Relationship between Health-Related Quality of Life and Physical Activity in Children with Hyperactivity
Abstract
1. Introduction
2. Materials and Methods
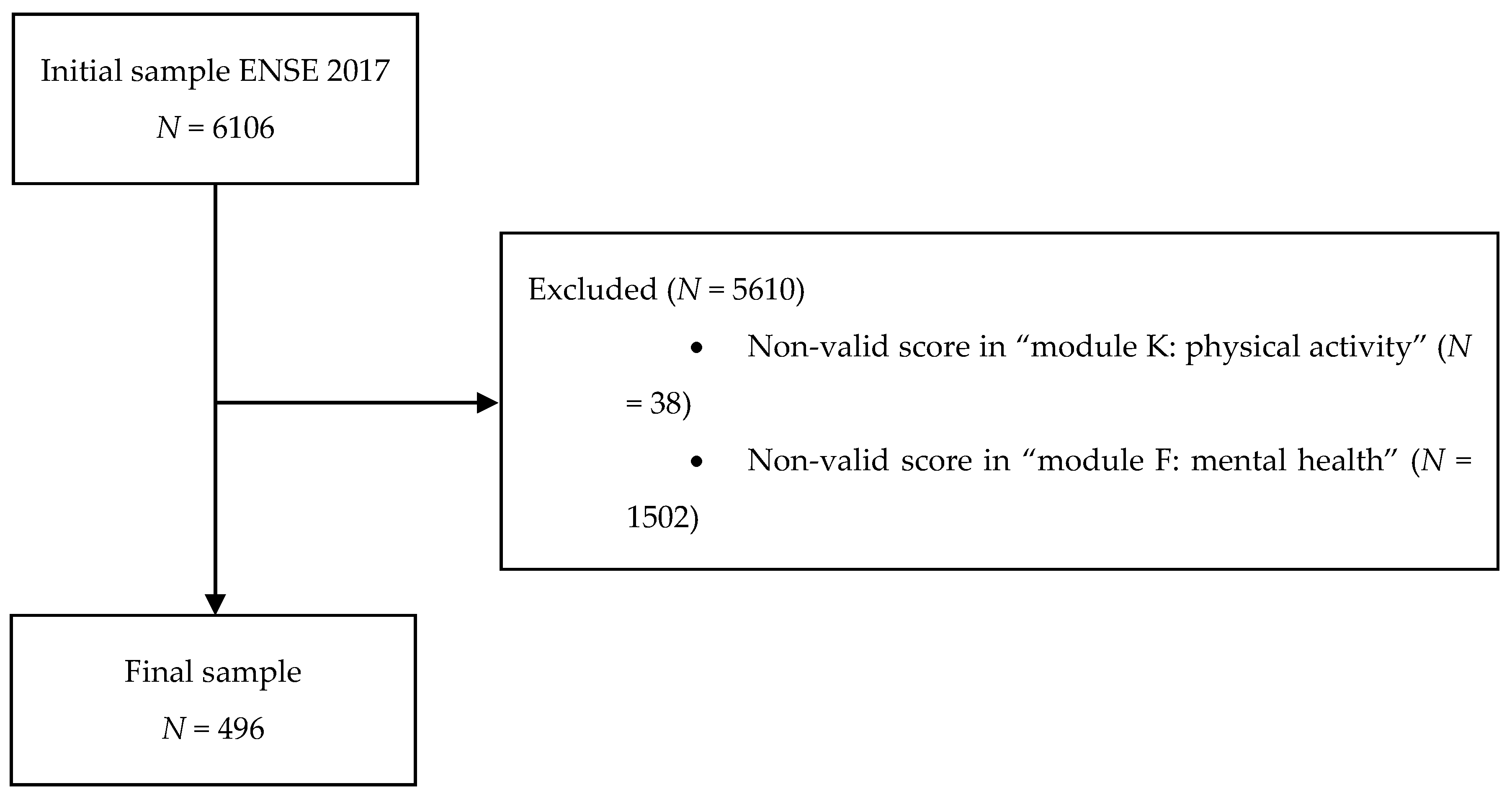
2.1. Participants
2.2. Evaluation Procedure and Instruments
2.3. Variables Used in the Analysis
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- Boys, aged 8–14 years old with ADHD may be more likely to engage in physical activity than girls of the same age with ADHD.
- There may be a decline in HRQoL in the transition from primary to secondary school education in children with ADHD.
- The practice of physical activity may contribute to the improvement of HRQoL in children with ADHD; it may be possible to achieve greater benefits at higher levels of physical activity practice.
