Methodological Approaches to Support Process Improvement in Emergency Departments: A Systematic Review
Abstract
1. Introduction
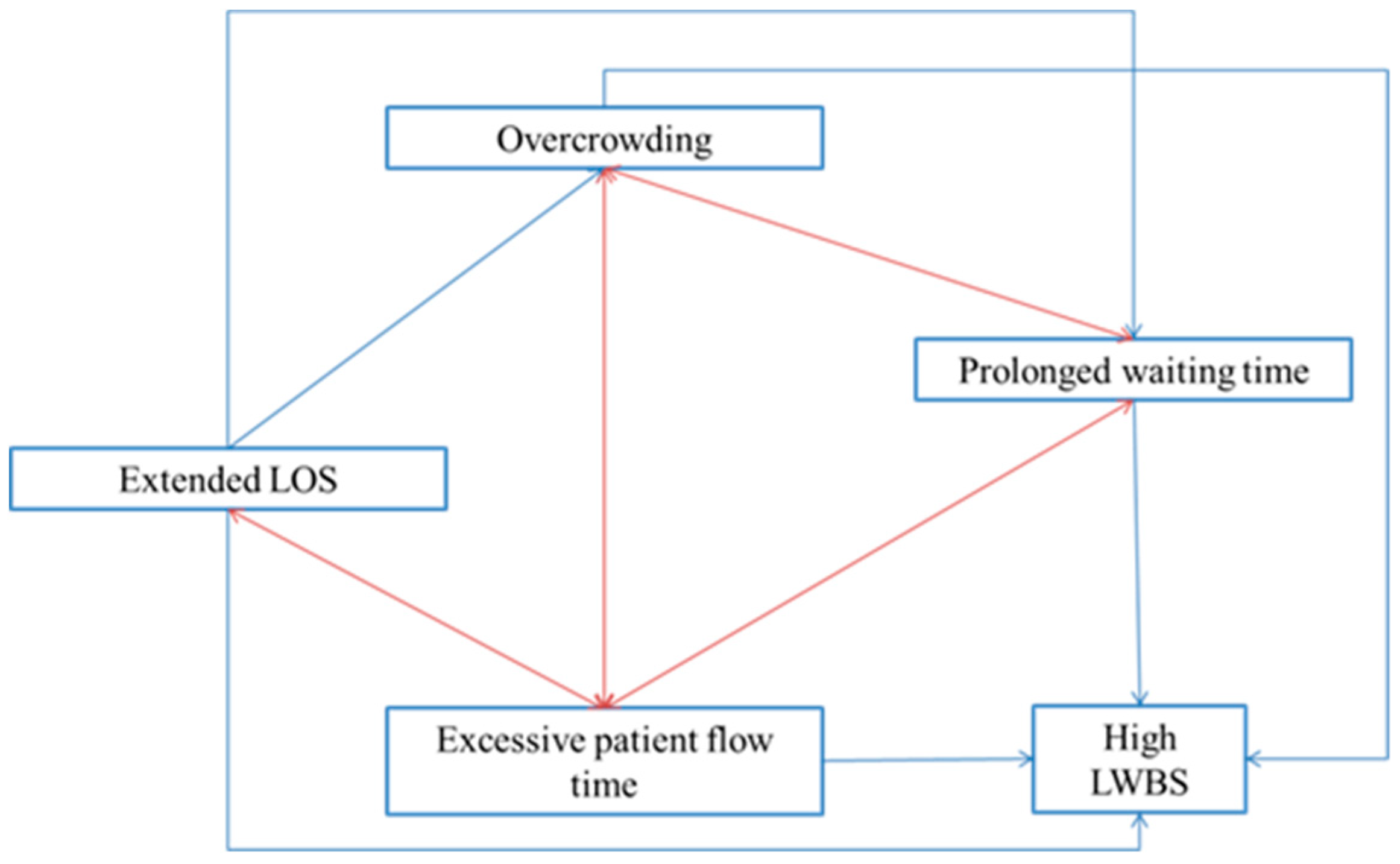
1.1. The Top-Five Leading Problems in EDs: Causes and Consequences
1.1.1. Overcrowding
1.1.2. Prolonged Waiting Time
1.1.3. Extended Length of Stay (LOS)
1.1.4. Excessive Patient Flow time
1.1.5. High Number of Patients Who Leave the ED without Being Seen
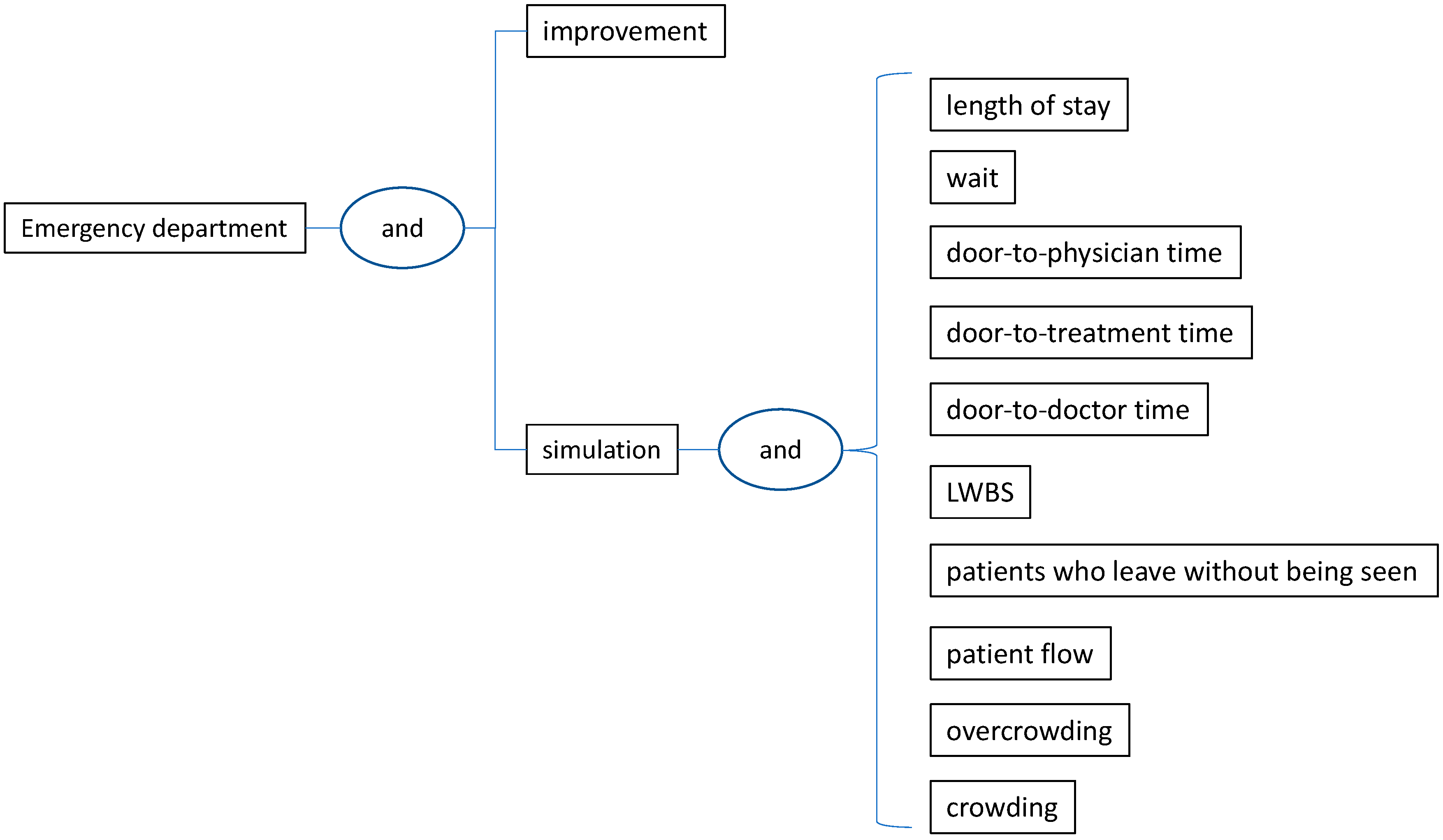
2. Methods
2.1. Framework for Literature Review
2.2. The Process-Improvement Methodologies Used for Tackling the 5-Top Leading Problems in EDs
3. Results
3.1. Papers Focusing on Reducing the Extended LOS
3.2. Papers Focusing on Reducing the Waiting Time
3.3. Papers Focusing on Tackling the Overcrowding
3.4. Papers Focusing on Diminishing the Patient Flow Time in ED
3.5. Papers Focusing on Diminishing the Number of Patients Who Leave the ED Without Being Seen
4. Discussion
5. Concluding Remarks and Future Directions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Soril, L.J.J.; Leggett, L.E.; Lorenzetti, D.L.; Noseworthy, T.W.; Clement, F.M. Reducing frequent visits to the emergency department:A systematic review of interventions. PLoS ONE 2015, 10, e0123660. [Google Scholar] [CrossRef] [PubMed]
- Jarvis, P.R.E. Improving emergency department patient flow. Clin. Exp. Emerg. Med. 2016, 3, 63. [Google Scholar] [CrossRef] [PubMed]
- Emergency Department Quality Improvement: Transforming the Delivery of Care. Available online: https://www.healthcatalyst.com/insights/emergency-department-quality-improvement-transforming-delivery-care (accessed on 20 March 2020).
