Association Rule Learning Is an Easy and Efficient Method for Identifying Profiles of Traumas and Stressors that Predict Psychopathology in Disaster Survivors: The Example of Sri Lanka
Abstract
1. Introduction
2. Method
2.1. Participants
2.2. Measures
3. Data Analysis
3.1. Conversion of WRPBP Items of the PRPWPQ into Discrete Variables
- (1)
- Some anxiety: Respondents whose average score on the items in the anxiety subscale of the WRPBP section of the PRPWPQ was 2 (a little bit) or greater were considered to have at least some anxiety.
- (2)
- Severe anxiety: Respondents whose average score on the items on the anxiety subscale of the WRPBP section of the PRPWPQ was 3 (quite a bit) or greater were considered to have severe anxiety.
- (3)
- Some depression: Respondents whose average score on the items on the depression subscale of the WRPBP section of the PRPWPQ was 2 (a little bit) or greater were considered to have at least some depressive symptoms.
- (4)
- Severe depression: Respondents whose average score on the items on the depression subscale of the WRPBP section of the PRPWPQ was 3 (quite a bit) or greater were considered to have severe depression.
3.2. Percentage of Individuals who Experienced Specific Traumas and Stressful Life Events and are Currently Experiencing Anxiety and Depression
3.3. Identifying Association Rules
- (1)
- maximum rule length is 5;
- (2)
- Support for the rules is larger than ;
- (3)
- Confidence for the rules is larger than .
4. Results
4.1. Trauma Exposure
4.2. Stressful Life Events
4.3. Anxiety and Depression
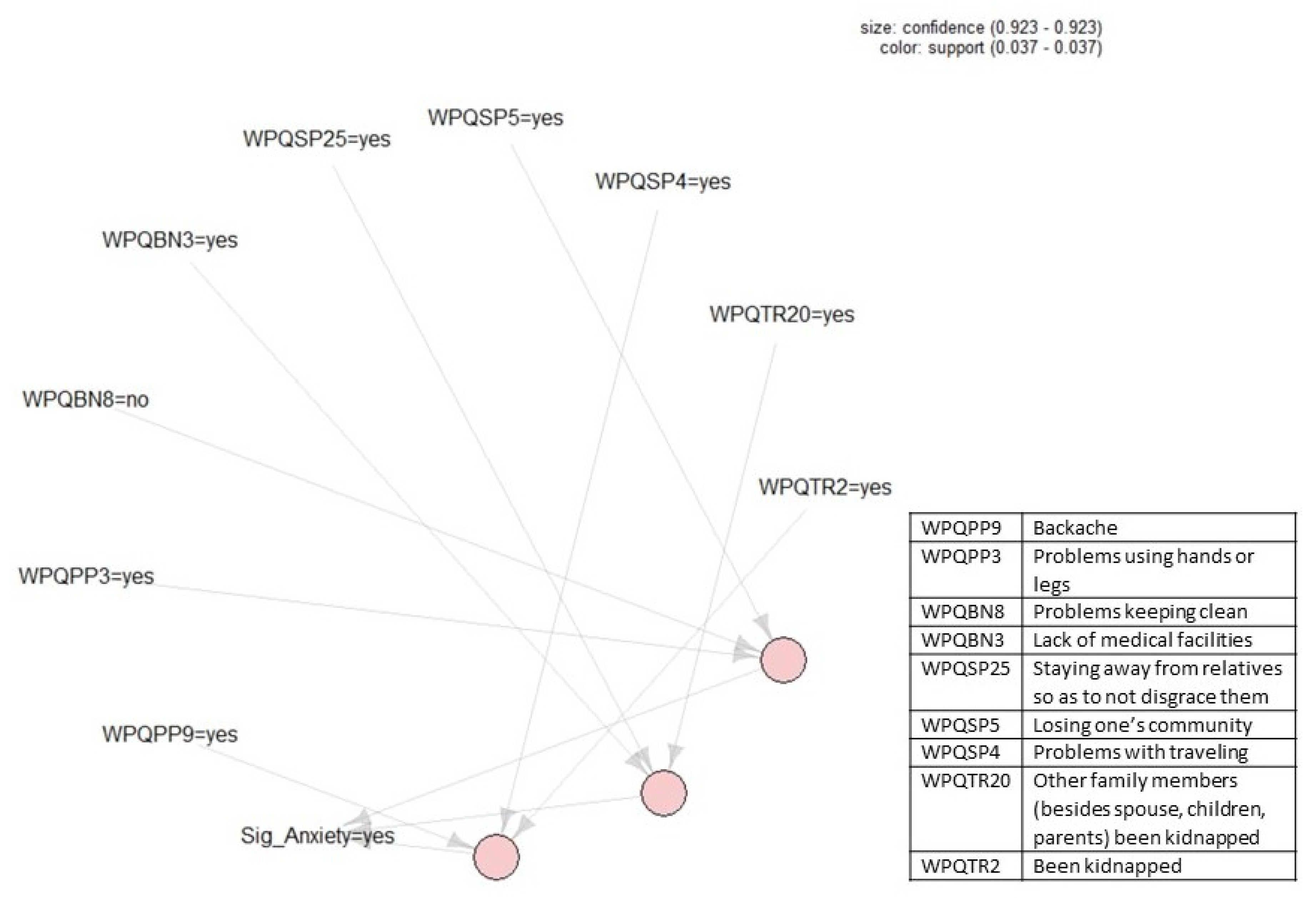
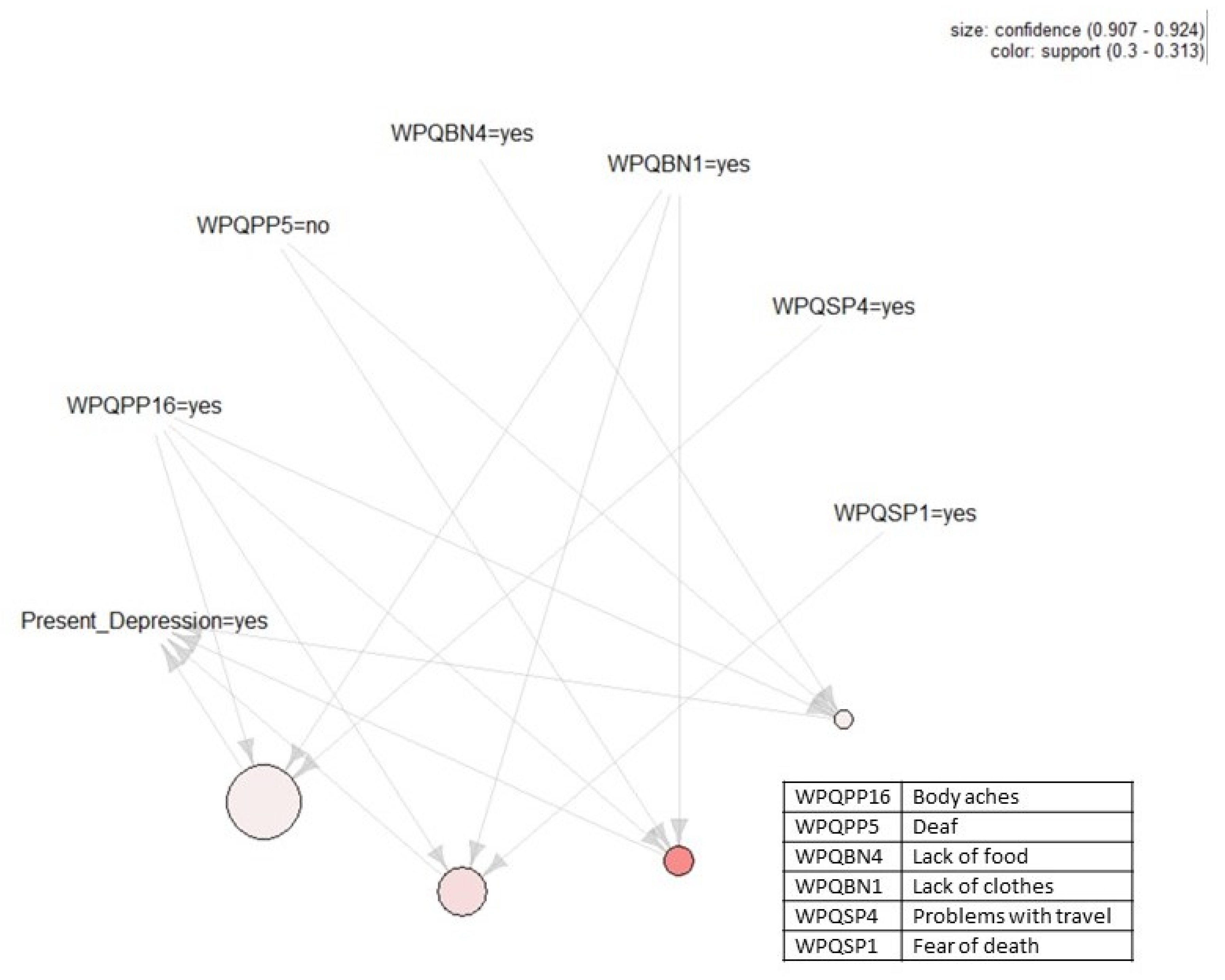
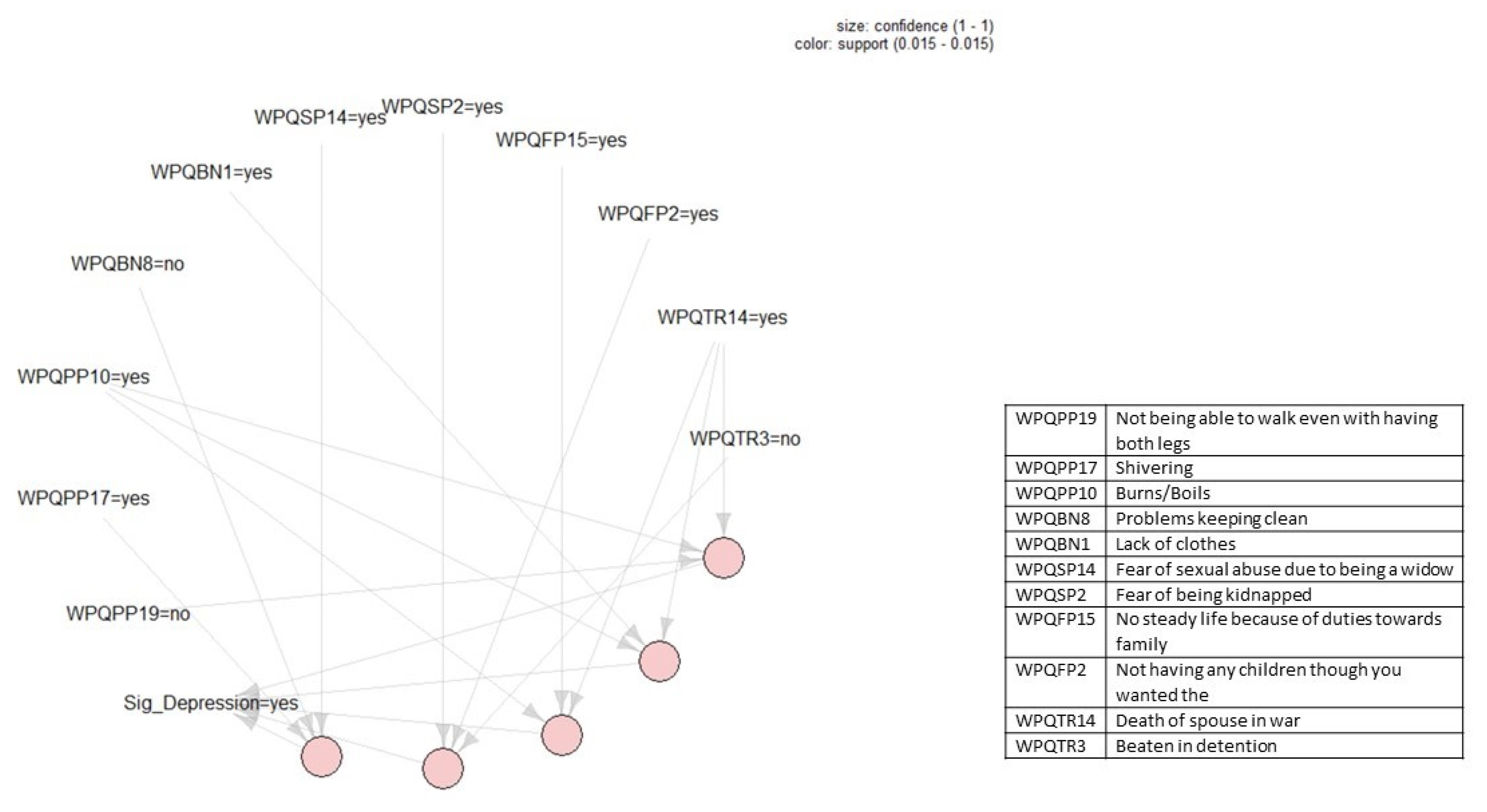
4.4. Association Rules
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- United Nations High Commissioner for Refugees. Global Trends: Forced Displacement in 2018; United Nations High Commissioner for Refugees: Geneva, Switzerland, 2019. [Google Scholar]
- Bogic, M.; Njoku, A.; Priebe, S. Long-term mental health of war-refugees: A systematic literature review. BMC Int. Health Hum. Rights 2015, 15, 29. [Google Scholar] [CrossRef]
- Morina, N.; Akhtar, A.; Barth, J.; Schnyder, U. Psychiatric disorders in refugees and internally displaced persons after forced displacement: A systematic review. Front. Psychiatry 2018, 9, 433. [Google Scholar] [CrossRef]
