The Influence of Income and Livelihood Diversification on Health-Related Quality of Life in Rural Ethiopia
Abstract
1. Introduction
2. Materials and Methods
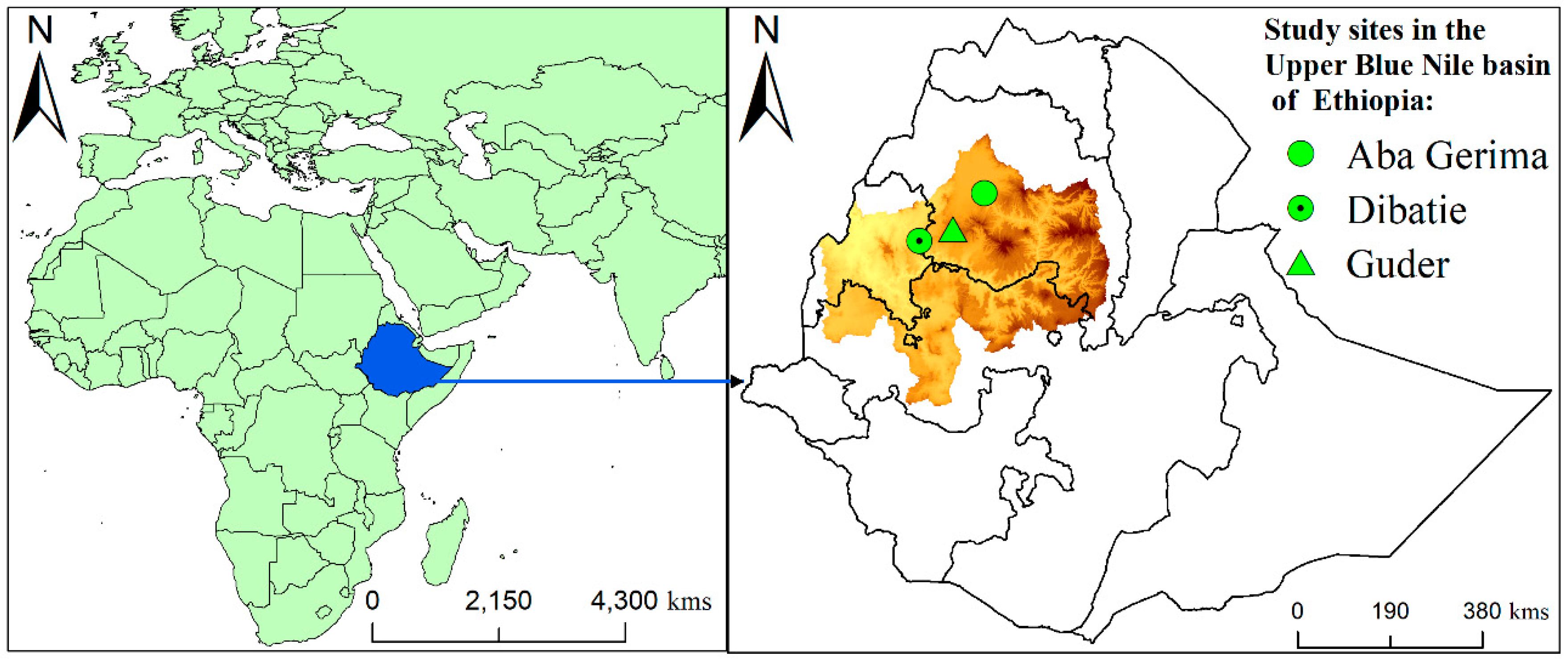
2.1. Study Design and Sites
2.2. Data Collection, Sampling, and Participants
2.3. Outcome Variables
2.4. Other Study Variables
- Demographic characteristics included age, gender of household head (male: 1/female: 0), marital status (single/married), education (no schooling, primary, and secondary), ethnicity, household size (number of individuals in household), land size (land size operated by household), and monthly income.