- Migita, R.; Yoshida, H.; Rutman, L.; Woodward, G.A. Quality Improvement Methodologies: Principles and Applications in the Pediatric Emergency Department. Pediatr. Clin. N. Am. 2018, 65, 1283–1296. [Google Scholar] [CrossRef] [PubMed]
- Holden, R.J. Lean thinking in emergency departments: A critical review. Ann. Emerg. Med. 2011, 57, 265–278. [Google Scholar] [CrossRef] [PubMed]
- Mazzocato, P.; Savage, C.; Brommels, M.; Aronsson, H.; Thor, J. Lean thinking in healthcare: A realist review of the literature. Qual. Saf. Health Care 2010, 19, 376–382. [Google Scholar] [CrossRef]
- Günal, M.M.; Pidd, M. Discrete event simulation for performance modelling in health care: A review of the literature. J. Simul. 2010, 4, 42–51. [Google Scholar] [CrossRef]
- Paul, S.A.; Reddy, M.C.; Deflitch, C.J. A systematic review of simulation studies investigating emergency department overcrowding. Simulation 2010, 86, 559–571. [Google Scholar] [CrossRef]
- Vanbrabant, L.; Braekers, K.; Ramaekers, K.; Van Nieuwenhuyse, I. Simulation of emergency department operations: A comprehensive review of KPIs and operational improvements. Comput. Ind. Eng. 2019, 131, 356–381. [Google Scholar] [CrossRef]
- Saghafian, S.; Austin, G.; Traub, S.J. Operations research/management contributions to emergency department patient flow optimization: Review and research prospects. IIE Trans. Healthc. Syst. Eng. 2015, 5, 101–123. [Google Scholar] [CrossRef]
- Althaus, F.; Paroz, S.; Hugli, O.; Ghali, W.A.; Daeppen, J.; Peytremann-Bridevaux, I.; Bodenmann, P. Effectiveness of interventions targeting frequent users of emergency departments: A systematic review. Ann. Emerg. Med. 2011, 58, 41–52. [Google Scholar] [CrossRef]
- Flores-Mateo, G.; Violan-Fors, C.; Carrillo-Santisteve, P.; Peiró, S.; Argimon, J. Effectiveness of organizational interventions to reduce emergency department utilization: A systematic review. PLoS ONE 2012, 7, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Boyle, A.; Beniuk, K.; Higginson, I.; Atkinson, P. Emergency Department Crowding: Time for Interventions and Policy Evaluations. Emerg. Med. Int. 2012, 2012, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Crawford, K.; Morphet, J.; Jones, T.; Innes, K.; Griffiths, D.; Williams, A. Initiatives to reduce overcrowding and access block in Australian emergency departments: A literature review. Collegian 2014, 21, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Uscher-Pines, L.; Pines, J.; Kellermann, A.; Gillen, E.; Mehrotra, A. Deciding to Visit the Emergency Departement for Non-Urgent Conditions: A Systematic Review of the Literature. Am. J. Manag. Care 2013, 19, 47. [Google Scholar]
- Oredsson, S.; Jonsson, H.; Rognes, J.; Lind, L.; Göransson, K.E.; Ehrenberg, A.; Asplund, K.; Castrén, M.; Farrohknia, N. A systematic review of triage-related interventions to improve patient flow in emergency departments. Scand. J. Trauma Resusc. Emerg. Med. 2011, 19. [Google Scholar] [CrossRef]
- Clarey, A.J.; Cooke, M.W. Patients who leave emergency departments without being seen: Literature review and English data analysis. Emerg. Med. J. 2012, 29, 617–621. [Google Scholar] [CrossRef]
- Marcozzi, D.; Carr, B.; Liferidge, A.; Baehr, N.; Browne, B. Trends in the Contribution of Emergency Departments to the Provision of Hospital-Associated Health Care in the USA. Int. J. Health Serv. 2018, 48, 267–288. [Google Scholar] [CrossRef]
- Bellow, A.A.; Gillespie, G.L. The evolution of ED crowding. J. Emerg. Nurs. 2014, 40, 153–160. [Google Scholar] [CrossRef]
- Ashour, O.M.; Okudan Kremer, G.E. Dynamic patient grouping and prioritization: A new approach to emergency department flow improvement. Health Care Manag. Sci. 2016, 19, 192–205. [Google Scholar] [CrossRef]
- Tiwari, Y.; Goel, S.; Singh, A. Arrival time pattern and waiting time distribution of patients in the emergency outpatient department of a tertiary level health care institution of North India. J. Emerg. Trauma Shock 2014, 7, 160–165. [Google Scholar]
- Driesen, B.E.J.M.; Van Riet, B.H.G.; Verkerk, L.; Bonjer, H.J.; Merten, H.; Nanayakkara, P.W.B. Long length of stay at the emergency department is mostly caused by organisational factors outside the influence of the emergency department: A root cause analysis. PLoS ONE 2018, 13, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Mason, S.; Weber, E.J.; Coster, J.; Freeman, J.; Locker, T. Time patients spend in the emergency department: England’s 4-hour rule—A case of hitting the target but missing the point? Ann. Emerg. Med. 2012, 59, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Herring, A.; Wilper, A.; Himmelstein, D.U.; Woolhandler, S.; Espinola, J.A.; Brown, D.F.M.; Camargo Jr, C.A. Increasing length of stay among adult visits to U.S. emergency departments, 2001–2005. Acad. Emerg. Med. 2009, 16, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Easter, B.; Houshiarian, N.; Pati, D.; Wiler, J.L. Designing efficient emergency departments: Discrete event simulation of internal-waiting areas and split flow sorting. Am. J. Emerg Med. 2019, 37, 2186–2193. [Google Scholar] [CrossRef]
- Fuentes, E.; Shields, J.; Chirumamilla, N.; Martinez, M.; Kaafarani, H.; Yeh, D.D.; White, B.; Filbin, M.; DePesa, C.; Velmahos, G.; et al. “One-way-street” streamlined admission of critically ill trauma patients reduces emergency department length of stay. Intern. Emerg. Med. 2017, 12, 1019–1024. [Google Scholar] [CrossRef]
- Ajdari, A.; Boyle, L.N.; Kannan, N.; Wang, J.; Rivara, F.P.; Vavilala, M.S. Simulation of the Emergency Department Care Process for Pediatric Traumatic Brain Injury. J. Healthc. Qual. 2018, 40, 110–118. [Google Scholar] [CrossRef]
- Best, A.M.; Dixon, C.A.; Kelton, W.D.; Lindsell, C.J.; Ward, M.J. Using discrete event computer simulation to improve patient flow in a Ghanaian acute care hospital. Am. J. Emerg. Med. 2014, 32, 917–922. [Google Scholar] [CrossRef]
- Bokhorst, J.A.C.; van der Vaart, T. Acute medical unit design – The impact of rearranged patient flows. Socio-Econ. Plan. Sci. 2018, 62, 75–83. [Google Scholar] [CrossRef]
- Coughlan, J.; Eatock, J.; Patel, N. Simulating the use of re-prioritisation as a wait-reduction strategy in an emergency department. Emerg. Med. J. 2011, 28, 1013–1018. [Google Scholar] [CrossRef]
- Gul, M.; Guneri, A.F. A computer simulation model to reduce patient length of stay and to improve resource utilization rate in an emergency department service system. Int. J. Ind. Eng. Theory Appl. Pract. 2012, 19, 221–231. [Google Scholar]
- Hung, G.R.; Kissoon, N. Impact of an observation unit and an emergency department-admitted patient transfer mandate in decreasing overcrowding in a pediatric emergency department: A discrete event simulation exercise. Pediatr. Emerg. Care 2009, 25, 160–163. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, I.M.; Liong, C.; Bakar, S.A.; Najmuddin, A.F. Performance improvement of the yellow zone in emergency department using discrete event simulation approach. Int. J. Eng. Technol. 2018, 7, 102–105. [Google Scholar]
- Keyloun, K.R.; Lofgren, E.; Hebert, S. Modeling operational quality metrics and costs of long-acting antibiotics for acute bacterial skin and skin structure infection treatment in the emergency department. J. Med. Econ. 2019, 22, 652–661. [Google Scholar] [CrossRef] [PubMed]
- Khare, R.K.; Powell, E.S.; Reinhardt, G.; Lucenti, M. Adding More Beds to the Emergency Department or Reducing Admitted Patient Boarding Times: Which Has a More Significant Influence on Emergency Department Congestion? Ann. Emerg. Med. 2009, 53, 575–585. [Google Scholar] [CrossRef]
- Konrad, R.; DeSotto, K.; Grocela, A.; McAuley, P.; Wang, J.; Lyons, J.; Bruin, M. Modeling the impact of changing patient flow processes in an emergency department: Insights from a computer simulation study. Oper. Res. Health Care 2013, 2, 66–74. [Google Scholar] [CrossRef]
- La, J.; Jewkes, E.M. Defining an optimal ED fast track strategy using simulation. J. Enterp. Inf. Manag. 2013, 26, 109–118. [Google Scholar] [CrossRef]
- Baia Medeiros, D.T.; Hahn-Goldberg, S.; Aleman, D.M.; O’Connor, E. Planning Capacity for Mental Health and Addiction Services in the Emergency Department: A Discrete-Event Simulation Approach. J. Healthc. Eng. 2019, 2019, 8973515. [Google Scholar] [CrossRef]
- Oh, C.; Novotny, A.M.; Carter, P.L.; Ready, R.K.; Campbell, D.D.; Leckie, M.C. Use of a simulation-based decision support tool to improve emergency department throughput. Oper. Res. Health Care 2016, 9, 29–39. [Google Scholar] [CrossRef]
- Paul, J.A.; Lin, L. Models for improving patient throughput and waiting at hospital emergency departments. J. Emerg. Med. 2012, 43, 1119–1126. [Google Scholar] [CrossRef]
- Rasheed, F.; Lee, Y.H.; Kim, S.H.; Park, I.C. Development of emergency department load relief area-gauging benefits in empirical terms. Simul. Healthc. 2012, 7, 343–352. [Google Scholar] [CrossRef]
- Rosmulder, R.W.; Krabbendam, J.J.; Kerkhoff, A.H.M.; Houser, C.M.; Luitse, J.S.K. Erratum to: Computer Simulation Within Action Research: A Promising Combination for Improving Healthcare Delivery? (Syst Pract Action Res, 10.1007/s11213-011-9191-y). Syst. Pract. Action Res. 2011, 24, 273. [Google Scholar] [CrossRef][Green Version]
- Saoud, M.S.; Boubetra, A.; Attia, S. A simulation knowledge extraction-based decision support system for the healthcare emergency department. Int. J. Healthc. Inf. Syst. Inform. 2016, 11, 19–37. [Google Scholar] [CrossRef]
- Steward, D.; Glass, T.F.; Ferrand, Y.B. Simulation-Based Design of ED Operations with Care Streams to Optimize Care Delivery and Reduce Length of Stay in the Emergency Department. J. Med. Syst. 2017, 41, 162. [Google Scholar] [CrossRef] [PubMed]
- Thomas Schneider, A.J.; Luuk Besselink, P.; Zonderland, M.E.; Boucherie, R.J.; Van Den Hout, W.B.; Kievit, J.; Bilars, P.; Jaap Fogteloo, A.; Rabelink, T.J. Allocating emergency beds improves the emergency admission flow. Interfaces 2018, 48, 384–394. [Google Scholar] [CrossRef]
- Wang, T.; Guinet, A.; Belaidi, A.; Besombes, B. Modelling and simulation of emergency services with ARIS and Arena. case study: The emergency department of Saint Joseph and Saint Luc hospital. Prod. Plan. Control. 2009, 20, 484–495. [Google Scholar] [CrossRef]
