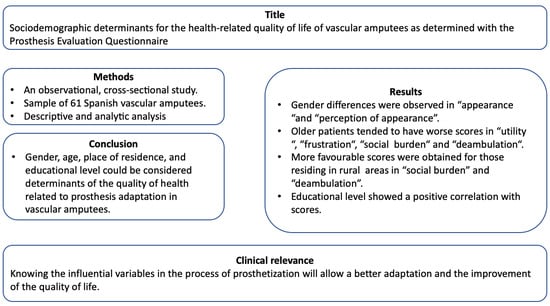
Sociodemographic Determinants for the Health-Related Quality of Life of Patients with Vascular Amputations as Determined with the Prosthesis Evaluation Questionnaire
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Population
2.3. Data Collection
2.4. Analysis Strategy
2.5. Ethical Considerations
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Batten, H.R.; McPhail, S.M.; Mandrusiak, A.M.; Varghese, P.N.; Kuys, S.S. Gait speed as an indicator of prosthetic walking potential following lower limb amputation. Prosthet. Orthot. Int. 2019, 43, 196–203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fowkes, F.G.; Rudan, D.; Rudan, I.; Aboyans, V.; Denenberg, J.O.; McDermott, M.M.; Criqui, M.H. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: A systematic review and analysis. Lancet 2013, 382, 1329–1340. [Google Scholar] [CrossRef]
- Behrendt, C.A.; Sigvant, B.; Szeberin, Z.; Beiles, B.; Eldrup, N.; Thomson, I.A.; Debus, E.S. International Variations in Amputation Practice: A VASCUNET Report. Eur. J. Endovasc. Surg. 2018, 56, 391–399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubio, J.A.; Salido, C.; Albarracín, A.; Jiménez, S.; Alvárez, J. Incidencia de amputaciones de extremidades inferiores en el área 3 de Madrid. Estudio retrospectivo del periodo 2001–2006. Rev. Clin. Esp. 2010, 210, 65–69. [Google Scholar] [CrossRef]
- Jordan, R.W.; Marks, A.; Higman, D. The cost of major lower limb amputation: A 12-year experience. Prosthet. Orthot. Int. 2012, 36, 430–434. [Google Scholar] [CrossRef] [Green Version]
- Miller, M.J.; Magnusson, D.M.; Lev, G.; Fields, T.T.; Cook, P.F.; Stevens-Lapsley, J.E.; Christiansen, C.L. Relationships Among Perceived Functional Capacity, Self-Efficacy, and Disability After Dysvascular Amputation. PmR 2018, 10, 1056–1061. [Google Scholar] [CrossRef]
- Chihuri, S.; Wong, C.K. Factors associated with the likelihood of fall-related injury among people with lower limb loss. INJ Epidemiol. 2018, 5, 42. [Google Scholar] [CrossRef]
- Fajardo-Martos, I.; Roda, O.; Zambudio-Periago, R.; Bueno-Cavanillas, A.; Hita-Contreras, F.; Sanchez-Montesinos, I. Predicting successful prosthetic rehabilitation in major lower-limb amputation patients: A 15-year retrospective cohort study. Braz. J. Phy Ther. 2018, 22, 205–214. [Google Scholar] [CrossRef]
- Christensen, J.; Doherty, P.; Bjorner, J.B.; Langberg, H. Reliability and construct validity of a new Danish translation of the Prosthesis Evaluation Questionnaire in a population of Danish amputees. Prosthet. Orthot. Int. 2017, 41, 469–475. [Google Scholar] [CrossRef]
- Sarandjian, A.; Thompson, A.R.; Datta, D. The experience of men using an upper limb prosthesis following amputation: Positive coping and minimizing feeling different. Disabil. Rehabil. 2008, 30, 871–883. [Google Scholar] [CrossRef]
- Wurdeman, S.R.; Stevens, P.M.; Campbell, J.H. Mobility Analysis of Amputees (MAAT I): Quality of life and satisfaction are strongly related to mobility for patients with a lower limb prosthesis. Prosthet. Orthot. Int. 2018, 42, 498–503. [Google Scholar] [CrossRef] [Green Version]
