Factors Affecting Treatment with Life-Saving Interventions, Computed Tomography Scans and Specialist Consultations
Abstract
1. Introduction
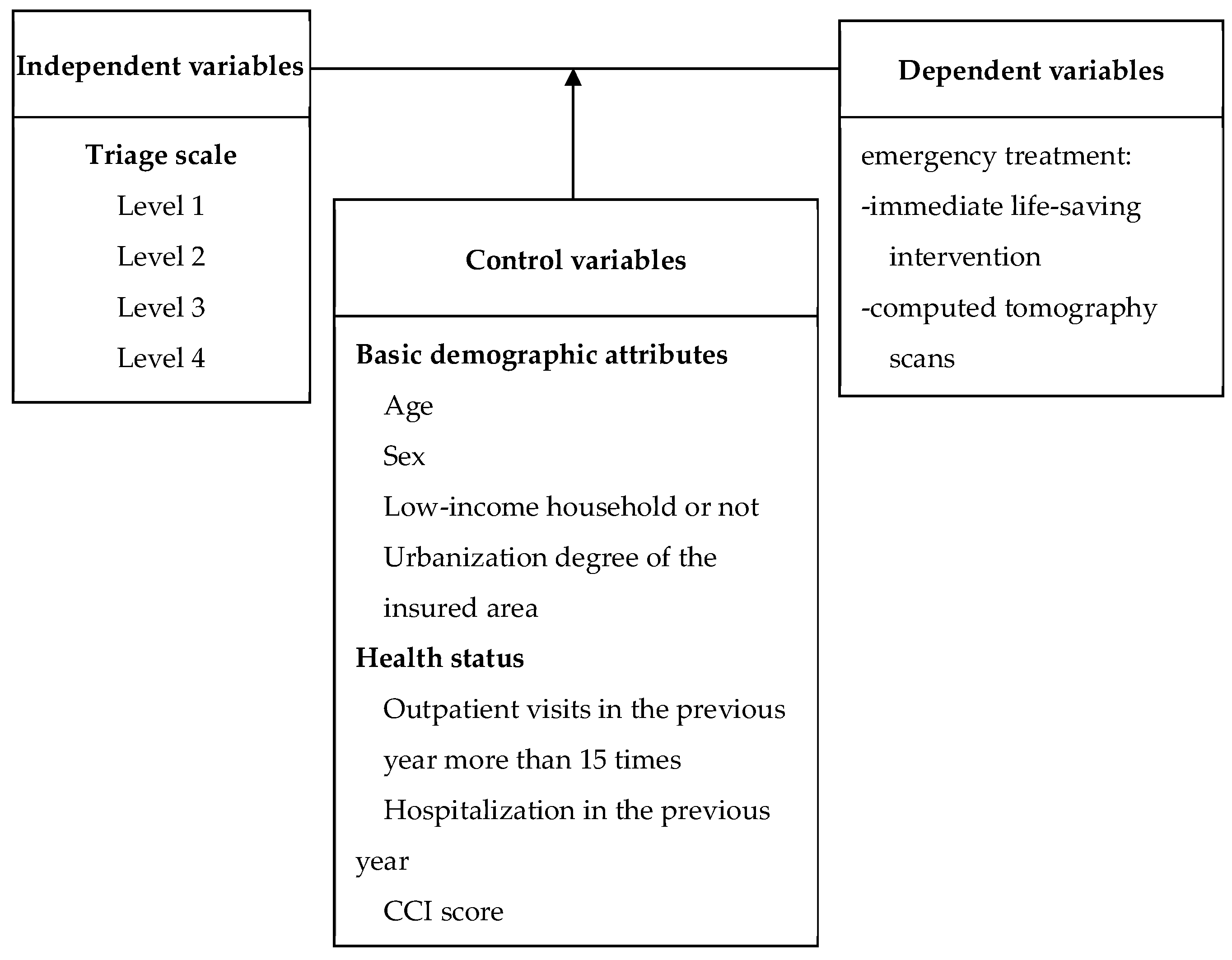
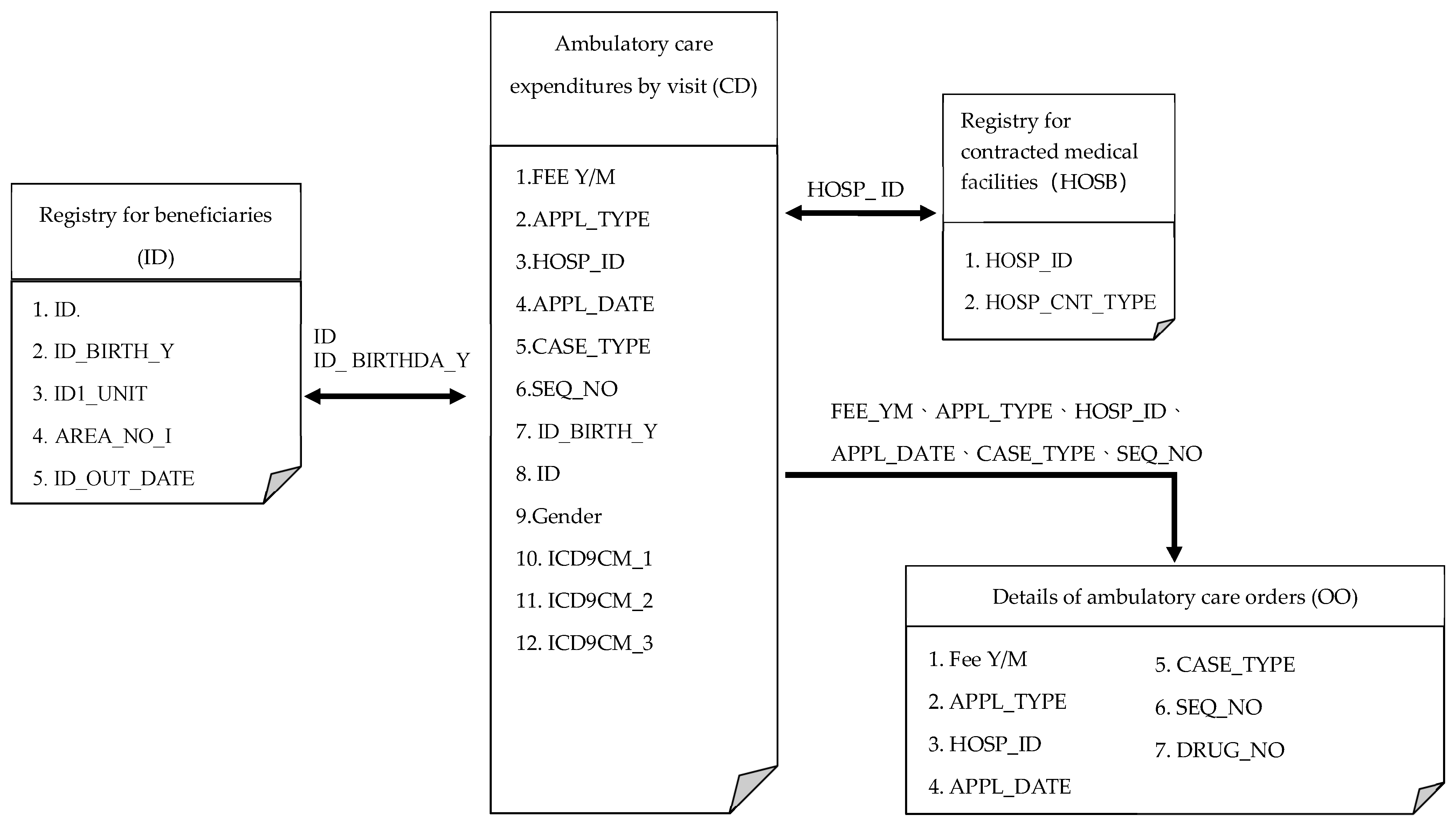
2. Research Methods
3. Results
4. Discussion
5. Limitation
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Eskander, A.; Krzyzanowska, M.K.; Fischer, H.D.; Liu, N.; Austin, P.C.; Irish, J.C.; Raphael, M. Emergency department visits and unplanned hospitalizations in the treatment period for head and neck cancer patients treated with curative intent: A population-based analysis. Oral Oncol. 2018, 83, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Vranas, K.C.; Lin, A.L.; Zive, D.; Tolle, S.W.; Halpern, S.D.; Slatore, C.G.; Sullivan, D.R. The Association of physician orders for life-sustaining treatment with intensity of treatment among patients presenting to the emergency department. Ann. Emerg. Med. 2020, 75, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Reay, G.; Smith-MacDonald, L.; Then, K.L.; Hall, M.; Rankin, J.A. Triage emergency nurse decision-making: Incidental findings from a focus group study. Int. Emerg. Nurs. 2020, 48, 100791. [Google Scholar] [CrossRef] [PubMed]
- Yau, F.F.F.; Tsai, T.C.; Lin, Y.R.; Wu, K.H.; Syue, Y.J.; Li, C.J. Can different physicians providing urgent and non-urgent treatment improve patient flow in emergency department? Am. J. Emerg. Med. 2018, 36, 993–997. [Google Scholar] [CrossRef] [PubMed]
- McNamara, R.L.; Wang, Y.; Herrin, J.; Curtis, J.P.; Bradley, E.H.; Magid, D.J.; NRMI Investigators. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J. Am. Coll. Cardiol. 2006, 47, 2180–2186. [Google Scholar] [CrossRef]
- DeVon, H.A.; Hogan, N.; Ochs, A.L.; Shapiro, M. Time to treatment for acute coronary syndromes: The cost of indecision. J. Cardiovasc. Nurs. 2010, 25, 106. [Google Scholar] [CrossRef]
- Gausche-Hill, M.; Schmitz, C.; Lewis, R.J. Pediatric preparedness of US emergency departments: A 2003 survey. Pediatrics 2007, 120, 1229–1237. [Google Scholar] [CrossRef]
