Stronger Increases in Cognitive Functions among Socio-Economically Disadvantaged Older Adults in China: A Longitudinal Analysis with Multiple Birth Cohorts
Abstract
1. Introduction
2. Methods
2.1. Study Samples
2.2. Variable Definitions
2.3. Statistical Analysis
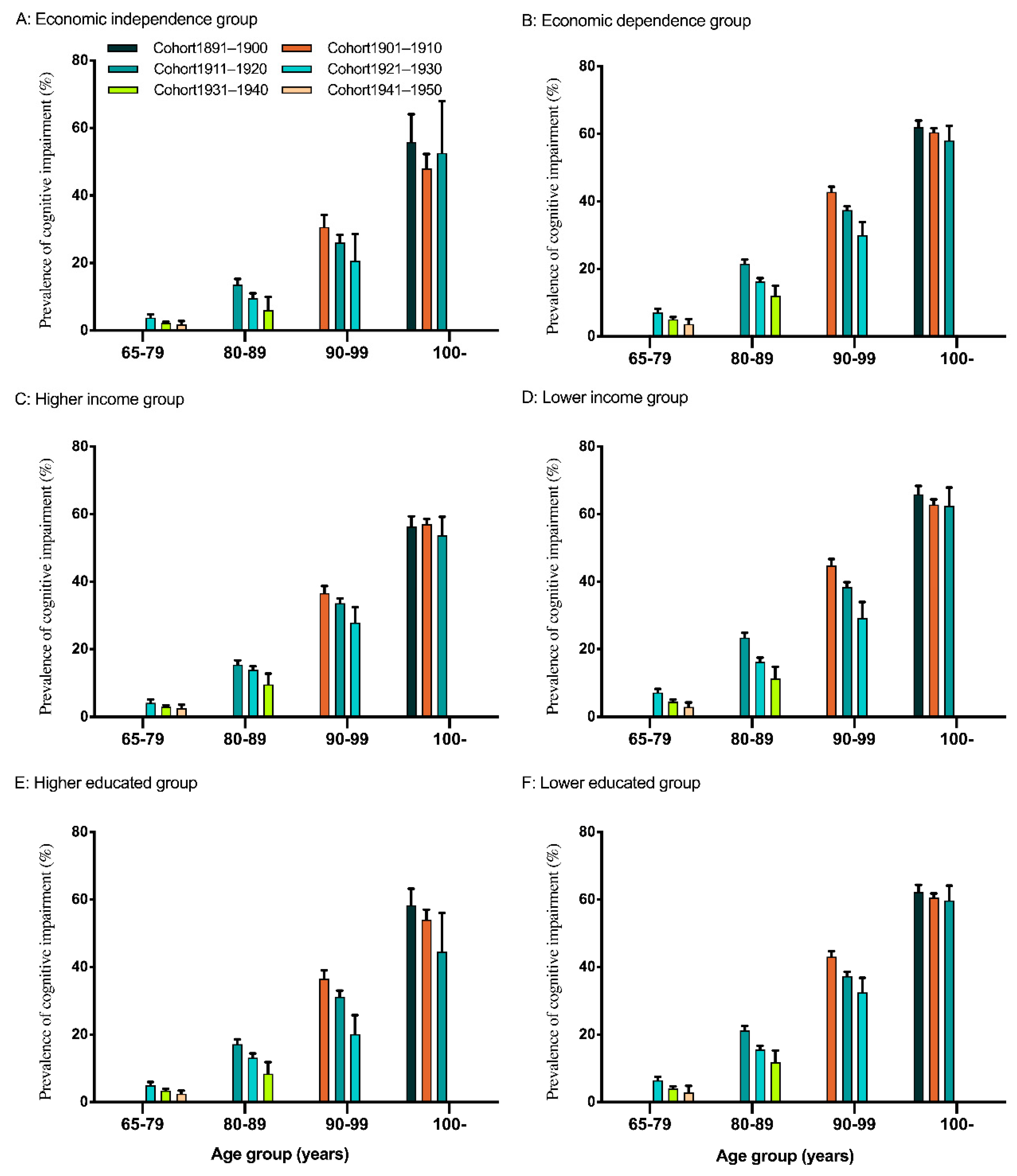
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kowal, P.; Goodkind, D.; He, W. An Aging World: 2015; International Population Reports; U.S. Government Printing Office: Washington, DC, USA, 2016. Available online: http://www.census.gov/library/publications/2016/demo/P95-16-1.html (accessed on 9 September 2018).
