Physical Fitness and Self-Rated Health in Children and Adolescents: Cross-Sectional and Longitudinal Study
Abstract
:1. Introduction
2. Methods
2.1. Study Design, Settings, and Participants
2.2. Measurements
2.2.1. Physical Characteristics
2.2.2. Self-Rated Health (SRH)
2.2.3. Physical Fitness
2.3. Statistical Analysis
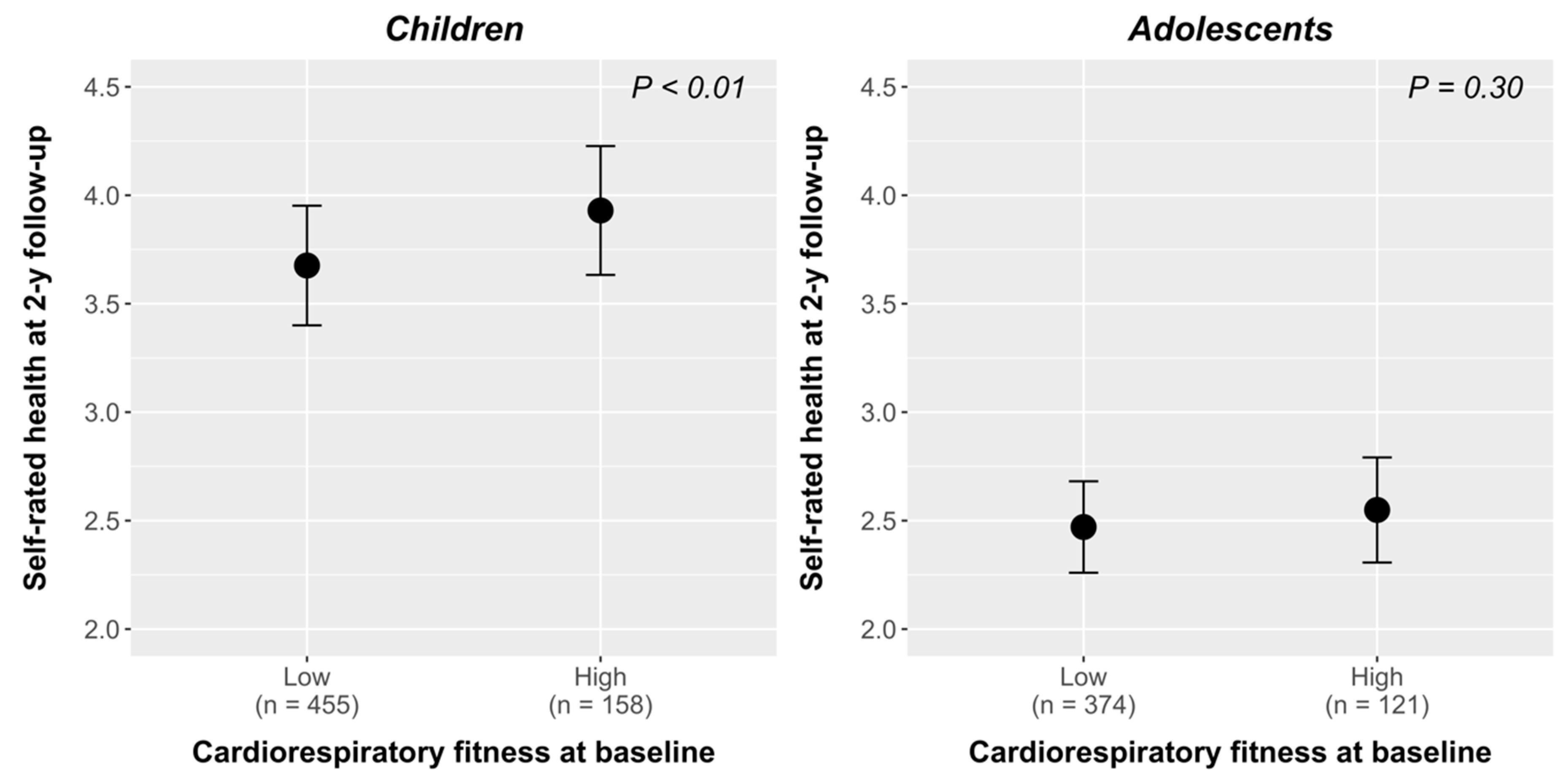
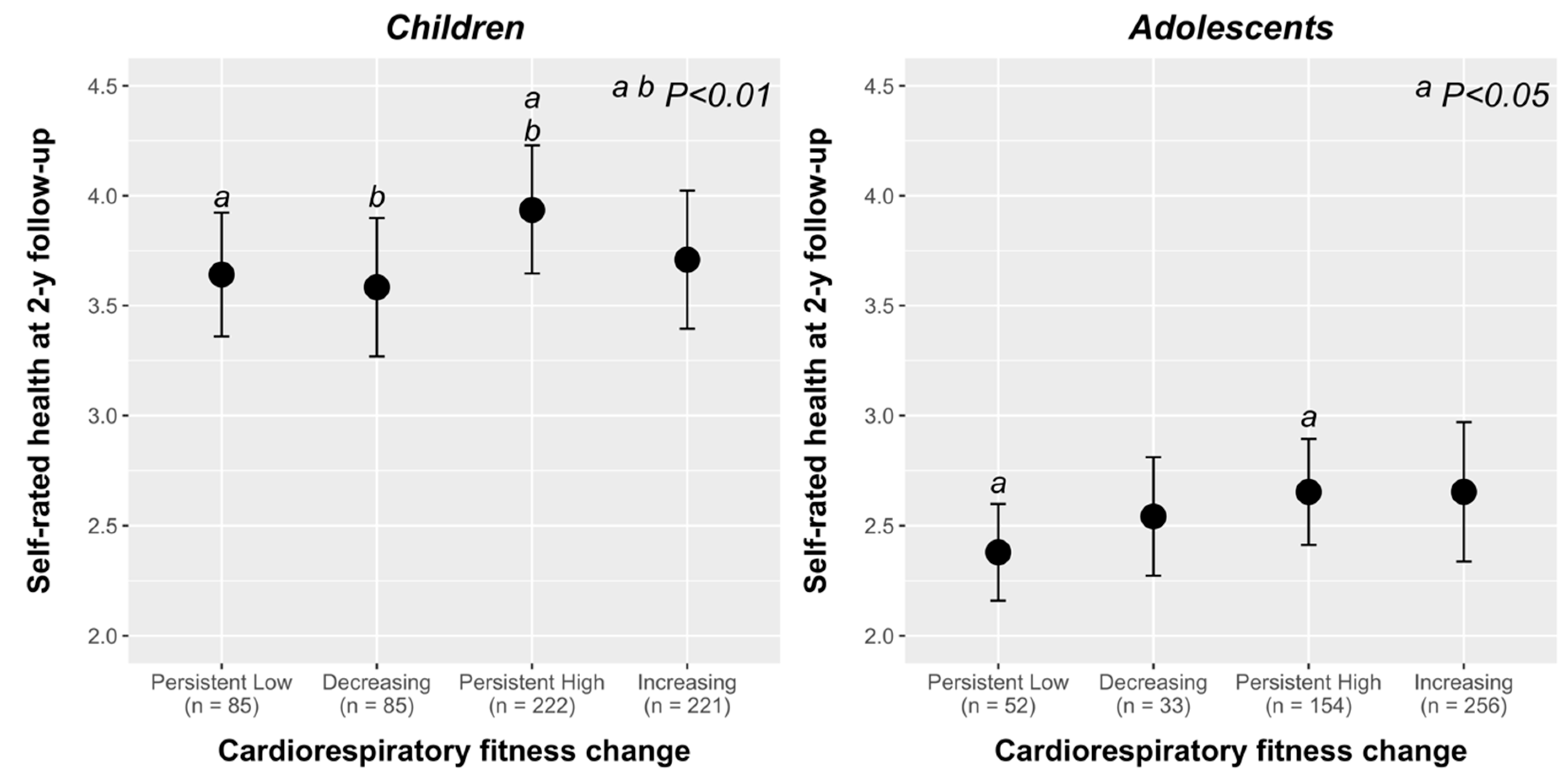
3. Results
4. Discussion
Strengths and limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethics Approval
Provenance and Peer Review
References
- Idler, E.L.; Benyamini, Y. Self-rated health and mortality: A review of twenty-seven community studies. J. Health Soc. Behav. 1997, 38, 21–37. [Google Scholar] [CrossRef] [Green Version]
- Gander, J.; Lee, D.C.; Sui, X.; Hebert, J.R.; Hooker, S.P.; Blair, S.N. Self-rated health status and cardiorespiratory fitness as predictors of mortality in men. Br. J. Sports Med. 2011, 45, 1095–1100. [Google Scholar] [CrossRef] [PubMed]
- Mechanic, D.; Hansell, S. Adolescent competence, psychological well-being, and self-assessed physical health. J. Health Soc. Behav. 1987, 28, 364–374. [Google Scholar] [CrossRef] [PubMed]
- Zullig, K.J.; Valois, R.F.; Huebner, E.S.; Drane, J.W. Adolescent health-related quality of life and perceived satisfaction with life. Qual. Life Res. 2005, 14, 1573–1584. [Google Scholar] [CrossRef] [PubMed]
- Heard, H.E.; Gorman, B.K.; Kapinus, C.A. Family Structure and Self-Rated Health in Adolescence and Young Adulthood. Popul. Res. Policy Rev. 2008, 27, 773. [Google Scholar] [CrossRef]
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Sjostrom, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. (Lond.) 2008, 32, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Ruiz, J.R.; Castro-Pinero, J.; Artero, E.G.; Ortega, F.B.; Sjostrom, M.; Suni, J.; Castillo, M.J. Predictive validity of health-related fitness in youth: A systematic review. Br. J. Sports Med. 2009, 43, 909–923. [Google Scholar] [CrossRef]
- Castro-Pinero, J.; Perez-Bey, A.; Segura-Jimenez, V.; Aparicio, V.A.; Gomez-Martinez, S.; Izquierdo-Gomez, R.; Marcos, A.; Ruiz, J.R. Cardiorespiratory Fitness Cutoff Points for Early Detection of Present and Future Cardiovascular Risk in Children: A 2-Year Follow-up Study. Mayo Clin. Proc. 2017, 92, 1753–1762. [Google Scholar] [CrossRef]