- Increased frequency of physical activity in children aged 8–14 with ADHD could be related to feeling good and fit; feeling full of energy, having more fun with friends, and doing better in school.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Villar, I.O. Déficit de Atención con Hiperactividad: Manual Para Padres y Educadores; Ciencias de la Educación Preescolar y Especial: Madrid, Spain, 1998. [Google Scholar]
- Cardo, E.; Servera, M. Attention deficit hyperactivity disorder: The state of the matter and further research approaches. Rev. De Neurol. 2008, 46, 365–372. [Google Scholar]
- González, M.I.N.; Villamisar, D.A.G. El concepto de hiperactividad infantil en perspectiva: Breve análisis de su evolución histórica. Rev. De Hist. De La Psicol. 2010, 31, 23–36. [Google Scholar]
- Spencer, T.J. Attention-deficit/hyperactivity disorder. Arch. Neurol. 2002, 59, 314–316. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- de Sanidad, M.; Servicios Sociales e Igualdad. Clasificación Internacional de Enfermedades—10ª Revisión Modificación Clínica; Ministerio de Sanidad, Servicios Sociales e Igualdad, Secretaría General Técnica: Madrid, Spain, 2018. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/normalizacion/CIE10/CIE10ES_2018_diag_pdf_20180202.pdf (accessed on 17 April 2020).
- Faraone, S.V.; Sergeant, J.; Gillberg, C.; Biederman, J. The worldwide prevalence of ADHD: Is it an American condition? World Psychiatry Off. J. World Psychiatr. Assoc. (Wpa) 2003, 2, 104–113. [Google Scholar]
- Polanczyk, G.; de Lima, M.S.; Horta, B.L.; Biederman, J.; Rohde, L.A. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am. J. Psychiatry 2007, 164, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Wehmeier, P.M.; Schacht, A.; Barkley, R.A. Social and Emotional Impairment in Children and Adolescents with ADHD and the Impact on Quality of Life. J. Adolesc. Health 2010, 46, 209–217. [Google Scholar] [CrossRef]
- LeFever, G.B.; Villers, M.S.; Morrow, A.L.; Vaughn, E.S. Parental perceptions of adverse educational outcomes among children diagnosed and treated for ADHD: A call for improved school/provider collaboration. Psychol. Sch. 2002, 39, 63–71. [Google Scholar] [CrossRef]
- Biederman, J.; Monuteaux, M.C.; Doyle, A.E.; Seidman, L.J.; Wilens, T.E.; Ferrero, F.; Morgan, C.L.; Faraone, S.V. Impact of executive function deficits and attention-deficit/hyperactivity disorder (ADHD) on academic outcomes in children. J. Consult. Clin. Psychol. 2004, 72, 757–766. [Google Scholar] [CrossRef]
- Shaw, M.; Hodgkins, P.; Caci, H.; Young, S.; Kahle, J.; Woods, A.G.; Arnold, L.E. A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: Effects of treatment and non-treatment. BMC Med. 2012, 10, 99. [Google Scholar] [CrossRef]
- Klassen, A.F.; Miller, A.; Fine, S. Health-related quality of life in children and adolescents who have a diagnosis of attention-deficit/hyperactivity disorder. Pediatrics 2004, 114, E541–E547. [Google Scholar] [CrossRef]
- Hernández Martínez, M.; Pastor Hernández, N.; Pastor Durán, X.; Boix Lluch, C.; Sans Fitó, A. Calidad de vida en niños con trastorno por déficit de atención con o sin hiperactividad (TDAH). Pediatría Atención Primaria 2017, 19, 31–39. [Google Scholar]
- Ahnemark, E.; Di Schiena, M.; Fredman, A.C.; Medin, E.; Soderling, J.K.; Ginsberg, Y. Health-related quality of life and burden of illness in adults with newly diagnosed attention-deficit/hyperactivity disorder in Sweden. BMC Psychiatry 2018, 18, 223. [Google Scholar] [CrossRef] [PubMed]
- Peasgood, T.; Bhardwaj, A.; Biggs, K.; Brazier, J.E.; Coghill, D.; Cooper, C.L.; Daley, D.; De Silva, C.; Harpin, V.; Hodgkins, P.; et al. The impact of ADHD on the health and well-being of ADHD children and their siblings. Eur. Child Adolesc. Psychiatry 2016, 25, 1217–1231. [Google Scholar] [CrossRef] [PubMed]
- Spieth, L.E.; Harris, C.V. Assessment of health-related quality of life in children and adolescents: An integrative review. J. Pediatric Psychol. 1996, 21, 175–193. [Google Scholar] [CrossRef] [PubMed]
- Testa, M.A.; Simonson, D.C. Current concepts—Assessment of quality-of-life outcomes. N. Engl. J. Med. 1996, 334, 835–840. [Google Scholar] [CrossRef] [PubMed]
- Schwartzmann, L. Health-Related Quality of Life: Conceptual Aspects. Available online: https://www.researchgate.net/publication/262590501_Calidad_de_vida_relacionada_con_la_salud_Aspectos_conceptuales (accessed on 15 April 2020).