- Mollica, R.F. Healing Invisible Wounds: Paths to Hope and Recovery in a Violent World; Harcourt: Orlando, FL, USA, 2008. [Google Scholar]
- Neuner, F. Assisting war-torn populations–Should we prioritize reducing daily stressors to improve mental health? Comment of Miller and Rasmussen (2010). Soc. Sci. Med. 2010, 71, 1381–1384. [Google Scholar] [CrossRef]
- Silove, D. The ADAPT model: A conceptual framework for mental health and psychosocial programming in post conflict settings. Intervention 2013, 11, 237–248. [Google Scholar] [CrossRef]
- Miller, K.E.; Rasmussen, A. War exposure, daily stressors, and mental health in conflict and post-conflict settings: Bridging the divide between trauma focused and psychosocial frameworks. Soc. Sci. Med. 2010, 70, 7–16. [Google Scholar] [CrossRef]
- Miller, K.E.; Rasmussen, A. War experiences, daily stressors and mental health five years on: Elaborations and future directions. Intervention 2014, 12, 33–42. [Google Scholar] [CrossRef]
- Miller, K.; Rasmussen, A. The mental health of civilians displaced by armed conflict: An ecological model of refugee distress. Epidemiol. Psychiatr. Sci. 2017, 26, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Kai, H.W.; Huinan, L.; Li, L.; Jeffery, H.; Hyojin, K.; Seong, E.; Bonnano, G.A.; Hobfoll, S.E.; Hall, B.J. Everyday life experiences and mental health among conflict-affected forced migrants: A meta-analysis. J. Affect. Disor. 2020, 264, 50–68. [Google Scholar]
- Medicins Sans Frontieres. Mental Health Guidelines–A Handbook for Implementing Mental Health Programmes in Areas of Mass Violence; Lightning Source UK; Medicins Sans Frontieres: Amsterdam, The Netherlands, 2005. [Google Scholar]
- Inter-Agency Standing Committee (IASC). IASC Guidelines on Mental Health and Psychosocial Support. in Emergency Settings; IASC: Geneva, Switzerland, 2006. [Google Scholar]
- Fernando, G.A.; Miller, K.E.; Berger, D.E. Growing pains: The impact of disaster-related and daily stressors on the psychological and psychosocial functioning of youth in Sri Lanka. Child. Dev. 2020, 81, 1192–1210. [Google Scholar] [CrossRef] [PubMed]