- Henriksson, P.; Henriksson, H.; Tynelius, P.; Berglind, D.; Lof, M.; Lee, I.M.; Shiroma, E.J.; Ortega, F.B. Fitness and Body Mass Index during Adolescence and Disability Later in Life: A Cohort Study. Ann. Intern. Med. 2019, 170, 230–239. [Google Scholar] [CrossRef]
- Kantomaa, M.T.; Tammelin, T.; Ebeling, H.; Stamatakis, E.; Taanila, A. High levels of physical activity and cardiorespiratory fitness are associated with good self-rated health in adolescents. J. Phys. Act. Health 2015, 12, 266–272. [Google Scholar] [CrossRef]
- Mota, J.; Santos, R.M.; Silva, P.; Aires, L.; Martins, C.; Vale, S. Associations between self-rated health with cardiorespiratory fitness and obesity status among adolescent girls. J. Phys. Act. Health 2012, 9, 378–381. [Google Scholar] [CrossRef] [PubMed]
- Padilla-Moledo, C.; Castro-Pinero, J.; Ortega, F.B.; Mora, J.; Marquez, S.; Sjostrom, M.; Ruiz, J.R. Positive health, cardiorespiratory fitness and fatness in children and adolescents. Eur. J. Public Health 2011, 22, 52–56. [Google Scholar] [CrossRef] [Green Version]
- Morales, P.F.; Sanchez-Lopez, M.; Moya-Martinez, P.; Garcia-Prieto, J.C.; Martinez-Andres, M.; Garcia, N.L.; Martinez-Vizcaino, V. Health-related quality of life, obesity, and fitness in schoolchildren: The Cuenca study. Qual. Life Res. 2013, 22, 1515–1523. [Google Scholar] [CrossRef] [PubMed]
- Andersen, J.R.; Natvig, G.K.; Aadland, E.; Moe, V.F.; Kolotkin, R.L.; Anderssen, S.A.; Resaland, G.K. Associations between health-related quality of life, cardiorespiratory fitness, muscle strength, physical activity and waist circumference in 10-year-old children: The ASK study. Qual. Life Res. 2017, 26, 3421–3428. [Google Scholar] [CrossRef] [PubMed]
- Padilla-Moledo, C.; Ruiz, J.R.; Ortega, F.B.; Mora, J.; Castro-Pinero, J. Associations of muscular fitness with psychological positive health, health complaints, and health risk behaviors in Spanish children and adolescents. J. Strength Cond. Res. 2012, 26, 167–173. [Google Scholar] [CrossRef]
