1. Introduction
Traditionally, the task of prescribing medicines has been the domain of physicians but the international trend of growing demands for healthcare services, increasing budget constraints on healthcare delivery and efforts to extend the scope of nursing practices have contributed to demands for nurse prescribing. The practice was first introduced in Idaho, in the United States of America, in 1969 [
1]. Since then, nurses have gained the right to prescribe in more than 14 countries, including Australia, Canada, Ireland, Israel, Iran, New Zealand, Norway, Spain, Sweden, the Netherlands, the Republic of South Africa, the United Kingdom, the United States of America and, since 2016, in Poland. When permitted by legislation and qualified, nurse prescribers are responsible for the clinical assessment of patients, for establishing diagnoses and for decisions about the appropriateness of medications, treatments or applications, including the issuing of prescriptions. Usually the practice of nurse prescribing is permitted for a limited list of active substances. This scope of prescribing is either called ‘initial’, ‘independent’ or ‘substitutive’ [
2] and in our paper we refer to it as ‘nurse independent prescribing’. Another type of prescribing is practised by ‘supplementary’ prescribers: either nurses or pharmacists; who practise in a voluntary partnership with an independent prescriber, either a doctor or a dentist. Here, the nurse supplementary prescriber collaborates or consults with the independent prescriber before issuing the prescription [
3], and in our paper we refer to these as ‘nurse supplementary prescribers’. Nurse prescribing is described in the literature as a necessary piece for consolidating and improving the jigsaw puzzle of the professional nursing identity [
4].
New legal provisions for nurse prescribing were introduced in Poland in January 2016. In the absence of any literature on the Polish situation of nurse prescribing, the present study involved an analysis of nurses and midwives opinions immediately prior to the implementation of legal nurse prescribing (2015), and the actual prescribing behaviours and trends of nurses and midwives in the two years immediately following the new law coming into force (2016 and 2017). These two phases formed one integrated whole because, though nurse prescribing was permitted from January 2016, it was not mandatory and prescribing activity was an option at the discretion of suitably qualified nurses and midwives. As such, it was expected that the opinions of nurses may have a direct bearing on their actual prescribing practices; and therefore, the relationship between the two sets of data needed to be understood through an integrated analysis of the before-and-after phasing of the research. Though it is true that in 2016 and 2017, more nurses also finished the nurse prescribing course that we had surveyed in 2015, and that therefore the number of prescribers increased, those from the first phase of the study did become prescribers and the analyzed data also derived from their prescribing. Also, the rationale for our retrospective analysis was because this was the only way could have data to analyze from the whole country for the whole two year period.
In Poland, the new provisions authorized nurses and midwives to prescribe (decide on the choice of medication) and to issue prescriptions for medicines and foods for special dietary purposes, to give referrals for a range of specified diagnostic tests, and to issue orders and prescriptions for reimbursable medical devices. The new entitlement for Polish nurses and midwives takes two forms:
- a)
Nurse independent prescribing and issuing prescriptions, defined as an element of the independent provision of preventive, diagnostic, therapeutic and rehabilitation services; and
- b)
Issuing a prescription which is a continuation of medical prescribing (‘nurse supplementary prescribing’), defined as an element of the fulfilment of a doctor’s orders in the process of diagnosis, treatment and rehabilitation.