- Livelihood diversification: We applied the normalized Herfindahl–Simpson diversification index to estimate the livelihood diversification index [31]. In order to do so, we first classified livelihood activities by means of on-farm livelihood activities encompassing crop and livestock production, off-farm activities (wages for labor from other farms), nonfarm activities (earning apart from agricultural sources), and self-employment. To estimate livelihood structures at the household level, we also collected information on the income derived from each livelihood activity in the last year. We then calculated the total income share of livelihood activity carried out by the household in a year as follows:where n denotes the number of livelihood activities, qi is household income from activity i, and Si is the share of livelihood activity i in a given household in 1 year.Secondly, the Herfindahl–Simpson diversity index was adopted to estimate the level of livelihood diversification index, and the indices were then calculated using the following formula:where HHIi represents the Herfindahl–Simpson diversity index, S2i is the squared income share from each livelihood activity, i is the activity, and n is the number of livelihood activities. Finally, we applied the total number of livelihood activities to normalize the Herfindahl–Simpson diversity index to address the limitations linked to uniformity and dominance characteristics using the following formula [31]:where HHIi denotes the normalized Herfindahl–Simpson diversification index, ranging from 0 to 1 (concentration in one activity to full or complete diversification), where higher index values indicate a greater amount of diversification.
- Livestock ownership: The livestock population was calculated using tropical livestock unit (TLU) scores [39]. The TLU conversion factors developed by the Food and Agriculture Organization (FAO) allow for the combination of multiple types of livestock into a weighted measure representing total body weight and market value. A single animal weighing 250 kg represents a single TLU, given weighting factors of 0.7 for cattle, 0.1 for sheep/goats, 0.2 for swine, and 0.01 for chicken.
2.5. Data Analysis
3. Results
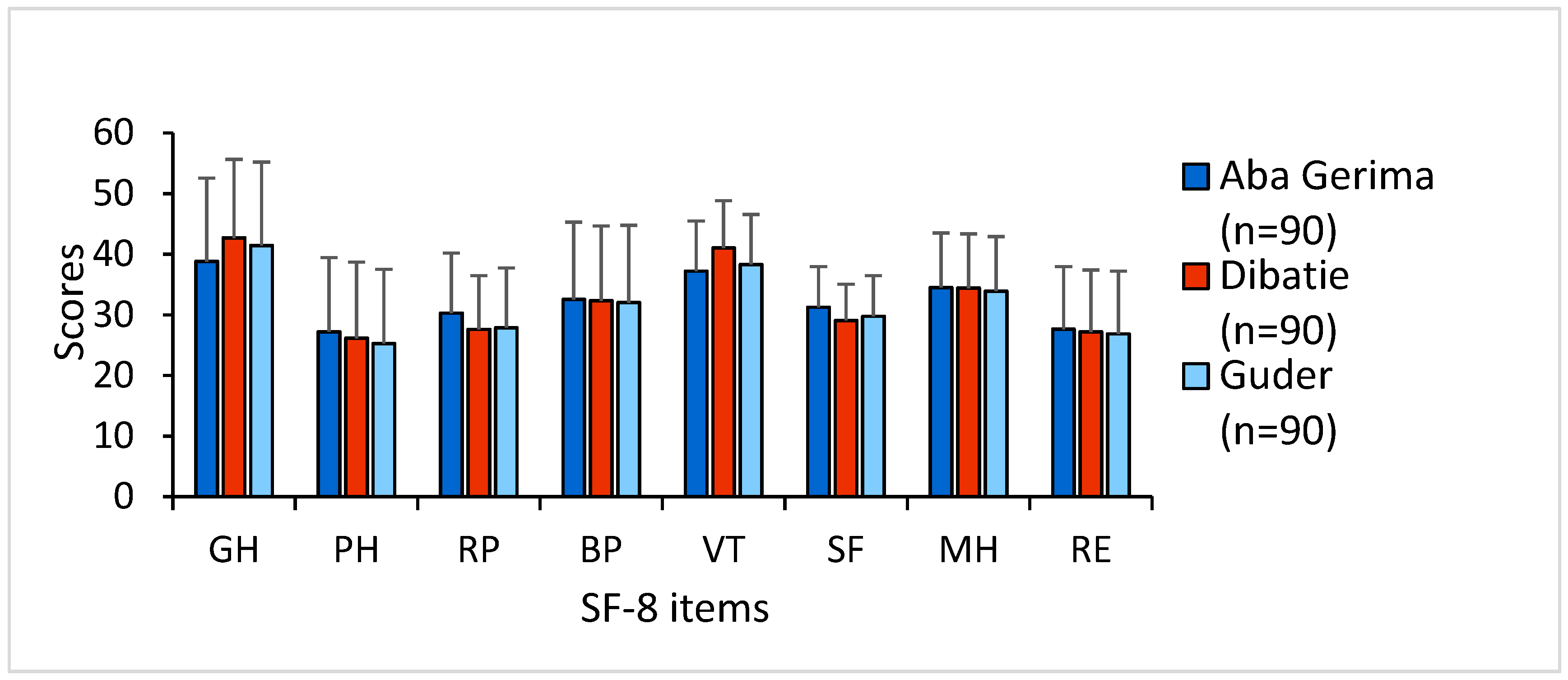
3.1. Descriptive Summary and Internal Consistency Reliability
3.2. Health Status by Participants’ General Characteristics
3.3. Factors Associated with General Physical and Mental Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Guyatt, G.H.; Feeny, D.H.; Patrick, D.L. Measuring Health-Related Quality of Life. Ann. Intern. Med. 1993, 118, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Fayers, P.M.; Sprangers, M.A. Understanding self-rated health. Lancet 2002, 359, 187–188. [Google Scholar] [CrossRef]
- Boström, L.; Chiatti, C.; Thordardottir, B.; Ekstam, L.; Malmgren, F. Health-Related Quality of Life among People Applying for Housing Adaptations: Associated Factors. Int. J. Environ. Res. Public Health 2018, 15, 2130. [Google Scholar] [CrossRef] [PubMed]