- Yi, Z.; Vaupel, J.W.; Zhenyu, X.; Chunyuan, Z.; Yuzhi, L. Sociodemographic and health profiles of the oldest old in China. Popul. Dev. Rev. 2002, 28, 251–273. [Google Scholar] [CrossRef]
- Zhang, Z. Gender differentials in cognitive impairment and decline of the oldest old in China. J. Gerontol. B Psychol. Sci. Soc. Sci. 2006, 61, S107. [Google Scholar] [CrossRef] [PubMed]
- Blazer, D.F.; Yaffe, K.; Liverman, C.T. Cognitive Aging Progress in Understanding and Opportunities for Action; National Academy of Sciences: Washington, DC, USA, 2015; pp. 2–3. [Google Scholar]
- Park, B.; Park, J.; Jun, J.K. Cognitive impairment, depression, comorbidity of the two and associated factors among the early sixties in a rural Korean community. PLoS ONE 2013, 8, e79460. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, D.; Ni Mhaolain, A.; Crosby, L.; Ryan, D.; Lacey, L.; Coen, R.F.; Lawlor, B.A. Dependence and caregiver burden in Alzheimer’s disease and mild cognitive impairment. Am. J. Alzheimer Dis. Dement. 2011, 26, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Lyu, J.; Burr, J.A. Socioeconomic status across the life course and cognitive function among older adults. An examination of the latency, pathways, and accumulation hypotheses. J. Aging Health 2015, 28, 40. [Google Scholar] [CrossRef]
- Marengoni, A.; Fratiglioni, L.; Bandinelli, S.; Ferrucci, L. Socioeconomic status during lifetime and cognitive impairment no-dementia in late life: The population-based aging in the Chianti Area (InCHIANTI) Study. J. Alzheimer Dis. 2010, 6, S452–S453. [Google Scholar] [CrossRef][Green Version]
- Yaffe, K.; Falvey, C.; Harris, T.B.; Newman, A.; Satterfield, S.; Koster, A.; Simonsick, E. Effect of socioeconomic disparities on incidence of dementia among biracial older adults: Prospective study. BMJ 2013, 347, 7051. [Google Scholar] [CrossRef]
- Horvat, P.; Richards, M.; Malyutina, S.; Pajak, A.; Kubinova, R.; Tamosiunas, A.; Bobak, M. Life course socioeconomic position and mid-late life cognitive function in Eastern Europe. J. Gerontol. B Psychol. Sci. Soc. Sci. 2014, 69, 470–481. [Google Scholar] [CrossRef] [PubMed]
- Dodge, H.H.; Zhu, J.; Lee, C.W.; Chang, C.C.H.; Ganguli, M. Cohort effects in age-associated cognitive trajectories. J. Gerontol. B Psychol. Sci. Soc. Sci. 2014, 69, 687–694. [Google Scholar] [CrossRef]
- Sattler, C.; Toro, P.; Schönknecht, P.; Schröder, J. Cognitive activity, education and socioeconomic status as preventive factors for mild cognitive impairment and Alzheimer’s disease. Psychiatry Res. 2012, 196, 90–95. [Google Scholar] [CrossRef]
- Lee, S.; Kawachi, I.; Berkman, L.F.; Grodstein, F. Education, other socioeconomic indicators, and cognitive function. Am. J. Epidemiol. 2003, 157, 712. [Google Scholar] [CrossRef]