The entitlement of Polish nurses and midwives to practise as either independent or supplementary prescribers is dependent on their level of tertiary education in nursing or obstetrics, or a specialist’s qualification. Nurses and midwives are permitted to act as independent prescribers and/or supplementary prescribers if, on the one hand, they are master’s graduates (having graduated prior to 2019) who have subsequently completed the relevant specialist ‘Nurse Prescribing Course’ (which was required prior to 2019, but not after), or, alternatively, if they are master’s graduates who graduated after 2019 (and thus did not require additional specialist training because it was integrated into the master’s program). It should be noted that if a nurse or midwife is permitted to prescribe on the basis of either of the two qualification routes stated above, they may, from day to day, either perform as an independent prescriber, or a supplementary prescriber, depending on the practice situation, where sometimes the nurse might act by herself, independently, and at another time, by cooperating with a doctor, be acting as a supplementary prescriber. Nurses and midwives are limited to acting as supplementary prescribers if they are bachelor’s or master’s degree graduates (graduating prior to 2019) who have subsequently completed the relevant specialist ‘Nurse Prescribing Course’, or, if they are bachelor’s degree graduates (graduating since 2019), or, if they are graduates of Poland’s former professional (medical) schools having completed eight years of education plus a further two year specialization (e.g., as a pediatric nurse, surgery nurse) and if they have subsequently completed the relevant specialist ‘Nurse Prescribing Course’. There are two different ‘Nurse Prescribing Courses’ established by the Minister of Health: one for independent prescribing and another for supplementary prescribing. These courses, with practice and theory components, are delivered by medical universities throughout the country and graduates are awarded a Diploma that permits them to prescribe.
Among high-income countries worldwide, Australia, Canada, New Zealand and the US have implemented laws granting the prescribing of a wide range of medicines to advanced practice nurses (APN) with a master’s degree [
5]. The extent of prescribing rights in different countries ranges from nearly all medicines within nurses’ specializations (Ireland for nurse prescribers, Netherlands for nurse specialists, UK for nurse independent prescribers) to a limited set of medicines (Cyprus, Denmark, Estonia, Finland, France, Norway, Spain, Sweden) [
6]. While nurses in the United Kingdom initially could only prescribe from the Formulary for Nurse Prescribers, currently they may independently prescribe more than 250 different active substances, including controlled drugs [
7]. In some countries, for example in Uganda, nurses even have the right to prescribe morphine [
8].
In Poland, suitably qualified nurses and midwives (as described above) may, as part of the fulfilment of a doctor’s orders during the patient’s diagnosis, treatment and rehabilitation, issue prescriptions as a continuation of medical prescriptions. In the main, nurse independent prescribers in Poland may prescribe specific medical devices, medicinal food and medicinal products with specific active substances, except for medicines containing very potent substances or controlled drugs. The above mentioned ‘specific’ medications should be understood as referring exclusively to those medicines, devices and products listed in the regulations of the Minister of Health. The regulations list 31 active substances, including: anti-emetics, anti-infective medications for topical use, gynaecological anti-infective medications, medications used in anaemia, certain antibiotics, topical anaesthetics, analgesics, anxiolytics, antiparasitics, bronchodilators, vitamin D3 and infusion fluids. If it is necessary to use other drugs not listed in the regulations, that are also over the counter (OTC) category medicines, a nurse or a midwife can recommend them by making an appropriate note in the medical record. They may also issue prescriptions for medications that are not included in the regulations of the Minister of Health, in cases of repeat prescribing, that is, where a doctor has already issued an appropriate instruction for the nurse or the midwife. The only extant restriction to this entitlement concerns a specific group of very potent medications, narcotics and psychotropics. There was also a further restriction (during 2017 and 2018), that nurses and midwives were not permitted to issue prescriptions for medical devices, and this caused real impediments to nurses’ care for patients. For instance, cases such as the following required a doctor’s prescription: ongoing provision of wound treatment where subsidized categories of dressings were required; or, ensuring recurring access to blood glucose test strips in the treatment of diabetic patients. Yet in such cases a doctor may not have been present when the nurse was treating the patient, especially for instance, during in-home care. That restriction in the law was subsequently changed, and since 2019 nurses are permitted to prescribe medical devices.