- Jordans, M.J.D.; Semrau, M.; Thornicroft, G.; van Ommeren, M. Role of current perceived needs in explaining the association between past trauma exposure and distress in humanitarian settings in Jordan and Nepal. Br. J. Psychiatry 2014, 201, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Newnham, E.A.; Pearson, R.M.; Stein, A.; Betancourt, T.S. Youth mental health after civil war: The importance of daily stressors. Br. J. Psychiatry 2015, 206, 116–121. [Google Scholar] [CrossRef]
- Rasmussen, A.; Nguyen, L.; Wilkinson, J.; Vundla, S.; Raghavan, S.; Miller, K.E.; Keller, A.S. Rates and impact of trauma and current stressors among Darfuri refugees in Eastern Chad. Am. J. Orthopsychiatry 2010, 80, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Chen, E.E.; Wojcik, S.P. A practical guide to big data research in Psychology. Psychol. Methods 2016, 4, 458–474. [Google Scholar] [CrossRef] [PubMed]
- De Schryver, M.; Vindevogel, S.; Rasmussen, A.E.; Cramer, A.O. Unpacking constructs: A network approach for studying war exposure, daily stressors and post-traumatic stress disorder. Front. Psychol. 2015, 6, 1896. [Google Scholar] [CrossRef] [PubMed]
- Jayawickreme, N.; Mootoo, C.; Fountain, C.; Rasmussen, A.; Jayawickreme, E.; Bertuccio, R.F. Post-conflict struggles as networks of problems: A network analysis of trauma, daily stressors and psychological distress among Sri Lankan war survivors. Soc. Sci. Med. 2017, 190, 119–132. [Google Scholar] [CrossRef]
- Mootoo, C.; Fountain, C.; Rasmussen, A. Formative psychosocial evaluation using dynamic networks: Trauma, stressors, and distress among Darfur refugees living in Chad. Confl. Health 2019, 13, 30. [Google Scholar] [CrossRef]
- Agrawal, R.; Imielinski, T.; Swami, A. Mining association rules between sets of items in large databases. In Proceedings of the 1993 ACM SIGMOD International Conference on Management of Data, Washington, DC, USA, 26–28 May 1993; Buneman, P., Jajodia, S., Eds.; pp. 207–216. [Google Scholar]
- Chen, Y.-L.; Tang, K.; Shen, R.-J.; Hu, Y.-H. Market basket analysis in a multiple store environment. Decis Support. Syst. 2005, 40, 339–354. [Google Scholar] [CrossRef]
- Agrawal, R.; Srikant, R. Fast algorithms for mining association rules. In Proceedings of the 20th VLDB Conference, Santiago, Chile, 12–15 September 1994; pp. 478–499. [Google Scholar]