- Lubans, D.R.; Morgan, P.J.; Cliff, D.P.; Barnett, L.M.; Okely, A.D. Fundamental movement skills in children and adolescents: Review of associated health benefits. Sports Med. 2010, 40, 1019–1035. [Google Scholar] [CrossRef] [Green Version]
- Jylha, M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc. Sci. Med. 2009, 69, 307–316. [Google Scholar] [CrossRef]
- Bjorner, J.; Kristensen, T.; Orth-Gomer, K.; Tibblin, G.; Sullivan, M.; Westerholm, P. Self-Rated Health: A Useful Concept in Research, Prevention, and Clinical Medicine; Swedish Council for Planning and Coordination of Research: Stockholm, Sweden, 1996. [Google Scholar]
- Palacios-Cena, D.; Alonso-Blanco, C.; Jimenez-Garcia, R.; Hernandez-Barrera, V.; Carrasco-Garrido, P.; Pileno-Martinez, E.; Fernandez-de-Las-Penas, C. Time trends in leisure time physical activity and physical fitness in elderly people: 20 year follow-up of the Spanish population national health survey (1987–2006). BMC Public Health 2011, 11, 799. [Google Scholar] [CrossRef] [Green Version]
- Starr, J.M.; Deary, I.J.; Macintyre, S. Associations with successful ageing in the “Healthy Old People in Edinburgh” cohort: Being well, fit and healthy. Aging Clin. Exp. Res. 2003, 15, 336–342. [Google Scholar] [CrossRef]
- Castro-Pinero, J.; Carbonell-Baeza, A.; Martinez-Gomez, D.; Gomez-Martinez, S.; Cabanas-Sanchez, V.; Santiago, C.; Veses, A.M.; Bandres, F.; Gonzalez-Galo, A.; Gomez-Gallego, F.; et al. Follow-up in healthy schoolchildren and in adolescents with Down syndrome: Psycho-environmental and genetic determinants of physical activity and its impact on fitness, cardiovascular diseases, inflammatory biomarkers and mental health; the UP&DOWN study. BMC Public Health 2014, 14, 400. [Google Scholar]
- Ruiz, J.R.; Espana Romero, V.; Castro Pinero, J.; Artero, E.G.; Ortega, F.B.; Cuenca Garcia, M.; Jimenez Pavon, D.; Chillon, P.; Girela Rejon, M.J.; Mora, J.; et al. ALPHA-fitness test battery: Health-related field-based fitness tests assessment in children and adolescents. Nutr. Hosp. 2011, 26, 1210–1214. [Google Scholar]
