Proximity to Screening Site, Rurality, and Neighborhood Disadvantage: Treatment Status among Individuals with Sexually Transmitted Infections in Yakima County, Washington
Abstract
:1. Introduction
2. Material and Methods
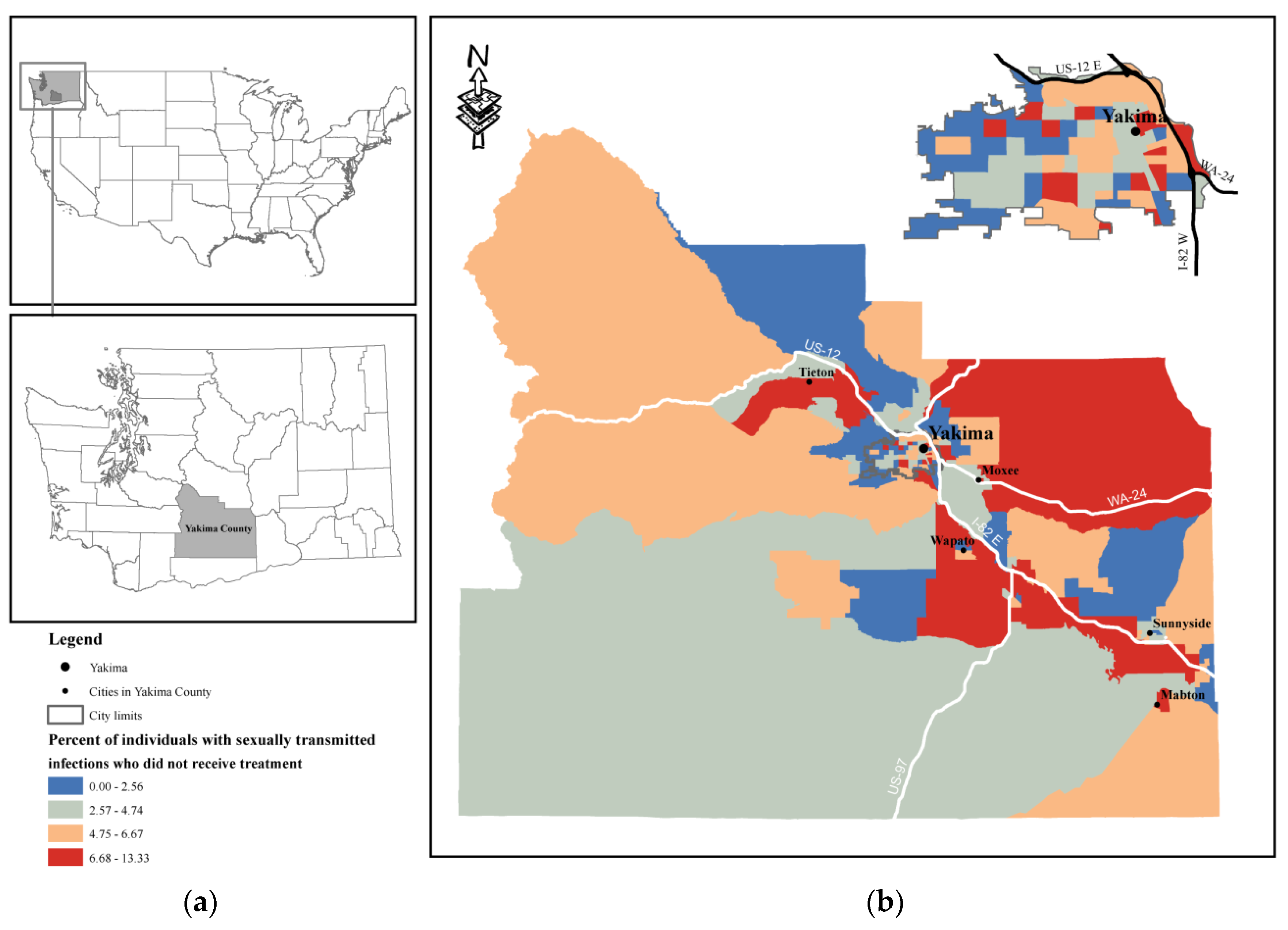
2.1. Study Area
2.2. Study Design and Participants
2.3. Measures
2.3.1. Outcome Variables
2.3.2. Explanatory Variables
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2017; U.S. Department of Health and Human Services: Atlanta, GA, USA, 2018.