- Karlamangla, A.S.; Miller-Martinez, D.; Aneshensel, C.S.; Seeman, T.E.; Wight, R.G.; Chodosh, J. Trajectories of cognitive function in late life in the United States: Demographic and socioeconomic predictors. Am. J. Epidemiol. 2009, 170, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Cao, J. Longitudinal Changes in Cognitive Function of Old Adults and its Socio-economic Differences- Multiple Birth Cohorts Study Based on SDH; Nanjing Medical University: Nanjing, China, 2019; pp. 10–101. [Google Scholar]
- Wee, L.E.; Yeo, W.X.; Yang, G.R.; Hannan, N.; Lim, K.; Chua, C.; Koh, G.C.H. Individual and area level socioeconomic status and its association with cognitive function and cognitive impairment (low MMSE) among community-dwelling elderly in Singapore. Dement. Geriatr. Cogn. Dis. Extra 2012, 2, 529–542. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Zeng, Y. Data assessment of the Chinese Longitudinal Healthy Longevity Survey. In Determinants of Healthy Longevity of the Oldest-Old in China; Zeng, Y., Xiao, Z., Zhang, C., Eds.; Peking University Press: Beijing, China, 2004. [Google Scholar]
- Gu, D.; Qin, X. Sociodemographic effects on the dynamics of task-specific ADL functioning at the oldest-old ages: The case of China. J. Cross Cult. Gerontol. 2007, 22, 61. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Qian, D.; Yang, F. Socioeconomic disparities in leisure activities over the life course of the oldest-old in China. Australas. J. Ageing 2019, 1–9. [Google Scholar] [CrossRef]
- Zeng, Y. Introduction to the Chinese Longitudinal Healthy Longevity Survey (CLHLS): Healthy longevity in China; Springer: Dordrecht, The Netherlands, 2008; pp. 23–38. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Nguyen, H.T.; Black, S.A.; Ray, L.A.; Espino, D.V.; Markides, K.S. Cognitive impairment and mortality in older Mexican Americans. J. Am. Geriatr. Soc. 2010, 51, 178–183. [Google Scholar] [CrossRef]
- Zhu, X.; Qiu, C.; Zeng, Y.; Li, J. Leisure Activities, Education, and Cognitive Impairment in Chinese Older Adults: A Population-Based Longitudinal Study. International Psychogeriatrics; Cambridge University Press: Cambridge, UK, 2017; pp. 727–739. [Google Scholar]
- Statistical Bureau of China. The 4th National Census in 1990; China Statistics Press: Beijing, China, 1993. [Google Scholar]
- Xu, Y.; Wang, L.; He, J.; Bi, Y.; Li, M.; Wang, T.; Xu, M. Prevalence and control of diabetes in Chinese adults. JAMA 2013, 310, 948–958. [Google Scholar] [CrossRef]
- Lv, Y.B.; Gao, X.; Yin, Z.X.; Chen, H.S.; Luo, J.S.; Brasher, M.S.; Shi, X.M. Revisiting the association of blood pressure with mortality in oldest old people in China: Community based, longitudinal prospective study. BMJ 2018, 361, k2158. [Google Scholar] [CrossRef]