- Zeng, Z.; Ma, X.; Hu, Y.; Li, J.; Bryant, D. A Simulation Study to Improve Quality of Care in the Emergency Department of a Community Hospital. J. Emerg. Nurs. 2012, 38, 322–328. [Google Scholar] [CrossRef]
- Allaudeen, N.; Vashi, A.; Breckenridge, J.S.; Haji-Sheikhi, F.; Wagner, S.; Posley, K.A.; Asch, S.M. Using Lean Management to Reduce Emergency Department Length of Stay for Medicine Admissions. Qual Manag. Health Care 2017, 26, 91–96. [Google Scholar] [CrossRef]
- Arbune, A.; Wackerbarth, S.; Allison, P.; Conigliaro, J. Improvement through Small Cycles of Change: Lessons from an Academic Medical Center Emergency Department. J. Healthc. Qual. 2017, 39, 259–269. [Google Scholar] [CrossRef]
- Carter, P.M.; Desmond, J.S.; Akanbobnaab, C.; Oteng, R.A.; Rominski, S.D.; Barsan, W.G.; Cunningham, R.M. Optimizing clinical operations as part of a global emergency medicine initiative in Kumasi, Ghana: Application of lean manufacturing principals to low-resource health systems. Acad. Emerg. Med. 2012, 19, 338–347. [Google Scholar] [CrossRef]
- Dickson, E.W.; Anguelov, Z.; Bott, P.; Nugent, A.; Walz, D.; Singh, S. The sustainable improvement of patient flow in an emergency treatment centre using Lean. Int. J. Six Sigma Compet. Advant. 2008, 4, 289–304. [Google Scholar] [CrossRef]
- Dickson, E.W.; Anguelov, Z.; Vetterick, D.; Eller, A.; Singh, S. Use of Lean in the Emergency Department: A Case Series of 4 Hospitals. Ann. Emerg. Med. 2009, 54, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Dickson, E.W.; Singh, S.; Cheung, D.S.; Wyatt, C.C.; Nugent, A.S. Application of Lean Manufacturing Techniques in the Emergency Department. J. Emerg. Med. 2009, 37, 177–182. [Google Scholar] [CrossRef]
- Elamir, H. Improving patient flow through applying lean concepts to emergency department. Lead. Health Serv. 2018, 31, 293–309. [Google Scholar] [CrossRef] [PubMed]
- Hitti, E.A.; El-Eid, G.R.; Tamim, H.; Saleh, R.; Saliba, M.; Naffaa, L. Improving Emergency Department radiology transportation time: A successful implementation of lean methodology. BMC Health Serv. Res. 2017, 17, 625. [Google Scholar] [CrossRef] [PubMed]
- Kane, M.; Chui, K.; Rimicci, J.; Callagy, P.; Hereford, J.; Shen, S.; Norris, R.; Pickham, D. Lean manufacturing improves emergency department throughput and patient satisfaction. J. Nurs. Admin. 2015, 45, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Migita, R.; Del Beccaro, M.; Cotter, D.; Woodward, G.A. Emergency department overcrowding: Developing emergency department capacity through process improvement. Clin. Pediatr. Emerg. Med. 2011, 12, 141–150. [Google Scholar] [CrossRef]
- Murrell, K.L.; Offerman, S.R.; Kauffman, M.B. Applying Lean: Implementation of a rapid triage and treatment system. West. J. Emerg Med. 2011, 12, 184–191. [Google Scholar]
- Ng, D.; Vail, G.; Thomas, S.; Schmidt, N. Applying the Lean principles of the Toyota Production System to reduce wait times in the emergency department. Can. J. Emerg. Med. 2010, 12, 50–57. [Google Scholar] [CrossRef]
- Peng, L.S.; Rasid, M.F.; Salim, W.I. Using modified triage system to improve emergency department efficacy: A successful Lean implementation. Int. J. Healthc. Manag. 2019. [Google Scholar] [CrossRef]
- Polesello, V.; Dittadi, R.; Afshar, H.; Bassan, G.; Rosada, M.; Ninno, L.D.; Carraro, P. Improving pre-analytical laboratory turnaround time for the emergency department: Outcomes of a pneumatic tube system introduction. Biochim. Clin. 2019, 43, 150–155. [Google Scholar]
- Rotteau, L.; Webster, F.; Salkeld, E.; Hellings, C.; Guttmann, A.; Vermeulen, M.J.; Bell, R.S.; Zwarenstein, M.; Rowe, B.H.; Nigam, A.; et al. Ontario’s emergency department process improvement program: The experience of implementation. Acad. Emerg. Med. 2015, 22, 720–729. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, M.; Suárez, M.; Asenjo, M.; Bragulat, E. Improvement of emergency department patient flow using lean thinking. Int. J. Qual. Health Care 2018, 30, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Sayed, M.J.E.; El-Eid, G.R.; Saliba, M.; Jabbour, R.; Hitti, E.A. Improving emergency department door to doctor time and process reliability: A successful implementation of lean methodology. Medicine 2015, 94, e1679. [Google Scholar] [CrossRef] [PubMed]
- Van Der Linden, M.C.; Van Ufford, H.M.E.; De Beaufort, R.A.Y.; Grauss, R.W.; Hofstee, H.M.A.; Hoogendoorn, J.M.; Meylaerts, S.A.G.; Rijsman, R.M.; De Rooij, T.P.W.; Smith, C.; et al. The impact of a multimodal intervention on emergency department crowding and patient flow. Int. J. Emerg. Med. 2019, 12, 21. [Google Scholar] [CrossRef]
- Vermeulen, M.J.; Stukel, T.A.; Guttmann, A.; Rowe, B.H.; Zwarenstein, M.; Golden, B.; Nigam, A.; Anderson, G.; Bell, R.S.; Schull, M.J. Evaluation of an emergency department lean process improvement program to reduce length of stay. Ann. Emerg. Med. 2014, 64, 427–438. [Google Scholar] [CrossRef]
- White, B.A.; Chang, Y.; Grabowski, B.G.; Brown, D.F.M. Using lean-based systems engineering to increase capacity in the emergency department. West. J. Emerg. Med. 2014, 15, 770–776. [Google Scholar] [CrossRef][Green Version]
- Cheng, I.; Zwarenstein, M.; Kiss, A.; Castren, M.; Brommels, M.; Schull, M. Factors associated with failure of emergency wait-time targets for high acuity discharges and intensive care unit admissions. Can. J. Emerg. Med. 2018, 20, 112–124. [Google Scholar] [CrossRef]
- Forero, R.; Man, N.; McCarthy, S.; Richardson, D.; Mohsin, M.; Toloo, G.S.; FitzGerald, G.; Ngo, H.; Mountain, D.; Fatovich, D.; et al. Impact of the national emergency access target policy on emergency departments’ performance: A time-trend analysis for New South Wales, Australian capital territory and queensland. EMA Emerg. Med. Australas 2019, 31, 253–261. [Google Scholar] [CrossRef]
- Kaushik, N.; Khangulov, V.S.; O’hara, M.; Arnaout, R. Reduction in laboratory turnaround time decreases emergency room length of stay. Open Access Emerg. Med. 2018, 10, 37–45. [Google Scholar] [CrossRef]
- Maniaci, M.J.; Lachner, C.; Vadeboncoeur, T.F.; Hodge, D.O.; Dawson, N.L.; Rummans, T.A.; Roy, A.; Burton, M.C. Involuntary patient length-of-stay at a suburban emergency department. Am. J. Emerg. Med. 2019. [Google Scholar] [CrossRef]
- Singh, N.; Robinson, R.D.; Duane, T.M.; Kirby, J.J.; Lyell, C.; Buca, S.; Gandhi, R.; Mann, S.M.; Zenarosa, N.R.; Wang, H. Role of ED crowding relative to trauma quality care in a Level 1 Trauma Center. Am. J. Emerg. Med. 2019, 37, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Street, M.; Mohebbi, M.; Berry, D.; Cross, A.; Considine, J. Influences on emergency department length of stay for older people. Eur. J. Emerg. Med. 2018, 25, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Van der Veen, D.; Remeijer, C.; Fogteloo, A.J.; Heringhaus, C.; de Groot, B. Independent determinants of prolonged emergency department length of stay in a tertiary care centre: A prospective cohort study. Scand. J. Trauma Resusc. Emerg. Med. 2018, 26, 81. [Google Scholar] [CrossRef] [PubMed]
- Yau, F.F.; Tsai, T.; Lin, Y.; Wu, K.; Syue, Y.; Li, C. Can different physicians providing urgent and non-urgent treatment improve patient flow in emergency department? Am. J. Emerg. Med. 2018, 36, 993–997. [Google Scholar] [CrossRef] [PubMed]
- Brent, A.S.; Rahman, W.M.; Knarr, L.L.; Harrison, J.A.; Kearns, K.L.; Lindstrom, D.S. Reducing cycle times in pediatric emergency medicine. Pediatr. Emerg. Care 2009, 25, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, C.M.B.; Christenson, J.M. Use of continuous quality improvement to facilitate patient flow through the triage and Fast-Track areas of an emergency department. J. Emerg. Med. 1995, 13, 847–855. [Google Scholar] [CrossRef]
- Fernandes, C.M.B.; Christenson, J.M.; Price, A. Continuous quality improvement reduces length of stay for fast-track patients in an emergency department. Acad. Emerg. Med. 1996, 3, 258–263. [Google Scholar] [CrossRef]
- Higgins, G.L., III; Becker, M.H. A continuous quality improvement approach to IL-372 documentation compliance in an academic emergency department, and its impact on dictation costs, billing practices, and average patient length of stay. Acad. Emerg. Med. 2000, 7, 269–275. [Google Scholar] [CrossRef]
- Lovett, P.B.; Illg, M.L.; Sweeney, B.E. A Successful Model for a Comprehensive Patient Flow Management Center at an Academic Health System. Am. J. Med. Qual. 2014, 31, 246–255. [Google Scholar] [CrossRef]
- Preyde, M.; Crawford, K.; Mullins, L. Patients’ satisfaction and wait times at Guelph General Hospital Emergency Department before and after implementation of a process improvement project. Can. J. Emerg. Med. 2012, 14, 157–168. [Google Scholar] [CrossRef]
- Rehmani, R.; Amatullah, A.F. Quality improvement program in an Emergency Department. Saudi Med. J. 2008, 29, 418–422. [Google Scholar] [PubMed]
- Ajmi, F.; Zgaya, H.; Othman, S.B.; Hammadi, S. Agent-based dynamic optimization for managing the workflow of the patient’s pathway. Simul. Model. Pract. Theory 2019, 96, 101935. [Google Scholar] [CrossRef]
- Haydar, S.A.; Strout, T.D.; Baumann, M.R. Sustainable Mechanism to Reduce Emergency Department (ED) Length of Stay: The Use of ED Holding (ED Transition) Orders to Reduce ED Length of Stay. Acad. Emerg. Med. 2016, 23, 776–785. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Prybutok, G.L. Ninety to Nothing: A PDSA quality improvement project. Int. J. Health Care Qual. Assur. 2018, 31, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Oueida, S.; Kotb, Y.; Aloqaily, M.; Jararweh, Y.; Baker, T. An edge computing based smart healthcare framework for resource management. Sensors 2018, 18, 4307. [Google Scholar] [CrossRef]
- Derni, O.; Boufera, F.; Khelfi, M.F. Coloured Petri net for modelling and improving emergency department based on the simulation model. Int. J. Simul. Process. Model. 2019, 14, 72–86. [Google Scholar] [CrossRef]
- Bellew, S.D.; Collins, S.P.; Barrett, T.W.; Russ, S.E.; Jones, I.D.; Slovis, C.M.; Self, W.H. Implementation of an Opioid Detoxification Management Pathway Reduces Emergency Department Length of Stay. Acad. Emerg. Med. 2018, 25, 1157–1163. [Google Scholar] [CrossRef]