- Brown, C.A., III; Bair, A.E.; Pallin, D.J.; Walls, R.M.; NEAR III Investigators. Techniques, success, and adverse events of emergency department adult intubations. Ann. Emerg. Med. 2015, 65, 363–370. [Google Scholar] [CrossRef]
- Lodwick, D.L.; Cooper, J.N.; Lawrence, A.E.; Kelleher, K.J.; Minneci, P.C.; Deans, K.J. Factors Affecting Emergency Department Computed Tomography Use in Children. J. Surg. Res. 2019, 241, 294–301. [Google Scholar] [CrossRef]
- Levin, D.C.; Rao, V.M.; Parker, L.; Frangos, A.J. Continued growth in emergency department imaging is bucking the overall trends. J. Am. Coll. Radiol. 2014, 11, 1044–1047. [Google Scholar] [CrossRef]
- Broder, J.; Fordham, L.A.; Warshauer, D.M. Increasing utilization of computed tomography in the pediatric emergency department, 2000–2006. Emerg. Radiol. 2007, 14, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Lehtimäki, T.T.; Kärkkäinen, J.M.; Saari, P.; Manninen, H.; Paajanen, H.; Vanninen, R. Detecting acute mesenteric ischemia in CT of the acute abdomen is dependent on clinical suspicion: Review of 95 consecutive patients. Eur. J. Radiol. 2015, 84, 2444–2453. [Google Scholar] [CrossRef] [PubMed]
- Tilsed, J.V.T.; Casamassima, A.; Kurihara, H.; Mariani, D.; Martinez, I.; Pereira, J.; D’Almeida, A.J.G. ESTES guidelines: Acute mesenteric ischaemia. Eur. J. Trauma Emerg. Surg. 2016, 42, 253–270. [Google Scholar] [CrossRef]
- Björck, M.; Koelemay, M.; Acosta, S.; Goncalves, F.B.; Kölbel, T.; Kolkman, J.J.; Kolh, P. Editor’s choice–management of the diseases of mesenteric arteries and veins: Clinical practice guidelines of the European Society of Vascular Surgery (ESVS). Eur. J. Vasc. Endovasc. Surg. 2017, 53, 460–510. [Google Scholar] [CrossRef] [PubMed]
- Woods, R.A.; Lee, R.; Ospina, M.B.; Blitz, S.; Lari, H.; Bullard, M.J.; Rowe, B.H. Consultation outcomes in the emergency department: Exploring rates and complexity. Can. J. Emerg. Med. 2008, 10, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Nelson, K.A.; Boslaugh, S.E.; Hodge, D. Risk factors for extremely long length-of-stay among pediatric emergency patients. Pediatr. Emerg. Care 2009, 25, 835–840. [Google Scholar] [CrossRef] [PubMed]