- Schwartzmann, L. Calidad de vida relacionada con la salud: Aspectos conceptuales. Cienc. Y Enfermería 2003, 9, 09–21. [Google Scholar]
- Bize, R.; Johnson, J.A.; Plotnikoff, R.C. Physical activity level and health-related quality of life in the general adult population: A systematic review. Prev. Med. 2007, 45, 401–415. [Google Scholar] [CrossRef]
- Anokye, N.K.; Trueman, P.; Green, C.; Pavey, T.G.; Taylor, R.S. Physical activity and health related quality of life. BMC Public Health 2012, 12, 8. [Google Scholar] [CrossRef]
- Tessier, S.; Vuillemin, A.; Bertrais, S.; Boini, S.; Le Bihan, E.; Oppert, J.M.; Hercberg, S.; Guillemin, F.; Briancon, S. Association between leisure-time physical activity and health-related quality of life changes over time. Prev. Med. 2007, 44, 202–208. [Google Scholar] [CrossRef]
- Wu, X.Y.; Han, L.H.; Zhang, J.H.; Luo, S.; Hu, J.W.; Sun, K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS ONE 2017, 12, 1–29. [Google Scholar] [CrossRef]
- Marker, A.M.; Steele, R.G.; Noser, A.E. Physical Activity and Health-Related Quality of Life in Children and Adolescents: A Systematic Review and Meta-Analysis. Health Psychol. 2018, 37, 893–903. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J. Study of Health Related Quality of Life for Community Dwelling Elders Focusing on Physical Activity. Soc. Sci. Educ. 2013, 9, 3–10. [Google Scholar]
- Wendel-Vos, G.C.W.; Schuit, A.J.; Tijhuis, M.A.R.; Krombout, D. Leisure time physical activity and health-related quality of life: Cross-sectional and longitudinal associations. Qual. Life Res. 2004, 13, 667–677. [Google Scholar] [CrossRef] [PubMed]
- Hoza, B.; Martin, C.P.; Pirog, A.; Shoulberg, E.K. Using Physical Activity to Manage ADHD Symptoms: The State of the Evidence. Curr. Psychiatry Rep. 2016, 18, 113. [Google Scholar] [CrossRef]
- Song, M.; Lauseng, D.; Lee, S.; Nordstrom, M.; Katch, V. Enhanced Physical Activity Improves Selected Outcomes in Children With ADHD: Systematic Review. West. J. Nurs. Res. 2016, 38, 1155–1184. [Google Scholar] [CrossRef]
- Suarez-Manzano, S.; Ruiz-Ariza, A.; De La Torre-Cruz, M.; Martinez-Lopez, E.J. Acute and chronic effect of physical activity on cognition and behaviour in young people with ADHD: A systematic review of intervention studies. Res. Dev. Disabil. 2018, 77, 12–23. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Consumo y Bienestar Social—Portal Estadístico del SNS—Encuesta Nacional de Salud de España. 2017. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2017.htm (accessed on 16 April 2020).
- Ravens-Sieberer, U. The Kidscreen Questionnaires: Quality of Life Questionnaires for Children and Adolescents; handbook; Pabst Science Publ.: Lengerich, Germany, 2006. [Google Scholar]
- Ravens-Sieberer, U.; Erhart, M.; Rajmil, L.; Herdman, M.; Auquier, P.; Bruil, J.; Power, M.; Duer, W.; Abel, T.; Czemy, L. Reliability, construct and criterion validity of the KIDSCREEN-10 score: A short measure for children and adolescents’ well-being and health-related quality of life. Qual. Life Res. 2010, 19, 1487–1500. [Google Scholar] [CrossRef]
- European Commission, Flash Eurobarometer. Series #246 on the Mental Health and Wellbeing of Children and Young people. Parents’ views on the mental health of their child. Analytical Report. 2009. Available online: https://data.europa.eu/euodp/es/data/dataset/S736_246 (accessed on 16 April 2020).