- Jaacks, L.M.; Gordon-Larsen, P.; Mayer-Davis, E.J.; Adair, L.S.; Popkin, B. Age, period and cohort effects on adult body mass index and overweight from 1991 to 2009 in China: The China Health and Nutrition Survey. Int. J. Epidemiol. 2013, 42, 828–837. [Google Scholar] [CrossRef]
- Murphy, R.; Tao, R.; Lu, X. Son preference in rural China: Patrilineal families and socioeconomic change. Popul. Dev. Rev. 2011, 37, 665–690. [Google Scholar] [CrossRef]
- Wagstaff, A.; Yip, W.; Lindelow, M.; Hsiao, W.C. China’s health system and its reform: A review of recent studies. Health Econ. 2010, 18, S7–S23. [Google Scholar] [CrossRef]
- Liu, A. Chinese Adults’ Dietary Patterns and Their Relationship with Hypertension among Residents in Nine Provinces (1997–2009); China Center for Disease Control and Prevention: Beijing, China, 2011. [Google Scholar]
- Ma, Y. The Impact of Socioeconomic Status and Dietary-Related Factors on Blood Pressure among Adults in 9 Provinces of China (1991–2009); China Center for Disease Control and Prevention: Beijing, China, 2011. [Google Scholar]
- Chen, M.; Qian, D.; Feng, Z.; Si, L. Is outpatient care benefit distribution of government healthcare subsidies equitable in rural ethnic minority areas of China? Results from cross-sectional studies in 2010 and 2013. BMJ Open 2018, 8, e019564. [Google Scholar] [CrossRef]
- Si, L.; Chen, M.; Palmer, A.J. Has equity in government subsidy on healthcare improved in China? Evidence from the China’s National Health Services Survey. Int. J. Equity Health 2017, 16, 6. [Google Scholar] [CrossRef]
- Sheffield, K.M.; Peek, M.K. Changes in the prevalence of cognitive impairment among older Americans, 1993–2004: Overall trends and differences by race/ethnicity. Am. J. Epidemiol. 2011, 174, 274. [Google Scholar] [CrossRef]
- Zhan, H.J. Aging, health care, and elder care: Perpetuation of gender inequalities in China. Health Care Women Int. 2005, 26, 693–712. [Google Scholar] [CrossRef]
- Zimmer, Z.; Kwong, J. Socioeconomic status and health among older adults in rural and urban China. J. Aging Health 2004, 16, 44. [Google Scholar] [CrossRef] [PubMed]
- Hannum, E. Poverty and basic education in rural China: Villages, households, and girls’ and boys’ enrollment. Comput. Educ. Rev. 2003, 47, 141–159. [Google Scholar] [CrossRef]
- Li, C.; Zeng, L.; Dibley, J.M.; Wang, D.; Pei, L.; Yan, H. Evaluation of socio-economic inequalities in the use of maternal health services in rural western China. Public Health 2015, 129, 1251–1257. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | 2002 | 2005 | 2008 | 2011 | 2014 |
|---|---|---|---|---|---|
| Follow up | 6087 | 6236 | 4482 | 2974 | |
