis of recent peri-implant soft tissue alterations and patient satisfaction. A photographic study. Int. J. Oral Maxillofac. Implants 2011, 26, 578–586. [Google Scholar] [PubMed]
- Kumar, M.; Shanavas, M.; Sidappa, A.; Kiran, M. Cone beam computed tomography—Know its secrets. J. Int. Oral Health 2015, 7, 64–68. [Google Scholar] [PubMed]
- Jacobs, R.; Salmon, B.; Codari, M.; Hassan, B.; Bornstein, M.M. Cone beam computed tomography in implant dentistry: Recommendations for clinical use. BMC Oral Health 2018, 18, 88. [Google Scholar] [CrossRef] [PubMed]
- Vercruyssen, M.; Laleman, I.; Jacobs, R.; Quirynen, M. Computer-supported implant planning and guided surgery: A narrative review. Clin. Oral Implants Res. 2015, 26, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Fortin, T.; Loup, C.J.; Champleboux, G.; Sautot, P.; Lavallée, S. Computer-Assisted Dental Implant Surgery Using Computed Tomography. J. Image Guid. Surg. 1995, 1, 53–58. [Google Scholar] [CrossRef]
- Tahmaseb, A.; Wismeijer, D.; Coucke, W.; Derksen, W. Computer technology applications in surgical implant dentistry: A systematic review. Int. J. Oral Maxillofac. Implants 2014, 29, 25–42. [Google Scholar] [CrossRef]
- Brief, J.; Edinger, D.; Hassfeld, S.; Eggers, G. Accuracy of image-guided implantology. Clin. Oral Implants Res. 2005, 16, 495–501. [Google Scholar] [CrossRef]
- Bouchard, C.; Magill, J.C.; Nikonovskiy, V.; Byl, M.; Murphy, B.A.; Kaban, L.B. Osteomark: A surgical navigation system for oral and maxillofacial surgery. J. Oral Maxillofac. Surg. 2012, 41, 265–270. [Google Scholar] [CrossRef]
- Nijmeh, A.D.; Goodger, N.M.; Hawkes, D.; Edwards, P.J.; McGurk, M. Image-guided navigation in oral and maxillofacial surgery. Br. J. Oral Maxillofac. Surg. 2005, 43, 294–302. [Google Scholar] [CrossRef]
- Strong, E.B.; Rafii, A.; Holhweg-Majert, B.; Fuller, S.C.; Metzger, M.C. Comparison of 3 optical navigation systems for computer-aided maxillofacial surgery. Arch. Otolaryngol. Head Neck. Surg. 2008, 134, 1080–1084. [Google Scholar] [CrossRef]
- Wittwer, G.; Adeyemo, W.L.; Schicho, K.; Birkfellner, W.; Enislidis, G. Prospective randomized clinical comparison of 2 dental implant navigation systems. Int. J. Oral Maxillofac. Implants 2007, 22, 785–790. [Google Scholar] [PubMed]
- Poeschl, P.W.; Schmidt, N.; Guevara-Rojas, G.; Seemann, R.; Ewers, R.; Zipko, H.T. Comparison of cone-beam and conventional multislice computed tomography for image-guided dental implant planning. Clin. Oral Investig. 2013, 17, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Cagir, B.; Rangraj, M.; Maffuci, L.; Herz, B.L. The learning curve for laparoscopic cholecystectomy. J. Laparoendosc. Surg. 1994, 4, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Hatlie, M.J. Climbing ‘the learning curve’. New technologies, emerging obligations. JAMA 1993, 270, 1364–1365. [Google Scholar] [CrossRef]
- Pernar, L.I.M.; Robertson, F.C.; Tavakkoli, A.; Sheu, E.G.; Brooks, D.C.; Smink, D.S. An appraisal of the learning curve in robotic general surgery. Surg. Endosc. 2017, 31, 4583–4596. [Google Scholar] [CrossRef]