- Rand, W.M. Objective Criteria for the Evaluation of Clustering Methods. J. Am. Stat. Assoc. 1971, 66, 846–850. [Google Scholar] [CrossRef]
- Fried, E.I.; Cramer, A.O.J. Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspect. Psychol. Sci. 2017, 12, 999–1020. [Google Scholar] [CrossRef]
- Jayawickreme, N.; Rasmussen, A.; Karasz, A.; Verkuilen, J.; Jayawickreme, E. Network models can help focus research on the role of culture and context in psychopathology, but don’t discount latent variable models. Behav. Brain Sci. 2019, 42, e14. [Google Scholar] [CrossRef]
- Forbes, M.K.; Wright, A.G.C.; Markon, K.E.; Kruger, R.F. Evidence that psychopathology symptom networks have limited replicability. J. Abnorm. 2017, 126, 969–988. [Google Scholar] [CrossRef] [PubMed]
- Bringmann, L.F.; Elmer, T.; Epskamp, S.; Krause, R.W.; Schoch, D.; Wichers, M.; Wigman, J.T.W.; Snippe, E. What do centrality measures measure in psychological networks? J. Abnorm. 2019, 128, 892–903. [Google Scholar] [CrossRef] [PubMed]
- Jayawickreme, E.; Jayawickreme, N.; Miller, E. Triumphalism, fear and humiliation: The psychological legacy of Sri Lanka’s civil war. Dyn. Asymmetric Confl. 2010, 3, 208–222. [Google Scholar] [CrossRef]
- Vhurumuku, E.; Nanayakkara, L.; Petersson, A.; Kumarasiri, R.H.W.A.; Rupasena, L.P. Food Security in the Northern and Eastern Provinces of Sri Lanka; United Nations World Food Program: Colombo, Sri Lanka, 2012. [Google Scholar]
- Harrison, F. Still Counting the Dead: Survivors of Sri Lanka’s Hidden War; Portobello: London, UK, 2012. [Google Scholar]
- Jayawickreme, N.; Jayawickreme, E.; Goonesekara, M.; Foa, E.B. Distress, well-being and war: Qualitative analyses of civilian interviews from north-eastern Sri Lanka and validation of culturally- sensitive measures of well-being and distress. Intervention 2009, 7, 204–222. [Google Scholar] [CrossRef]
- Jayawickreme, N.; Jayawickreme, E.; Atanasov, P.; Goonasekera, M.A.; Foa, E.B. Are Culturally Specific Measures of Trauma-Related Anxiety and Depression Needed? The Case of Sri Lanka. Psychol. Assess. 2012, 24, 791–800. [Google Scholar] [CrossRef]
- Rudin, C. Stop explaining black box machine learning models for high stakes decisions and use interpretable models instead. Nat. Mach. Intell. 2019, 1, 206–215. [Google Scholar] [CrossRef]