| New participants | 14,950 | 7876 | 8184 | 3228 | 2548 |
| Deceased interviewees/ No response | 8863 | 7727 | 9938 | 4736 | |
| Surviving interviewees, mean (standard error) or % | |||||
| Birth cohorts a | |||||
| Cohort 1891–1900 | 11.8 | 3.7 | 0.7 | 0.1 | 0.1 |
| Cohort 1901–1910 | 26.9 | 25.5 | 22.4 | 11.6 | 5.2 |
| Cohort 1911–1920 | 27.1 | 30.6 | 30.8 | 25.2 | 20.1 |
| Cohort 1921–1930 | 20.5 | 19.1 | 22.9 | 27.9 | 29.7 |
| Cohort 1931–1940 | 13.7 | 21.2 | 18.6 | 26.4 | 32.9 |
| Cohort 1941–1950 | 4.7 | 8.8 | 12.1 | ||
| Age group (years) b | |||||
| 65–79 | 31.3 | 33.0 | 27.3 | 33.2 | 33.7 |
| 80–89 | 26.2 | 24.2 | 25.8 | 27.5 | 31.3 |
| 90–99 | 22.9 | 24.8 | 27.4 | 25.5 | 22.9 |
| 100– | 19.6 | 18.0 | 19.4 | 13.8 | 12.1 |
| Men c | 42.9 | 43.3 | 43.1 | 45.4 | 46.4 |
| Urban area d | 46.0 | 45.1 | 40.0 | 48.7 | 47.0 |
| Economic independence e | 26.8 | 29.5 | 26.2 | 28.0 | 27.1 |
| Household income per capita f | 48.2 | 44.7 | 47.3 | 50.8 | 47.3 |
| Education g | 38.5 | 39.8 | 38.0 | 42.4 | 43.1 |
| Marital status h | |||||
| Never married | 1.2 | 0.8 | 0.8 | 1.0 | 1.1 |
| Widowed | 66.3 | 65.4 | 66.5 | 59.9 | 58.1 |
| Divorced/separated | 2.4 | 2.3 | 2.0 | 1.9 | 1.8 |
| Married | 30.1 | 31.6 | 30.7 | 37.1 | 39.0 |
| Smoking i | |||||
| Currently smoking | 65.3 | 63.4 | 66.9 | 64.9 | 69.3 |
| Past smoking | 16.1 | 17.0 | 16.0 | 16.7 | 13.8 |
| Non-smoking | 18.6 | 19.6 | 17.1 | 18.4 | 16.8 |
| Drinking j | |||||
| Currently drinking | 66.8 | 65.3 | 69.1 | 67.3 | 74.6 |
| Past drinking | 12.5 | 14.1 | 13.9 | 15.3 | 10.2 |
| Non-drinking | 20.7 | 20.6 | 17.1 | 17.5 | 15.2 |
| Frequency of fruit intake k | |||||
| Every day or almost every day | 11.1 | 11.4 | 13.0 | 13.8 | 14.5 |
| Quite often | 22.7 | 24.9 | 25.3 | 24.0 | 27.0 |
| Occasionally | 39.8 | 36.8 | 37.3 | 35.1 | 33.0 |
| Rarely or never | 26.4 | 26.9 | 24.3 | 27.2 | 25.5 |
| Frequency of vegetables intake l | |||||
| Every day or almost every day | 52.2 | 49.8 | 62.3 | 56.8 | 55.5 |
| Quite often | 33.7 | 35.2 | 25.6 | 31.3 | 32.7 |
| Occasionally | 10.4 | 10.9 | 9.5 | 8.2 | 8.2 |
| Rarely or never | 3.7 | 4.0 | 2.5 | 3.7 | 3.6 |
| ADL disability m | 29.9 | 25.1 | 21.1 | 26.7 | 24.6 |
| Cognitive impairment n | 25.0 | 25.7 | 28.2 | 23.6 | 21.4 |
| SBP o | 133.8(0.1) | 130.9(0.2) | 135.8(0.2) | 136.7(0.2) | 139.6(0.3) |
| Cognitive functions p | 22.1(0.1) | 22.0(0.1) | 21.2(0.1) | 22.7(0.1) | 23.2(0.1) |
| Age (years) | Economic Dependence Group | Cohort1891–1900 | Cohort1901–1910 | Cohort1911–1920 | Cohort1921–1930 | Cohort1931–1940 | Cohort1941–1950 |
|---|---|---|---|---|---|---|---|
| 65–79 | Economic dependence | 26.1(0.1) | 26.9(0.1) | 27.8(0.1) | |||
| Economic independence | 27.6(0.1) | 28.2(0.0) | 28.6(0.1) | ||||