- Perenboom, R.J.M.; Wijlhuizen, G.J.; Garre, F.G.; Heerkens, Y.F.; Meeteren, N.L.U. An empirical exploration of the relations between the health components of the International Classification of Functioning, Disability and Health (ICF). Disabil. Rehabil. 2012, 34, 1556–1561. [Google Scholar] [CrossRef] [PubMed]
- Roberts, B.; Ocaka, K.F.; Browne, J.; Oyok, T.; Sondorp, E. Factors associated with the health status of internally displaced persons in northern Uganda. J. Epidemiol. Community Health 2009, 63, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Roberts, B.; Browne, J.; Ocaka, K.F.; Oyuk, T.; Sondrop, E. The reliability and validity of the SF-8 with a conflict-affected population in northern Uganda. Health Qual. Life Outcomes 2008, 6, 108. [Google Scholar] [CrossRef]
- Braveman, P.; Gottlieb, L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014, 129, 19–31. [Google Scholar] [CrossRef]
- Mackenbach, J.P.; Bopp, M.; Deboosere, P.; Kovacs, K.; Leinsalu, M.; Martikainen, P.; Menvielle, G.; Regidor, E.; de Gelder, R. Determinants of the magnitude of socioeconomic inequalities in mortality: A study of 17 European countries. Health Place 2017, 47, 44–53. [Google Scholar] [CrossRef]
- Kawachi, I.; Kennedy, B.P. The relationship of income inequality to mortality: Does the choice of indicator matter? Soc. Sci. Med. 1997, 45, 1121–1127. [Google Scholar] [CrossRef]
- Tan, Z.; Shi, F.; Zhang, H.; Li, N.; Xu, Y.; Liang, Y. Household income, income inequality, and health-related quality of life measured by the EQ-5D in Shaanxi, China: A cross-sectional study. Int. J. Equity Health 2018, 17, 32. [Google Scholar] [CrossRef]
- Kennedy, B.P.; Kawachi, I.; Glass, R.; Prothrow-Stith, D. Income distribution, socioeconomic status, and self rated health in the United States: Multilevel analysis. BMJ 1998, 317, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Pappa, E.; Chatzikonstantinidou, S.; Chalkiopoulos, G.; Papadopoulos, A.; Niakas, D. Health-Related Quality of Life of the Roma in Greece: The Role of Socio-Economic Characteristics and Housing Conditions. Int. J. Environ. Res. Public Health 2015, 12, 6669–6681. [Google Scholar] [CrossRef] [PubMed]
- Pappa, E.; Kontodimopoulos, N.; Papadopoulos, A.A.; Niakas, D. Assessing the socio-economic and demographic impact on health-related quality of life: Evidence from Greece. Int. J. Public Health 2009, 54, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Puteh, S.E.W.; Siwar, C.; Zaidi, M.A.S.; Kadir, H.A. Health related quality of life (HRQOL) among low socioeconomic population in Malaysia. BMC Public Health 2019, 19, 551. [Google Scholar] [CrossRef]
- Zhang, Y.; Ou, F.; Gao, S.; Gao, Q.; Hu, L.; Liu, Y. Effect of Low Income on Health-Related Quality of Life: A Cross-sectional Study in Northeast China. Asia Pac. J. Public Health 2015, 27, 1013–1025. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.L.K.; Guo, V.Y.; Wong, C.K.H.; Yu, E.Y.T.; Fung, C.S.C. Poverty and health-related quality of life of people living in Hong Kong: Comparison of individuals from low-income families and the general population. J. Public Health 2017, 39, 258–265. [Google Scholar] [CrossRef]