- Than, M.P.; Pickering, J.W.; Dryden, J.M.; Lord, S.J.; Aitken, S.A.; Aldous, S.J.; Allan, K.E.; Ardagh, M.W.; Bonning, J.W.N.; Callender, R.; et al. ICare-ACS (Improving Care Processes for Patients with Suspected Acute Coronary Syndrome): A Study of Cross-System Implementation of a National Clinical Pathway. Circulation 2018, 137, 354–363. [Google Scholar] [CrossRef]
- Brouns, S.H.A.; Stassen, P.M.; Lambooij, S.L.E.; Dieleman, J.; Vanderfeesten, I.T.P.; Haak, H.R. Organisational factors induce prolonged emergency department length of stay in elderly patients—A retrospective cohort study. PLoS ONE 2015, 10, e135066. [Google Scholar] [CrossRef]
- Chan, T.C.; Killeen, J.P.; Kelly, D.; Guss, D.A. Impact of rapid entry and accelerated care at triage on reducing emergency department patient wait times, lengths of stay, and rate of left without being seen. Ann. Emerg. Med. 2005, 46, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Christensen, M.; Rosenberg, M.; Mahon, E.; Pineda, S.; Rojas, E.; Soque, V.; Soque, V.; Johansen, M.L. Pivot Nursing: An Alternative to Traditional ED Triage. J. Emerg. Nurs. 2016, 42, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Christianson, J.B.; Warrick, L.H.; Howard, R.; Vollum, J. Deploying Six Sigma in a health care system as a work in progress. Jt. Commun. J. Qual. Patient Saf. 2005, 31, 603–613. [Google Scholar] [CrossRef]
- DeFlitch, C.; Geeting, G.; Paz, H.L. Reinventing emergency department flow via healthcare delivery science. Health Environ. Res. Des. J. 2015, 8, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Rexachs, D.; Epelde, F.; Luque, E. An agent-based model for quantitatively analyzing and predicting the complex behavior of emergency departments. J. Comput. Sci. 2017, 21, 11–23. [Google Scholar] [CrossRef]
- Oueida, S.; Kotb, Y.; Kadry, S.; Ionescu, S. Healthcare Operation Improvement Based on Simulation of Cooperative Resource Preservation Nets for None-Consumable Resources. Complexity 2018, 2018, 4102968. [Google Scholar] [CrossRef]
- Sloan, J.; Chatterjee, K.; Sloan, T.; Holland, G.; Waters, M.; Ewins, D.; Laundy, N. Effect of a pathway bundle on length of stay. Emerg. Med. J. 2009, 26, 479–483. [Google Scholar] [CrossRef]
- Stone-Griffith, S.; Englebright, J.D.; Cheung, D.; Korwek, K.M.; Perlin, J.B. Data-driven process and operational improvement in the emergency department: The ED Dashboard and Reporting Application. J. Healthc. Manag. 2012, 57, 167–181. [Google Scholar] [CrossRef]
- Bish, P.A.; McCormick, M.A.; Otegbeye, M. Ready-JET-Go: Split Flow Accelerates ED Throughput. J. Emerg. Nurs. 2016, 42, 114–119. [Google Scholar] [CrossRef]
- Blick, K.E. Providing critical laboratory results on time, every time to help reduce emergency department length of stay: How our laboratory achieved a six sigma level of performance. Am. J. Clin. Pathol. 2013, 140, 193–202. [Google Scholar] [CrossRef]
- Chadha, R.; Singh, A.; Kalra, J. Lean and queuing integration for the transformation of health care processes A lean health care model. Clin. Gov. 2012, 17, 191–199. [Google Scholar] [CrossRef]
- Chen, T.; Wang, C. Multi-objective simulation optimization for medical capacity allocation in emergency department. J. Simul. 2016, 10, 50–68. [Google Scholar] [CrossRef]
- Elalouf, A.; Wachtel, G. An alternative scheduling approach for improving patient-flow in emergency departments. Oper. Res. Health Care 2015, 7, 94–102. [Google Scholar] [CrossRef]
- Feng, Y.; Wu, I.; Chen, T. Stochastic resource allocation in emergency departments with a multi-objective simulation optimization algorithm. Health Care Manag. Sci. 2017, 20, 55–75. [Google Scholar] [CrossRef]
- Ferrand, Y.B.; Magazine, M.J.; Rao, U.S.; Glass, T.F. Managing responsiveness in the emergency department: Comparing dynamic priority queue with fast track. J. Oper Manag. 2018, 58–59, 15–26. [Google Scholar] [CrossRef]
- Furterer, S.L. Applying Lean Six Sigma methods to reduce length of stay in a hospital’s emergency department. Qual. Eng. 2018, 30, 389–404. [Google Scholar] [CrossRef]
- Ghanes, K.; Jouini, O.; Diakogiannis, A.; Wargon, M.; Jemai, Z.; Hellmann, R.; Thomas, V.; Koole, G. Simulation-based optimization of staffing levels in an emergency department. Simulation 2015, 91, 942–953. [Google Scholar] [CrossRef]
- Goienetxea Uriarte, A.; Ruiz Zúñiga, E.; Urenda Moris, M.; Ng, A.H.C. How can decision makers be supported in the improvement of an emergency department? A simulation, optimization and data mining approach. Oper. Res. Health Care 2017, 15, 102–122. [Google Scholar]
- He, S.; Sim, M.; Zhang, M. Data-driven patient scheduling in emergency departments: A hybrid robust-stochastic approach. Manag. Sci. 2019, 65, 4123–4140. [Google Scholar] [CrossRef]
- Huang, D.; Bastani, A.; Anderson, W.; Crabtree, J.; Kleiman, S.; Jones, S. Communication and bed reservation: Decreasing the length of stay for emergency department trauma patients. Am. J. Emerg. Med. 2018, 36, 1874–1879. [Google Scholar] [CrossRef]
- Kaner, M.; Gadrich, T.; Dror, S.; Marmor, Y.N. Generating and evaluating simulation scenarios to improve emergency department operations. IIE Trans. Healthc. Syst. Eng. 2014, 4, 156–166. [Google Scholar] [CrossRef]
- Lee, E.K.; Atallah, H.Y.; Wright, M.D.; Post, E.T.; Thomas, C.; Wu, D.T.; Haley, L.L. Transforming hospital emergency department workflow and patient care. Interfaces 2015, 45, 58–82. [Google Scholar] [CrossRef]
- Lo, M.D.; Rutman, L.E.; Migita, R.T.; Woodward, G.A. Rapid electronic provider documentation design and implementation in an academic pediatric emergency department. Pediatr. Emerg. Care 2015, 31, 798–804. [Google Scholar] [CrossRef] [PubMed]
- Oueida, S.; Kotb, Y.; Ionescu, S.; Militaru, G. AMS: A new platform for system design and simulation. Int, J. Simul. Model. 2019, 18, 33–46. [Google Scholar] [CrossRef]
- Rachuba, S.; Knapp, K.; Ashton, L.; Pitt, M. Streamlining pathways for minor injuries in emergency departments through radiographer-led discharge. Oper. Res. Health Care 2018, 19, 44–56. [Google Scholar] [CrossRef]
- Romano, E.; Guizzi, G.; Chiocca, D. A decision support tool, implemented in a system dynamics model, to improve the effectiveness in the hospital emergency department. Int. J. Procure Manag. 2015, 8, 141–168. [Google Scholar] [CrossRef]
- Ross, G.; Johnson, D.; Kobernick, M. Evaluation of a critical pathway for stroke. J. Am. Osteopath Assoc. 1997, 97, 269–276. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ross, A.J.; Murrells, T.; Kirby, T.; Jaye, P.; Anderson, J.E. An integrated statistical model of Emergency Department length of stay informed by Resilient Health Care principles. Saf. Sci. 2019, 120, 129–136. [Google Scholar] [CrossRef]
- Shin, S.Y.; Brun, Y.; Balasubramanian, H.; Henneman, P.L.; Osterweil, L.J. Discrete-Event Simulation and Integer Linear Programming for Constraint-Aware Resource Scheduling. IEEE Trans. Syst. Man Cybern. Syst. 2018, 48, 1578–1593. [Google Scholar] [CrossRef]
- Sinreich, D.; Jabali, O. Staggered work shifts: A way to downsize and restructure an emergency department workforce yet maintain current operational performance. Health Care Manag. Sci 2007, 10, 293–308. [Google Scholar] [CrossRef]
- Sinreich, D.; Jabali, O.; Dellaert, N.P. Reducing emergency department waiting times by adjusting work shifts considering patient visits to multiple care providers. IIE Trans. 2012, 44, 163–180. [Google Scholar] [CrossRef]
- Sir, M.Y.; Nestler, D.; Hellmich, T.; Das, D.; Laughlin, M.J.; Dohlman, M.C.; Pasupathy, K. Optimization of multidisciplinary staffing improves patient experiences at the mayo clinic. Interfaces 2017, 47, 425–441. [Google Scholar] [CrossRef]
- Techar, K.; Nguyen, A.; Lorenzo, R.M.; Yang, S.; Thielen, B.; Cain-Nielsen, A.; Hemmila, M.R.; Tignanelli, C.J. Early Imaging Associated With Improved Survival in Older Patients With Mild Traumatic Brain Injuries. J. Surg. Res. 2019, 242, 4–10. [Google Scholar] [CrossRef]
- Visintin, F.; Caprara, C.; Puggelli, F. Experimental design and simulation applied to a pediatric emergency department: A case study. Comput. Ind. Eng. 2019, 128, 755–781. [Google Scholar] [CrossRef]
- Yousefi, M.; Ferreira, R.P.M. An agent-based simulation combined with group decision-making technique for improving the performance of an emergency department. Braz. J. Med. Biol. Res. 2017, 50. [Google Scholar] [CrossRef]
- Yousefi, M.; Yousefi, M.; Ferreira, R.P.M.; Kim, J.H.; Fogliatto, F.S. Chaotic genetic algorithm and Adaboost ensemble metamodeling approach for optimum resource planning in emergency departments. Artif. Intell. Med. 2018, 84, 23–33. [Google Scholar] [CrossRef]
- Yousefi, M.; Yousefi, M.; Fogliatto, F.S.; Ferreira, R.P.M.; Kim, J.H. Simulating the behavior of patients who leave a public hospital emergency department without being seen by a physician: A cellular automaton and agent-based framework. Braz. J. Med. Biol. Res. 2018, 51. [Google Scholar] [CrossRef]
- Zeltyn, S.; Marmor, Y.N.; Mandelbaum, A.; Carmeli, B.; Greenshpan, O.; Mesika, Y.; Wasserkrug, S.; Vortman, P.; Shtub, A.; Lauterman, T.; et al. Simulation-based models of emergency departments: Operational, tactical, and strategic staffing. ACM Trans. Model. Comput. Simul. 2011, 21, 1–25. [Google Scholar] [CrossRef]
- Ashour, O.M.; Okudan Kremer, G.E. A simulation analysis of the impact of FAHP-MAUT triage algorithm on the Emergency Department performance measures. Expert Syst. Appl. 2013, 40, 177–187. [Google Scholar] [CrossRef]
- Aroua, A.; Abdulnour, G. Optimization of the emergency department in hospitals using simulation and experimental design: Case study. Procedia Manuf. 2018, 17, 878–885. [Google Scholar] [CrossRef]
- Abo-Hamad, W.; Arisha, A. Simulation-based framework to improve patient experience in an emergency department. Eur. J. Oper. Res. 2013, 224, 154–166. [Google Scholar] [CrossRef]
- Acuna, J.A.; Zayas-Castro, J.L.; Charkhgard, H. Ambulance allocation optimization model for the overcrowding problem in US emergency departments: A case study in Florida. Socio-Econ. Plan. Sci. 2019. [Google Scholar] [CrossRef]
- Ala, A.; Chen, F. Alternative mathematical formulation and hybrid meta-heuristics for patient scheduling problem in health care clinics. Neural Comput. Appl. 2019, in press. [Google Scholar] [CrossRef]
- Yousefi, M.; Yousefi, M. Human resource allocation in an emergency department: A metamodel-based simulation optimization. Kybernetes 2019, 49, 779–796. [Google Scholar] [CrossRef]