Nurses and midwives in Poland may prescribe a medication and issue a prescription following a personal physical examination of the patient. Prescriptions may also be issued without a personal physical examination of the patient only if justified by evidence of the patient’s health reflected in the medical record. They therefore have the right to inspect the patient’s medical record and to obtain complete information from the doctor on the patient’s health, diagnosis, suggested diagnostic, therapeutic, rehabilitation and preventive methods and the foreseeable consequences of the measures taken, as far as is necessary for the nurses and midwives to determine the health services that ought to be provided to the patient. In other words, they may fulfil their entitlement to order and issue prescriptions without any formal obstacles. Additionally, nurses and midwives are entitled to obtain and process the data included in medical records.
Nurses and midwives are obliged to practice their profession with due diligence, in accordance with the rules pertaining to professional ethics, observing the patient’s rights, protecting the patient’s safety and making use of the indications of current medical knowledge. If a prescribing error is committed, civil liability may be considered; while in exceptional cases where there is a criminal offence, criminal liability may be considered. It is also possible for nurses and midwives to be held professionally responsible before a nurses’ and midwives’ court. Nurse prescribing and the validity of prescription issuance is overseen by the National Health Fund (NHF) which is also the government body which delivers funding for Poland’s free national health care services.
The study aimed to investigate attitudinal influences on, and actual results of, the early phases of nurse prescribing in Poland at the time it was introduced at the beginning of 2016. The paper analyzes the opinions of nurses, expected to be influential on nurses’ actual practices, prior to legislative change and compares this with actual nurse prescribing behaviours during the early years of implementing legal nurse prescribing. Analyzing the opinions of nurses prior to implementation was important, partly because there were no other studies available, and because whether a qualified nurse or midwife would practice as a prescriber was at their own discretion, not that of their employer. As the first study of its kind in Poland, the paper addressed a knowledge gap in the field, and provides baseline data analysis for subsequent research.
3. Results
3.1. Study of Nurses’ and Midwives’ Opinions
There were 804 women and 15 men involved in the questionnaire study (the first phase of the research), which reflects the actual gender ratio of working nurses in Poland [
14]. 152 (18.7%) respondents were 22–29 years old (normally, a nurse with a bachelor’s degree starts work when they are 22); 95 (11.7%): 30–39 years old; 318 (39.2%): 40–49 years old; 228 (28.1%): 50–59 years old; 19 (2.3%) respondents were over 60 years old, and 7 respondents did not state their age.
Most respondents held a bachelor’s degree: 357 (43.7%); while 263 (32.2%) had a master’s degree; and the remainder (199, 24.1%) were graduates of medical secondary schools, qualifying under Poland’s former nursing education system. Hence all of the respondents would have been permitted to take a special course preparing them to prescribe medications or issue prescriptions. The group of nurses and midwives whose highest qualification was from medical secondary school constituted 24.1% of the respondents, but they also included persons who had a specialisation which permitted them to be enrolled on the course. The other respondents from the secondary school sub-group also had the possibility of completing the specialisation, which qualifies nurses to be prescribers, and therefore they were also eligible to participate in our study. The results are shown in
Table 1.
The questionnaire first asked the respondents about the roles they play in patient pharmacotherapy processes which are understood as the necessary scope of practice for nurses who are prescribing or assisting with prescribing (it was possible to give multiple concurrent answers). The study subjects identified that their role was primarily in monitoring doctor’s indications (68%), educating patients about the administration of their medications (67.3%), and monitoring and reporting adverse reactions (65%). A smaller number of respondents identified the role of assisting doctors (performing supplementary activities) with the issuing of prescriptions (28.6%). Nurses also less frequently identified their role as conducting drug reviews (32.9%). The results are shown in
Table 2.
While analyzing possible relationships between the practice role and the years of experience of the respondents, we found that there was a statistically significant difference between respondents with 31–40 years’ experience, who were more likely, and those with 0–10 years’ experience, who were less likely, to assist with the issuing of prescriptions, H test = 11.45; p < 0.05. However, those with the lowest level of experience (0–10 years) were found to monitor compliance with the doctor’s instructions significantly more often than other groups, H test = 13.79; p < 0.05.