- Joffe, M. Health, Livelihoods, and Nutrition in Low-Income Rural Systems. Food Nutr. Bull. 2007, 28, 227–236. [Google Scholar] [CrossRef]
- Hawkes, C.; Ruel, M. The links between agriculture and health: An intersectoral opportunity to improve the health and livelihoods of the poor. Bull. World Health Organ. 2006, 84, 984–990. [Google Scholar] [CrossRef]
- World Bank. Seventh Ethiopia Economic Update: Special Topic: Poverty and Household Welfare in Ethiopia, 2011–2016 (English); World Bank Group: Washington, DC, USA, 2019; Available online: http://documents.worldbank.org/curated/en/432421554200542956/Special-Topic-Poverty-and-Household-Welfare-in-Ethiopia-2011–2016 (accessed on 28 February 2020).
- Adem, M.; Tadele, E.; Mossie, H.; Ayenalem, M. Income diversification and food security situation in Ethiopia: A review study. Cogent Food Agric. 2018, 4, 1513354. [Google Scholar] [CrossRef]
- Abeje, M.T.; Tsunekawa, A.; Haregeweyn, N.; Ayalew, Z.; Nigussi, Z.; Berihun, D.; Adgo, E.; Elias, A. Multidimensional Poverty and Inequality: Insights from the Upper Blue Nile Basin, Ethiopia. Soc. Indic. Res. 2020. [Google Scholar] [CrossRef]
- Abeje, M.T.; Tsunekawa, A.; Haregeweyn, N.; Nigussie, Z.; Adgo, E.; Ayalew, Z.; Tsubo, M.; Elias, A.; Berihun, D.; Quandt, A.; et al. Communities’ Livelihood Vulnerability to Climate Variability in Ethiopia. Sustainability 2019, 11, 6302. [Google Scholar] [CrossRef]
- Manlosa, A.O.; Hanspach, J.; Schultner, J.; Dorresteijin, I.; Fischer, J. Livelihood strategies, capital assets, and food security in rural Southwest Ethiopia. Food Secur. 2019, 11, 167–181. [Google Scholar] [CrossRef] [PubMed]
- Assefa, Y.; Gelaw, Y.; Hill, P.; Taye, B.; Dammn, V.W. Community health extension program of Ethiopia, 2003–2018: Successes and challenges toward universal coverage for primary healthcare services. Glob. Health 2019, 15, 24. [Google Scholar] [CrossRef] [PubMed]
- Habtemariam, M.K.; Semegn, S.T. Setting health sector priorities: A brief overview of Ethiopia’s experience. Cost Eff. Resour. Alloc. 2018, 16, 46. [Google Scholar] [CrossRef]
- Mousley, E.; Deribe, K.; Tamiru, A.; Davey, G. The impact of podoconiosis on quality of life in Northern Ethiopia. Health Qual. Life Outcomes 2013, 11, 122. [Google Scholar] [CrossRef]
- Shumye, S.; Belayneh, Z.; Mengistu, N. Health related quality of life and its correlates among people with depression attending outpatient department in Ethiopia: A cross sectional study. Health Qual. Life Outcomes 2019, 17, 169. [Google Scholar] [CrossRef]
- Gebremichael, D.Y.; Hadush, K.T.; Kebede, E.M.; Zegeye, R.T. Gender difference in health related quality of life and associated factors among people living with HIV/AIDS attending anti-retroviral therapy at public health facilities, western Ethiopia: Comparative cross sectional study. BMC Public Health 2018, 18, 537. [Google Scholar] [CrossRef]