- Duguay, C.; Chetouane, F. Modeling and Improving Emergency Department Systems using Discrete Event Simulation. Simulation 2007, 83, 311–320. [Google Scholar] [CrossRef]
- Ibrahim, I.M.; Liong, C.; Bakar, S.A.; Ahmad, N.; Najmuddin, A.F. Estimating optimal resource capacities in emergency department. Indian J. Public Health Res. Dev. 2018, 9, 1558–1565. [Google Scholar] [CrossRef]
- Joshi, V.; Lim, C.; Teng, S.G. Simulation Study: Improvement for Non-Urgent Patient Processes in the Emergency Department. EMJ Eng. Manag. J. 2016, 28, 145–157. [Google Scholar] [CrossRef]
- Kaushal, A.; Zhao, Y.; Peng, Q.; Strome, T.; Weldon, E.; Zhang, M.; Chochinov, A. Evaluation of fast track strategies using agent-based simulation modeling to reduce waiting time in a hospital emergency department. Socio-Econ. Plan. Sci. 2015, 50, 18–31. [Google Scholar] [CrossRef]
- Lamprecht, J.; Kolisch, R.; Pförringer, D. The impact of medical documentation assistants on process performance measures in a surgical emergency department. Eur. J. Med. Res. 2019, 24, 1–8. [Google Scholar] [CrossRef]
- Taboada, M.; Cabrera, E.; Epelde, F.; Iglesias, M.L.; Luque, E. Agent-based emergency decision-making aid for hospital emergency departments. Emergencias 2012, 24, 189–195. [Google Scholar]
- Wang, J.; Li, J.; Tussey, K.; Ross, K. Reducing length of stay in emergency department: A simulation study at a community hospital. IEEE Trans. Syst. Man Cybern. Part. A Syst. Hum. 2012, 42, 1314–1322. [Google Scholar] [CrossRef]
- Yang, K.K.; Lam, S.S.W.; Low, J.M.W.; Ong, M.E.H. Managing emergency department crowding through improved triaging and resource allocation. Oper. Res. Health Care 2016, 10, 13–22. [Google Scholar] [CrossRef]
- Hogan, B.; Rasche, C.; Von Reinersdorff, A.B. The First View Concept: Introduction of industrial flow techniques into emergency medicine organization. Eur. J. Emerg. Med. 2012, 19, 136–139. [Google Scholar] [CrossRef]
- Ieraci, S.; Digiusto, E.; Sonntag, P.; Dann, L.; Fox, D. Streaming by case complexity: Evaluation of a model for emergency department Fast Track. EMA Emerg. Med. Australas 2008, 20, 241–249. [Google Scholar] [CrossRef]
- Improta, G.; Romano, M.; Di Cicco, M.V.; Ferraro, A.; Borrelli, A.; Verdoliva, C.; Triassi, M.; Cesarelli, M. Lean thinking to improve emergency department throughput at AORN Cardarelli hospital. BMC Health Serv. Res. 2018, 18, 914. [Google Scholar] [CrossRef]
- Piggott, Z.; Weldon, E.; Strome, T.; Chochinov, A. Application of lean principles to improve early cardiac care in the emergency department. Can. J. Emerg. Med. 2011, 13, 325–332. [Google Scholar] [CrossRef]
- Rees, G.H. Organisational readiness and Lean Thinking implementation: Findings from three emergency department case studies in New Zealand. Health Serv. Manag. Res. 2014, 27, 1–9. [Google Scholar] [CrossRef]
- Rutman, L.E.; Migita, R.; Woodward, G.A.; Klein, E.J. Creating a leaner pediatric emergency department: How rapid design and testing of a front-end model led to decreased wait time. Pediatr. Emerg. Care 2015, 31, 395–398. [Google Scholar] [CrossRef]
- Vashi, A.A.; Sheikhi, F.H.; Nashton, L.A.; Ellman, J.; Rajagopal, P.; Asch, S.M. Applying Lean Principles to Reduce Wait Times in a VA Emergency Department. Mil. Med. 2019, 184, E169–E178. [Google Scholar] [CrossRef]
- White, B.A.; Yun, B.J.; Lev, M.H.; Raja, A.S. Applying systems engineering reduces radiology transport cycle times in the emergency department. West. J. Emerg. Med. 2017, 18, 410–418. [Google Scholar] [CrossRef]
- Bordoloi, S.K.; Beach, K. Improving operational efficiency in an Inner-city Emergency Department. Health Serv. Manag. Res. 2007, 20, 105–112. [Google Scholar] [CrossRef]
- Meng, F.; Teow, K.L.; Ooi, C.K.; Heng, B.H.; Tay, S.Y. Minimization of the coefficient of variation for patient waiting system governed by a generic maximum waiting policy. J. Ind. Manag. Optim. 2017, 13, 1759–1770. [Google Scholar] [CrossRef]
- Leo, G.; Lodi, A.; Tubertini, P.; Di Martino, M. Emergency Department Management in Lazio, Italy. Omega 2016, 58, 128–138. [Google Scholar] [CrossRef]
- Nezamoddini, N.; Khasawneh, M.T. Modeling and optimization of resources in multi-emergency department settings with patient transfer. Oper. Res. Health Care 2016, 10, 23–34. [Google Scholar] [CrossRef]
- Rothwell, S.; McIltrot, K.; Khouri-Stevens, Z. Addressing Emergency Department Issues Using Advanced Practice in Saudi Arabia. J. Nurse Pract. 2018, 14, e41–e44. [Google Scholar] [CrossRef]
- Spaite, D.W.; Bartholomeaux, F.; Guisto, J.; Lindberg, E.; Hull, B.; Eyherabide, A.; Lanyon, S.; Criss, E.A.; Valenzuela, T.D.; Conroy, C. Rapid process redesign in a university-based emergency department: Decreasing waiting time intervals and improving patient satisfaction. Ann. Emerg. Med. 2002, 39, 168–177. [Google Scholar] [CrossRef]
- Doupe, M.B.; Chateau, D.; Chochinov, A.; Weber, E.; Enns, J.E.; Derksen, S.; Sarkar, J.; Schull, M.; Lobato de Faria, R.; Katz, A.; et al. Comparing the Effect of Throughput and Output Factors on Emergency Department Crowding: A Retrospective Observational Cohort Study. Ann. Emerg. Med. 2018, 72, 410–419. [Google Scholar] [CrossRef]
- Eiset, A.H.; Kirkegaard, H.; Erlandsen, M. Crowding in the emergency department in the absence of boarding—A transition regression model to predict departures and waiting time. BMC Med. Res. Methodol. 2019, 19, 68. [Google Scholar] [CrossRef]
- Cookson, D.; Read, C.; Mukherjee, P.; Cooke, M. Improving the quality of Emergency Department care by removing waste using Lean Value Stream mapping. Int. J. Clin. Lead. 2011, 17, 25–30. [Google Scholar]
- Fulbrook, P.; Jessup, M.; Kinnear, F. Implementation and evaluation of a ‘Navigator’ role to improve emergency department throughput. Australas Emerg. Nurs. J. 2017, 20, 114–121. [Google Scholar] [CrossRef]
- Popovich, M.A.; Boyd, C.; Dachenhaus, T.; Kusler, D. Improving Stable Patient Flow through the Emergency Department by Utilizing Evidence-Based Practice: One Hospital’s Journey. J. Emerg. Nurs. 2012, 38, 474–478. [Google Scholar] [CrossRef]
- Aminuddin, W.M.W.M.; Ismail, W.R.; Harunarashid, H. Resources improvement in emergency department using simulation and data envelopment analysis. Sains Malays. 2018, 47, 2231–2240. [Google Scholar]
- Andersen, A.R.; Nielsen, B.F.; Reinhardt, L.B.; Stidsen, T.R. Staff optimization for time-dependent acute patient flow. Eur. J. Oper. Res. 2019, 272, 94–105. [Google Scholar] [CrossRef]
- Zhao, Y.; Peng, Q.; Strome, T.; Weldon, E.; Zhang, M.; Chochinov, A. Bottleneck detection for improvement of emergency department efficiency. Bus. Process. Manag. J. 2015, 21, 564–585. [Google Scholar] [CrossRef]
- Azadeh, A.; Hosseinabadi Farahani, M.; Torabzadeh, S.; Baghersad, M. Scheduling prioritized patients in emergency department laboratories. Comput. Methods Programs Biomed. 2014, 117, 61–70. [Google Scholar] [CrossRef]
- Bal, A.; Ceylan, C.; Taçoğlu, C. Using value stream mapping and discrete event simulation to improve efficiency of emergency departments. Int. J. Healthc. Manag. 2017, 10, 196–206. [Google Scholar] [CrossRef]
- Benson, R.; Harp, N. Using systems thinking to extend continuous quality improvement. Qual. Lett. Healthc. Lead. 1994, 6, 17–24. [Google Scholar]
- Daldoul, D.; Nouaouri, I.; Bouchriha, H.; Allaoui, H. A stochastic model to minimize patient waiting time in an emergency department. Oper. Res. Health Care 2018, 18, 16–25. [Google Scholar] [CrossRef]
- Diefenbach, M.; Kozan, E. Effects of bed configurations at a hospital emergency department. J. Simul. 2011, 5, 44–57. [Google Scholar] [CrossRef]
- EL-Rifai, O.; Garaix, T.; Augusto, V.; Xie, X. A stochastic optimization model for shift scheduling in emergency departments. Health Care Manag. Sci. 2015, 18, 289–302. [Google Scholar] [CrossRef]
- Gartner, D.; Padman, R. Machine learning for healthcare behavioural OR: Addressing waiting time perceptions in emergency care. J. Oper. Res. Soc. 2019. [Google Scholar] [CrossRef]
- González, J.; Ferrer, J.; Cataldo, A.; Rojas, L. A proactive transfer policy for critical patient flow management. Health Care Manag. Sci. 2019, 22, 287–303. [Google Scholar] [CrossRef]
- Izady, N.; Worthington, D. Setting staffing requirements for time dependent queueing networks: The case of accident and emergency departments. Eur. J. Oper. Res. 2012, 219, 531–540. [Google Scholar] [CrossRef]
- Kuo, Y.H. Integrating simulation with simulated annealing for scheduling physicians in an understaffed emergency department. Hong Kong Inst. Eng. Trans. 2014, 21, 253–261. [Google Scholar] [CrossRef]
- Lau, H.; Dadich, A.; Nakandala, D.; Evans, H.; Zhao, L. Development of a cost-optimization model to reduce bottlenecks: A health service case study. Expert Syst. 2018, 35, e12294. [Google Scholar] [CrossRef]
- Martínez, P.; Martínez, J.; Nuño, P.; Cavazos, J. Improvement of patient care time in an emergency department through the application of lean manufacturing. Inf. Tecnol. 2015, 26, 187–198. [Google Scholar] [CrossRef]
- Mazzocato, P.; Holden, R.J.; Brommels, M.; Aronsson, H.; Bäckman, U.; Elg, M.; Thor, J. How does lean work in emergency care? A case study of a lean-inspired intervention at the Astrid Lindgren Children’s hospital, Stockholm, Sweden. BMC Health Serv. Res. 2012, 12, 28. [Google Scholar] [CrossRef]
- Ben Othman, S.; Zgaya, H.; Hammadi, S.; Quilliot, A.; Martinot, A.; Renard, J. Agents endowed with uncertainty management behaviors to solve a multiskill healthcare task scheduling. J. Biomed. Inform. 2016, 64, 25–43. [Google Scholar] [CrossRef]
- Ben Othman, S.; Hammadi, S. A multi-criteria optimization approach to health care tasks scheduling under resources constraints. Int. J. Comput. Intell. Syst. 2017, 10, 419–439. [Google Scholar] [CrossRef][Green Version]
- Perry, A. Code Critical: Improving Care Delivery for Critically Ill Patients in the Emergency Department. J. Emerg. Nurs. 2019, 46, 199–204. [Google Scholar] [CrossRef]
- Stephens, A.S.; Broome, R.A. Impact of emergency department occupancy on waiting times, rates of admission and representation, and length of stay when hospitalised: A data linkage study. EMA Emerg. Med. Australas 2019, 31, 555–561. [Google Scholar] [CrossRef]
- Umble, M.; Umble, E.J. Utilizing buffer management to improve performance in a healthcare environment. Eur. J. Oper. Res. 2006, 174, 1060–1075. [Google Scholar] [CrossRef]