Secondly, the questionnaire sought nurses’ and midwives’ opinions on whether they should issue prescriptions as part of their professional duties. Positive opinions to the new entitlements were demonstrated by 371 (45.3%) people answering: “strongly agree” and “agree”. 329 (40.2%) respondents expressed negative opinions related to them not being paid by either the NHF or their employers for undertaking new responsibilities. The remainder of the group did not express either positive or negative opinions. The distribution of answers is summarized in
Table 3.
Our analysis revealed that age was not a factor in the respondents’ opinions on prescribing (H test = 5.43; p = 0.246); but we did find a correlation between the respondents’ years of experience and their opinion on prescribing (H test = 17.65; p < 0.05). To identify which groups showed significant differences from other groups, the Bonferroni method of multiple comparisons was used. The analysis showed that respondents with 11–20 years’ experience disagreed with prescribing by nurses and midwives significantly more often than respondents from all other groups (0–10 years, 21–30 years, 31–40 years and greater than 40 years). A correlation was also found between the opinions and the respondents’ levels of education. Respondents with a master’s degree expressed more favourable opinions on prescribing by nurses and midwives than those respondents who graduated from a medical secondary school, a medical college or from bachelor’s degree studies.
The third survey question concerned the respondents’ subjective assessment of whether their own preparedness for prescribing before entering the course was sufficient. According to 50% of the respondents, their knowledge and skills were unsatisfactory for the task ahead (with answers of “strongly disagree”: 156 people; and “disagree”: 254 people). 183 (22.3%) respondents “agreed” that their preparedness for prescribing was sufficient, while only 42 (5.1%) “strongly agreed” that their preparedness was sufficient. Nearly 23% (185 respondents) answered “neither agree nor disagree”.
Respondents identified two benefits for patients of nurse prescribing: in the treatment of chronic diseases (590 answers, 72.1%); and the management and treatment of acute pain and infections (229 answers, 27.9%).
Respondents were also asked for their opinions on what benefits they will draw from prescribing, and what dangers they foresee in the new entitlement (multiple answers could be given). The benefits they identified included:
- a)
Greater professional autonomy: 527 answers (64.3%);
- b)
Higher professional status: 348 answers (42.5%);
- c)
Higher remuneration: 219 answers (26.7%);
- d)
Greater work satisfaction: 186 answers (22.7%).
The dangers they identified included:
- a)
Greater legal responsibility and liability: 631 answers (77.3%);
- b)
Reduced time for patient care: 585 answers (71.4%);
- c)
No additional remuneration: 584 answers (70.9%);
- d)
Increased workload: 509 answers (62.1%);
- e)
Inadequate preparation: 385 answers (47%);
- f)
Conflicts in the therapeutic team: 240 answers (29.3%);
- g)
Lack of substantive support: 227 answers (27.7%).
Respondents were also asked which groups of medications they would be ready to prescribe independently, from within the choice of medications permitted by the legal regulations for nurse prescribing. Respondents indicated that they would independently issue prescriptions for analgesics in the first place. The results of the analysis are shown in
Table 4.
The analysis demonstrated that there was a correlation between the educational level of respondents and their preference for prescribing medicinal products. Those with a master’s degree said they would issue a prescription for medications statistically significantly more often than respondents who graduated from medical secondary school, medical college or bachelor’s degree studies.
3.2. Prescribing Data Analysis: Retrospective Research
A secondary analysis, comparing the first year of implementation data obtained from NHF with that for the second year of implementation showed that the number of nurse prescriptions had been increasing. In 2016, there were 536 nurse independent prescriptions issued, and in 2017 there were twice as many, i.e., 1323. The number of nurse supplementary prescriptions issued in 2016 was 28,674, and in 2017 it was almost six times higher at 161,087. Prescribing rates differ from one province to another because of population differences and the varied numbers of prescribers in each province. These results were further broken down by province. It is evident that in Poland, nurse supplementary prescribing, on doctors’ orders, was more frequent than nurse independent prescribing, in the NHF prescribing data during the first two years after the introduction of the new law.