- Arwert, H.J.; van Doorn-Loogman, M.H.; Koning, J.; Terburg, M.; Rol, M.; Roebroeck, M.E. Residual-limb quality and functional mobility 1 year after transtibial amputation caused by vascular insufficiency. JRRD 2007, 44, 717–722. [Google Scholar] [CrossRef]
- Larner, S.; van Ross, E.; Hale, C. Do psychological measures predict the ability of lower limb amputees to learn to use a prosthesis? Clin. Rehabil. 2003, 17, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Legro, M.W.; Reiber, G.D.; Smith, D.G.; del Aguila, M.; Larsen, J.; Boone, D. Prosthesis evaluation questionnaire for persons with lower limb amputations: Assessing prosthesis-related quality of life. Arch. Phys. Med. Rehabil. 1998, 79, 931–938. [Google Scholar] [CrossRef]
- Erwin, C.B.; Emst, S.; Pieter, U.D.; Jan, H.B. Prosthesis satisfaction in lower limb amputees. a systematic review of associated factors and questionnaires. Medicine 2018, 97, 39. [Google Scholar]
- Day, S.J.; Buis, A. Cross cultural equivalence testing of the Prosthetic Evaluation Questionnaire (PEQ) for an Arabic speaking population. Prosthet. Orthot. Int. 2012, 36, 173–180. [Google Scholar] [CrossRef] [Green Version]
- Benavent, J.V.; Igual, C.; Mora, E.; Antonio, R.; Tenias, J.M. Cross-cultural validation of the Prosthesis Evaluation Questionnaire in vascular amputees fitted with prostheses in Spain. Prosthet. Orthot. Int. 2016, 40, 713–719. [Google Scholar] [CrossRef] [Green Version]
- Franchignoni, F.; Giordano, A.; Ferriero, G.; Orlandini, D.; Amoresano, A.; Perucca, L. Measuring mobility in people with lower limb amputation: Rasch analysis of the mobility section of the prosthesis evaluation questionnaire. J. Rehabil. Med. 2007, 39, 138–144. [Google Scholar] [CrossRef] [Green Version]
- Repo, J.P.; Piitulainen, K.; Hakkinen, A.; Roine, R.P.; Kautiainen, H.; Becker, P.; Tukiainen, E.J. Reliability and validity of the Finnish version of the prosthesis evaluation questionnaire. Disabil. Rehabil. 2018, 40, 2081–2087. [Google Scholar] [CrossRef]
- Penn-Barwell, J.G. Outcomes in lower limb amputation following trauma: A systematic review and meta-analysis. Injury 2011, 42, 1474–1479. [Google Scholar] [CrossRef]
- Torbjornsson, E.; Ottosson, C.; Blomgren, L.; Bostrom, L.; Fagerdahl, A.M. The patient’s experience of amputation due to peripheral arterial disease. J. Vasc. Nur. 2017, 35, 57–63. [Google Scholar] [CrossRef]
- Grzebien, A.; Chabowski, M.; Malinowski, M.; Uchmanowicz, I.; Milan, M.; Janczak, D. Analysis of selected factors determining quality of life in patients after lower limb amputation—A review article. Pol. Przegl. Chir. 2017, 89, 57–61. [Google Scholar] [CrossRef]
- Solar, O.; Irwin, A. A Conceptual Framework for Action on the Social Determinants of Health; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Alrajhl, M.; Aldhafri, S.; Alkharusi, H.; Alharthy, I.; Albarasgi, H.; Alhadabi, A. Grade and gender effects on self-concept development. Open Psychol. 2019, 12, 66–75. [Google Scholar] [CrossRef]
- Buijck, B.I.; van Eijk, M.S.; Zuidema, S.U.; Gerritsen, D.L.; Koopmans, R.T.; van der Linde, H. Determinants of quality of life in older adults after lower limb amputation and rehabilitation in skilled nursing facilities. J. Am. Geriatr. Soc. 2012, 60, 796–798. [Google Scholar] [CrossRef]