- The WHO World Mental Health Survey Consortium. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 2004, 291, 2581–2590. [Google Scholar] [CrossRef]
- Ruzek, J.I.; Yeager, C.M. Internet and mobile technologies: Addressing the mental health of trauma survivors in less resources communities. Confl. Health 2017, 4, e16. [Google Scholar] [CrossRef]
- Murray, S.M.; Kass, N.; Mendelson, T.; Bass, J. The ethics of mental health survey research in low-and middle-income countries. Confl. Health 2016, 3, e12. [Google Scholar] [CrossRef]

| Percentage | % |
|---|---|
| Witnessed the injury of loved ones | 47.5 |
| Witnessed the death of loved ones | 44.5 |
| Beaten in detention | 36.5 |
| Been imprisoned | 35.9 |
| Family members (besides spouse, children, parents) been kidnapped | 17.5 |
| Injured by airstrikes or bomb explosions or sudden attacks | 15.4 |
| Been kidnapped | 12.5 |
| Tortured by being beaten with a bag containing petrol | 11.9 |
| Children been kidnapped | 11.6 |
| Death of child/children in war | 11.3 |
| Death of spouse in war | 9.2 |
| Children been handicapped | 9.2 |
| Tortured by being pricked under the nail with a pin | 9.2 |
| Death of mother and/or father in war | 8.9 |
| Tortured by being burnt with a cigarette butt in detention | 8.6 |
| Electrocuted in detention | 7.7 |
| Husband or wife been kidnapped | 7.7 |
| Husband or wife been handicapped | 5.6 |
| Tortured by being forcibly fed mosquito coil | 4.2 |
| Caught in a land mine | 3.3 |
| Parent(s) been kidnapped | 2.4 |
| Been raped | 1.2 |
| Percentage | % |
|---|---|
| Family Problems | |
| Insufficient support from relatives | 48.7 |
| Children/spouse has psychological problems | 47.2 |
| No steady life because of duties towards family | 46.6 |
| Unable to take care of children | 36.2 |
| Having been separated from husband/wife/children/other relatives | 28.5 |
| Unable to get children married/give dowry | 26.7 |
| Not being able to travel to meet relatives due to travel restrictions | 26.4 |
| Not having anyone to take care of you in old age | 23.7 |
| Being dependent on relatives | 22.6 |
| Problems with husband/wife at home | 22.6 |
| Taking care of your children and siblings as a single person | 20.5 |
| Problems between children | 20.2 |
| Unable to control (i.e., discipline) your children | 18.4 |
| Problems with marriage plans | 11 |