- Gebru, T.; Lentiro, K. The impact of community-based health insurance on health-related quality of life and associated factors in Ethiopia: A comparative cross-sectional study. Health Qual. Life Outcomes 2018, 16, 110. [Google Scholar] [CrossRef]
- Ebabu, K.; Tsunekawa, A.; Haregeweyn, N.; Adgo, E.; Meshesha, D.T.; Aklog, D.; Masunaga, T.; Tsubo, M.; Sultan, D.; Fenta, A.A.; et al. Exploring the variability of soil properties as influenced by land use and management practices: A case study in the Upper Blue Nile basin, Ethiopia. Soil Tillage Res. 2020, 200, 104614. [Google Scholar] [CrossRef]
- Abeje, M.T.; Tsunekawa, A.; Adgo, E.; Haregeweyn, N.; Nigussie, Z.; Ayalew, Z.; Elias, A.; Molla, D.; Berihun, D. Exploring Drivers of Livelihood Diversification and Its Effect on Adoption of Sustainable Land Management Practices in the Upper Blue Nile Basin, Ethiopia. Sustainability 2019, 11, 2991. [Google Scholar] [CrossRef]
- Nigussie, Z.; Tsunekawa, A.; Haregeweyn, N.; Adgo, E.; Nohmi, M.; Tsubo, M.; Aklog, D.; Meshesha, D.T.; Abele, S. Farmers’ Perception about Soil Erosion in Ethiopia. Land Degrad. Dev. 2017, 28, 401–411. [Google Scholar] [CrossRef]
- Hoi, L.V.; Chuc, N.T.K.; Lindholm, L. Health-related quality of life, and its determinants, among older people in rural Vietnam. BMC Public Health 2010, 10, 549. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.; Kosinski, M.; Dewey, J.; Gandek, B. How to Score and Interpret Single-Item Health Status Measures: A Manual for Users of the SF-8 Health Survey; QualityMetric Incorporated: Lincoln, RI, USA, 2001. [Google Scholar]
- Roberts, B.; Damundu, E.Y.; Lomoro Sondrop, E. The influence of demographic characteristics, living conditions, and trauma exposure on the overall health of a conflict-affected population in Southern Sudan. BMC Public Health 2010, 10, 518. [Google Scholar] [CrossRef] [PubMed]
- Lang, L.; Zhang, L.; Zhang, P.; Li, Q.; Bian, J.; Guo, Y. Evaluating the reliability and validity of SF-8 with a large representative sample of urban Chinese. Health Qual. Life Outcomes 2018, 16, 55. [Google Scholar] [CrossRef] [PubMed]
- Lefante, J.; Harmon, G.; Ashby, K.; Barnard, D.; Webber, L. Use of the SF-8 to assess health-related quality of life for a chronically ill, low-income population participating in the Central Louisiana Medication Access Program (CMAP). Qual. Life Res. 2005, 14, 665–673. [Google Scholar] [CrossRef]
- Aoto, H.; Tanimura, C.; Majbauddin, A.; Kobayashi, N.; Morita, T.; Inoue, K.; Otani, S.; Fukada, M.; Hanaki, K. A Conceptual Model for Quality of Life among People with Type 2 Diabetes in the Philippines. Yonago Acta Med. 2019, 62, 53–61. [Google Scholar] [CrossRef]
- Food and Agriculture Organization (FAO). Tropical Livestock Units (TLU). 1999. Available online: http://www.fao.org/ag/againfo/programmes/en/lead/toolbox/Mixed1/TLU.htm#Exchange (accessed on 3 February 2020).