- Elsey, E.J.; Griffiths, G.; Humes, D.J.; West, J. Meta-analysis of operative experiences of general surgery trainees during training. Br. J. Surg. 2017, 104, 22–33. [Google Scholar] [CrossRef]
- Pedersen, R.C.; Li, Y.; Chang, J.S.; Lew, W.K.; Patel, K.K. Effect of Endovascular Interventions on General Surgery Trainee Operative Experience; a Comparison of Case Log Reports. Ann. Vasc. Surg. 2016, 33, 98–102. [Google Scholar] [CrossRef]
- Karami, D.; Alborzinia, H.R.; Amid, R.; Kadkhodazadeh, M.; Yousefi, N.; Badakhshan, S. In-Office Guided Implant Placement for Prosthetically Driven Implant Surgery. Craniomaxillofac. Trauma. Reconstr. 2017, 10, 246–254. [Google Scholar] [CrossRef]
- Stefanelli, L.V.; DeGroot, B.S.; Lipton, D.I.; Mandelaris, G.A. Accuracy of a Dynamic Dental Implant Navigation System in a Private Practice. Int. J. Oral Maxillofac. Implants 2019, 34, 205–213. [Google Scholar] [CrossRef]
- Chen, C.K.; Yuh, D.Y.; Huang, R.Y.; Fu, E.; Tsai, C.F.; Chiang, C.Y. Accuracy of Implant Placement with a Navigation System, a Laboratory Guide, and Freehand Drilling. Int. J. Oral Maxillofac. Implants 2018, 33, 1213–1218. [Google Scholar] [CrossRef]
- Widmann, G.; Bale, R.J. Accuracy in computer-aided implant surgery—A review. Int. J. Oral Maxillofac. Implants 2006, 21, 305–313. [Google Scholar] [PubMed]
- Kaewsiri, D.; Panmekiate, S.; Subbalekha, K.; Mattheos, N.; Pimkhaokham, A. The accuracy of static vs. dynamic computer-assisted implant surgery in single tooth space: A randomized controlled trial. Clin. Oral Implants Res. 2019, 30, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Schneider, D.; Marquardt, P.; Zwahlen, M.; Jung, R.E. A systematic review on the accuracy and the clinical outcome of computer-guided template-based implant dentistry. Clin. Oral Implants Res. 2009, 20, 73–86. [Google Scholar] [CrossRef] [PubMed]
- Block, M.S.; Emery, R.W.; Lank, K.; Ryan, J. Implant Placement Accuracy Using Dynamic Navigation. Int. J. Oral Maxillofac. Implants 2017, 32, 92–99. [Google Scholar] [CrossRef]
- Somogyi-Ganss, E.; Holmes, H.I.; Jokstad, A. Accuracy of a novel prototype dynamic computer-assisted surgery system. Clin. Oral Implants Res. 2015, 26, 882–890. [Google Scholar] [CrossRef]
- Tallarico, M.; Kim, Y.J.; Cocchi, F.; Martinolli, M.; Meloni, S.M. Accuracy of newly developed sleeve-designed templates for insertion of dental implants: A prospective multicenters clinical trial. Clin. Implant Dent. Relat. Res. 2018, 21, 108–113. [Google Scholar] [CrossRef]
- Emery, R.W.; Merritt, S.A.; Lank, K.; Gibbs, J.D. Accuracy of Dynamic Navigation for Dental Implant Placement-Model-Based Evaluation. J. Oral. Implantol. 2016, 42, 399–405. [Google Scholar] [CrossRef]
- Casap, N.; Wexler, A.; Eliashar, R. Computerized navigation for surgery of the lower jaw: Comparison of 2 navigation systems. J. Oral Maxillofac. Surg. 2008, 66, 1467–1475. [Google Scholar] [CrossRef]
- Vasak, C.; Watzak, G.; Gahleitner, A.; Strbac, G.; Schemper, M.; Zechner, W. Computed tomography-based evaluation of template (NobelGuide)-guided implant positions: A prospective radiological study. Clin. Oral Implants Res. 2011, 22, 1157–1163. [Google Scholar] [CrossRef]