- Tanner, J.M.; Whitehouse, R.H. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch. Dis. Child. 1976, 51, 170–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lämmle, L.; Woll, A.; Mensik, G.; Bös, K. Distal and proximal factors of health behaviors and their associations with health in children and adolescents. Int. J. Environ. Res. Public Heatlh 2013, 10, 2944–2978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanchez-Oliva, D.; Leech, R.M.; Grao-Cruces, A.; Esteban-Cornejo, I.; Padilla-Moledo, C.; Veiga, O.L.; Cabanas-Sanchez, V.; Castro-Pinero, J. Does modality matter? A latent profile and transition analysis of sedentary behaviours among school-aged youth: The UP&DOWN study. J. Sports Sci. 2020, 1–8. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Castro-Pinero, J.; Espana-Romero, V.; Artero, E.G.; Ortega, F.B.; Cuenca, M.M.; Jimenez-Pavon, D.; Chillon, P.; Girela-Rejon, M.J.; Mora, J.; et al. Field-based fitness assessment in young people: The ALPHA health-related fitness test battery for children and adolescents. Br. J. Sports Med. 2011, 45, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Castro-Pinero, J.; Artero, E.G.; Espana-Romero, V.; Ortega, F.B.; Sjostrom, M.; Suni, J.; Ruiz, J.R. Criterion-related validity of field-based fitness tests in youth: A systematic review. Br. J. Sports Med. 2010, 44, 934–943. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Artero, E.G.; Ruiz, J.R.; Vicente-Rodriguez, G.; Bergman, P.; Hagstromer, M.; Ottevaere, C.; Nagy, E.; Konsta, O.; Rey-Lopez, J.P.; et al. Reliability of health-related physical fitness tests in European adolescents. The HELENA Study. Int. J. Obes. (Lond.) 2008, 32 (Suppl. 5), S49–S57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Espana-Romero, V.; Ortega, F.B.; Vicente-Rodriguez, G.; Artero, E.G.; Rey, J.P.; Ruiz, J.R. Elbow position affects handgrip strength in adolescents: Validity and reliability of Jamar, DynEx, and TKK dynamometers. J. Strength Cond. Res. 2010, 24, 272–277. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Espana-Romero, V.; Ortega, F.B.; Sjostrom, M.; Castillo, M.J.; Gutierrez, A. Hand span influences optimal grip span in male and female teenagers. J. Hand. Surg. Am. 2006, 31, 1367–1372. [Google Scholar] [CrossRef]
- Christensen, R.H.B. Ordinal—Regression Models for Ordinal Data. R Package Version 2018.8-25. 2018. Available online: http://www.cran.r-project.org/package=ordinal/ (accessed on 29 March 2020).