- Adler, D.; Abar, B.; Durham, D.D.; Bastani, A.; Bernstein, S.L.; Baugh, C.W.; Hudson, M.F. Validation of the emergency severity index (Version 4) for the triage of adult emergency department patients with active cancer. J. Emerg. Med. 2019, 57, 354–361. [Google Scholar] [CrossRef]
- Polivka, B.J.; Nickel, J.T.; Salsberry, P.J.; Kuthy, R.; Shapiro, N.; Slack, C. Hospital and emergency department use by young low-income children. Nurs. Res. 2000, 49, 253–261. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. The Historical Data of Minimum Living Expense. Available online: https://dep.mohw.gov.tw/dosaasw/cp-566-45261-103.html (accessed on 12 March 2020).
- Ministry of Health and Welfare. National Health Insurance Annual Report. Available online: http://www.nhi.gov.tw/resource/Webdata/2018-19%E5%85%A8%E6%B0%91%E5%81%A5%E5%BA%B7%E4%BF%9D%E9%9A%AA%E5%B9%B4%E5%A0%B1.pdf (accessed on 12 March 2020).
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Deyo, R.A.; Cherkin, D.C.; Ciol, M.A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 1992, 45, 613–619. [Google Scholar] [CrossRef]
- Chang, E.T.; Lin, C.L.; Chen, S.F.; Hsu, C.Y.; Shen, Y.C. Risk of bone fractures in patients with narcolepsy: A nationwide population-based cohort study. Sleep Med. 2020, 70, 55–59. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.C.; Hsu, H.K.; Lai, T.S.; Chiang, W.C.; Lin, S.L.; Chen, Y.M.; Chu, T.S. Emergency department utilization and resuscitation rate among patients receiving maintenance hemodialysis. J. Formos. Med. Assoc. 2019, 118, 1652–1660. [Google Scholar] [CrossRef] [PubMed]
- Ko, M.C.; Lien, H.Y.; Woung, L.C.; Chen, C.Y.; Chen, Y.L.; Chen, C.C. Difference in frequency and outcome of geriatric emergency department utilization between urban and rural areas. J. Chin. Med. Assoc. 2019, 82, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.L.; Hsu, Y.H.; Su, W.L.; Damayanti, N.A.; Chen, C.W.; Lin, Y.J.; Tsai, K.S.; Li, C.Y. Urban-rural disparity of preventive healthcare utilization among children under the universal health insurance coverage in Taiwan: A national birth cohort analysis. Public Health 2020, 182, 102–109. [Google Scholar] [CrossRef]
