Association between Daily Living Walking Speed and Walking Speed in Laboratory Settings in Healthy Older Adults
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Measures
2.2.1. DWS and LWS Measurements
2.2.2. Other Measurements
2.2.3. Physical Frailty Assessment
2.3. Statistical Analyses
2.4. Ethical Considerations
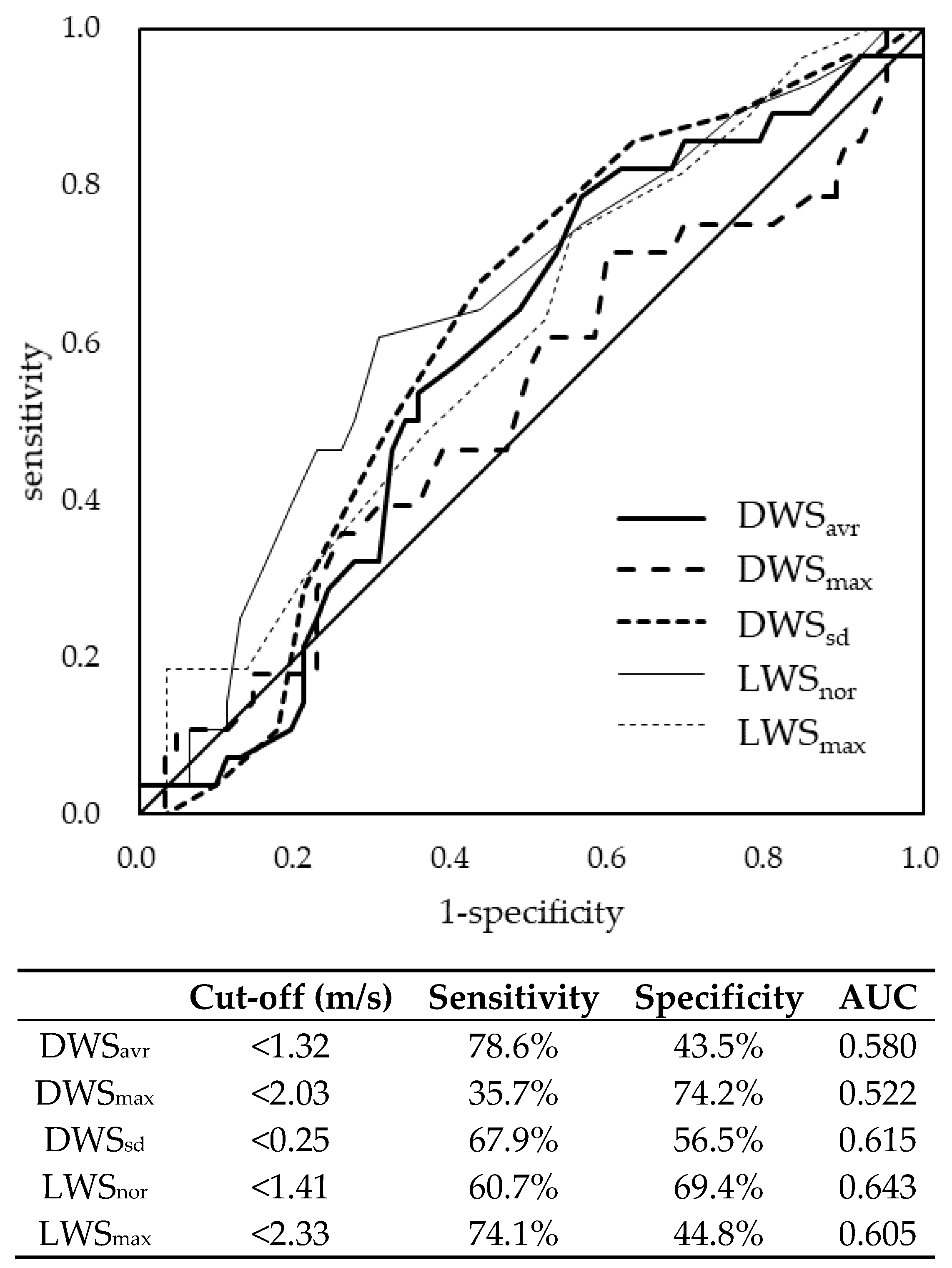
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Murray, M.P.; Kory, R.C.; Clarkson, B.H. Walking patterns in healthy old men. J. Gerontol. 1969, 24, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, M.; Morimoto, Y.; Kimura, M.; Fuchimoto, K.; Fuchimoto, T. A kinematic analysis of walking and physical fitness testing in elderly women. J. Can. Sci. Sport 1991, 16, 223–228. [Google Scholar]
- Kawajiri, H.; Mishina, H.; Asano, S.; Kono, Y.; Hayashi, H.; Niwa, J.I.; Doyu, M.; Kimura, S.; Yamada, S. Maximum walking speed at discharge could be a prognostic factor for vascular events in patients with mild stroke: A cohort study. Arch. Phys. Med. Rehabil. 2019, 100, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Tateuchi, H.; Akiyama, H.; Goto, K.; So, K.; Kuroda, Y.; Ichihashi, N. Gait- and posture-related factors associated with changes in hip pain and physical function in patients with secondary hip osteoarthritis: A prospective cohort study. Arch. Phys. Med. Rehabil. 2019, 100, 2053–2062. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E.; Vellas, B.; Abellan van Kan, G.; Anker, S.D.; Bauer, J.M.; Bernabei, R. Frailty consensus: A call to action. J. Am. Med. Dir. Assoc. 2013, 14, 392–397. [Google Scholar] [CrossRef] [Green Version]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Searle, S.D.; Mitnitski, A.; Gahbauer, E.A.; Gill, T.M.; Rockwood, K. A standard procedure for creating a frailty index. BMC Geriatr. 2008, 8, 24. [Google Scholar] [CrossRef] [Green Version]
- Subra, J.; Gillette-Guyonnet, S.; Cesari, M.; Oustric, S.; Vellas, B. The integration of frailty into clinical practice: Preliminary results from the Gérontopôle. J. Nutr. Health Aging 2012, 16, 714–720. [Google Scholar] [CrossRef]
- Shinkai, S. Walking speed as a good predictor for the onset of functional dependence in a Japanese rural community population. Age. Ageing 2000, 29, 441–446. [Google Scholar] [CrossRef] [Green Version]