- Ruiz, J.R.; Cavero-Redondo, I.; Ortega, F.B.; Welk, G.J.; Andersen, L.B.; Martinez-Vizcaino, V. Cardiorespiratory fitness cut points to avoid cardiovascular disease risk in children and adolescents; what level of fitness should raise a red flag? A systematic review and meta-analysis. Br. J. Sports Med. 2016, 50, 1451–1458. [Google Scholar] [CrossRef]
- Russell, L. Emmeans: Estimated Marginal Means, aka Least-Squares Means. R Package Version 1.1. Secondary Emmeans: Estimated Marginal Means, aka Least-Squares Means. R package version 1.1. 2019. Available online: https://CRAN.R-project.org/package=emmeans (accessed on 29 March 2020).
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2017; Available online: http://www.R-project.org/ (accessed on 29 March 2020).
- Arnett, J.J. Adolescent storm and stress, reconsidered. Am. Psychol. 1999, 54, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Adkins, D.L.; Boychuk, J.; Remple, M.S.; Kleim, J.A. Motor training induces experience-specific patterns of plasticity across motor cortex and spinal cord. J. Appl. Physiol. (1985) 2006, 101, 1776–1782. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.J.; Park, I.; Lee, H.J.; Lee, O. The reliability and validity of gait speed with different walking pace and distances against general health, physical function, and chronic disease in aged adults. J. Exerc. Nutr. Biochem. 2016, 20, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Starr, J.M.; McGurn, B.; Whiteman, M.; Pattie, A.; Whalley, L.J.; Deary, I.J.; Starr, J.M.; Deary, I.J.; Macintyre, S.; Shenkin, S.D.; et al. Life long changes in cognitive ability are associated with prescribed medications in old age. Int. J. Geriatr. Psychiatry 2004, 19, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Vingilis, E.R.; Wade, T.J.; Seeley, J.S. Predictors of adolescent self-rated health. Analysis of the National Population Health Survey. Can. J. Public Health 2002, 93, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Wade, T.J.; Pevalin, D.J.; Vingilis, E. Revisiting student self-rated physical health. J. Adolesc. 2000, 23, 785–791. [Google Scholar] [CrossRef]
- Bugge, A.; El-Naaman, B.; McMurray, R.G.; Froberg, K.; Andersen, L.B. Tracking of clustered cardiovascular disease risk factors from childhood to adolescence. Pediatr. Res. 2013, 73, 245–249. [Google Scholar] [CrossRef]
- Kristensen, P.L.; Wedderkopp, N.; Moller, N.C.; Andersen, L.B.; Bai, C.N.; Froberg, K. Tracking and prevalence of cardiovascular disease risk factors across socio-economic classes: A longitudinal substudy of the European Youth Heart Study. BMC Public Health 2006, 6, 20. [Google Scholar] [CrossRef] [Green Version]
- Andersen, L.B.; Haraldsdottir, J. Tracking of cardiovascular disease risk factors including maximal oxygen uptake and physical activity from late teenage to adulthood. An 8-year follow-up study. J. Intern. Med. 1993, 234, 309–315. [Google Scholar] [CrossRef]
- Dwyer, T.; Magnussen, C.G.; Schmidt, M.D.; Ukoumunne, O.C.; Ponsonby, A.L.; Raitakari, O.T.; Zimmet, P.Z.; Blair, S.N.; Thomson, R.; Cleland, V.J.; et al. Decline in physical fitness from childhood to adulthood associated with increased obesity and insulin resistance in adults. Diabetes Care 2009, 32, 683–687. [Google Scholar] [CrossRef] [Green Version]