- Qiu, Y.; Yao, M.; Guo, Y.; Zhang, X.; Zhang, S.; Zhang, Y.; Huang, Y.; Zhang, L. Health-Related Quality of Life of Medical Students in a Chinese University: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 5165. [Google Scholar] [CrossRef]
- Wubshet, F.; Engida, T. Health Education in Ethiopia; Taylor, N., Quinn, F., Littledyke, M., Coll, R.K., Eds.; Sense Publishers: Rotterdam, The Netherlands, 2012; pp. 123–131. [Google Scholar] [CrossRef]
- Lahana, E.; Pappa, E.; Niaka, D. The impact of ethnicity, place of residence and socioeconomic status on health-related quality of life: Results from a Greek health survey. Int. J. Public Health 2010, 55, 391–400. [Google Scholar] [CrossRef]
- Clause-Verdreau, A.C.; Audureau, É.; Leplège, A.; Coste, J. Contrasted trends in health-related quality of life across gender, age categories and work status in France, 1995–2016: Repeated population-based cross-sectional surveys using the SF-36. J. Epidemiol. Community Health 2019, 73, 65–72. [Google Scholar] [CrossRef]
- Lund, C.; Breen, A.; Flisher, A.J.; Kakuma, R.; Corrigall, J.; Joska, J.A.; Swartz, L.; Patel, V. Poverty and common mental disorders in low and middle income countries: A systematic review. Soc. Sci. Med. 2010, 71, 517–528. [Google Scholar] [CrossRef]
- Varijakshapanicker, P.; Mckune, S.; Miller, L.; Hendrickx, S.; Balehegn, M.; Dahl, G.E.; Adesogan, A.T. Sustainable livestock systems to improve human health, nutrition, and economic status. Anim. Front. 2019, 9, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Baliatsas, C.; Dückers, M.; Smit, L.; Heederik, D.; Yzermans, J. Morbidity Rates in an Area with High Livestock Density: A Registry-Based Study Including Different Groups of Patients with Respiratory Health Problems. Int. J. Environ. Res. Public Health 2020, 17, 1591. [Google Scholar] [CrossRef] [PubMed]

| SF-8 Item | Reliability | Spearman’s Correlation Coefficient | |||
|---|---|---|---|---|---|
| Mean (SD) | Cronbach’s α Coefficient | Item–Total Correlation | PCS | MCS | |
| General health | 41.03 (13.89) | 0.949 | 0.775 | 0.877 | 0.535 |
| Physical functioning | 26.11 (12.74) | 0.940 | 0.861 | 0.862 | 0.527 |
| Role physical | 28.47 (10.16) | 0.940 | 0.863 | 0.837 | 0.578 |
| Bodily pain | 32.24 (12.86) | 0.938 | 0.885 | 0.876 | 0.570 |
| Vitality | 38.87 (9.02) | 0.944 | 0.799 | 0.807 | 0.703 |
| Social functioning | 29.85 (6.83) | 0.947 | 0.810 | 0.733 | 0.706 |
| Role emotional | 34.20 (9.25) | 0.942 | 0.833 | 0.679 | 0.830 |
| Mental health | 27.10 (10.64) | 0.941 | 0.846 | 0.709 | 0.787 |
| Overall PCS score | 30.50 (12.18) | ||||
| Overall MCS score | 34.40 (7.26) |
| Variables | All | N (%) | PCS Mean ± SD | p Value | MCS Mean ± SD | p Value |
|---|---|---|---|---|---|---|