| 80–89 | Economic dependence | 22.5(0.1) | 23.7(0.1) | 25.1(0.3) | |||
| Economic independence | 25.3(0.2) | 26.2(0.1) | 27.3(0.3) | ||||
| 90–99 | Economic dependence | 17.7(0.1) | 18.8(0.1) | 20.6(0.4) | |||
| Economic independence | 21.5(0.3) | 22.6(0.2) | 23.9(0.6) | ||||
| 100-– | Economic dependence | 13.3(0.2) | 13.6(0.1) | 14.4(0.5) | |||
| Economic independence | 15.6(0.9) | 17.2(0.5) | 17.3(1.7) |
| Age (years) | Household Income Group | Cohort1891–1900 | Cohort1901–1910 | Cohort1911–1920 | Cohort1921–1930 | Cohort1931–1940 | Cohort1941–1950 |
|---|---|---|---|---|---|---|---|
| 65–79 | Lower income | 26.1(0.1) | 27.2(0.1) | 28.0(0.1) | |||
| Higher income | 27.4(0.1) | 27.9(0.0) | 28.5(0.1) | ||||
| 80–89 | Lower income | 22.1(0.1) | 23.8(0.1) | 25.4(0.3) | |||
| Higher income | 24.3(0.1) | 24.8(0.1) | 26.1(0.3) | ||||
| 90–99 | Lower income | 17.3(0.2) | 18.7(0.2) | 20.6(0.5) | |||
| Higher income | 19.4(0.2) | 20.1(0.1) | 21.7(0.4) | ||||
| 100– | Lower income | 12.3(0.3) | 13.1(0.2) | 13.3(0.7) | |||
| Higher income | 14.8(0.3) | 14.6(0.2) | 15.6(0.6) |
| Age (years) | Education Group | Cohort1891–1900 | Cohort1901–1910 | Cohort1911–1920 | Cohort1921–1930 | Cohort1931–1940 | Cohort1941–1950 |
|---|---|---|---|---|---|---|---|
| 65–79 | Lower educated | 26.1(0.1) | 27.1(0.1) | 28.0(0.1) | |||
| Higher educated | 27.4(0.1) | 28.1(0.0) | 28.6(0.1) | ||||
| 80–89 | Lower educated | 22.1(0.1) | 23.7(0.1) | 25.3(0.3) | |||
| Higher educated | 24.3(0.1) | 25.1(0.1) | 26.3(0.3) | ||||
| 90–99 | Lower educated | 17.3(0.2) | 18.7(0.1) | 20.5(0.5) | |||
| Higher educated | 10.4(0.2) | 22.4(0.1) | 22.0(0.5) | ||||
| 100– | Lower educated | 13.0(0.2) | 13.1(0.2) | 13.4(0.6) | |||
| Higher educated | 15.7(0.5) | 14.8(0.2) | 15.9(0.6) |
| Variables | Model A | Model B | Model C | Model D | ||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Birth cohorts | 3.98(3.88, 4.07) | 0.28(0.14, 0.43) | 3.68(3.58, 3.77) | 0.26(0.12, 0.41) | 3.66(3.56, 3.76) | 0.27(0.12, 0.41) | 3.84(3.74, 3.95) | 0.46(0.31, 0.61) |
| Gender | 6.14(5.68, 6.59) | 4.16(3.74, 4.58) | 5.03(4.57, 5.49) | 3.45(3.03, 3.87) | 5.03(4.55, 5.52) | 3.43(2.99, 3.88) | 3.43(2.89, 3.97) | 1.97(1.47, 2.46) |
| Area | 1.08(0.68, 1.49) | 1.71(1.35, 2.08) | 0.37(−0.03, 0.78) | 1.26(0.89, 1.63) | 0.65(0.22, 1.08) | 1.53(1.13, 1.92) | −0.18(−0.63, 0.27) | 0.66(0.24, 1.07) |
| Birth cohorts * Gender | −1.04(−1.16, −0.91) | −0.69(−0.80, −0.57) | −1.04(−1.17, −0.91) | −0.68(−0.80, −0.57) | −1.01(−1.14, −0.88) | −0.67(−0.79, −0.54) | −0.56(−0.71, −0.41) | −0.26(−0.4, −0.12) |
| Birth cohorts * Area | −0.11(−0.22, −0.005) | −0.21(−0.31, −0.11) | −0.09(−0.20, 0.02) | −0.20−0.30, −0.10) | −0.10(−0.22, 0.01) | −0.24(−0.35, −0.13) | 0.15(0.03, 0.28) | 0.03(−0.09, 0.14) |