- Heistaro, S.; Jousilahti, P.; Lahelma, E.; Vartiainen, E.; Puska, P. Self rated health and mortality: A long term prospective study in eastern Finland. J. Epidemiol. Community Health 2001, 55, 227–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, R.M.; Simonek, J.; Ihász, F.; Hantiu, I.; Uvacsek, M.; Kalabiska, I.; Klarova, R. Self-rated health, psychosocial functioning, and other dimensions of adolescent health in Central and Eastern European adolescents. Eur. J. Psychiatry 2009, 23, 101–114. [Google Scholar] [CrossRef] [Green Version]
- Ganna, A.; Ingelsson, E. 5 year mortality predictors in 498,103 UK Biobank participants: A prospective population-based study. Lancet 2015, 386, 533–540. [Google Scholar] [CrossRef]
| Children | Adolescents | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Baseline | 2-year Follow-Up | Baseline | 2-year Follow-Up | |||||||||
| (n = 687) | (n = 613) | p | (n = 691) | (n = 495) | p | ||||||||
| Physical characteristics | |||||||||||||
| Age (years) | 10.63 | (1.37) | 12.59 | (1.33) | <0.001 | 14.65 | 1.49 | 16.34 | (1.39) | <0.001 | |||
| Weight (kg) | 41.33 | (11.17) | 50.18 | (11.03) | <0.001 | 56.69 | 11.88 | 61.31 | (11.72) | <0.001 | |||
| Height (cm) | 144.22 | (10.44) | 155.6 | (10.45) | <0.001 | 162.73 | 9.38 | 167.5 | (8.51) | <0.001 | |||
| Weight status (n, %) | |||||||||||||
| Underweight | 21 | (3) | 24 | (4) | <0.001 | 22 | (3) | 19 | (3) | <0.001 | |||
| Normal weight | 357 | (52) | 355 | (58) | 516 | (75) | 371 | (75) | |||||
| Overweight | 235 | (34) | 178 | (29) | 116 | (17) | 86 | (17) | |||||
| Obese | 74 | (11) | 56 | (9) | 37 | (5) | 19 | (3) | |||||
| Pubertal status (n, %) | |||||||||||||
| 1 | 98 | (14) | 4 | (0.6) | <0.001 | 36 | (5) | - | - | <0.001 | |||
| 2 | 467 | (68) | 138 | (22) | 201 | (29) | 3 | (0.6) | |||||
| 3 | 114 | (17) | 270 | (44) | 311 | (46) | 67 | (13) | |||||
| 4 | 8 | (1) | 142 | (23) | 137 | (20) | 218 | (44) | |||||
| 5 | - | - | 59 | (9) | - | - | 207 | (42) | |||||
| Self-reported health (n, %) | 3.99 | (0.81) | 4.00 | (0.82) | 0.867 | 3.74 | (0.81) | 2.64 | (0.80) | <0.001 | |||
| 1 | 2 | (0.3) | 2 | (0.3) | <0.001 | 2 | (0.3) | - | - | <0.001 | |||
| 2 | 17 | (2) | 13 | (2) | 32 | (5) | 31 | (6) | |||||
| 3 | 166 | (24) | 153 | (25) | 232 | (34) | 185 | (37) | |||||
| 4 | 301 | (44) | 258 | (42) | 306 | (44) | 209 | (42) | |||||
| 5 | 201 | (29) | 187 | (31) | 119 | (17) | 70 | (14) | |||||
| Physical fitness | |||||||||||||
| Cardiorespiratory fitness (stage) | 3.69 | (1.84) | 4.93 | (0.99) | <0.001 | 5.78 | (2.53) | 6.32 | (1.00) | <0.001 | |||
| Upper isometric muscular strength (kg) | 16.91 | (4.74) | 22.27 | (7.05) | <0.001 | 27.67 | (7.77) | 32.26 | (8.06) | <0.001 | |||
| UIMS/WG | 0.41 | (0.08) | 0.44 | (0.10) | <0.001 | 0.49 | (0.10) | 0.53 | (0.10) | <0.001 | |||
| Lower body explosive strength (cm) | 130.35 | (23.39) | 145.0 | (27.51) | <0.001 | 164.06 | (33.51) | 174.7 | (36.84) | <0.001 | |||
| Motor fitness (s) | 13.27 | (1.15) | 12.43 | (0.98) | 0.454 | 12.07 | (1.14) | 11.75 | (1.01) | 0.395 | |||
| Muscular strength score (z-score) | −0.03 | (1.73) | −0.01 | (1.69) | 0.895 | 0.06 | (1.70) | 0.02 | (1.66) | 0.733 | |||
| Global physical fitness (z-score) | −0.07 | (3.22) | −0.02 | (1.92) | 0.798 | 0.19 | (3.08) | 0.03 | (1.77) | 0316 | |||