Nurse independent prescribing may apply to specifically defined medications and medical devices (dressings and blood glucose test strips). During the implementation period nurse independent prescriptions were mainly issued for dressings. 321 prescriptions were issued for reimbursed dressings in 2016, and in 2017 there were 665 such prescriptions. In the medication group, prescriptions for oral antibiotics predominated.
Table 5 below summarizes the results. During the questionnaire phase of the research, nurses were asked which drugs they anticipated prescribing and they thought they would be mainly prescribing anti-emetics, and only rarely antibiotics. However, the actual case was exactly the opposite, as the prescriptions data showed that nurses issued relatively few prescriptions for anti-emetics, and instead, mainly prescribed antibiotics.
Data from the Polish NHF indicates that nurse independent prescribing mostly takes place in relation to pain management and combating infections. Prescriptions were issued to patients of diverse ages, but mostly to the elderly, i.e., 65–85 year-olds.
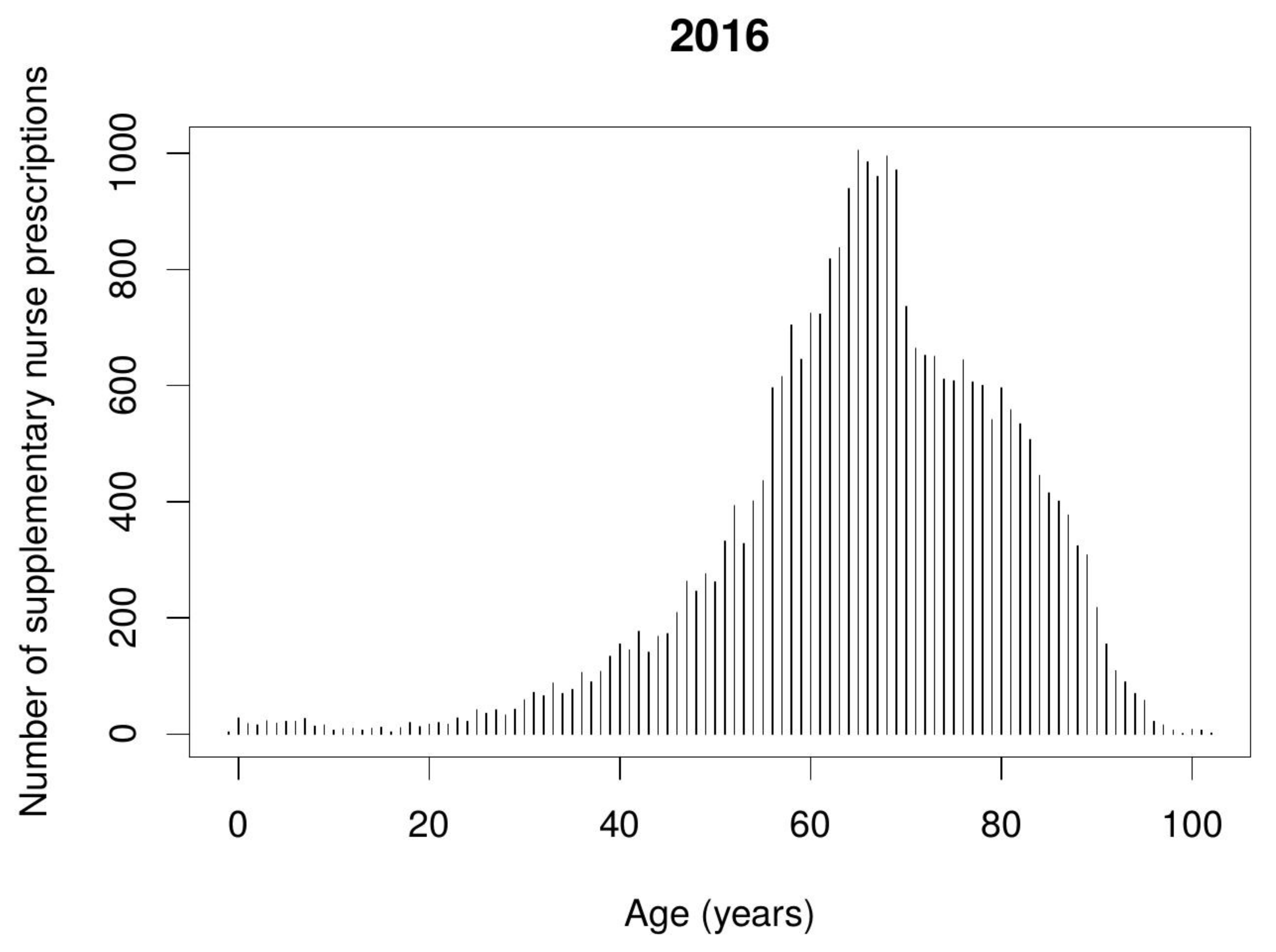
Figure 1 and
Figure 2 show the number of nurse independent prescriptions depending on the patient’s age.