- Artaud, F.; Singh-Manoux, A.; Dugravot, A.; Tzourio, C.; Elbaz, A. Decline in fast gait speed as a predictor of disability in older adults. J. Am. Geriatr. Soc. 2015, 63, 1129–1136. [Google Scholar] [CrossRef]
- Albert, S.M.; Bear-Lehman, J.; Anderson, S.J. Declines in mobility and changes in performance in the instrumental activities of daily living among mildly disabled community-dwelling older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2015, 70, 71–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donoghue, O.A.; Savva, G.M.; Cronin, H.; Kenny, R.A.; Horgan, N.F. Using timed up and go and usual gait speed to predict incident disability in daily activities among community-dwelling adults aged 65 and older. Arch. Phys. Med. Rehabil. 2014, 95, 1954–1961. [Google Scholar] [CrossRef] [PubMed]
- Verghese, J.; Annweiler, C.; Ayers, E.; Barzilai, N.; Beauchet, O.; Bennett, D.A.; Bridenbaugh, S.A.; Buchman, A.S.; Callisaya, M.L.; Camicioli, R.; et al. Motoric cognitive risk syndrome: Multicountry prevalence and dementia risk. Neurology 2014, 83, 718–726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jung, H.W.; Jang, L.Y.; Lee, C.K.; Yu, S.S.; Hwang, J.K.; Jeon, C.; Lee, Y.S.; Lee, E. Usual gait speed is associated with frailty status, institutionalization, and mortality in community-dwelling rural older adults: A longitudinal analysis of the Aging Study of Pyeongchang Rural Area. Clin. Interv. Aging 2018, 13, 1079–1089. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Studenski, S. Gait speed and survival in older adults. JAMA 2011, 305, 50–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hardy, S.E.; Perera, S.; Roumani, Y.F.; Chandler, J.M.; Studenski, S.A. Improvement in usual gait speed predicts better survival in older adults. J. Am. Geriatr. Soc. 2007, 55, 1727–1734. [Google Scholar] [CrossRef]
- De la Sierra, A. Definition of white coat hypertension. Hypertension 2013, 62, 16–17. [Google Scholar] [CrossRef] [Green Version]
- Schimpl, M.; Moore, C.; Lederer, C.; Neuhaus, A.; Sambrook, J.; Danesh, J.; Ouwehand, W.; Daumer, M. Association between walking speed and age in healthy, free-living individuals using mobile accelerometry—A cross-sectional study. PLoS ONE 2011, 6, e23299. [Google Scholar] [CrossRef]