- Washington State Department of Health. Sexually Transmitted Infection Cases and Rates by County Washington State Reported Cases Diagnosed in 2018. Available online: https://www.doh.wa.gov/YouandYourFamily/IllnessandDisease/SexuallyTransmittedDisease (accessed on 3 April 2020).
- Gesink, D.C.; Sullivan, A.B.; Norwood, T.A.; Serre, M.L.; Miller, W.C. Does core area theory apply to sexually transmitted diseases in rural environments? Sex. Transm. Dis. 2013, 40, 32–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yarbrough, M.L.; Burnham, C.-A.D. The ABCs of STIs: An update on sexually transmitted infections. Clin. Chem. 2016, 62, 811. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention. Incidence, Prevalence, and Cost of Sexually Transmitted Infections in the United States; Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Available online: https://npin.cdc.gov/publication/incidence-prevalence-and-cost-sexually-transmitted-infections-united-states (accessed on 3 April 2020).
- Centers for Disease Control and Prevention. Chlamydia—CDC Fact Sheet (Detailed). Available online: https://www.cdc.gov/std/chlamydia/stdfact-chlamydia-detailed.htm (accessed on 3 September 2019).
- Golden, R.M.; Kerndt, R.P. Improving clinical operations: Can we and should we save our std clinics? Sex. Transm. Dis. 2010, 37, 264–265. [Google Scholar] [CrossRef] [PubMed]
- Kuehn, B.M. A proactive approach needed to combat rising stisa proactive approach needed to combat rising STIsA proactive approach needed to combat rising STIs. JAMA 2019, 321, 330–332. [Google Scholar] [CrossRef] [PubMed]
- Arcury, T.A.; Gesler, W.M.; Preisser, J.S.; Sherman, J.; Spencer, J.; Perin, J. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv. Res. 2005, 40, 135–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tilson, E.C.; Sanchez, V.; Ford, C.L.; Smurzynski, M.; Leone, P.A.; Fox, K.K.; Irwin, K.; Miller, W.C. Barriers to asymptomatic screening and other STD services for adolescents and young adults: Focus group discussions. BMC Public Health 2004, 4, 21. [Google Scholar] [CrossRef]
- Avuvika, E.; Masese, L.; Wanje, G.; Wanyonyi, J.; Nyaribo, B.; Omoni, G.; Baghazal, A.; McClelland, R.S. Barriers and facilitators of screening for sexually transmitted infections in adolescent girls and young women in mombasa, Kenya: A qualitative study. PLoS ONE 2017, 12, e0169388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monnet, E.; Ramée, C.; Minello, A.; Jooste, V.; Carel, D.; Di Martino, V. Socioeconomic context, distance to primary care and detection of hepatitis C: A French population-based study. Soc. Sci. Med. 2008, 66, 1046–1056. [Google Scholar] [CrossRef]
- Leibowitz, A.A.; Taylor, S.L. Distance to public test sites and HIV testing. Med. Care Rese. Rev. 2007, 64, 568–584. [Google Scholar] [CrossRef]
- Chan, L.; Hart, L.G.; Goodman, D.C. Geographic access to health care for rural medicare beneficiaries. J. Rural Health 2006, 22, 140–146. [Google Scholar] [CrossRef]
- Parekh, N.; Donohue, J.M.; Corbelli, J.; Men, A.; Kelley, D.; Jarlenski, M. Screening for sexually transmitted infections after cervical cancer screening guideline and medicaid policy changes: A population-based analysis. Med. Care. 2018, 56, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Henderson, E.R.; Subramaniam, D.S.; Chen, J. Rural-urban differences in human immunodeficiency virus testing among US adults: Findings from the behavioral risk factor surveillance system. Sex. Transm. Dis. 2018, 45, 808–812. [Google Scholar] [CrossRef] [Green Version]
- Warr, D.; Hillier, L. That’s the problem with living in a small town: Privacy and sexual health issues for young rural people. Aust. J. Rural Health 1997, 5, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Holtgrave, D.R.; Crosby, R.A. Social capital, poverty, and income inequality as predictors of gonorrhoea, syphilis, chlamydia and AIDS case rates in the United States. Sex. Transm. Infect. 2003, 79, 62. [Google Scholar] [CrossRef] [Green Version]