| Education | 1.9(1.71, 2.08) | 1.38(1.21, 1.55) | 1.82(1.5, 2.14) | 1.24(0.95, 1.53) | 4.06(3.42, 4.70) | 3.1(2.51, 3.68) | ||
| Household income | 0.76(0.62, 0.90) | 0.85(0.72, 0.98) | 1.05(0.83, 1.26) | 1.10(0.91, 1.3) | 1.69(1.27, 2.12) | 2.02(1.63, 2.41) | ||
| Economic independence | 1.33(1.16, 1.51) | 0.54(0.38, 0.71) | 1.62(1.28, 1.96) | 0.56(0.25, 0.87) | 4.47(3.71, 5.23) | 3.42(2.72, 4.12) | ||
| Gender * Economic independence | −0.40(−0.76, −0.04) | −0.21(−0.54, 0.12) | −0.61(−0.97, −0.24) | −0.42(−0.75, −0.09) | ||||
| Gender*Education | 0.13(−0.24, 0.50) | 0.20(−0.14, 0.54) | −0.06(−0.43, 0.31) | 0.02(−0.32, 0.36) | ||||
| Gender * Household income | −0.14(−0.41, 0.14) | −0.14(−0.39, 0.11) | −0.05(−0.33, 0.22) | −0.03(−0.28, 0.23) | ||||
| Area * Economic independence | 0.01(−0.33, 0.36) | 0.28(−0.04, 0.59) | −0.35(−0.70, 0.01) | −0.08(−0.41, 0.24) | ||||
| Area * Education | 0.02(−0.29, 0.33) | 0.05(−0.23, 0.34) | −0.10(−0.41, 0.21) | −0.05(−0.34, 0.23) | ||||
| Area * Household income | −0.52(−0.79, −0.25) | −0.46(−0.71, −0.20) | −0.49(−0.76, −0.21) | −0.43(−0.68, −0.18) | ||||
| Birth cohorts * Education | −0.59(−0.74, −0.44) | −0.49(−0.62, −0.35) | ||||||
| Birth cohorts * Household income | −0.20(−0.31, −0.09) | −0.28(−0.39, −0.18) | ||||||
| Birth cohorts * Economic independence | −0.63(−0.79, −0.48) | −0.64(−0.78, −0.50) | ||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, F.; Cao, J.; Qian, D.; Ma, A. Stronger Increases in Cognitive Functions among Socio-Economically Disadvantaged Older Adults in China: A Longitudinal Analysis with Multiple Birth Cohorts. Int. J. Environ. Res. Public Health 2020, 17, 2418. https://doi.org/10.3390/ijerph17072418
Yang F, Cao J, Qian D, Ma A. Stronger Increases in Cognitive Functions among Socio-Economically Disadvantaged Older Adults in China: A Longitudinal Analysis with Multiple Birth Cohorts. International Journal of Environmental Research and Public Health. 2020; 17(7):2418. https://doi.org/10.3390/ijerph17072418
Chicago/Turabian StyleYang, Fan, Jiangling Cao, Dongfu Qian, and Aixia Ma. 2020. "Stronger Increases in Cognitive Functions among Socio-Economically Disadvantaged Older Adults in China: A Longitudinal Analysis with Multiple Birth Cohorts" International Journal of Environmental Research and Public Health 17, no. 7: 2418. https://doi.org/10.3390/ijerph17072418
APA StyleYang, F., Cao, J., Qian, D., & Ma, A. (2020). Stronger Increases in Cognitive Functions among Socio-Economically Disadvantaged Older Adults in China: A Longitudinal Analysis with Multiple Birth Cohorts. International Journal of Environmental Research and Public Health, 17(7), 2418. https://doi.org/10.3390/ijerph17072418