- Beckmann, K.R.; Melzer-Lange, M.D.; Gorelick, M.H. Emergency department management of sexually transmitted infections in US adolescents: Results from the National Hospital Ambulatory Medical Care Survey. Ann. Emerg. Med. 2004, 43, 333–338. [Google Scholar] [CrossRef]
- Bell, C.N.; Walton, Q.L.; Thomas, C.S. Race and income moderate the association between depressive symptoms and obesity. Prev. Med. 2019, 119, 1–6. [Google Scholar] [CrossRef]
- Carney, R.M.; Freedland, K.E.; Miller, G.E.; Jaffe, A.S. Depression as a risk factor for cardiac mortality and morbidity: A review of potential mechanisms. J. Psychosom. Res. 2002, 53, 897–902. [Google Scholar] [CrossRef]
- Flegal, K.M.; Kit, B.K.; Orpana, H.; Graubard, B.I. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA 2013, 309, 71–82. [Google Scholar] [CrossRef]
- Samaras, N.; Chevalley, T.; Samaras, D.; Gold, G. Older patients in the emergency department: A review. Ann. Emerg. Med. 2010, 56, 261–269. [Google Scholar] [CrossRef]
- Marengoni, A.; Angleman, S.; Melis, R.; Mangialasche, F.; Karp, A.; Garmen, A.; Fratiglioni, L. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 2011, 10, 430–439. [Google Scholar] [CrossRef]
- Vogeli, C.; Shields, A.E.; Lee, T.A.; Gibson, T.B.; Marder, W.D.; Weiss, K.B.; Blumenthal, D. Multiple chronic conditions: Prevalence, health consequences, and implications for quality, care management, and costs. J. Gen. Intern. Med. 2007, 22, 391–395. [Google Scholar] [CrossRef] [PubMed]
- Kirves, H.; Handolin, L.; Niemelä, M.; Pitkäniemi, J.; Randell, T. Paramedics’ and pre-hospital physicians’ assessments of anatomic injury in trauma patients: A cohort study. Scand. J. Trauma Resusc. Emerg. Med. 2010, 18, 60. [Google Scholar] [CrossRef] [PubMed]
- Asplin, B.R.; Magid, D.J.; Rhodes, K.V.; Solberg, L.I.; Lurie, N.; Camargo, C.A., Jr. A conceptual model of emergency department crowding. Ann. Emerg. Med. 2003, 42, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Rao, M.B.; Lerro, C.; Gross, C.P. The shortage of on-call surgical specialist coverage: A national survey of emergency department directors. Acad. Emerg. Med. 2010, 17, 1374–1382. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, S.A.; Washington, D.L.; Lambe, S.; Fink, A.; Asch, S.M. Predictors of on-call specialist response times in California emergency departments. Acad. Emerg. Med. 2006, 13, 505–512. [Google Scholar] [CrossRef] [PubMed]