- Schimpl, M.; Lederer, C.; Daumer, M. Development and validation of a new method to measure walking speed in free-living environments using the Actibelt® platform. PLoS ONE 2011, 6, e23080. [Google Scholar] [CrossRef] [Green Version]
- Obuchi, S.P.; Tsuchiya, S.; Kawai, H. Test-retest reliability of daily life gait speed as measured by smartphone global positioning system. Gait Post 2018, 61, 282–286. [Google Scholar] [CrossRef]
- Takayanagi, N.; Sudo, M.; Yamashiro, Y.; Lee, S.; Kobayashi, Y.; Niki, Y.; Shimada, H. Relationship between daily and in-laboratory gait speed among healthy community-dwelling older adults. Sci. Rep. 2019, 9, 3496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Ancum, J.M.; van Schooten, K.S.; Jonkman, N.H.; Huijben, B.; van Lummel, R.C.; Meskers, C.G.M.; Maier, A.B.; Pijnappels, M. Gait speed assessed by a 4-m walk test is not representative of daily-life gait speed in community-dwelling adults. Maturitas 2019, 121, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, Y.; Suzuki, H.; Kawai, H.; Hirano, H.; Yoshida, H.; Kojima, M. Physical and sociopsychological characteristics of older community residents with mild cognitive impairment as assessed by the Japanese Version of the Montreal Cognitive Assessment. J. Geriatr. Psychiatry Neurol. 2013, 26, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Kera, T.; Kawai, H.; Yoshida, H.; Hirano, H.; Kojima, M.; Fujiwara, Y.; Ihara, K.; Obuchi, S. Classification of frailty using the Kihon checklist: A cluster analysis of older adults in urban areas. Geriatr. Gerontol. Int. 2017, 17, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Kawai, H.; Ihara, K.; Kera, T.; Hirano, H.; Fujiwara, Y.; Tanaka, M.; Kojima, M.; Obuchi, S. Association between statin use and physical function among community-dwelling older Japanese adults. Geriatr. Gerontol. Int. 2018, 18, 623–630. [Google Scholar] [CrossRef]
- G*Power 3.1 Manual. Available online: http://www.psychologie.hhu.de/fileadmin/redaktion/Fakultaeten/Mathematisch-Naturwissenschaftliche_Fakultaet/Psychologie/AAP/gpower/GPowerManual.pdf (accessed on 3 April 2020).