- Aymerich, M.; Berra, S.; Guillamón, I.; Herdman, M.; Alonso, J.; Ravens-Sieberer, U.; Rajmil, L. Desarrollo de la versión en español del KIDSCREEN: Un cuestionario de calidad de vida para la población infantil y adolescente. Gac. Sanit. 2005, 19, 93–102. [Google Scholar] [CrossRef]
- Lohr, K.N. Assessing health status and quality-of-life instruments: Attributes and review criteria. Qual. Life Res. 2002, 11, 193–205. [Google Scholar] [CrossRef]
- Sharpe, H.; Patalay, P.; Fink, E.; Vostanis, P.; Deighton, J.; Wolpert, M. Exploring the relationship between quality of life and mental health problems in children: Implications for measurement and practice. Eur. Child Adolesc. Psychiatry 2016, 25, 659–667. [Google Scholar] [CrossRef]
- Goodman, R. The strengths and difficulties questionnaire: A research note. J. Child Psychol. Psychiatry Allied Discip. 1997, 38, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R. A Modified Version of the Rutter Parent Questionnaire Including Extra Items on Childrens Strengths—A Research Note. J. Child Psychol. Psychiatry Allied Discip. 1994, 35, 1483–1494. [Google Scholar] [CrossRef] [PubMed]
- Russell, G.; Rodgers, L.R.; Ford, T. The Strengths and Difficulties Questionnaire as a Predictor of Parent-Reported Diagnosis of Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder. PLoS ONE 2013, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kuntsi, J.; Neale, B.M.; Chen, W.; Faraone, S.V.; Asherson, P. The IMAGE project: Methodological issues for the molecular genetic analysis of ADHD. Behav. Brain Funct. BBF 2006, 2, 27. [Google Scholar] [CrossRef]
- Fenollar-Cortes, J.; Calvo-Fernandez, A.; Garcia-Sevilla, J.; Canto-Diez, T.J. Strength and Difficulties Questionnaire (SDQ) as predictor of ADHD: Performance between SCT rates and "Hyperactivity/Impulsivity" and "inattention" domains of ADHD in a clinical sample. An. De Psicol. 2016, 32, 313–319. [Google Scholar]
- Goodman, R.; Ford, T.; Simmons, H.; Gatward, R.; Meltzer, H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br. J. Psychiatry 2000, 177, 534–539. [Google Scholar] [CrossRef]
- Klasen, H.; Woerner, W.; Wolke, D.; Meyer, R.; Overmeyer, S.; Kaschnitz, W.; Rothenberger, A.; Goodman, R. Comparing the German versions of the Strengths and Difficulties Questionnaire (SDQ-Deu) and the Child Behavior Checklist. Eur. Child Adolesc. Psychiatry 2000, 9, 271–276. [Google Scholar] [CrossRef]
- Huss, M.; Hölling, H.; Kurth, B.-M.; Schlack, R. How often are German children and adolescents diagnosed with ADHD? Prevalence based on the judgment of health care professionals: Results of the German health and examination survey (KiGGS). Eur. Child Adolesc. Psychiatry 2008, 17, 52–58. [Google Scholar] [CrossRef]
- Schlack, R.; Hölling, H.; Kurth, B.-M.; Huss, M. Die Prävalenz der Aufmerksamkeitsdefizit-/Hyperaktivitätsstörung (ADHS) bei Kindern und Jugendlichen in Deutschland. Bundesgesundheitsblatt-Gesundh.-Gesundh. 2007, 50, 827–835. [Google Scholar] [CrossRef]
- Doepfner, M.; Breuer, D.; Wille, N.; Erhart, M.; Ravens-Sieberer, U.; Grp, B.S. How often do children meet ICD-10/DSM-IV criteria of attention deficit-/hyperactivity disorder and hyperkinetic disorder? Parent-based prevalence rates in a national sample—Results of the BELLA study. Eur. Child Adolesc. Psychiatry 2008, 17, 59–70. [Google Scholar] [CrossRef]
- Cuffe, S.P.; Moore, C.G.; McKeown, R. ADHD and Health Services Utilization in the National Health Interview Survey. J. Atten. Disord. 2009, 12, 330–340. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R. Psychometric properties of the strengths and difficulties questionnaire. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 1337–1345. [Google Scholar] [CrossRef] [PubMed]
- International Physical Activity Questionnaire (IPAQ). In Grupo de Consenso de Expertos en Actividad Física. 1998. Available online: www.ipaq.ki.se (accessed on 16 April 2020).