- Xu, K.; Chan, C.W. Using future information to reduce waiting times in the emergency department via diversion. Manuf. Serv. Oper. Manag. 2016, 18, 314–331. [Google Scholar] [CrossRef]
- Zeinali, F.; Mahootchi, M.; Sepehri, M.M. Resource planning in the emergency departments: A simulation-based metamodeling approach. Simul. Model. Pract. Theory 2015, 53, 123–138. [Google Scholar] [CrossRef]
- Ahalt, V.; Argon, N.T.; Ziya, S.; Strickler, J.; Mehrotra, A. Comparison of emergency department crowding scores: A discrete-event simulation approach. Health Care Manag. Sci. 2018, 21, 144–155. [Google Scholar] [CrossRef]
- Fitzgerald, J.A.; Eljiz, K.; Dadich, A.; Sloan, T.; Hayes, K.J. Health services innovation: Evaluating process changes to improve patient flow. Int. J. Healthc. Technol. Manag. 2011, 12, 280–292. [Google Scholar] [CrossRef]
- Peck, J.S.; Benneyan, J.C.; Nightingale, D.J.; Gaehde, S.A. Characterizing the value of predictive analytics in facilitating hospital patient flow. IIE Trans. Healthc. Syst. Eng. 2014, 4, 135–143. [Google Scholar] [CrossRef]
- Restrepo-Zea, J.H.; Jaén-Posada, J.S.; Piedrahita, J.J.E.; Flórez, P.A.Z. Emergency department overcrowding: A four-hospital analysis in Medellín and a strategy simulation. Rev. Gerenc. Polit. Salud 2018, 17, 130–144. [Google Scholar]
- Aaronson, E.; Mort, E.; Soghoian, S. Mapping the process of emergency care at a teaching hospital in Ghana. Healthcare 2017, 5, 214–220. [Google Scholar] [CrossRef]
- Al Owad, A.; Samaranayake, P.; Karim, A.; Ahsan, K.B. An integrated lean methodology for improving patient flow in an emergency department–case study of a Saudi Arabian hospital. Prod. Plan. Control 2018, 29, 1058–1081. [Google Scholar] [CrossRef]
- Vose, C.; Reichard, C.; Pool, S.; Snyder, M.; Burmeister, D. Using LEAN to improve a segment of emergency department flow. J. Nurs. Admin. 2014, 44, 558–563. [Google Scholar] [CrossRef]
- Hu, B.; Wang, Z.; Wang, S.; He, L.; Wu, J.; Wang, F.; Zhu, X.; Gu, S. Key factors affecting the correlation between improving work efficiency and emergency department overcrowding in the tertiary level A hospitals. Chin. J. Emerg. Med. 2018, 27, 943–948. [Google Scholar]
- Wang, X. Emergency department staffing: A separated continuous linear programming approach. Math. Probl. Eng. 2013, 2013, 680152. [Google Scholar] [CrossRef]
- Aldarrab, A. Application of Lean Six Sigma for patients presenting with ST-elevation myocardial infarction: The Hamilton Health Sciences experience. Healthc. Q. 2006, 9, 56–61. [Google Scholar] [CrossRef]
- Beck, M.J.; Okerblom, D.; Kumar, A.; Bandyopadhyay, S.; Scalzi, L.V. Lean intervention improves patient discharge times, improves emergency department throughput and reduces congestion. Hosp. Pract. 2016, 44, 252–259. [Google Scholar] [CrossRef]
- El-Rifai, O.; Garaix, T.; Xie, X. Proactive on-call scheduling during a seasonal epidemic. Oper. Res. Health Care 2016, 8, 53–61. [Google Scholar] [CrossRef][Green Version]
- Garrett, J.S.; Berry, C.; Wong, H.; Qin, H.; Kline, J.A. The effect of vertical split-flow patient management on emergency department throughput and efficiency. Am. J. Emerg. Med. 2018, 36, 1581–1584. [Google Scholar] [CrossRef]
- Hussein, N.A.; Abdelmaguid, T.F.; Tawfik, B.S.; Ahmed, N.G.S. Mitigating overcrowding in emergency departments using Six Sigma and simulation: A case study in Egypt. Oper. Res. Health Care 2017, 15, 1–12. [Google Scholar] [CrossRef]
- Landa, P.; Sonnessa, M.; Tànfani, E.; Testi, A. Multiobjective bed management considering emergency and elective patient flows. Int. Trans. Oper. Res. 2018, 25, 91–110. [Google Scholar] [CrossRef]
- Peltan, I.D.; Bledsoe, J.R.; Oniki, T.A.; Sorensen, J.; Jephson, A.R.; Allen, T.L.; Samore, M.H.; Hough, C.L.; Brown, S.M. Emergency Department Crowding Is Associated With Delayed Antibiotics for Sepsis. Ann. Emerg. Med. 2019, 73, 345–355. [Google Scholar] [CrossRef]
- Khanna, S.; Sier, D.; Boyle, J.; Zeitz, K. Discharge timeliness and its impact on hospital crowding and emergency department flow performance. EMA Emerg. Med. Australas 2016, 28, 164–170. [Google Scholar] [CrossRef]
- Vile, J.L.; Allkins, E.; Frankish, J.; Garland, S.; Mizen, P.; Williams, J.E. Modelling patient flow in an emergency department to better understand demand management strategies. J. Simul. 2017, 11, 115–127. [Google Scholar] [CrossRef]
- Matt, D.T.; Arcidiacono, G.; Rauch, E. Applying lean to healthcare delivery processes—A case-based. Int. J. Adv. Sci. Eng. Inf. Technol. 2018, 8, 123–133. [Google Scholar] [CrossRef]
- Goldmann, D.A.; Saul, C.A.; Parsons, S.; Mansoor, C.; Abbott, A.; Damian, F.; Young, G.J.; Homer, C.; Caputo, G.L. Hospital-based continuous quality improvement: A realistic appraisal. Clin. Perform. Qual. Health Care 1993, 1, 69–80. [Google Scholar]
- Henderson, D.; Dempsey, C.; Larson, K.; Appleby, D. The impact of IMPACT on St. John’s Regional Health Center. Mo. Med. 2003, 100, 590–592. [Google Scholar]
- Jackson, G.; Andrew, J. Using a multidisciplinary CQI approach to reduce ER-to-floor admission time. J. Healthc. Qual. 1996, 18, 18–21. [Google Scholar] [CrossRef]
- Markel, K.N.; Marion, S.A. CQI: Improving the time to thrombolytic therapy for patients with acute myocardial infarction in the emergency department. J. Emerg. Med. 1996, 14, 685–689. [Google Scholar] [CrossRef]
- Courtad, B.; Baker, K.; Magazine, M.; Polak, G. Minimizing flowtime for paired tasks. Eur. J. Oper. Res. 2017, 259, 818–828. [Google Scholar] [CrossRef]
- Iyer, S.; Reeves, S.; Varadarajan, K.; Alessandrini, E. The acute care model: A new framework for quality care in emergency medicine. Clin. Pediatr. Emerg. Med. 2011, 12, 91–101. [Google Scholar] [CrossRef]
- Mohan, S.; Nandi, D.; Stephens, P.; M’Farrej, M.; Vogel, R.L.; Bonafide, C.P. Implementation of a clinical pathway for chest pain in a pediatric emergency department. Pediatr. Emerg. Care 2018, 34, 778–782. [Google Scholar] [CrossRef]
- Ollivere, B.; Rollins, K.; Brankin, R.; Wood, M.; Brammar, T.J.; Wimhurst, J. Optimising fast track care for proximal femoral fracture patients using modified early warning score. Ann. R. Coll. Surg. Engl. 2012, 94, e267–e271. [Google Scholar] [CrossRef]
- Azadeh, A.; Rouhollah, F.; Davoudpour, F.; Mohammadfam, I. Fuzzy modelling and simulation of an emergency department for improvement of nursing schedules with noisy and uncertain inputs. Int. J. Serv. Oper. Manag. 2013, 15, 58–77. [Google Scholar] [CrossRef]
- Brenner, S.; Zeng, Z.; Liu, Y.; Wang, J.; Li, J.; Howard, P.K. Modeling and analysis of the emergency department at university of Kentucky Chandler Hospital using simulations. J. Emerg. Nurs. 2010, 36, 303–310. [Google Scholar] [CrossRef]
- Guo, H.; Gao, S.; Tsui, K.; Niu, T. Simulation Optimization for Medical Staff Configuration at Emergency Department in Hong Kong. IEEE Trans. Autom. Sci. Eng. 2017, 14, 1655–1665. [Google Scholar] [CrossRef]
- Hajjarsaraei, H.; Shirazi, B.; Rezaeian, J. Scenario-based analysis of fast track strategy optimization on emergency department using integrated safety simulation. Saf. Sci. 2018, 107, 9–21. [Google Scholar] [CrossRef]
- Huang, Y.; Klassen, K.J. Using six sigma, lean, and simulation to improve the phlebotomy process. Qual. Manag. J. 2016, 23, 6–21. [Google Scholar] [CrossRef]
- Keeling, K.B.; Brown, E.; Kros, J.F. Using process capability analysis and simulation to improve patient flow. Appl. Manag. Sci. 2013, 16, 219–229. [Google Scholar]
- Ryan, A.; Hunter, K.; Cunningham, K.; Williams, J.; O’Shea, H.; Rooney, P.; Hickey, F. STEPS: Lean thinking, theory of constraints and identifying bottlenecks in an emergency department. Ir. Med. J. 2013, 106, 105–107. [Google Scholar]
- Shirazi, B. Fast track system optimization of emergency departments: Insights from a computer simulation study. Int. J. Model. Simul. Sci. Comput. 2016, 7, 1650015. [Google Scholar] [CrossRef]
- Stanton, P.; Gough, R.; Ballardie, R.; Bartram, T.; Bamber, G.J.; Sohal, A. Implementing lean management/Six Sigma in hospitals: Beyond empowerment or work intensification? Int. J. Hum. Resour. Manag. 2014, 25, 2926–2940. [Google Scholar] [CrossRef]
- Weimann, E. Lean management and continuous improvement process in hospitals. Pneumologe 2018, 15, 202–208. [Google Scholar] [CrossRef]
- Hitti, E.; Hadid, D.; Tamim, H.; Al Hariri, M.; El Sayed, M. Left without being seen in a hybrid point of service collection model emergency department. Am. J. Emerg. Med. 2019. [Google Scholar] [CrossRef]
- Jiang, S.; Chin, K.; Tsui, K.L. A universal deep learning approach for modeling the flow of patients under different severities. Comput. Methods Programs Biomed. 2018, 154, 191–203. [Google Scholar] [CrossRef]
- Welch, S.J.; Allen, T.L. Data-driven quality improvement in the Emergency Department at a level one trauma and tertiary care hospital. J. Emerg. Med. 2006, 30, 269–276. [Google Scholar] [CrossRef]
- Schwab, R.A.; DelSorbo, S.M.; Cunningham, M.R.; Craven, K.; Watson, W.A. Using statistical process control to demonstrate the effect of operational interventions on quality indicators in the emergency department. J. Healthc. Qual. 1999, 21, 38–41. [Google Scholar] [CrossRef]
- Nuñez-Perez, N.; Ortíz-Barrios, M.; McClean, S.; Salas-Navarro, K.; Jimenez-Delgado, G.; Castillo-Zea, A. Discrete-event simulation to reduce waiting time in accident and emergency departments: A case study in a district general clinic. In Lecture Notes in Computer Science; 10586 LNCS:352-363; Springer: Cham, Switzerland, 2017. [Google Scholar]
- Troncoso-Palacio, A.; Neira-Rodado, D.; Ortíz-Barrios, M.; Jiménez-Delgado, G.; Hernández-Palma, H. Using discrete-event-simulation for improving operational efficiency in laboratories: A case study in pharmaceutical industry. In Lecture Notes in Computer Science; 10942 LNCS:440-451; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Ortiz-Barrios, M.; Pancardo, P.; Jiménez-Delgado, G.; De Ávila-Villalobos, J. Applying Multi-phase DES Approach for Modelling the Patient Journey Through Accident and Emergency Departments. In Lecture Notes in Computer Science; 11582 LNCS:87-100; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Ortiz, M.A.; McClean, S.; Nugent, C.D.; Castillo, A. Reducing appointment lead-time in an outpatient department of gynecology and obstetrics through discrete-event simulation: A case study. In Lecture Notes in Computer Science; 10069 LNCS:274-285; Springer: Cham, Switzerland, 2016. [Google Scholar]