- Tamaki, K.; Kusunoki, H.; Tsuji, S.; Wada, Y.; Nagai, K.; Itoh, M.; Sano, K.; Amano, M.; Maeda, H.; Hasegawa, Y.; et al. The relationship between dietary habits and frailty in rural Japanese community-dwelling older adults: Cross-sectional observation study using a brief self-administered dietary history questionnaire. Nutrients 2018, 10, 1982. [Google Scholar] [CrossRef] [Green Version]
- Satake, S.; Senda, K.; Hong, Y.J.; Miura, H.; Endo, H.; Sakurai, T.; Kondo, I.; Toba, K. Validity of the Kihon Checklist for assessing frailty status. Geriatr. Gerontol. Int. 2015, 16, 709–715. [Google Scholar] [CrossRef]
- Satake, S.; Shimokata, H.; Senda, K.; Kondo, I.; Toba, K. Validity of Total Kihon Checklist Score for predicting the incidence of 3-year dependency and mortality in a community-dwelling older population. J. Am. Med. Dir. Assoc. 2017, 18, 552.e1–552.e6. [Google Scholar] [CrossRef]
- Seino, S.; Shinkai, S.; Fujiwara, Y.; Obuchi, S.; Yoshida, H.; Hirano, H.; Kim, H.K.; Ishizaki, T.; Takahashi, R. Reference values and age and sex differences in physical performance measures for community-dwelling older Japanese: A pooled analysis of six cohort studies. PLoS ONE 2014, 9, e99487. [Google Scholar] [CrossRef] [Green Version]
- Yamada, Y.; Nanri, H.; Watanabe, Y.; Yoshida, T.; Yokoyama, K.; Itoi, A.; Date, H.; Yamaguchi, M.; Miyake, M.; Yamagata, E.; et al. Prevalence of frailty assessed by Fried and Kihon Checklist indexes in a prospective cohort study: Design and demographics of the Kyoto-Kameoka Longitudinal Study. J. Am. Med. Dir. Assoc. 2017, 18, 733.e7–733.e15. [Google Scholar] [CrossRef]
- Franěk, M.; Režný, L. The effect of priming with photographs of environmental settings on walking speed in an outdoor environment. Front. Psychol. 2017, 8, 73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carvalho, C.; Sunnerhagen, K.S.; Willén, C. Walking speed and distance in different environments of subjects in the later stage post-stroke. Physiother. Theory Pract. 2010, 26, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Rech, A.; Radaelli, R.; Goltz, F.R.; da Rosa, L.H.; Schneider, C.D.; Pinto, R.S. Echo intensity is negatively associated with functional capacity in older women. Age 2014, 36, 9708. [Google Scholar] [CrossRef] [PubMed]
- Sewo Sampaio, P.Y.; Sampaio, R.A.; Yamada, M.; Arai, H. Systematic review of the Kihon Checklist: Is it a reliable assessment of frailty? Geriatr. Gerontol. Int. 2016, 16, 893–902. [Google Scholar] [CrossRef]
| Variables | DWS-Analyzed Participants (n = 90) | Other Participants (n = 679) | p† | ||||
|---|---|---|---|---|---|---|---|
| Sample with Complete Data, n | Mean | SD | Sample with Complete Data, n | Mean | SD | ||
| Age (years) | 90 | 71.8 | 5.59 | 679 | 73.8 | 6.81 | 0.003 |
| Height (cm) | 90 | 158.2 | 9.28 | 679 | 156.7 | 9.20 | 0.147 |
| Weight (kg) | 90 | 57.5 | 11.58 | 679 | 56.3 | 11.28 | 0.340 |
| SMI (kg/m2) | 88 | 6.56 | 1.01 | 675 | 6.48 | 1.06 | 0.465 |
| Grip strength (kg) | 86 | 27.8 | 8.19 | 657 | 27.5 | 8.64 | 0.714 |
| One-legged stance (s) | 90 | 56.7 | 11.65 | 673 | 46.1 | 21.07 | <0.001 |
| KCL score | 83 | 3.0 | 2.97 | 585 | 4.2 | 3.47 | 0.002 |
| DWSavr (m/s) | 90 | 1.28 | 0.115 | - | - | - | - |
| DWSmax (m/s) | 90 | 2.14 | 0.189 | - | - | - | - |