- Ministerio de Sanidad, C.Y.B.S. Encuesta Nacional de Salud; Ministerio de Sanidad, Consumo y Bienestar Social Secretaría General Técnica Centro de Publicaciones: Madrid, Spain, 2017. [Google Scholar]
- Estadística, I.N.D. (Ed.) ENSE 2017: Metodología; Gobierno de España: Madrid, Spain, 2018. [Google Scholar]
- Chen, G.; Stevens, K.; Rowen, D.; Ratcliffe, J. From KIDSCREEN-10 to CHU9D: Creating a unique mapping algorithm for application in economic evaluation. Health Qual. Life Outcomes 2014, 12, 134. [Google Scholar] [CrossRef] [PubMed]
- Stevens, K. Valuation of the Child Health Utility 9D Index. PharmacoEconomics 2012, 30, 729–747. [Google Scholar] [CrossRef]
- Chen, G.; Ratcliffe, J. A Review of the Development and Application of Generic Multi-Attribute Utility Instruments for Paediatric Populations. PharmacoEconomics 2015, 33, 1013–1028. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Gosch, A.; Erhart, M.; Rueden, U.; Nickel, J.; Kurth, B.-M.; Duer, W.; Fuerth, K.; Czemy, L.; Auquier, P. The KIDSCREEN Questionnaires—Quality of life Questionnaires for Children and Adolescents—Handbook; Pabst Science Publishers: Lengerich, Germany, 2006. [Google Scholar]
- Miller, R.G.J. Simultaneous Statistical Inference, 2nd ed.; Springer: New York, NY, USA, 1981; Volume XVI, p. 299. [Google Scholar]
- Barrera, M.A.M. Uso de la correlación de Spearman en un estudio de intervención en fisioterapia. Rev. Mov. Científico 2014, 8, 98–104. [Google Scholar] [CrossRef]
- Sampieri, R.H.; Collado, C.F.; Lucio, P.B.; Pérez, M. Metodología de la Investigación; Mcgraw-Hill México: Mexico City, Mexico, 1998; Volume 6, Available online: https://www.esup.edu.pe/descargas/dep_investigacion/Metodologia%20de%20la%20investigaci%C3%B3n%205ta%20Edici%C3%B3n.pdf (accessed on 16 April 2020).
- Reguant Alvarez, M.; Vilà Baños, R.; Torrado Fonseca, M. La relació entre dues variables segons l’escala de mesurament amb SPSS. In REIRE Revista d’Innovació i Recerca en Educació; Universitat de Barcelona: Barcelona, Spain, 2018; Volume 11. [Google Scholar]
- Lasheras, L.; Aznar, S.; Merino, B.; López, E.G. Factors associated with physical activity among Spanish youth through the National Health Survey. Prev. Med. 2001, 32, 455–464. [Google Scholar] [CrossRef]
- Peiró-Velert, C.; Devís-Devís, J.; Beltrán-Carrillo, V.J.; Fox, K.R. Variability of Spanish adolescents’ physical activity patterns by seasonality, day of the week and demographic factors. Eur. J. Sport Sci. 2008, 8, 163–171. [Google Scholar] [CrossRef]
- Riddoch, C.J.; Bo Andersen, L.; Wedderkopp, N.; Harro, M.; Klasson-Heggebo, L.; Sardinha, L.B.; Cooper, A.R.; Ekelund, U. Physical activity levels and patterns of 9- and 15-yr-old European children. Med. Sci. Sports Exerc. 2004, 36, 86–92. [Google Scholar] [CrossRef]
- Ridley, K.; Zabeen, S.; Lunnay, B.K. Children’s physical activity levels during organised sports practices. J. Sci. Med. Sport 2018, 21, 930–934. [Google Scholar] [CrossRef]
- Michel, G.; Bisegger, C.; Fuhr, D.C.; Abel, T. Age and gender differences in health-related quality of life of children and adolescents in Europe: A multilevel analysis. Qual. Life Res. 2009, 18, 1147. [Google Scholar] [CrossRef]
- Gavala Gonzalez, J. Motivations for Sevillian Young People to Abandon Physical Activity Practice. Rev. Iberoam. De Cienc. De La Act. Fis. Y El Deporte 2012, 1, 15–23. [Google Scholar]
- Currie, C.; Roberts, C.; Settertobulte, W.; Morgan, A.; Smith, R.; Samdal, O.; Barnekow Rasmussen, V.; World Health Organization. Young People’s Health in Context: Health Behaviour in School-Aged Children (HBSC) Study: International Report from the 2001/2002 Survey; WHO Regional Office for Europe: Copenhagen, Denmark, 2004. [Google Scholar]