| Gender | Male | 218 (80.70) | 29.28 ± 11.42 | <0.001 | 33.62 ± 6.67 | <0.001 |
| Female | 52 (19.30) | 35.90 ± 14.00 | 38.09 ± 8.69 | |||
| Age | ≤30 | 16 (5.90) | 26.79 ± 10.34 | 0.068 | 33.84 ± 6.60 | 0.038 |
| 31–40 | 69 (25.60) | 29.09 ± 11.29 | 32.50 ± 5.90 | |||
| 41–50 | 81 (30.00) | 29.90 ± 12.57 | 34.31 ± 7.23 | |||
| 51–60 | 53 (19.60) | 32.25 ± 11.74 | 35.10 ± 7.14 | |||
| 61–70 | 35 (13.00) | 35.30 ± 12.98 | 36.87 ± 8.60 | |||
| >70 | 16 (5.90) | 31.99 ± 13.70 | 37.29 ± 9.52 | |||
| Marital status | Single | 56 (20.70) | 36.10 ± 14.10 | <0.001 | 37.57 ± 8.45 | <0.001 |
| Married | 214 (79.30) | 29.10 ± 11.27 | 33.68 ± 6.77 | |||
| Education | No schooling | 211 (78.10) | 31.43 ± 12.73 | 0.130 | 34.92 ± 7.64 | 0.431 |
| ≤Primary | 41 (15.20) | 26.09 ± 9.44 | 33.09 ± 5.66 | |||
| ≥Secondary | 18 (6.70) | 30.48 ± 9.60 | 32.49 ± 5.98 | |||
| Ethnicity | Amhara | 205 (75.90) | 30.02 ± 12.36 | 0.364 | 34.16 ± 6.72 | 0.202 |
| Agew | 57 (21.10) | 32.60 ± 11.58 | 36.18 ± 9.28 | |||
| Others | 8 (3.00) | 29.66 ± 12.90 | 30.61 ± 1.13 | |||
| Household size | ≤5 | 130 (48.10) | 32.25 ± 13.15 | 0.027 | 35.24 ± 7.79 | 0.103 |
| >5 | 140 (51.90) | 28.97 ± 11.09 | 33.78 ± 6.77 | |||
| Land owned | <1 ha | 123 (45.60) | 31.10 ± 12.74 | 0.505 | 35.04 ± 7.65 | 0.255 |
| ≥1 ha | 147 (54.40) | 30.10 ± 11.79 | 34.02 ± 6.99 | |||
| Watersheds | Guder | 90 (33.30) | 30.04 ± 11.21 | 0.884 | 34.28 ± 7.04 | 0.886 |
| Aba Gerima | 90 (33.30) | 30.91 ± 13.93 | 34.38 ± 7.51 | |||
| Dibatie | 90 (33.30) | 30.71 ± 11.44 | 34.79 ± 7.42 | |||
| Income (Birr/month) | <300 (Q1) | 68 (25.20) | 30.00 ± 12.38 | 0.012 | 35.64 ± 8.51 | 0.053 |
| 301–650 (Q2) | 67 (24.80) | 27.57 ± 10.98 | 32.91 ± 6.44 | |||
| 651–1000(Q3) | 68 (25.20) | 30.24 ± 12.18 | 33.87 ± 6.75 | |||
| >1000 (Q4) | 67 (24.80) | 34.42 ± 12.52 | 35.51± 7.13 | |||
| Livelihood diversification * | ≤0.01 (Q1) | 104 (38.50) | 29.11 ± 12.32 | 0.022 | 34.51 ± 7.33 | 0.287 |
| 0.02–0.24 (Q2) | 32 (11.90) | 28.22 ± 11.06 | 33.09 ± 6.69 | |||
| 0.25–0.50 (Q3) | 68 (25.20) | 29.97 ± 10.76 | 33.65 ± 6.30 | |||
| ≥0.51 (Q4) | 64 (23.70) | 34.53 ± 13.20 | 35.86 ± 8.26 | |||
| Tropical livestock unit | ≤2.30 (Q1) | 70 (25.90) | 35.33 ± 14.39 | 0.045 | 36.91 ± 8.76 | 0.025 |
| 2.31–3.85 (Q2) | 68 (25.20) | 29.43 ± 11.83 | 34.64 ± 7.51 | |||
| 3.86-5.45 (Q3) | 68 (25.20) | 28.94 ± 10.25 | 32.52 ± 5.49 | |||
| ≥5.46 (Q4) | 64 (23.70) | 28.23 ± 10.72 | 33.74 ± 6.35 |
| PCS | MCS | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | β | SE | 95% CI | p | β | SE | 95% CI | p |
| Female (male ref) | 2.47 | 2.40 | −2.26; 7.21 | 0.305 | 2.82 | 1.41 | 0.02; 5.61 | 0.048 |
| Age ≤ 30 (age > 70 ref) | −4.10 | 4.01 | −12.01; 3.79 | 0.307 | −3.97 | 2.64 | −9.18; 1.23 | 0.134 |