| DWSsd (m/s) | 90 | 0.24 | 0.028 | - | - | - | - |
| LWSnor (m/s) | 90 | 1.42 | 0.216 | 672 | 1.35 | 0.273 | 0.007 |
| LWSmax (m/s) | 85 | 2.24 | 0.387 | 643 | 2.08 | 0.457 | 0.001 |
| n | % | n | % | ||||
| Female | 90 | 56 | 62.2 | 679 | 409 | 60.2 | 0.717 |
| Hypertension | 90 | 37 | 41.1 | 676 | 287 | 42.5 | 0.808 |
| Stroke | 90 | 4 | 4.4 | 676 | 47 | 7.0 | 0.370 |
| Heart disease | 90 | 13 | 14.4 | 676 | 116 | 17.2 | 0.518 |
| Diabetes | 90 | 7 | 7.8 | 676 | 83 | 12.3 | 0.213 |
| Osteoarthritis | 90 | 21 | 23.3 | 676 | 88 | 13.0 | 0.009 |
| Frailty (J-CHS) | 90 | 679 | <0.001 | ||||
| Robust | 62 | 68.9 | 320 | 47.1 | |||
| Pre-frailty | 28 | 31.1 | 327 | 48.2 | |||
| Frailty | 0 | 0.0 | 32 | 4.7 | |||
| n | DWSs (m/s) | LWSs (m/s) | p† | ICC (95% CI) | p‡ | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||||
| DWSavr vs. LWSnor | 90 | 1.28 | 0.115 | 1.42 | 0.216 | <0.001 | 0.341 (0.145–0.511) | 0.999 |
| DWSavr vs. LWSmax | 85 | 1.28 | 0.116 | 2.24 | 0.387 | <0.001 | 0.226 (0.015–0.418) | 1.000 |
| DWSmax vs. LWSnor | 90 | 2.14 | 0.189 | 1.42 | 0.216 | <0.001 | 0.303 (0.103–0.479) | 1.000 |
| DWSmax vs. LWSmax | 85 | 2.14 | 0.192 | 2.24 | 0.387 | 0.016 | 0.188 (−0.025–0.385) | 1.000 |
| Age | SMI | Grip Strength | One-Legged Stance | KCL Score | LWSnor | LWSmax | |
|---|---|---|---|---|---|---|---|
| DWSavr | −0.348 ** | 0.233 * | 0.408 ** | 0.233 * | −0.085 | 0.411 ** | 0.412 ** |
| DWSmax | −0.222 * | −0.065 | 0.068 | 0.048 | −0.166 | 0.306 ** | 0.237 * |
| DWSsd | −0.208 * | 0.128 | 0.244 * | 0.121 | −0.147 | 0.411 ** | 0.340 ** |
| LWSnor | −0.145 | 0.067 | 0.085 | 0.161 | −0.288 ** | 1 | 0.564 ** |
| LWSmax | −0.163 | 0.279 * | 0.363 ** | 0.159 | −0.257 * | 0.564 ** | 1 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawai, H.; Obuchi, S.; Watanabe, Y.; Hirano, H.; Fujiwara, Y.; Ihara, K.; Kim, H.; Kobayashi, Y.; Mochimaru, M.; Tsushima, E.; et al. Association between Daily Living Walking Speed and Walking Speed in Laboratory Settings in Healthy Older Adults. Int. J. Environ. Res. Public Health 2020, 17, 2707. https://doi.org/10.3390/ijerph17082707
Kawai H, Obuchi S, Watanabe Y, Hirano H, Fujiwara Y, Ihara K, Kim H, Kobayashi Y, Mochimaru M, Tsushima E, et al. Association between Daily Living Walking Speed and Walking Speed in Laboratory Settings in Healthy Older Adults. International Journal of Environmental Research and Public Health. 2020; 17(8):2707. https://doi.org/10.3390/ijerph17082707
Chicago/Turabian StyleKawai, Hisashi, Shuichi Obuchi, Yutaka Watanabe, Hirohiko Hirano, Yoshinori Fujiwara, Kazushige Ihara, Hunkyung Kim, Yoshiyuki Kobayashi, Masaaki Mochimaru, Eiki Tsushima, and et al. 2020. "Association between Daily Living Walking Speed and Walking Speed in Laboratory Settings in Healthy Older Adults" International Journal of Environmental Research and Public Health 17, no. 8: 2707. https://doi.org/10.3390/ijerph17082707
APA StyleKawai, H., Obuchi, S., Watanabe, Y., Hirano, H., Fujiwara, Y., Ihara, K., Kim, H., Kobayashi, Y., Mochimaru, M., Tsushima, E., & Nakamura, K. (2020). Association between Daily Living Walking Speed and Walking Speed in Laboratory Settings in Healthy Older Adults. International Journal of Environmental Research and Public Health, 17(8), 2707. https://doi.org/10.3390/ijerph17082707