- Pinto, C.N.; Dorn, L.D.; Chinchilli, V.M.; Du, P. Chlamydia and gonorrhea acquisition among adolescents and young adults in pennsylvania: A rural and urban comparison. Sex. Transm. Dis. 2018, 45, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Ford, J.L.; Browning, C.R. Neighborhoods and infectious disease risk: Acquisition of chlamydia during the transition to young adulthood. J. Urban Health Bull. N. Y. Acad. Med. 2014, 91, 136–150. [Google Scholar] [CrossRef] [Green Version]
- United States Census Census Bureau. 2017 American Community Survey 5-Year Estimates. Available online: https://data.census.gov/cedsci/ (accessed on 10 September 2019).
- WWAMI Rural Health Research Center. Rural-Urban Commuting Area Codes (RUCAs). Available online: http://depts.washington.edu/uwruca/ (accessed on 10 September 2019).
- USDA. Rural-Urban Commuting Area codes. Available online: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/ (accessed on 10 September 2019).
- Singh, G.K. Area deprivation and widening inequalities in US mortality, 1969–1998. Am. J. Public Health 2003, 93, 1137–1143. [Google Scholar] [CrossRef]
- Kind, A.J.; Jencks, S.; Brock, J.; Yu, M.; Bartels, C.; Ehlenbach, W.; Greenberg, C.; Smith, M. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: A retrospective cohort study. Ann. Intern. Med. 2014, 161, 765–774. [Google Scholar] [CrossRef] [Green Version]
- Krieger, N.; Waterman, P.D.; Chen, J.T.; Soobader, M.J.; Subramanian, S.V. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: Geocoding and choice of area-based socioeconomic measures—The public health disparities geocoding project (US). Public Health Rep. 2003, 118, 240–260. [Google Scholar] [CrossRef]
- Mabey, D. Epidemiology of STIs: Worldwide. Medicine 2010, 38, 216–219. [Google Scholar] [CrossRef]
- Geisler, W.M.; Chyu, L.; Kusunoki, Y.; Upchurch, D.M.; Hook, E.W. Health insurance coverage, health care-seeking behaviors, and genital chlamydial infection prevalence in sexually active young adults. Sex. Transm. Dis. 2006, 33, 389–396. [Google Scholar] [CrossRef]
- Ford, J.V.; Barnes, R.; Rompalo, A.; Hook, E.W., III. Sexual health training and education in the U.S. Public Health Rep. 2013, 128 (Suppl. 1), 96–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clayton, H.B.; Brener, N.D.; Barrios, L.C.; Jayne, P.E.; Everett Jones, S. Professional development on sexual health education is associated with coverage of sexual health topics. Pedag. Health Promot. 2017, 4, 115–124. [Google Scholar] [CrossRef]
- Sieving, R.E.; Gewirtz O’Brien, J.R.; Saftner, M.A.; Argo, T.A. Sexually transmitted diseases among us adolescents and young adults: Patterns, clinical considerations, and prevention. Nurs. Clin. 2019, 54, 207–225. [Google Scholar] [CrossRef]
- Cartmell, K.B.; Young-Pierce, J.; McGue, S.; Alberg, A.J.; Luque, J.S.; Zubizarreta, M.; Brandt, H.M. Barriers, facilitators, and potential strategies for increasing HPV vaccination: A statewide assessment to inform action. Papillomavirus Res. (Amst. Neth.) 2018, 5, 21–31. [Google Scholar] [CrossRef]
- Charlton, B.M.; Corliss, H.L.; Missmer, S.A.; Frazier, A.L.; Rosario, M.; Kahn, J.A.; Austin, S.B. Reproductive health screening disparities and sexual orientation in a cohort study of U.S. adolescent and young adult females. J. Adolesc. Health 2011, 49, 505–510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yen, W. How Long and How Far Do Adults Travel and Will Adults Travel for Primary Care? Washington State Office Of Financial Management. Available online: https://ofm.wa.gov/pubs-reports/how-long-and-how-far-do-adults-travel-and-will-adults-travel-primary-care (accessed on 3 September 2019).