- Fang, Y.; An, X.; Jeong, S.M.; Choi, B.H. Accuracy of computer-guided implant placement in anterior regions. J. Prosthet Dent. 2019, 121, 836–842. [Google Scholar] [CrossRef]
- Sun, T.M.; Lan, T.H.; Pan, C.Y.; Lee, H.E. Dental implant navigation system guide the surgery future. Kaohsiung. J. Med. Sci. 2018, 34, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Rungcharassaeng, K.; Caruso, J.M.; Kan, J.Y.; Schutyser, F.; Boumans, T. Accuracy of computer-guided surgery: A comparison of operator experience. J. Prosthet Dent. 2015, 114, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Cushen, S.E.; Turkyilmaz, I. Impact of operator experience on the accuracy of implant placement with stereolithographic surgical templates: An in vitro study. J. Prosthet Dent. 2013, 109, 248–254. [Google Scholar] [CrossRef]
- Cassetta, M.; Stefanelli, L.V.; Giansanti, M.; Calasso, S. Accuracy of implant placement with a stereolithographic surgical template. Int. J. Oral Maxillofac. Implants 2012, 27, 655–663. [Google Scholar] [PubMed]
| Deviation | Navigation and Surgical Stent | Navigation | Surgical Stent | Freehand | p-Value * | Multiple Comparison | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Error | Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | ||
| Total (mm) | 0.98 ± 0.19 | 0.91–1.05 | 1.25 ± 0.09 | 1.22–1.28 | 1.49 ± 0.08 | 1.47–1.53 | 1.89 ± 0.09 | 1.86–1.93 | <0.0001 # | NS > N > S > F |
| Longitudinal (mm) | 0.52 ± 0.20 | 0.44–0.59 | 0.73 ± 0.13 | 0.68–0.77 | 1.00 ± 0.15 | 0.96–1.06 | 1.42 ± 0.25 | 1.51–1.33 | <0.0001 # | NS > N > S > F |
| Angular (degree) | 2.20 ± 0.38 | 2.06–2.34 | 3.24 ± 0.36 | 3.11–3.38 | 4.54 ± 0.29 | 4.43–4.65 | 6.12 ± 0.12 | 6.08–6.17 | <0.0001 # | NS > N > S > F |
| Prepare Time | 30 min | 20 min | 15 min | 10 min | ||||||
| Total Error (mm) | Longitudinal Error (mm) | Angular Error (degree) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | 95% CI | p-Value * | Mean ± SD | 95% CI | p-Value * | Mean ± SD | 95% CI | p-Value * | |
| Experimental group | |||||||||
| Maxillary | 1.15 ± 0.26 | 1.08–1.23 | 0.0003 * | 0.63 ± 0.24 | 0.56–0.69 | <0.0001 * | 3.07 ± 0.99 | 2.78–3.36 | 0.0123 * |
| Mandible | 1.33 ± 0.20 | 1.27–1.39 | 0.88 ± 0.22 | 0.81–0.94 | 3.59 ± 0.99 | 3.29–3.88 | |||
| Anterior | 1.19 ± 0.26 | 1.11–1.26 | 0.0377 * | 0.69 ± 0.26 | 0.61–0.76 | 0.0150 * | 3.19 ± 1.02 | 2.89–3.49 | 0.2029 |
| Posterior | 1.29 ± 0.22 | 1.23–1.36 | 0.81 ± 0.25 | 0.74–0.89 | 3.46 ± 1.01 | 3.17–3.76 | |||
| Control group | |||||||||
| Maxillary | 1.82 ± 0.04 | 1.79–1.84 | <0.0001 * | 1.21 ± 0.09 | 1.16–1.25 | <0.0001 * | 6.02 ± 0.04 | 6.01–6.05 | <0.0001 * |
| Mandible | 1.97 ± 0.07 | 1.93–2.01 | 1.63 ± 0.17 | 1.53–1.71 | 6.22 ± 0.09 | 6.17–6.27 | |||
| Anterior | 1.85 ± 0.07 | 1.81–1.88 | 0.0050 * | 1.31 ± 0.19 | 1.21–1.41 | 0.0170 * | 6.07 ± 0.09 | 6.03–6.12 | 0.0130 * |
| Posterior | 1.94 ± 0.09 | 1.88–1.99 | 1.52 ± 0.26 | 1.38–1.66 | 6.18 ± 0.13 | 6.11–6.24 | |||
| Tooth Position | Navigation and Surgical Stent | Navigation | Surgical Stent | Freehand | p-Value * | Multiple Comparison | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | |||