- Martínez, A.; Gallardo, A.; García-Tascón, M.; Segarra, E. Análisis De La Participación De Los Escolares (9-18 Años) En El Programa De Promoción Deportiva De La Región De Murcia. J. Sport Health Res. 2018, 10, 101–116. [Google Scholar]
- Ng, Q.X.; Ho, C.Y.X.; Chan, H.W.; Yong, B.Z.J.; Yeo, W.S. Managing childhood and adolescent attention-deficit/hyperactivity disorder (ADHD) with exercise: A systematic review. Complementary Ther. Med. 2017, 34, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Cerrillo-Urbina, A.; García-Hermoso, A.; Sánchez-López, M.; Jesús Pardo-Guijarro, M.; L Santos Gómez, J.; Martinez Vizcaino, V. The Effects of Physical Exercise in Children with Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-analysis of Randomized Control Trials: Exercise and Attention Deficit Hyperactivity Disorder; Wiley: Hoboken, NJ, USA, 2015; Volume 41. [Google Scholar]
- Reeves, M.J.; Bailey, R.P. The effects of physical activity on children diagnosed with attention deficit hyperactivity disorder: A review. Education 3–13 2016, 44, 591–603. [Google Scholar] [CrossRef]
- Gopinath, B.; Hardy, L.L.; Baur, L.A.; Burlutsky, G.; Mitchell, P. Physical activity and sedentary behaviors and health-related quality of life in adolescents. Pediatrics 2012, 130, e167–e174. [Google Scholar] [CrossRef]
- Bowling, A. Measuring Health: A Review of Quality of Life Measurement Scales; Open University Press: Buckingham, UK, 1991. [Google Scholar]
- Smith, J.J.; Eather, N.; Weaver, R.G.; Riley, N.; Beets, M.W.; Lubans, D.R. Behavioral Correlates of Muscular Fitness in Children and Adolescents: A Systematic Review. Sports Med. (Auckl. N.Z.) 2019, 49, 887–904. [Google Scholar] [CrossRef]
- Biddle, S.J.; Asare, M. Physical activity and mental health in children and adolescents: A review of reviews. Br. J. Sports Med. 2011, 45, 886–895. [Google Scholar] [CrossRef]
- Rodriguez-Ayllon, M.; Cadenas-Sanchez, C.; Estevez-Lopez, F.; Munoz, N.E.; Mora-Gonzalez, J.; Migueles, J.H.; Molina-Garcia, P.; Henriksson, H.; Mena-Molina, A.; Martinez-Vizcaino, V.; et al. Role of Physical Activity and Sedentary Behavior in the Mental Health of Preschoolers, Children and Adolescents: A Systematic Review and Meta-Analysis. Sports Med. (Auckl. N.Z.) 2019, 49, 1383–1410. [Google Scholar] [CrossRef]
- Eime, R.M.; Young, J.A.; Harvey, J.T.; Charity, M.J.; Payne, W.R. A systematic review of the psychological and social benefits of participation in sport for children and adolescents: Informing development of a conceptual model of health through sport. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 98. [Google Scholar] [CrossRef]
- Tomporowski, P.D.; Davis, C.L.; Miller, P.H.; Naglieri, J.A. Exercise and children’s intelligence, cognition, and academic achievement. Educ. Psychol. Rev. 2008, 20, 111–131. [Google Scholar] [CrossRef] [PubMed]
- Wigal, S.B.; Nemet, D.; Swanson, J.M.; Regino, R.; Trampush, J.; Ziegler, M.G.; Cooper, D.M. Catecholamine response to exercise in children with attention deficit hyperactivity disorder. Pediatric Res. 2003, 53, 756–761. [Google Scholar] [CrossRef] [PubMed]
- Wigal, S.B.; Emmerson, N.; Gehricke, J.-G.; Galassetti, P. Exercise: Applications to Childhood ADHD. J. Atten. Disord. 2013, 17, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Kiluk, B.D.; Weden, S.; Culotta, V.P. Sport Participation and Anxiety in Children With ADHD. J. Atten. Disord. 2009, 12, 499–506. [Google Scholar] [CrossRef]