- Bell, G.; Potterat, J. Partner notification for sexually transmitted infections in the modern world: A practitioner perspective on challenges and opportunities. Sex. Transm. Infect. 2011, 87 (Suppl. 2), ii34–ii36. [Google Scholar] [CrossRef] [Green Version]
| Characteristics | Total (No. (%)) | Treatment Received | Days Until Treatment * | |
|---|---|---|---|---|
| Yes (15,313, 95%) | No (762, 5%) | |||
| Proximity | ||||
| ≤5 Miles | 9676 (60.19) | 9244 (60.37) | 432 (56.59) | 4.19 (7.53) |
| 5 < x < 10 Miles | 3123 (19.43) | 2981 (19.47) | 142 (18.64) | 4.48 (14.88) |
| ≥10 Miles | 3276 (20.38) | 3088 (20.17) | 188 (24.67) | 4.90 (10.26) |
| RUCA | ||||
| Metropolitan | 12,700 (79.00) | 12,138 (79.27) | 562 (73.75) | 4.10 (7.37) |
| Micropolitan, Small town, or Rural | 3375 (21.00) | 3175 (20.73) | 200 (26.25) | 5.51 (16.32) |
| Area deprivation index * | 9.11 (1.44) | 9.11 (1.45) | 9.20 (1.27) | 9.11 (1.44) |
| Age * | 24.87 (8.10) | 24.90 (8.11) | 24.24 (7.84) | 24.87 (8.10) |
| Gender | ||||
| Male | 4435 (27.59) | 4260 (27.82) | 175 (22.97) | 3.43 (13.17) |
| Female | 11,635 (72.38) | 11,049 (72.15) | 586 (76.90) | 4.76 (8.33) |
| Unknown | 5 (0.03) | 4 (0.03) | 1 (0.13) | 3.50 (3.79) |
| Race | ||||
| White | 7435 (46.25) | 7080 (46.24) | 355 (46.59) | 4.31 (11.52) |
| Non-white | 4702 (29.25) | 4497 (29.37) | 205 (26.90) | 4.94 (9.99) |
| Unknown | 3938 (24.50) | 3736 (24.40) | 202 (26.51) | 3.89 (5.65) |
| Ethnicity | ||||
| Non-Hispanic | 4575 (28.46) | 4357 (28.45) | 218 (28.61) | 4.04 (7.17) |
| Hispanic | 8575 (53.34) | 8219 (53.67) | 356 (46.72) | 4.77 (11.84) |
| Unknown | 2925 (18.20) | 2737 (17.87) | 188 (24.67) | 3.8 (6.93) |
| Characteristics | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Proximity | ||||
| ≤5 Miles | Reference | Reference | ||
| 5 < x < 10 Miles | 1.01 (0.82–1.25) | 0.91 | 1.00 (0.80–1.24) | 0.99 |
| ≥10 Miles | 1.27 (1.05–1.53) | 0.01 | 1.27 (1.05–1.53) | 0.02 |
| RUCA | ||||
| Metropolitan | Reference | Reference | ||
| Micropolitan, Small town, or Rural | 1.40 (1.13–1.72) | 0.002 | 1.49 (1.20–1.86) | <0.001 |
| Area deprivation index | 1.06 (0.99–1.13) | 0.07 | 1.08 (1.01–1.16) | 0.02 |
| Age | 0.99 (0.98–0.99) | 0.03 | 0.99 (0.98–0.99) | 0.04 |
| Gender | ||||
| Male | Reference | Reference | ||
| Female | 1.27 (1.07–1.51) | 0.01 | 1.25 (1.05–1.50) | 0.01 |
| Race | ||||
| White | Reference | Reference | ||
| Non-white | 0.88 (0.74–1.06) | 0.18 | 0.85 (0.70–1.02) | 0.08 |
| Unknown | 1.09 (0.91–1.30) | 0.37 | 0.94 (0.77–1.15) | 0.54 |
| Ethnicity | ||||