| Alcohol abuse by self | 9.2 |
| Alcohol abuse by husband or wife | 7.4 |
| Not having any children though you wanted them | 7.4 |
| Being dependent on wife | 7.4 |
| Alcohol abuse by parents | 4.2 |
| Not being properly looked after or cared for by children | 0.6 |
| Economic Problems | |
| Not being able to earn enough money for your basic needs | 89.3 |
| Not having money | 86.1 |
| Loss of material goods | 84.9 |
| Unavailability of employment | 83.1 |
| Not being able to work due to illness | 83.1 |
| Financial debt | 82.8 |
| Not being able to do the job you desire | 81 |
| Loss of house/land | 77.2 |
| Loss of work equipment | 73 |
| Not beingable to work due to being a single parent | 52.2 |
| Social Problems | |
| Fear of death (from bombs/ land mines/armed groups) | 65.6 |
| Problems with travel | 57 |
| Stress when moving to a new place | 51.3 |
| Not being able to do usual routines after having moved to a new place | 49.9 |
| Fear of being kidnapped | 49.3 |
| Not being able to talk freely | 46 |
| Not having offical documents | 33.5 |
| Losing one’s community | 30 |
| Living with relatives | 25.5 |
| Unable to participate in cultural events | 21.1 |
| Living alone (without anyone) | 20.8 |
| Having to give bribes to get basic services | 16.9 |
| Not being respected by society | 16.6 |
| Lack of security due to being alone | 16.3 |
| Staying away from relatives so not to disgrace them | 16.3 |
| Isolated in society due to unemployment | 13.1 |
| Been a victim of theft | 12.2 |
| Isolated in society due to history of being imprisoned | 11.9 |
| Living in a camp | 11 |
| Neglected by society | 10.7 |
| Living with non-relatives | 9.8 |
| Not being able to get married | 7.4 |
| Isolated from society due to being a widow | 7.1 |
| Problems with neighors or others in the camp | 6.2 |
| Fear of sexual abuse due to being a widow | 5.9 |
| Unable to get married due to stigma | 3.3 |
| Lack of Basic Needs | |
| Lack of proper security | 62.3 |
| Losing your rights | 59.9 |
| Lack of medical facilities | 59.9 |
| Lack of food | 54.9 |
| Lack of clothes | 53.4 |
| Lack of fuel | 49 |
| Not being able to obtain education | 40.1 |
| Lack of water | 34.4 |
| Problems keeping clean | 30.9 |
| Physical Problems | |
| Body aches | 62.6 |
| Headaches | 64.4 |