- Quesada, D.; Ahmed, N.U.; Fennie, K.P.; Gollub, E.L.; Ibrahimou, B. A Review: Associations Between Attention-deficit/hyperactivity Disorder, Physical Activity, Medication Use, Eating Behaviors and Obesity in Children and Adolescents. Arch. Psychiatr. Nurs. 2018, 32, 495–504. [Google Scholar] [CrossRef]
- Smith, A.L.; Hoza, B.; Linnea, K.; McQuade, J.D.; Tomb, M.; Vaughn, A.J.; Shoulberg, E.K.; Hook, H. Pilot Physical Activity Intervention Reduces Severity of ADHD Symptoms in Young Children. J. Atten. Disord. 2013, 17, 70–82. [Google Scholar] [CrossRef]
- Barkley, R.A. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychol. Bull. 1997, 121, 65–94. [Google Scholar] [CrossRef]
- Pontifex, M.B.; Saliba, B.J.; Raine, L.B.; Picchietti, D.L.; Hillman, C.H. Exercise Improves Behavioral, Neurocognitive, and Scholastic Performance in Children with Attention-Deficit/Hyperactivity Disorder. J. Pediatrics 2013, 162, 543–551. [Google Scholar] [CrossRef]
- Verret, C.; Guay, M.-C.; Berthiaume, C.; Gardiner, P.; Beliveau, L. A Physical Activity Program Improves Behavior and Cognitive Functions in Children With ADHD: An Exploratory Study. J. Atten. Disord. 2012, 16, 71–80. [Google Scholar] [CrossRef]
| Variables | TOTAL | BOYS | GIRLS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AGE | 8–12 (N = 366) | 13–14 (N = 130) | 8–14 (N = 496) | p | 8–12 (N = 200) | 13–14 (N = 74) | 8–14 (N = 274) | p* | 8–12 (N = 166) | 13–14 (N = 56) | 8–14 (N = 222) | p * | p ** |
| Median (IR) | 10 (2) | 14 (1) | 11 (4) | n/a | 10 (2) | 14 (1) | 11 (4) | n/a | 10 (2) | 14 (1) | 11 (4) | n/a | 0.763 |
| Mean (SD) | 9.83 (1.38) | 13.56 (0.49) | 10.81 (2.04) | 9.82 (1.35) | 13.57 (0.49) | 10.83 (2.04) | 9.84 (1.41) | 13.55 (0.50) | 10.77 (2.04) | ||||
| PA | |||||||||||||
| Median (IR) | 3 (2) | 3 (2) | 3 (2) | 0.113 | 3 (2) | 3 (1) | 3 (2) | 0.068 | 3 (2) | 3 (2) | 3 (2) | 0.768 | 0.005 |
| Mean (SD) | 2.83 (1.03) | 2.98 (1.02) | 2.87 (1.03) | 2.93 (0.99) | 3.16 (0.95) | 2.99 (0.98) | 2.70 (1.07) | 2.75 (1.08) | 2.72 (1.15) | ||||
| KS9 | |||||||||||||
| Median (IR) | 4.69 (0.56) | 4.44 (0.67) | 4.56 (0.61) | 0.034 | 4.61 (0.56) | 4.44 (0.78) | 4.56 (0.67) | 0.027 | 4.67 (0.56) | 4.56 (0.56) | 4.56 (0.56) | 0.501 | 0.081 |
| Mean (SD) | 4.54 (0.39) | 4.44 (0.44) | 4.52 (0.41) | 4.52 (0.41) | 4.37 (0.47) | 4.48 (0.43) | 4.57 (0.36) | 4.53 (0.39) | 4.56 (0.36) | ||||
| MAPPING CHU9D | |||||||||||||
| Median (IR) | 0.78 (0.08) | 0.77 (0.09) | 0.78 (0.08) | 0.313 | 0.77 (0.10) | 0.76 (0.10) | 0.77 (0.10) | 0.903 | 0.80 (0.07) | 0.78 (0.09) | 0.80 (0.08) | 0.185 | 0.014 |
| Mean (SD) | 0.78 (0.06) | 0.77 (0.06) | 0.78 (0.06) | 0.77 (0.07) | 0.77 (0.06) | 0.77 (0.06) | 0.79 (0.06) | 0.77 (0.05) | 0.78 (0.06) | ||||
| PA | KS9 | PA | MEANS DIF | MEDIANS DIF | p * | p ** | |
|---|---|---|---|---|---|---|---|
| 1 | Median (IR) Mean (SD) | 4.37 (0.45) 4.44 (0.56) | 2 | −0.11 | −0.11 | 0.005 | 0.092 |
| 3 | −0.15 | −0.11 | 0.023 | ||||
| 4 | −0.21 | −0.22 | <0.001 | ||||
| 2 | Median (IR) Mean (SD) | 4.49 (0.46) 4.56 (0.78) | 1 | 0.11 | 0.11 | 0.005 | 0.092 |
| 3 | −0.04 | 0.00 | 0.824 | ||||
| 4 | −0.09 | −0.11 | 0.159 | ||||
| 3 | Median (IR) Mean (SD) | 4.53 (0.36) 4.56 (0.45) | 1 | 0.15 | 0.11 | 0.005 | 0.023 |
| 2 | 0.04 | 0.00 | 0.824 | ||||
| 4 | −0.05 | −0.11 | 0.052 | ||||
| 4 | Median (IR) Mean (SD) | 4.58 (0.40) 4.67 (0.50) | 1 | 0.21 | 0.22 | 0.005 | <0.001 |
| 2 | 0.09 | 0.11 | 0.159 | ||||
| 3 | 0.05 | 0.11 | 0.052 |
| PA | MAPPING CHU9D | PA | MEAN DIF | MEDIANS DIF | p* | p** | |
|---|---|---|---|---|---|---|---|