In nurse supplementary prescribing, the predominant medications were those used in the treatment of chronic conditions, i.e., for hypertension to lower cholesterol levels, and for cardiovascular disorders. There were also numbers of medications used for digestive tract disorders. The fewest prescriptions were issued for proctological, gynaecological (by midwives) and antiparasitic medications. All results are shown below in
Table 6.
In the category ‘medical devices’ the following were prescribed: in 2016; 403 prescriptions for dressings, 862 prescriptions for blood glucose test strips; and in 2017: 1429 prescriptions for dressings and 4578 prescriptions for blood glucose test strips. In addition, prescriptions for foods for special dietary purposes were issued (in 2016: 51 prescriptions; in 2017: 131 prescriptions).
The most frequently issued nurse supplementary prescriptions were for medications used for hypertension. The diagram (
Figure 3) below shows which age groups these prescriptions were issued to, with the greatest frequently during 2017. Prescribing for the elderly in the 60–80 age group predominates.
Nurse supplementary prescribing was predominantly applied in the treatment of elderly patients aged 60–80 years old.
Figure 4 and
Figure 5 show the number of nurse supplementary prescriptions according to the patient’s age.
4. Discussion
Nurse prescribing already has a long history in many countries [
15]. Most studies emphasize nurse prescribing has a positive influence on health care results [
16,
17,
18,
19]. Some studies show that when comparing the clinical outcomes in patients arising from doctors’ prescribing with those arising from nurses prescribing, there are no significant differences [
1].
To date, there have not been any other analyses of nurse prescribing in Poland during the implementing period. Some Polish research has reported the positive opinions of nurses about prescribing [
20,
21,
22], but that research did not assess nurse prescribing practice. A better understanding of the determinants of prescribing patterns in Poland may help shape future workforce policy in the medical sector and contribute to the design and implementation of optimal and cost-effective initiatives to improve care quality.
The picture emerging from our own research indicates that even though they were enrolled in a specialist nurse prescribing course, which was a pre-requisite for authority to prescribe, during this preparation period nurses were not convinced that they should issue prescriptions (54.7% had either no opinion or negative opinions of the new entitlement). Additionally, nurses identified their lack of proper preparation as a barrier to the assimilation of nurse prescribing (47%). It was possible that some of the course participants, prior to completion, might have felt the course was more of a licensing formality than a substantive learning opportunity. However, even those with negative opinions participated in the free Diploma training courses. This might suggest they were unaware that though entitled, their own practice of nurse prescribing was optional rather than mandatory. It might also indicate their positive disposition towards their own professional development. Our study shows other links between professional development and prescribing in that nurse prescribing was more likely to be associated with nurses’ higher professional status (42.5%) and greater professional autonomy (64.3%). Though many respondents rated their preparedness for the new role as poor (23% offered no opinion on their knowledge and skills, and more than 50% were of the opinion that their knowledge and skills were poor), in the first two years of nurse prescribing the number of prescriptions issued grew more than five-fold. It is worth noting that nurse prescribing is generally associated with master’s degree holders [
23].