| Variables | Number of Patients (n = 138,713) | % | p Value |
|---|---|---|---|
| Basic characteristics | |||
| Patient sex | 0.0036 | ||
| Female | 69,898 | 50.39% | |
| Male | 68,818 | 49.61% | |
| Categories by age | <0.0001 | ||
| 0–18 | 12,060 | 8.69% | |
| 19–64 | 96,620 | 69.65% | |
| ≥ 65 and older | 30,033 | 21.65% | |
| Low-income households | <0.0001 | ||
| Yes | 3163 | 2.28% | |
| No | 135,550 | 97.72% | |
| Urbanization degree | <0.0001 | ||
| Municipal city | 106,036 | 76.44% | |
| Satellite city/town | 22,177 | 15.99% | |
| Village | 10,500 | 7.57% | |
| Health status in the previous year | |||
| Hospitalization in the previous year | <0.0001 | ||
| Yes | 20,450 | 14.74% | |
| No | 118,263 | 85.26% | |
| Number of instances of ambulatory care less than 15 times in the previous year | <0.0001 | ||
| Yes | 72,279 | 52.11% | |
| No | 66,434 | 47.89% | |
| CCI (Charlson Comorbidity Index) score | <0.0001 | ||
| 0 | 88,981 | 64.15% | |
| 1–2 | 37,091 | 26.74% | |
| ≥3 | 12,641 | 9.11% | |
| Level of emergency treatment hospitals | <0.0001 | ||
| Medical center | 40,215 | 28.99% | |
| Regional hospital | 73,361 | 52.89% | |
| Local hospital | 25,137 | 18.12% | |
| Emergency treatment conditions | |||
| Triaged scale | <0.0001 | ||
| Level 1 | 3374 | 2.43% | |
| Level 2 | 14,490 | 10.45% | |
| Level 3 | 89,967 | 64.28% | |
| Level 4 | 29,417 | 21.21% | |
| Level 5 | 2265 | 1.63% | |
| Immediate life-saving intervention | <0.0001 | ||
| Yes | 6977 | 5.03% | |
| No | 131,736 | 94.97% | |
| Computed tomography | <0.0001 | ||
| Yes | 12,304 | 8.87% | |
| No | 126,409 | 91.13% | |
| Specialist consultation | <0.0001 | ||
| Yes | 11,353 | 8.18% | |
| No | 127,360 | 91.82% | |
| Hospitalization after emergency treatment | <0.0001 | ||
| Yes | 19,122 | 13.79% | |
| No | 119,591 | 86.21% | |
| In-hospital mortality | <0.0001 | ||
| Yes | 998 | 0.72% | |
| No | 137,715 | 99.28% |
| Variable Name | Immediate Life-saving Intervention | Computed Tomography | Specialist Consultation | |||