- Sahu, A.; Sagar, R.; Sarkar, S.; Sagar, S. Psychological effects of amputation: A review of studies from India. Ind. Psychiatry J. 2016, 25, 4–10. [Google Scholar] [CrossRef]
- Reichmann, J.P.; Bartman, K.R. An integrative review of peer support for patients undergoing major limb amputation. J. Vasc. Nur. 2018, 36, 34–39. [Google Scholar] [CrossRef]
- Jiménez García, K. Ajuste psicosocial en pacientes amputados: La psicología en el contexto sanitario. Rev. Cúpula 2017, 31, 8–43. [Google Scholar]
- Vogel, T.R.; Petroski, G.F.; Kruse, R.L. Impact of amputation level and comorbidities on functional status of nursing home residents after lower extremity amputation. J. Vasc. Surg. 2014, 59, 1323–1330.e1321. [Google Scholar] [CrossRef] [Green Version]
- Waqar, S.; Noor, R.; Manan Haider Khan, M. Depression, Anxiety & Psychological adjustment among amputees. Int. J. Rehabil. Res. 2015, 4, 14–18. [Google Scholar]

| n (%) | |
|---|---|
| Residence Urban Rural | 20 (32.8%) 41 (67.2%) |
| Cultural level No formal education Primary education Secondary education | 13 (21.3%) 40 (65.6%) 8 (13.1%) |
| Work situation Employed Homemaker Retired | 4 (6.6%) 12 (19.7%) 45 (73.8%) |
| Speaks regional language (Valencian) No Yes | 16 (26.2%) 45 (73.8%) |
| Coincidence of residence with place of birth No Yes | 34 (55.7%) 27 (44.3%) |
| Min | P25 | Median | P75 | Max | |
|---|---|---|---|---|---|
| Utility | 1.0 | 5.4 | 6.5 | 7.8 | 8.8 |
| Appearance | 5.4 | 7.6 | 8.6 | 9.1 | 10.0 |
| Noise | 4.5 | 6.8 | 10.0 | 10.0 | 10.0 |
| Stump Health | 4.3 | 8.2 | 9.2 | 9.7 | 10.0 |
| Perception of Appearance | 0.0 | 6.8 | 8.3 | 9.5 | 10.0 |
| Well-being | 0.0 | 4.6 | 6.3 | 7.5 | 10.0 |
| Frustration | 0.0 | 4.3 | 6.0 | 9.0 | 10.0 |
| Social Burden | 0.0 | 4.6 | 7.0 | 8.3 | 10.0 |
| Ambulation | 0.0 | 2.9 | 5.5 | 7.8 | 9.8 |
| Male (n = 44) | Femal (n = 17) | p | |||||
|---|---|---|---|---|---|---|---|
| P25 | Median | P75 | P 25 | Median | P75 | ||
| Utility | 5.2 | 6.6 | 7.8 | 5.8 | 6.5 | 7.6 | 0.87 |
| Appearance | 8.3 | 9.0 | 9.4 | 7.0 | 7.8 | 8.3 | 0.001 |
| Noise | 7.6 | 10.0 | 10.0 | 5.8 | 9.0 | 10.0 | 0.18 |
| Stump Health | 8.3 | 9.2 | 9.7 | 7.8 | 9.3 | 9.9 | 0.76 |
| Perception of Appearance | 7.0 | 8.5 | 10.0 | 6.0 | 7.0 | 8.5 | 0.046 |
| Well-being | 4.0 | 6.5 | 7.5 | 6.0 | 6.0 | 7.3 | 0.84 |
| Frustration | 4.5 | 6.3 | 9.6 | 2.3 | 5.5 | 8.5 | 0.35 |
| Social Burden | 4.7 | 7.0 | 8.9 | 4.6 | 7.0 | 7.8 | 0.82 |
| Ambulation | 2.9 | 5.5 | 8.1 | 2.9 | 5.5 | 7.3 | 0.85 |
| <=70 Years (n = 26) | >70 Years (n = 35) | p | |||||
|---|---|---|---|---|---|---|---|
| P25 | Median | P75 | P 25 | Median | P75 | ||
| Utility | 5.8 | 7.6 | 8.0 | 5.1 | 6.3 | 7.3 | 0.02 |
| Appearance | 7.4 | 8.3 | 9.0 | 7.8 | 8.7 | 9.4 | 0.18 |
| Noise | 7.4 | 10.0 | 10.0 | 6.0 | 9.5 | 10.0 | 0.26 |
| Stump Health | 8.8 | 9.3 | 9.7 | 7.8 | 9.2 | 9.7 | 0.59 |
| Perception of Appearance | 6.2 | 8.5 | 10.0 | 7.0 | 8.0 | 9.0 | 0.70 |
| Well-being | 5.3 | 6.5 | 7.5 | 4.0 | 6.0 | 7.0 | 0.18 |
| Frustration | 5.4 | 7.5 | 10.0 | 3.5 | 5.5 | 6.5 | 0.04 |
| Social Burden | 6.2 | 7.5 | 9.0 | 4.5 | 6.3 | 7.5 | 0.01 |
| Deambulation | 4.3 | 7.4 | 8.2 | 2.1 | 5.3 | 6.2 | 0.01 |
| Rural (n = 20) | Urban (n = 41) | p | |||||