The experience of many countries, such as the USA, Canada, Australia, Ireland, New Zealand, Sweden, and the UK, where similar entitlements have been introduced, shows that they have brought positive effects for patients, including appreciating the quality of the information they receive about additional therapeutic procedures and gaining high levels of satisfaction from the treatment used [
24,
25]. Polish nurses have expressed concern about possible time reductions in patient care (71.4%); and they believed their workload would increase (62.1%). These opinions might suggest that they are overburdened with current duties and have no time for additional therapeutic activities.
Compliance with therapeutic indications is an important element of pharmacotherapy. International research has shown that the participation of nurses in prescribing improves compliance [
26]. Nurse prescribing is most beneficial in the treatment of the elderly (60–85 years old); nurse prescribers also help to reduce polypharmacy in the elderly; and our research also found that nurse supplementary prescribing was predominantly applied in the treatment of elderly patients aged 60–80 years [
27].
Research indicates that in countries with nurse prescribing, it mitigates situations of medical staff shortages; enables interdisciplinary cooperation; and bridges the distance between nurses and other professions, thus benefiting the whole team and allowing doctors to focus on more complicated clinical cases [
28,
29]. Concurrently, the practice reduces the professional distances between health care providers [
30]. In our own research, the respondents who had no experience of prescribing at the time of our study pointed out that conflicts might arise in the therapeutic team (29.3%); and some other studies also point to the possibility of conflicts [
31]. Polish nurses have also expressed concerns about being burdened with additional work (62.1% respondents), which would contribute to negative outcomes for the whole therapeutic team.
In Poland, respondents identified the increased risk of legal liability, because of the professional fault principle in Polish law, as a negative consequence of nurse prescribing (77.3%). In addition, respondents believed that the new roles are not associated with additional remuneration (70.9%). It is not mandatory under Polish law for an employer to raise the salary of a nurse prescriber in the public system. In the private sector, the employer’s pay system choices are unconstrained. In contrast, respondents did expect that their new prescribing duties would enhance their professional status (42.5%) and work satisfaction (22.7%). The new entitlement is linked to increasing professional autonomy (64.3%). These benefits have also been reported in other studies, including those by Carey et al. and Scrafton et al. [
32,
33].
Poland has recently introduced the role of doctor’s assistant. Previously this role was fulfilled by nurses; and as for the time being there are few medical assistants, nurse prescribing can serve as a legal equivalent, in that nurses may issue a prescription and the physician only signs it. Evidence from our own studies shows that this assisting role in the issuing of medical prescriptions was practised by 28.6% of respondents.
The Polish practice of nurse prescribing is mostly for nurse supplementary prescriptions issued on a doctor’s orders, and mostly for the elderly in the treatment of chronic diseases, especially hypertension. Nurse prescribers in the UK, New Zealand and the Netherlands are playing a significant therapeutic role for senior citizens with chronic diseases [
27,
34,
35]. In Ireland, the most frequently prescribed medications are analgesics and anti-inflammatory medications (containing paracetamol and ibuprofen), vaccines and antibiotics for adults [
36].
The potential limitations of this work should be noted. In the questionnaire phase of the study the precondition for inclusion in the study was that participants had to have attended a nurse prescribing training course. However, we did not assess whether all participants had successfully completed said course and become certified prescribers. Another limitation is that in Poland there is no general record of all nursing prescriptions, only those funded by the NHF; and prescriptions that were paid for in full by patients were excluded from our study. The opinions survey was carried out very shortly after the announcement that nurses would have new prescribing powers in Poland, and therefore, further studies would be needed to determine whether opinions have changed over time and to understand those changes.