| Children (n = 687) | Adolescents (n = 691) | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Model 1 | ||||||
| Pubertal status | 1.068 | 0.834–1.369 | 0.601 | 1.050 | 0.873–1.265 | 0.603 |
| Gender | 1.156 | 0.847–1.580 | 0.360 | 0.844 | 0.581–1.226 | 0.373 |
| BMI | 0.942 | 0.898–0.988 | 0.014 | 0.919 | 0.874–0.966 | <0.001 |
| Cardiorespiratory fitness | 1.048 | 1.020–1.076 | <0.001 | 1.057 | 1.037–1.076 | <0.001 |
| Pubertal status | 0.964 | 0.757–1.227 | 0.766 | 0.903 | 0.755–1.078 | 0.260 |
| Gender | 0.995 | 0.748–1.325 | 0.975 | 0.490 | 0.357–0.672 | <0.001 |
| UIMS/WG | 18.921 | 3.471–104.355 | <0.001 | 5.707 | 1.122–29.205 | 0.036 |
| Pubertal status | 1.061 | 0.828–1.359 | 0.641 | 1.032 | 0.852–1.252 | 0.747 |
| Gender | 0.946 | 0.707–1.267 | 0.710 | 0.515 | 0.360–0.736 | <0.001 |
| BMI | 0.911 | 0.872–0.952 | <0.001 | 0.882 | 0.841–0.925 | <0.001 |
| Lower body explosive strength | 1.002 | 0.996–1.008 | 0.535 | 1.004 | 0.999–1.010 | 0.112 |
| Pubertal status | 1.057 | 0.825–1.354 | 0.661 | 1.004 | 0.828–1.217 | 0.969 |
| Gender | 0.967 | 0.719–1.299 | 0.823 | 0.554 | 0.393–0.778 | <0.001 |
| BMI | 0.915 | 0.874–0.956 | <0.001 | 0.889 | 0.847–0.932 | <0.001 |
| Motor fitness | 1.067 | 0.933–1.184 | 0.313 | 1.192 | 1.066–1.309 | 0.007 |
| Pubertal status | 0.976 | 0.766–1.243 | 0.841 | 0.899 | 0.753–1.073 | 0.237 |
| Gender | 0.982 | 0.740–1.303 | 0.900 | 0.482 | 0.356–0.650 | <0.001 |
| Muscular strength score | 1.213 | 1.117–1.319 | <0.001 | 1.169 | 1.070–1.278 | <0.001 |
| Pubertal status | 0.980 | 0.769–1.249 | 0.872 | 0.898 | 0.752–1.073 | 0.236 |
| Gender | 0.959 | 0.724–1.272 | 0.773 | 0.472 | 0.350–0.635 | <0.001 |
| Global physical fitness | 1.170 | 1.081–1.266 | <0.001 | 1.154 | 1.100–1.210 | <0.001 |
| Model 2 | ||||||
| Pubertal status | 1.012 | 0.794–1.292 | 0.921 | 0.967 | 0.802–1.166 | 0.723 |
| Gender | 1.233 | 0.902–1.688 | 0.189 | 0.948 | 0.646–1.391 | 0.785 |
| Cardiorespiratory fitness | 1.059 | 1.029–1.090 | <0.001 | 1.073 | 1.050–1.097 | <0.001 |
| UIMS/WG | 5.993 | 0.670–54.072 | 0.109 | 0.487 | 0.063–3.757 | 0.490 |
| Lower body explosive strength | 1.000 | 0.991–1.009 | 0.954 | 0.996 | 0.988–1.003 | 0.342 |
| Motor fitness | 0.979 | 0.804–1.192 | 0.829 | 1.180 | 0.944–1.475 | 0.147 |
| Children (n = 613) | Adolescents (n = 496) | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Model 3 | ||||||
| Pubertal status | 0.854 | 0.714–1.019 | 0.080 | 0.983 | 0.752–1.285 | 0.900 |
| Gender | 0.873 | 0.627–1.217 | 0.423 | 0.603 | 0.380–0.953 | 0.031 |
| BMI | 0.954 | 0.910–0.999 | 0.044 | 0.961 | 0.907–1.018 | 0.175 |
| SRH baseline | 1.910 | 1.562–2.341 | <0.001 | 3.652 | 2.806–4.783 | <0.001 |
| Cardiorespiratory fitness | 1.056 | 1.023–1.091 | <0.001 | 1.024 | 0.999–1.051 | 0.058 |
| Pubertal status | 0.746 | 0.629–0.885 | <0.001 | 0.942 | 0.724–1.225 | 0.656 |
| Gender | 0.705 | 0.520–0.956 | 0.025 | 0.477 | 0.318–0.713 | <0.001 |
| SRH baseline | 2.032 | 1.663–2.488 | <0.001 | 3.980 | 3.082–5.176 | <0.001 |
| UIMS/WG | 2.154 | 0.344–13.519 | 0.412 | 0.981 | 0.135–7.164 | 0.985 |
| Pubertal status | 0.782 | 0.643–0.949 | 0.013 | 1.027 | 0.782–1.350 | 0.847 |
| Gender | 0.726 | 0.530–0.992 | 0.045 | 0.412 | 0.266–0.633 | <0.001 |
| BMI | 0.933 | 0.891–0.976 | 0.002 | 0.942 | 0.890–0.998 | 0.042 |