| 1 | Median (IR) Mean (SD) | 0.76 (0.07) 0.75 (0.09) | 2 | −0.01 | −0.02 | 0.005 | 0.206 |
| 3 | −0.03 | −0.05 | 0.002 | ||||
| 4 | −0.03 | −0.05 | 0.001 | ||||
| 2 | Median (IR) Mean (SD) | 0.77 (0.07) 0.77 (0.11) | 1 | 0.01 | 0.02 | 0.005 | 0.206 |
| 3 | −0.01 | −0.02 | 0.206 | ||||
| 4 | −0.02 | −0.03 | 0.083 | ||||
| 3 | Median (IR) Mean (SD) | 0.78 (0.06) 0.80 (0.08) | 1 | 0.03 | 0.05 | 0.005 | 0.002 |
| 2 | 0.01 | 0.02 | 0.206 | ||||
| 4 | −0.01 | −0.01 | 0.537 | ||||
| 4 | Median (IR) Mean (SD) | 0.78 (0.06) 0.80 (0.09) | 1 | 0.03 | 0.05 | 0.005 | 0.001 |
| 2 | 0.02 | 0.03 | 0.083 | ||||
| 3 | 0.01 | 0.01 | 0.537 |
| Variables | Do not Engage in Physical Activity (N = 72) | Do Engage in Physical Activity (N = 424) | p * |
|---|---|---|---|
| KS9 | |||
| Median (IR) | 4.44 (0.56) | 4.61 (0.55) | 0.003 |
| Mean (SD) | 4.37 (0.45) | 4.54 (0.39) | |
| MAPPING CHU9D | |||
| Median (IR) | 0.75 (0.10) | 0.78 (0.08) | 0.002 |
| Mean (SD) | 0.76 (0.07) | 0.78 (0.06) |
| Variable | PA |
|---|---|
| KS9 | rho |
| TOTAL | 0.151 ** |
| BOYS | 0.148 * |
| 8–12 | 0.143 * |
| 13–14 | 0.214 * |
| GIRLS | 0.177 ** |
| 8–12 | 0.133 |
| 13–14 | 0.291 * |
| MAPPING CHU9D | rho |
| TOTAL | 0.146 ** |
| BOYS | 0.178 ** |
| 8–12 | 0.197 ** |
| 13–14 | 0.109 * |
| GIRLS | 0.143 * |
| 8–12 | 0.062 |
| 13–14 | 0.441 ** |
| Questions | Spearman’s Correlation Coefficient | p |
|---|---|---|
| Has your child felt fit and well? | 0.133 * | 0.003 |
| Has your child felt full of energy? | 0.134 * | 0.003 |
| Has your child felt sad? | −0.041 | 0.528 |
| Has your child felt lonely? | −0.045 | 0.329 |
| Has your child had enough time for him/herself? | 0.019 | 0.667 |
| Has your child been able to do the things that he/she wants to do in his/her free time? | 0.064 | 0.152 |
| Has your child had fun with his/her friends? | 0.155 ** | 0.001 |
| Has your child got on well at school? | 0.091 * | 0.044 |
| Has your child been able to pay attention? | 0.072 | 0.107 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gallego-Méndez, J.; Perez-Gomez, J.; Calzada-Rodríguez, J.I.; Denche-Zamorano, Á.M.; Mendoza-Muñoz, M.; Carlos-Vivas, J.; Garcia-Gordillo, M.Á.; Adsuar, J.C. Relationship between Health-Related Quality of Life and Physical Activity in Children with Hyperactivity. Int. J. Environ. Res. Public Health 2020, 17, 2804. https://doi.org/10.3390/ijerph17082804
Gallego-Méndez J, Perez-Gomez J, Calzada-Rodríguez JI, Denche-Zamorano ÁM, Mendoza-Muñoz M, Carlos-Vivas J, Garcia-Gordillo MÁ, Adsuar JC. Relationship between Health-Related Quality of Life and Physical Activity in Children with Hyperactivity. International Journal of Environmental Research and Public Health. 2020; 17(8):2804. https://doi.org/10.3390/ijerph17082804
Chicago/Turabian StyleGallego-Méndez, Julio, Jorge Perez-Gomez, José Ignacio Calzada-Rodríguez, Ángel Manuel Denche-Zamorano, María Mendoza-Muñoz, Jorge Carlos-Vivas, Miguel Ángel Garcia-Gordillo, and Jose C. Adsuar. 2020. "Relationship between Health-Related Quality of Life and Physical Activity in Children with Hyperactivity" International Journal of Environmental Research and Public Health 17, no. 8: 2804. https://doi.org/10.3390/ijerph17082804
APA StyleGallego-Méndez, J., Perez-Gomez, J., Calzada-Rodríguez, J. I., Denche-Zamorano, Á. M., Mendoza-Muñoz, M., Carlos-Vivas, J., Garcia-Gordillo, M. Á., & Adsuar, J. C. (2020). Relationship between Health-Related Quality of Life and Physical Activity in Children with Hyperactivity. International Journal of Environmental Research and Public Health, 17(8), 2804. https://doi.org/10.3390/ijerph17082804