| Maxillary | <0.0001 # | |||||||||
| Total (mm) | 1.12 ± 0.13 | 1.05–1.19 | 1.31 ± 0.04 | 1.29–1.33 | 1.56 ± 0.05 | 1.54–1.59 | 1.82 ± 0.04 | 1.79–1.84 | NS > N > S > F | |
| Longitudinal (mm) | 0.66 ± 0.14 | 0.58–0.74 | 0.84 ± 0.07 | 0.80–0.87 | 1.13 ± 0.08 | 1.08–1.17 | 1.21 ± 0.09 | 1.16–1.25 | NS > N > S > F | |
| Angular (degree) | 2.43 ± 0.33 | 2.26–2.61 | 3.56 ± 0.24 | 3.43–3.69 | 4.77 ± 0.07 | 4.73–4.81 | 6.02 ± 0.04 | 6.01–6.05 | NS > N > S > F | |
| Mandible | <0.0001 # | |||||||||
| Total (mm) | 0.84 ± 0.13 | 0.78–0.91 | 1.18 ± 0.07 | 1.15–1.22 | 1.44 ± 0.03 | 1.42–1.45 | 1.97 ± 0.07 | 1.93–2.01 | NS > N > S > F | |
| Longitudinal (mm) | 0.37 ± 0.15 | 0.29–0.45 | 0.61 ± 0.06 | 0.58–0.64 | 0.89 ± 0.09 | 0.85–0.94 | 1.63 ± 0.17 | 1.53–1.71 | NS > N > S > F | |
| Angular (degree) | 1.97 ± 0.29 | 1.82–2.13 | 2.93 ± 0.12 | 2.87–2.99 | 4.31 ± 0.24 | 4.18–4.44 | 6.22 ± 0.09 | 6.17–6.27 | NS > N > S > F | |
| Anterior | <0.0001 # | |||||||||
| Total (mm) | 0.90 ± 0.18 | 0.80–1.00 | 1.20 ± 0.09 | 1.16–1.25 | 1.46 ± 0.06 | 1.43–1.49 | 1.85 ± 0.07 | 1.81–1.88 | NS > N > S > F | |
| Longitudinal (mm) | 0.45 ± 0.21 | 0.33–0.56 | 0.68 ± 0.12 | 0.61–0.74 | 0.94 ± 0.13 | 0.87–1.01 | 1.31 ± 0.19 | 1.21–1.41 | NS > N > S > F | |
| Angular (degree) | 2.07 ± 0.37 | 1.87–2.27 | 3.10 ± 0.29 | 2.95–3.26 | 4.41 ± 0.33 | 4.24–4.59 | 6.07 ± 0.09 | 6.03–6.12 | NS > N > S > F | |
| Posterior | <0.0001 # | |||||||||
| Total (mm) | 1.06 ± 0.16 | 0.97–1.14 | 1.29 ± 0.06 | 1.26–1.32 | 1.54 ± 0.08 | 1.49–1.58 | 1.94 ± 0.09 | 1.88–1.99 | NS > N > S > F | |
| Longitudinal (mm) | 0.59 ± 0.17 | 0.49–0.68 | 0.78 ± 0.13 | 0.71–0.84 | 1.08 ± 0.13 | 1.01–1.15 | 1.52 ± 0.26 | 1.38–1.66 | NS > N > S > F | |
| Angular (degree) | 2.34 ± 0.36 | 2.14–2.53 | 3.39 ± 0.39 | 3.17–3.59 | 4.67 ± 0.18 | 4.57–4.76 | 6.18 ± 0.13 | 6.11–6.24 | NS > N > S > F | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, T.-M.; Lee, H.-E.; Lan, T.-H. Comparing Accuracy of Implant Installation with a Navigation System (NS), a Laboratory Guide (LG), NS with LG, and Freehand Drilling. Int. J. Environ. Res. Public Health 2020, 17, 2107. https://doi.org/10.3390/ijerph17062107
Sun T-M, Lee H-E, Lan T-H. Comparing Accuracy of Implant Installation with a Navigation System (NS), a Laboratory Guide (LG), NS with LG, and Freehand Drilling. International Journal of Environmental Research and Public Health. 2020; 17(6):2107. https://doi.org/10.3390/ijerph17062107
Chicago/Turabian StyleSun, Ting-Mao, Huey-Er Lee, and Ting-Hsun Lan. 2020. "Comparing Accuracy of Implant Installation with a Navigation System (NS), a Laboratory Guide (LG), NS with LG, and Freehand Drilling" International Journal of Environmental Research and Public Health 17, no. 6: 2107. https://doi.org/10.3390/ijerph17062107
APA StyleSun, T.-M., Lee, H.-E., & Lan, T.-H. (2020). Comparing Accuracy of Implant Installation with a Navigation System (NS), a Laboratory Guide (LG), NS with LG, and Freehand Drilling. International Journal of Environmental Research and Public Health, 17(6), 2107. https://doi.org/10.3390/ijerph17062107