|---|---|---|---|---|---|---|
| AOR (95%CI) | p Value | AOR (95%CI) | p Value | AOR (95%CI) | p Value | |
| Patient- & disease-related factors | ||||||
| Patient sex | ||||||
| Female | 1 | 1 | 1 | |||
| Male | 1.29 [1.22,1.37] | <0.0001 *** | 1.22 [1.18,1.27] | <0.0001 *** | 1.05 [1.01, 1.09] | 0.0149 * |
| Patient age | ||||||
| 0–18 | 1 | 1 | 1 | |||
| 19–64 | 3.85 [3.06,4.83] | <0.0001 *** | 1.81 [ 1.65, 2.00] | <0.0001 *** | 1.45 [ 1.33,1.59] | <0.0001 *** |
| ≥65 | 8.01 [6.35,10.12] | <0.0001 *** | 3.23 [ 2.91, 3.58] | <0.0001 *** | 1.66 [ 1.51,1.83] | <0.0001 *** |
| Low-income households | ||||||
| No | 1.29 [1.07,1.55] | 0.0069 ** | 1.06 [ 0.93,1.21] | 0.4128 | 0.91 [ 0.79,1.05] | 0.2048 |
| Yes | 1 | 1 | 1 | |||
| Urbanization degree in the insured area | ||||||
| Urban | 1 | 1 | 1 | |||
| Satellite towns | 1.09 [1.01,1.18] | 0.0301 * | 1.08 [ 1.02,1.14] | 0.0068 ** | 1.12 [ 1.05,1.18] | 0.0002 *** |
| Villages | 1.08 [0.98,1.20] | 0.1376 | 1.28 [ 1.19,1.37] | <0.0001 *** | 1.22 [ 1.13,1.32] | <0.0001 *** |
| Medical utilization & health status | ||||||
| Hospitalized in the previous year | ||||||
| Yes | 1 | 1 | 1 | |||
| No | 0.69 [0.64,0.73] | <.0001 *** | 1.10 [ 1.04,1.16] | 0.0010 ** | 0.94 [ 0.88,0.99] | 0.0213 * |
| Less than 15 outpatient visits | ||||||
| Yes | 1 | 1 | 1 | |||
| No | 0.95 [0.88,1.02] | 0.1692 | 1.02 [ 0.97,1.06] | 0.5298 | 0.96 [ 0.91,1.00] | 0.0586 |
| CCI score | ||||||
| 0 | 1 | 1 | 1 | |||
| 1–2 | 1.43 [1.33,1.54] | <0.0001 *** | 1.13 [1.08,1.19] | <0.0001 *** | 0.98 [0.93,1.03] | 0.3461 |
| ≥3 | 1.77 [1.61,1.95] | <0.0001 *** | 1.07 [0.99,1.14] | 0.0821 | 1.02 [0.95,1.10] | 0.5559 |
| Health care system-related factors | ||||||
| Level of emergency hospital | ||||||
| Medical center | 1 | 1 | 1 | |||
| Regional hospital | 0.62 [0.59,0.66] | <0.0001 *** | 0.69 [0.66,0.72] | <0.0001 *** | 0.40 [0.39,0.42] | <0.0001 *** |
| Local hospital | 0.56 [0.51,0.62] | <0.0001 *** | 0.45 [0.42,0.48] | <0.0001 *** | 0.12 [0.11,0.13] | <0.0001 *** |
| Emergency triage scale | ||||||
| Level 1 | 68.33 [64.48,74.72] | <0.0001 *** | 2.52 [2.31,2.74] | <0.0001 *** | 1.93 [1.75,2.12] | <0.0001 *** |