|---|---|---|---|---|---|---|---|
| P25 | Median | P75 | P 25 | Median | P75 | ||
| Utility | 6.2 | 6.9 | 7.5 | 4.3 | 6.4 | 7.8 | 0.24 |
| Appearance | 8.2 | 8.5 | 9.0 | 7.1 | 8.6 | 9.2 | 0.55 |
| Noise | 6.0 | 9.3 | 10.0 | 7.8 | 10.0 | 10.0 | 0.25 |
| Stump Health | 8.3 | 9.3 | 9.7 | 8.2 | 9.2 | 9.9 | 0.87 |
| Perception of Appearance | 7.0 | 8.0 | 8.5 | 6.4 | 8.5 | 10.0 | 0.49 |
| Well-being | 5.5 | 6.0 | 7.5 | 3.3 | 6.5 | 7.5 | 0.59 |
| Frustration | 5.5 | 6.0 | 9.5 | 1.5 | 6.0 | 8.0 | 0.18 |
| Social Burden | 6.6 | 7.5 | 9.0 | 3.3 | 6.3 | 7.5 | 0.02 |
| Ambulation | 5.1 | 6.5 | 8.1 | 1.9 | 4.4 | 7.0 | 0.02 |
| No Formal Education (n = 13) | Completed Primary Education (n = 40) | Completed Secondary Education (n = 8) | p | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| P25 | Mean | P75 | P25 | Mean | P75 | P25 | Mean | P 75 | ||
| Utility | 3.9 | 6.1 | 6.9 | 5.3 | 6.4 | 7.7 | 7.8 | 8.0 | 8.2 | 0.006 |
| Appearance | 7.2 | 8.4 | 9.4 | 7.3 | 8.5 | 9.2 | 8.5 | 8.8 | 9.0 | 0.89 |
| Noise | 6.8 | 9.5 | 10.0 | 6.5 | 10.0 | 10.0 | 7.3 | 10.0 | 10.0 | 0.86 |
| Stump Health | 7.6 | 9.5 | 9.8 | 8.2 | 9.2 | 9.8 | 8.9 | 9.3 | 9.6 | 0.89 |
| Perception of Appearance | 5.6 | 7.0 | 9.0 | 6.8 | 8.0 | 9.6 | 8.5 | 8.9 | 10.0 | 0.056 |
| Well-being | 3.3 | 6.0 | 7.3 | 4.6 | 6.0 | 7.0 | 7.1 | 7.5 | 8.3 | 0.059 |
| Frustration | 2.3 | 6.0 | 9.8 | 3.5 | 5.8 | 8.3 | 7.1 | 7.5 | 9.4 | 0.10 |
| Social Burden | 3.3 | 4.7 | 8.0 | 4.6 | 6.8 | 7.5 | 8.8 | 9.0 | 9.9 | 0.003 |
| Ambulation | 3.5 | 4.9 | 7.3 | 2.2 | 5.4 | 6.5 | 7.5 | 8.1 | 9.6 | 0.009 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benavent, J.V.; Tenías, J.M.; Pellin, A.; Casaña Mohedo, J.; Cabellos-García, A.C.; Gea-Caballero, V. Sociodemographic Determinants for the Health-Related Quality of Life of Patients with Vascular Amputations as Determined with the Prosthesis Evaluation Questionnaire. Int. J. Environ. Res. Public Health 2020, 17, 2691. https://doi.org/10.3390/ijerph17082691
Benavent JV, Tenías JM, Pellin A, Casaña Mohedo J, Cabellos-García AC, Gea-Caballero V. Sociodemographic Determinants for the Health-Related Quality of Life of Patients with Vascular Amputations as Determined with the Prosthesis Evaluation Questionnaire. International Journal of Environmental Research and Public Health. 2020; 17(8):2691. https://doi.org/10.3390/ijerph17082691
Chicago/Turabian StyleBenavent, José Vicente, José María Tenías, Ana Pellin, Jorge Casaña Mohedo, Ana Cristina Cabellos-García, and Vicente Gea-Caballero. 2020. "Sociodemographic Determinants for the Health-Related Quality of Life of Patients with Vascular Amputations as Determined with the Prosthesis Evaluation Questionnaire" International Journal of Environmental Research and Public Health 17, no. 8: 2691. https://doi.org/10.3390/ijerph17082691
APA StyleBenavent, J. V., Tenías, J. M., Pellin, A., Casaña Mohedo, J., Cabellos-García, A. C., & Gea-Caballero, V. (2020). Sociodemographic Determinants for the Health-Related Quality of Life of Patients with Vascular Amputations as Determined with the Prosthesis Evaluation Questionnaire. International Journal of Environmental Research and Public Health, 17(8), 2691. https://doi.org/10.3390/ijerph17082691