| Non-Hispanic | Reference | Reference | ||
| Hispanic | 0.84 (0.70–1.00) | 0.06 | 0.77 (0.63–0.93) | 0.01 |
| Unknown | 1.38 (1.13–1.69) | 0.002 | 1.41 (1.12–1.78) | 0.003 |
| Characteristics | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Proximity | ||||
| ≤5 Miles | Reference | Reference | ||
| 5 < x < 10 Miles | 0.99 (0.93–1.04) | 0.68 | 1.00 (0.95–1.06) | 0.89 |
| ≥10 Miles | 1.10 (1.05–1.16) | <0.001 | 1.13 (1.07–1.18) | <0.001 |
| RUCA | ||||
| Metropolitan | Reference | Reference | ||
| Micropolitan, Small town, or Rural | 1.33 (1.23–1.43) | <0.001 | 1.23 (1.14–1.33) | <0.001 |
| Area deprivation index | 1.03 (1.01–1.06) | 0.002 | 1.01 (1.00–1.03) | 0.14 |
| Age | 0.99 (0.99–0.99) | <0.001 | 0.99 (0.99–0.99) | <0.001 |
| Gender | ||||
| Male | Reference | Reference | ||
| Female | 1.42 (1.36–1.47) | <0.001 | 1.38 (1.32–1.43) | <0.001 |
| Race | ||||
| White | Reference | Reference | ||
| Non-white | 1.13 (1.08–1.18) | <0.001 | 1.10 (1.06–1.15) | <0.001 |
| Unknown | 0.91 (0.87–0.95) | <0.001 | 0.93 (0.88–0.97) | 0.002 |
| Ethnicity | ||||
| Non-Hispanic | Reference | Reference | ||
| Hispanic | 1.12 (1.08–1.17) | <0.001 | 1.11 (1.06–1.16) | <0.001 |
| Unknown | 0.93 (0.89–0.98) | 0.01 | 0.99 (0.94–1.05) | 0.85 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amiri, S.; Pham, C.D.; Amram, O.; Alcover, K.C.; Oluwoye, O.; Bravo, L.; Sixberry, M.; McDonell, M.G.; Roll, J.M.; Fresco, A. Proximity to Screening Site, Rurality, and Neighborhood Disadvantage: Treatment Status among Individuals with Sexually Transmitted Infections in Yakima County, Washington. Int. J. Environ. Res. Public Health 2020, 17, 2679. https://doi.org/10.3390/ijerph17082679
Amiri S, Pham CD, Amram O, Alcover KC, Oluwoye O, Bravo L, Sixberry M, McDonell MG, Roll JM, Fresco A. Proximity to Screening Site, Rurality, and Neighborhood Disadvantage: Treatment Status among Individuals with Sexually Transmitted Infections in Yakima County, Washington. International Journal of Environmental Research and Public Health. 2020; 17(8):2679. https://doi.org/10.3390/ijerph17082679
Chicago/Turabian StyleAmiri, Solmaz, Christine D. Pham, Ofer Amram, Karl C. Alcover, Oladunni Oluwoye, Lilian Bravo, Melissa Sixberry, Michael G. McDonell, John M Roll, and Andre Fresco. 2020. "Proximity to Screening Site, Rurality, and Neighborhood Disadvantage: Treatment Status among Individuals with Sexually Transmitted Infections in Yakima County, Washington" International Journal of Environmental Research and Public Health 17, no. 8: 2679. https://doi.org/10.3390/ijerph17082679