| Age 31–40 (age > 70 ref) | −0.96 | 3.38 | −7.62; 5.69 | 0.776 | −4.80 | 2.36 | −9.45; −0.15 | 0.043 |
| Age 41–50 (age > 70 ref) | −0.54 | 3.39 | −7.23; 6.14 | 0.872 | −3.20 | 2.45 | −8.03; 1.62 | 0.193 |
| Age 51–60 (age > 70 ref) | 1.65 | 3.47 | −5.19; 8.49 | 0.636 | −2.58 | 2.47 | −7.46; 2.29 | 0.298 |
| Age 61–70 (age > 70 ref) | 3.62 | 3.60 | −3.48; 10.73 | 0.317 | −0.69 | 2.59 | −5.79; 4.41 | 0.790 |
| Married (single ref) | −3.90 | 2.47 | −8.77; 0.95 | 0.115 | −1.52 | 1.28 | −4.04; 1.01 | 0.237 |
| Household size | 0.13 | 0.40 | −0.65; 0.92 | 0.733 | 0.03 | 0.25 | −0.47; 0.54 | 0.890 |
| Income Q1 (Q4 ref) | −4.45 | 2.10 | −8.60; −0.31 | 0.035 | 0.46 | 1.31 | −2.12; 3.05 | 0.722 |
| Income Q2 (Q4 ref) | −5.38 | 2.04 | −9.40; −1.36 | 0.009 | −1.82 | 1.26 | −4.31; 0.65 | 0.148 |
| Income Q3 (Q4 ref) | −2.25 | 2.18 | −6.55; 2.04 | 0.302 | −0.70 | 1.26 | −3.19; 1.78 | 0.579 |
| Livelihood diversification * | 5.56 | 2.09 | 1.43; 9.68 | 0.008 | − | − | − | − |
| Tropical livestock unit | −0.54 | 0.22 | −0.99; −0.09 | 0.017 | −0.17 | 0.13 | −0.43; 0.08 | 0.197 |
| Constant | 35.69 | 4.10 | 27.60; 43.78 | <0.001 | 39.18 | 2.60 | 34.06; 44.31 | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Majbauddin, A.; Otani, S.; Tsunekawa, A.; Haregeweyn, N.; Abeje, M.T.; Nigussie, Z.; Alam, I.; Qing, Q.; Masumoto, T.; Kurozawa, Y. The Influence of Income and Livelihood Diversification on Health-Related Quality of Life in Rural Ethiopia. Int. J. Environ. Res. Public Health 2020, 17, 2709. https://doi.org/10.3390/ijerph17082709
Majbauddin A, Otani S, Tsunekawa A, Haregeweyn N, Abeje MT, Nigussie Z, Alam I, Qing Q, Masumoto T, Kurozawa Y. The Influence of Income and Livelihood Diversification on Health-Related Quality of Life in Rural Ethiopia. International Journal of Environmental Research and Public Health. 2020; 17(8):2709. https://doi.org/10.3390/ijerph17082709
Chicago/Turabian StyleMajbauddin, Abir, Shinji Otani, Atsushi Tsunekawa, Nigussie Haregeweyn, Misganaw Teshager Abeje, Zerihun Nigussie, Intekhab Alam, Qing Qing, Toshio Masumoto, and Youichi Kurozawa. 2020. "The Influence of Income and Livelihood Diversification on Health-Related Quality of Life in Rural Ethiopia" International Journal of Environmental Research and Public Health 17, no. 8: 2709. https://doi.org/10.3390/ijerph17082709
APA StyleMajbauddin, A., Otani, S., Tsunekawa, A., Haregeweyn, N., Abeje, M. T., Nigussie, Z., Alam, I., Qing, Q., Masumoto, T., & Kurozawa, Y. (2020). The Influence of Income and Livelihood Diversification on Health-Related Quality of Life in Rural Ethiopia. International Journal of Environmental Research and Public Health, 17(8), 2709. https://doi.org/10.3390/ijerph17082709