| Backache | 57.9 |
| Shivering | 41.8 |
| Eye problems | 33.5 |
| High blood pressure | 22 |
| Problems using hands or legs | 21.1 |
| Loss of teeth | 17.8 |
| Not being able to walk even with having both legs | 16 |
| Heart problems | 15.7 |
| Burns/boils | 15.4 |
| Fractures | 14.8 |
| Deaf | 10.1 |
| Head injury | 10.1 |
| Retention of bullet or bomb particles in the body | 9.5 |
| Loss of arms or legs in a landmine | 6.2 |
| Kidney problems | 7.1 |
| Stroke/blood clots | 6.8 |
| Loss of arms or legs of a child or spouse or breadwinner due to a landmine | 4.2 |
| Percentage | % |
|---|---|
| Some Anxiety | 67.1 |
| Severe Anxiety | 21.4 |
| Some Depression | 63.8 |
| Severe Depression | 15.1 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jayawickreme, N.; Atefi, E.; Jayawickreme, E.; Qin, J.; Gandomi, A.H. Association Rule Learning Is an Easy and Efficient Method for Identifying Profiles of Traumas and Stressors that Predict Psychopathology in Disaster Survivors: The Example of Sri Lanka. Int. J. Environ. Res. Public Health 2020, 17, 2850. https://doi.org/10.3390/ijerph17082850
Jayawickreme N, Atefi E, Jayawickreme E, Qin J, Gandomi AH. Association Rule Learning Is an Easy and Efficient Method for Identifying Profiles of Traumas and Stressors that Predict Psychopathology in Disaster Survivors: The Example of Sri Lanka. International Journal of Environmental Research and Public Health. 2020; 17(8):2850. https://doi.org/10.3390/ijerph17082850
Chicago/Turabian StyleJayawickreme, Nuwan, Ehsan Atefi, Eranda Jayawickreme, Jiale Qin, and Amir H. Gandomi. 2020. "Association Rule Learning Is an Easy and Efficient Method for Identifying Profiles of Traumas and Stressors that Predict Psychopathology in Disaster Survivors: The Example of Sri Lanka" International Journal of Environmental Research and Public Health 17, no. 8: 2850. https://doi.org/10.3390/ijerph17082850
APA StyleJayawickreme, N., Atefi, E., Jayawickreme, E., Qin, J., & Gandomi, A. H. (2020). Association Rule Learning Is an Easy and Efficient Method for Identifying Profiles of Traumas and Stressors that Predict Psychopathology in Disaster Survivors: The Example of Sri Lanka. International Journal of Environmental Research and Public Health, 17(8), 2850. https://doi.org/10.3390/ijerph17082850