- World Health Organization (WHO); Organisation for Economic Co-operation and Development (OECD); World Bank Group. Delivering Quality Health Services: A Global Imperative for Universal Health Coverage; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization, Organisation for Economic Co-operation and Development, and The World Bank: Geneva, Switzerland, 2018. [Google Scholar]


| Period | N (Papers/Period) | Extended LOS | Prolonged Waiting Time | Excessive Patient Flow Time in ED | Overcrowding | High LWBS |
|---|---|---|---|---|---|---|
| 1993–2004 | 11 (5.41%) | 4 | 2 | 8 | 0 | 1 |
| 2005–2006 | 5 (2.46%) | 2 | 2 | 0 | 1 | 2 |
| 2007–2008 | 7 (3.44%) | 3 | 3 | 3 | 0 | 1 |
| 2009–2010 | 9 (4.43%) | 8 | 2 | 2 | 1 | 2 |
| 2011–2012 | 26 (12.80%) | 14 | 19 | 8 | 7 | 3 |
| 2013–2014 | 20 (9.85%) | 10 | 6 | 10 | 9 | 1 |
| 2015–2016 | 34 (16.74%) | 17 | 21 | 12 | 10 | 5 |
| 2017–2018 | 64 (31.52%) | 34 | 22 | 19 | 18 | 5 |
| 2019 | 27 (13.30%) | 16 | 18 | 9 | 9 | 5 |
| N (papers/problem-period) | 108 | 95 | 71 | 55 | 25 | |
| Participation (%) | 53.20 | 46.79 | 34.97 | 27.09 | 12.31 | |
| Authors | Technique Type |
|---|---|
| Single | |
| Ajdari et al. [27]; Best et al. [28]; Bokhorst and van der Vaart [29]; Coughlan, Eatock, and Patel [30]; Gul and Guneri [31]; Hung and Kissoon [32]; Ibrahim et al. [33]; Keyloun, Lofgren, and Hebert [34]; Khare et al. [35]; Konrad et al. [36]; La and Jewkes [37]; Medeiros et al. [38]; Oh et al. [39]; Paul and Lin [40]; Rasheed et al. [41]; Rosmulder et al. [42]; Saoud, Boubetra, and Attia [43]; Steward, Glass, and Ferrand [44]; Thomas Schneider et al. [45]; Wang et al. [46]; Zeng et al. [47] | Simulation or Discrete-event simulation (DES) |
| Allaudeen et al. [48]; Arbune et al. [49]; Carter et al. [50]; Dickson et al. [51,52,53]; Elamir [54]; Hitti et al. [55]; Kane et al. [56]; Migita et al. [57]; Murrell, Offerman, and Kauffman [58]; Ng et al. [59]; Peng, Rasid, and Salim [60]; Polesello et al. [61]; Rotteau et al. [62]; Sánchez et al. [63]; Sayed et al. [64]; Van der linden et al. [65]; Vermeulen et al. [66]; White et al. [67] | Lean manufacturing |
| Cheng et al. [68]; Forero et al. [69]; Kaushik et al. [70]; Maniaci et al. [71]; Singh et al. [72]; Street et al. [73]; Van der Veen et al. [74]; Yau et al. [75]; | Regression |
| Brent et al. [76]; Fernandes and Christenson [77]; Fernandes, Christenson, and Price [78]; Higgins III and Becker [79]; Lovett et al. [80]; Preyde, Crawford, and Mullins [81]; Rehmani and Amatullah [82] | Continuous quality improvement |
| Ajmi et al. [83]; | Agent-based dynamic optimization |
| Haydar, Strout, and Baumann [84]; Prybutok [85] | PDSA (Plan, Do, Study, Act) cycle |
| Oueida et al. [86]; Derni, Boufera, and Khelfi [87] | Petri nets |
| Bellew et al. [88]; Than et al. [89] | Critical pathways |
| Brouns et al. [90] | Cohort study |
| Chan et al. [91] | Rapid Entry and Accelerated Care at Triage (REACT) |
| Christensen et al. [92] | Pivot nursing |
| Christianson et al. [93] | Six sigma |
| DeFlitch et al. [94] | Process redesign |
| Liu et al. [95] | Agent-based model |
| Oueida et al. [96] | Resource Preservation Net (RPN) |
| Sloan et al. [97] | Evidence-base care pathways |
| Stone-Griffith et al. [98] | ED dashboard and reporting application |
| Hybrid | |
| Ashour and Kremer [20] | Dynamic grouping and prioritization (DGP), Discrete-event simulation |
| Bish, McCormick, and Otegbeye [99] | Simulation, Queuing analyses |
| Blick [100] | Lean Six Sigma |
| Chadha, Singh, and Kalra [101] | Lean manufacturing, Queuing theory |
| Chen and Wang [102] | Non-dominated sorting particle swarm optimization (NSPSO), Multi-objective computing budget allocation (MOCBA), Discrete-event simulation |
| Easter et al. [25] | Discrete-event simulation, Analysis of Variance (ANOVA), Linear regression, Non-linear regression |
| Elalouf and Wachtel [103] | Approximation algorithm, Simulation |
| Feng, Wu, and Chen [104] | Non-dominated sorting genetic algorithm II (NSGA II), Multiple computing budget allocation (MOCBA), Discrete-event simulation |
| Ferrand et al. [105] | Simulation, Dynamic priority queue (DPQ) |
| Fuentes et al. [26] | Logistic regression, Linear regression, Paired t test, Wilcoxon signed rank |
| Furterer [106] | Lean Six Sigma |
| Ghanes et al. [107] | Optimization, Discrete-event simulation |
| Goienetxea Uriarte et al. [108] | Discrete-event simulation, Simulation-based multi-objective optimization, Data mining |
| He, Sim, and Zhang [109] | Mixed integer programming, Queuing network, Stochastic Programming |
| Huang et al. [110] | Descriptive statistics, Two-sample t-test, Multivariate linear regression |
| Kaner et al. [111] | Discrete-event simulation, Design of experiments |
| Lee et al. [112] | Machine learning, Simulation, Optimization |
| Lo et al. [113] | Lean principles, Simulation, Continuous process improvement |
| Oueida et al. [114] | Discrete-event simulation, Optimization |
| Rachuba et al. [115] | Process mapping, Discrete-event simulation |
| Romano, Guizzi, and Chiocca [116] | System dynamics simulation, Lean techniques, Causal loop diagram |
| Ross, Johnson, and Kobernick [117] | Critical pathways, Continuous quality improvement |
| Ross et al. [118] | Multivariate logistic regression, Ordinary least squares regression |
| Shin et al. [119] | Discrete-event simulation, Linear integer programming |
| Sinreich and Jabali [120] | Linear optimization model (S-model), Heuristic iterative simulation based algorithm |
| Sinreich, Jabali, and Dellaert [121] | Discrete-event simulation, Optimization |
| Sir et al. [122] | Classification and regression trees, Mixed integer programming |
| Techar et al. [123] | Multivariate logistic regression, Negative binomial models |
| Visintin, Caprara, and Puggelli [124] | Simulation, Experimental design |
| Yousefi and Ferreira [125] | Agent-based simulation, Group Decision Making |
| Yousefi et al. [126] | Agent-based simulation, Chaotic genetic algorithm, Adaptive boosting (AdaBoost) |
| Yousefi et al. [127] | Agent based modeling, Ordinary least squares regression |
| Zeltyn et al. [128] | Simulation, Queuing theory |
| Authors | Technique Type |
|---|---|
| Single | |
| Coughlan, Eatock, and Patel [30]; Duguay and Chetouane [135]; Hung and Kissoon [32]; Ibrahim et al. [33,136]; Joshi, Lim, and Teng [137]; Kaushal et al. [138]; Konrad et al. [36]; Lamprecht, Kolisch, and Pförringer [139]; Medeiros et al. [38]; Paul and Lin [40]; Rasheed et al. [41]; Saoud, Boubetra, and Attia [43]; Taboada et al. [140]; Wang et al. [141]; Yang et al. [142]; Zeng et al. [47] | Simulation or Discrete-event simulation |
| Carter et al. [50]; Elamir [54]; Hogan, Rasche, and Von Reinersdorff [143]; Ieraci et al. [144]; Improta et al. [145]; Kane et al. [56]; Murrell, Offerman, and Kauffman [58]; Ng et al. [59]; Piggott et al. [146]; Rees [147]; Rutman et al. [148]; Sánchez et al. [63]; Sayed et al. [64]; Vashi et al. [149]; Vermeulen et al. [66]; White et al. [150]; | Lean manufacturing |
| Ajmi et al. [83]; Bordoloi and Beach [151]; Meng et al. [152]; | Optimization |
| Leo et al. [153]; Nezamoddini and Khasawneh [154] | Integer programming |
| Queuing theory | |
| Preyde, Crawford, and Mullins [81]; Rothwell, McIltrot, and Khouri-Stevens [155] | Continuous quality improvement |
| DeFlitch et al. [94]; Spaite et al. [156] | Process redesign |
| Derni, Boufera, and Khelfi [87]; Oueida et al. [86] | Petri nets |
| Doupe et al. [157]; Eiset, Kirkegaard, and Erlandsen [158] | Regression |
| Chan et al. [91] | Rapid Entry and Accelerated Care at Triage (REACT) |
| Christensen et al. [92] | Pivot nursing |
| Cookson et al. [159] | Value Stream Mapping (VSM) |
| Fulbrook, Jessup, and Kinnear [160] | Nurse navigator |
| Oueida et al. [96] | Resource Preservation Net (RPN) |
| Popovich et al. [161] | Iowa Model of Evidence-Based Practice |
| Stone-Griffith et al. [98] | ED dashboard and reporting application |
| Hybrid | |
| Abo-Hamad and Arisha [131] | Simulation, Balance Scorecard (BSC), Preference ratios in multi-attribute evaluation (PRIME) |
| Acuna, Zayas-Castro, and Charkhgard [132] | Mixed integer programming, game theory, single and bi-objective optimization models |
| Ala and Chen [133] | Integer programming, Tabu search, L-shaped algorithm, Discrete-event simulation |
| Aminuddin, Ismail, and Harunarashid [162] | Simulation, Data Envelopment Analysis (DEA) |
| Andersen et al. [163] | Integer linear programming, Markov models, Discrete-event simulation |
| Aroua and Abdulnour [130]; Zhao et al. [164] | Simulation, Design of experiments (DOE) |
| Ashour and Kremer [20] | Dynamic grouping and prioritization (DGP), Discrete-event simulation |
| Azadeh et al. [165] | Mixed integer linear programming, Genetic algorithm (GA) |
| Bal, Ceylan, and Taçoğlu [166] | Value Stream Mapping (VSM), Discrete-event simulation |
| Benson and Harp [167] | Discrete-event simulation, System thinking |
| Bish, McCormick, and Otegbeye [99] | Simulation, Queuing analyses |
| Daldoul et al. [168] | Stochastic mixed integer programming, Sample average approximation |
| Diefenbach and Kozan [169] | Simulation, Optimization |
| Easter et al. [25] | Discrete-event simulation, ANOVA, Linear regression, Non-linear regression |
| EL-Rifai et al. [170] | Stochastic mixed-integer programming, Sample average approximation, Discrete-event simulation |
| Ferrand et al. [105] | Simulation, Dynamic priority queue (DPQ) |
| Gartner and Padman [171] | Discrete-event simulation, Machine learning |
| Ghanes et al. [107] | Optimization, Discrete-event simulation |
| Goienetxea Uriarte et al. [108] | Discrete-event simulation, Simulation-based multi-objective optimization, Data mining |
| González et al. [172] | Markov decision process, Approximate dynamic programming |
| He, Sim, and Zhang [109] | Mixed integer programming, Queuing network, Stochastic Programming |
| Izady and Worthington [173] | Discrete-event simulation, Queuing models, Heuristic Staffing Algorithm |
| Kuo [174] | Simulation-optimization |
| Lau et al. [175] | Genetic algorithm, Cost-optimization model |