| SRH baseline | 1.972 | 1.615–1.012 | <0.001 | 3.871 | 2.985–5.055 | <0.001 |
| Lower body explosive strength | 1.004 | 0.996–1.012 | 0.326 | 0.996 | 0.989–1.002 | 0.164 |
| Pubertal status | 0.810 | 0.673–0.974 | 0.025 | 1.001 | 0.763–1.314 | 0.993 |
| Gender | 0.703 | 0.512–0.964 | 0.029 | 0.452 | 0.296–0.687 | <0.001 |
| BMI | 0.928 | 0.886–0.971 | 0.001 | 0.947 | 0.894–1.002 | 0.061 |
| SRH baseline | 1.981 | 1.622–2.427 | <0.001 | 3.857 | 2.972–5.039 | <0.001 |
| Motor fitness | 1.022 | 0.873–1.196 | 0.785 | 0.952 | 0.794–1.141 | 0.592 |
| Pubertal status | 0.744 | 0.627–0.881 | <0.001 | 0.934 | 0.717–1.218 | 0.615 |
| Gender | 0.712 | 0.526–0.962 | 0.027 | 0.491 | 0.332–0.724 | <0.001 |
| SRH baseline | 1.980 | 1.619–2.427 | <0.001 | 4.040 | 3.118–5.271 | <0.001 |
| Muscular strength score | 1.110 | 1.105–1.213 | 0.052 | 1.012 | 0.911–1.125 | 0.822 |
| Pubertal status | 0.797 | 0.667–0.950 | 0.011 | 0.956 | 0.729–1.254 | 0.747 |
| Gender | 0.691 | 0.511–0.934 | 0.016 | 0.461 | 0.313–0.678 | <0.001 |
| SRH baseline | 1.901 | 1.554–2.333 | <0.001 | 3.715 | 2.860–4.856 | <0.001 |
| Global physical fitness | 1.086 | 1.026–1.150 | 0.004 | 1.053 | 0.990–1.119 | 0.101 |
| Model 4 | ||||||
| Pubertal status | 0.808 | 0.665–0.980 | 0.031 | 1.016 | 0.775–1.333 | 0.901 |
| Gender | 0.946 | 0.677–1.323 | 0.747 | 0.566 | 0.355–0.898 | 0.016 |
| SRH baseline | 1.943 | 1.588–2.384 | <0.001 | 3.720 | 2.861–4.870 | <0.001 |
| Cardiorespiratory fitness | 1.075 | 1.040–1.112 | <0.001 | 1.043 | 1.014–1.074 | 0.003 |
| UIMS/WG | 0.214 | 0.020–2.213 | 0.196 | 1.665 | 0.129–21.579 | 0.696 |
| Lower body explosive strength | 1.008 | 0.998–1.018 | 0.134 | 0.991 | 0.981–1.001 | 0.068 |
| Motor fitness | 0.917 | 0.740–1.137 | 0.431 | 1.003 | 0.765–1.313 | 0.985 |
| Model 5 | ||||||
| Pubertal status | 1.339 | 1.124–1.596 | 0.001 | 1.071 | 0.818–1.404 | 0.617 |
| Gender | 1.494 | 1.099–2.036 | 0.010 | 2.145 | 1.445–3.200 | <0.001 |
| SRH baseline | 5.730 | 4.535–7.296 | <0.001 | 4.294 | 3.296–5.646 | <0.001 |
| Δ Global physical fitness | 0.942 | 0.883–1.006 | 0.076 | 1.002 | 0.922–1.088 | 0.965 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Padilla-Moledo, C.; Fernández-Santos, J.D.; Izquierdo-Gómez, R.; Esteban-Cornejo, I.; Rio-Cozar, P.; Carbonell-Baeza, A.; Castro-Piñero, J. Physical Fitness and Self-Rated Health in Children and Adolescents: Cross-Sectional and Longitudinal Study. Int. J. Environ. Res. Public Health 2020, 17, 2413. https://doi.org/10.3390/ijerph17072413
Padilla-Moledo C, Fernández-Santos JD, Izquierdo-Gómez R, Esteban-Cornejo I, Rio-Cozar P, Carbonell-Baeza A, Castro-Piñero J. Physical Fitness and Self-Rated Health in Children and Adolescents: Cross-Sectional and Longitudinal Study. International Journal of Environmental Research and Public Health. 2020; 17(7):2413. https://doi.org/10.3390/ijerph17072413
Chicago/Turabian StylePadilla-Moledo, Carmen, Jorge DR Fernández-Santos, Rocio Izquierdo-Gómez, Irene Esteban-Cornejo, Paula Rio-Cozar, Ana Carbonell-Baeza, and Jose Castro-Piñero. 2020. "Physical Fitness and Self-Rated Health in Children and Adolescents: Cross-Sectional and Longitudinal Study" International Journal of Environmental Research and Public Health 17, no. 7: 2413. https://doi.org/10.3390/ijerph17072413