| Level 2 | 7.17 [6.72,7.64] | <0.0001 *** | 2.23 [2.13,2.34] | <0.0001 *** | 1.74 [1.65,1.84] | <0.0001 *** |
| Level 3 | 1 | 1 | 1 | |||
| Level 4 | 0.35 [0.31,0.41] | <0.0001 *** | 0.32 [0.29,0.34] | <0.0001 *** | 0.60 [0.57,0.64] | <0.0001 *** |
| Level 5 | 0.48 [0.31,0.75] | 0.0013 ** | 0.24 [0.18,0.33] | <0.0001 *** | 0.47 [0.37,0.59] | <0.0001 *** |
| Accredited level | Hospitals | Physicians | General ED beds | Psychiatric ED beds | CT |
|---|---|---|---|---|---|
| Academic medical centers | 22 | 13,094 | 21,693 | 1035 | 93 |
| Quasi-medical centers | 2 | 839 | 1299 | 170 | 6 |
| Regional hospitals | 75 | 9963 | 31,440 | 2144 | 147 |
| District hospitals | 307 | 4400 | 17,440 | 1088 | 146 |
| Others | 77 | 987 | 1319 | 2962 | 7 |
| Total | 483 | 29,283 | 73,191 | 7399 | 399 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.-C.; Chen, C.-Y.; Ko, M.-C.; Chien, Y.-C.; Su, E.C.-Y.; Chen, Y.-T. Factors Affecting Treatment with Life-Saving Interventions, Computed Tomography Scans and Specialist Consultations. Int. J. Environ. Res. Public Health 2020, 17, 2914. https://doi.org/10.3390/ijerph17082914
Chen C-C, Chen C-Y, Ko M-C, Chien Y-C, Su EC-Y, Chen Y-T. Factors Affecting Treatment with Life-Saving Interventions, Computed Tomography Scans and Specialist Consultations. International Journal of Environmental Research and Public Health. 2020; 17(8):2914. https://doi.org/10.3390/ijerph17082914
Chicago/Turabian StyleChen, Chu-Chieh, Chin-Yi Chen, Ming-Chung Ko, Yi-Chun Chien, Emily Chia-Yu Su, and Yi-Tui Chen. 2020. "Factors Affecting Treatment with Life-Saving Interventions, Computed Tomography Scans and Specialist Consultations" International Journal of Environmental Research and Public Health 17, no. 8: 2914. https://doi.org/10.3390/ijerph17082914
APA StyleChen, C.-C., Chen, C.-Y., Ko, M.-C., Chien, Y.-C., Su, E. C.-Y., & Chen, Y.-T. (2020). Factors Affecting Treatment with Life-Saving Interventions, Computed Tomography Scans and Specialist Consultations. International Journal of Environmental Research and Public Health, 17(8), 2914. https://doi.org/10.3390/ijerph17082914