| Martínez et al. [176] | Discrete-event simulation, Lean manufacturing |
| Mazzocato et al. [177] | Lean manufacturing, ANOVA |
| Othman et al. [178] | Multi-agent system, Multiskill task scheduling |
| Othman and Hammadi [179] | Fuzzy logic, Evolutionary algorithm |
| Oueida et al. [114]; Sinreich, Jabali, and Dellaert [121] | Discrete-event simulation, Optimization |
| Perry [180] | Lean manufacturing, Code critical |
| Romano, Guizzi, and Chiocca [116] | System dynamics simulation, Lean techniques, Causal loop diagram |
| Sir et al. [122] | Classification and regression trees, Mixed integer programming |
| Stephens and Broome [181] | Univariate analysis, Multivariate general linear regression, Binary logistic regression |
| Umble and Umble [182] | Theory of constraints, Buffer management, Synchronous management |
| Visintin, Caprara, and Puggelli [124] | Simulation, Experimental design |
| Xu and Chan [183] | Simulation, Queuing, Predictive models |
| Yousefi and Ferreira [125] | Agent-based simulation, Group Decision Making |
| Yousefi and Yousefi [134] | Agent-based simulation, Adaptive neuro-fuzzy inference system (ANFIS), Feed forward neural network (FNN), Recurrent neural network (RNN) |
| Zeinali, Mahootchi, and Sepehri [184] | Discrete-event simulation, Metamodels, Cross validation |
| Zeltyn et al. [128] | Simulation, Queuing theory |
| Authors | Technique Type |
|---|---|
| Single | |
| Ahalt et al. [185]; Ajmi et al. [83]; Best et al. [28]; Fitzgerald et al. [186]; Hung and Kissoon [32]; Ibrahim et al. [33,136]; Paul and Lin [40]; Peck et al. [187]; Rasheed et al. [41]; Restrepo-Zea et al. [188]; Thomas Schneider et al. [45]; Yang et al. [142] | Simulation or Discrete-event simulation |
| Aaronson, Mort, and Soghoian [189]; Al Owad et al. [190]; Elamir [54]; Hitti et al. [55]; Migita et al. [57]; Murrell, Offerman, and Kauffman [58]; Van der linden et al. [65]; Vose et al. [191]; White et al. [67,150] | Lean manufacturing |
| Nezamoddini and Khasawneh [154] | Integer programming |
| Eiset, Kirkegaard, and Erlandsen [158]; Hu et al. [192]; Singh et al. [72]; Van der Veen et al. [74] | Regression |
| Popovich et al. [161] | Iowa Model of Evidence-Based Practice |
| Wang [193] | Separated continuous linear programming (SCLP) |
| Fulbrook, Jessup, and Kinnear [160] | Nurse navigator |
| DeFlitch et al. [94] | Process redesign |
| Hybrid | |
| Abo-Hamad and Arisha [131] | Simulation, Balance Scorecard (BSC), Preference ratios in multi-attribute evaluation (PRIME) |
| Acuna, Zayas-Castro, and Charkhgard [132] | Mixed integer programming, game theory, single and bi-objective optimization models |
| Aldarrab et al. [194] | Lean Six Sigma |
| Ashour and Kremer [129] | Fuzzy Analytic Hierarchy Process (FAHP), Multi-attribute Utility Theory (MAUT), Discrete-event simulation |
| Ashour and Kremer [20] | Dynamic grouping and prioritization (DGP), Discrete-event simulation |
| Bal, Ceylan, and Taçoğlu [166] | Value Stream Mapping (VSM), Discrete-event simulation |
| Beck et al. [195] | Lean Six Sigma |
| Chen and Wang [102] | Non-dominated sorting particle swarm optimization (NSPSO), Multi-objective computing budget allocation (MOCBA), Discrete-event simulation |
| Elalouf and Wachtel [103] | Approximation algorithm, Simulation |
| El-Rifai, Garaix, and Xie [196] | Integer linear program (ILP), Sample Average Approximation (SAA) |
| Fuentes et al. [26] | Logistic regression, Linear regression, Paired t test, Wilcoxon signed rank |
| Garrett et al. [197] | Regression analysis, Vertical split flow |
| González et al. [172] | Markov decision process, Approximate dynamic programming |
| He, Sim, and Zhang [109] | Mixed integer programming, Queuing network, Stochastic Programming |
| Hussein et al. [198] | Six Sigma, Discrete-event simulation |
| Kaner et al. [111] | Discrete-event simulation, Design of experiments |
| Kuo [174] | Simulation-optimization |
| Landa et al. [199] | Multi-objective optimization, Discrete-event simulation |
| Othman et al. [178] | Multi-agent system, Multiskill task scheduling |
| Peltan et al. [200] | Multivariate regression, Markov multistate models |
| Romano, Guizzi, and Chiocca [116] | System dynamics simulation, Lean techniques, Causal loop diagram |
| Sinreich, Jabali, and Dellaert [121] | Discrete-event simulation, Optimization |
| Visintin, Caprara, and Puggelli [124] | Simulation, Experimental design |
| Authors | Technique Type |
|---|---|
| Single | |
| Coughlan, Eatock, and Patel [30]; Joshi, Lim, and Teng [137]; Khanna et al. [201]; Konrad et al. [36]; Lamprecht, Kolisch, and Pförringer [139]; Rasheed et al. [41]; Thomas Schneider et al. [45]; Vile et al. [202]; Yang et al. [142]; Zeng et al. [47] | Simulation or Discrete-event simulation |
| Al Owad et al. [190]; Dickson et al. [51]; Elamir [54]; Ieraci et al. [144]; Improta et al. [145]; Matt, Arcidiacono, and Rauch [203]; Ng et al. [59]; Rees [147]; Rotteau et al. [62]; Sánchez et al. [63]; Vermeulen et al. [66]; Vose et al. [191]; White et al. [67]; | Lean Manufacturing |
| Fernandes and Christenson [77]; Fernandes, Christenson, and Price [78]; Goldmann et al. [204]; Henderson et al. [205]; Jackson and Andrew [206]; Lovett et al. [80]; Markel and Marion [207]; Preyde, Crawford, and Mullins [81]; | Continuous quality improvement |
| Ajmi et al. [83]; Bordoloi and Beach [151] | Optimization |
| Yau et al. [75] | Regression models |
| Courtad et al. [208] | Mixed integer programming, |
| DeFlitch et al. [94]; Spaite et al. [156] | Process redesign |
| Derni, Boufera, and Khelfi, M [87] | Colored petri net |
| Fulbrook, Jessup, and Kinnear [160] | Nurse navigator |
| Haydar, Strout, and Baumann [84] | PDSA (Plan-do-study-act) cycle |
| Iyer et al. [209] | Acute care model |
| Mohan et al. [210] | Critical pathways |
| Ollivere et al. [211] | Fast track protocols |
| Oueida et al. [96] | Resource Preservation Net (RPN) |
| Popovich et al. [161] | Iowa Model of Evidence-Based Practice |
| Hybrid | |
| Ala and Chen [133] | Integer programming, Tabu search, L-shaped algorithm, Discrete-event simulation |
| Andersen et al. [163] | Linear programming, Discrete-event simulation |
| Azadeh et al. [212] | Fuzzy logic, Simulation |
| Benson and Harp [167] | Discrete-event simulation, System thinking |
| Bish, McCormick, and Otegbeye [99] | Simulation, Queuing analyses |
| Brenner et al. [213] | Simulation, What-if analysis |
| Diefenbach and Kozan [169] | Simulation, Optimization |
| Easter et al. [25] | Discrete-event simulation, ANOVA, Linear regression, Non-linear regression |
| Elalouf and Wachtel [103] | Approximation algorithm, Simulation |
| Ferrand et al. [105] | Simulation, Dynamic priority queue (DPQ) |
| Garrett et al. [197] | Regression analysis, Vertical split flow |
| Gartner and Padman [171] | Discrete-event simulation, Machine learning |
| González et al. [172] | Markov decision process, Approximate dynamic programming |
| Guo et al. [214] | Random boundary generation with feasibility detection (RBG-FD), Discrete-event simulation |
| Hajjarsaraei, Shirazi, and Rezaeian [215] | Discrete-event simulation, System dynamics |
| Huang and Klassen [216] | Six Sigma, Lean manufacturing, Simulation |
| Keeling, Brown, and Kros [217] | Capability analysis, simulation |
| Lau et al. [175] | Genetic algorithm, Cost-optimization model |
| Romano, Guizzi, and Chiocca [116] | System dynamics simulation, Lean techniques, Causal loop diagram |
| Ross et al. [118] | Multivariate logistic regression, Ordinary least squares regression |
| Ryan et al. [218] | Lean manufacturing, Theory of constraints, Logistic regression |
| Shirazi [219] | Simulation-based optimization |
| Stanton et al. [220] | Lean Six Sigma |
| Weimann [221] | Standardized project management, Change management, Continuous quality improvement, Lean manufacturing |
| Yousefi and Ferreira [125] | Agent-based simulation, Group Decision Making |
| Zeinali, Mahootchi, and Sepehri [184] | Discrete-event simulation, Metamodels, Cross validation |
| Authors | Technique Type |
|---|---|
| Single | |
| Carter et al. [50]; Dickson et al. [52]; Kane et al. [56]; Murrell, Offerman, and Kauffman [58]; Ng et al. [59]; Peng, Rasid, and Salim [60]; Sánchez et al. [63]; Sayed et al. [64]; Van der linden et al. [65]; Vashi et al. [149]; Vermeulen et al. [66] | Lean manufacturing (S) |
| Preyde, Crawford, and Mullins [81]; Rehmani and Amatullah [82]; Rothwell, McIltrot, and Khouri-Stevens [155]; Welch and Allen [224] | Continuous quality improvement (S) |
| Chan et al. [91] | Rapid Entry and Accelerated Care at Triage (REACT) |
| Christensen et al. [92] | Pivot nursing |
| Schwab et al. [225] | Statistical Process Control |
| DeFlitch et al. [94] | Process redesign |
| Hybrid | |
| Easter et al. [25] | Discrete-event simulation, ANOVA, Linear regression, Non-linear regression |
| Hitti et al. [222] | Logistic regression, Case-control study |
| Jiang, Chin, and Tsui [223] | Deep neural network (DNN), Genetic algorithm (GA) |
| Lee et al. [112] | Machine learning, Simulation, Optimization |
| Yousefi and Ferreira [125] | Agent-based simulation, Group Decision Making |
| Yousefi et al. [127] | Agent-based simulation, Ordinary least squares regression |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ortíz-Barrios, M.A.; Alfaro-Saíz, J.-J. Methodological Approaches to Support Process Improvement in Emergency Departments: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 2664. https://doi.org/10.3390/ijerph17082664
Ortíz-Barrios MA, Alfaro-Saíz J-J. Methodological Approaches to Support Process Improvement in Emergency Departments: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(8):2664. https://doi.org/10.3390/ijerph17082664
Chicago/Turabian StyleOrtíz-Barrios, Miguel Angel, and Juan-José Alfaro-Saíz. 2020. "Methodological Approaches to Support Process Improvement in Emergency Departments: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 8: 2664. https://doi.org/10.3390/ijerph17082664
APA StyleOrtíz-Barrios, M. A., & Alfaro-Saíz, J.-J. (2020). Methodological Approaches to Support Process Improvement in Emergency Departments: A Systematic Review. International Journal of Environmental Research and Public Health, 17(8), 2664. https://doi.org/10.3390/ijerph17082664





