Transitional Care Interventions for Patients with Heart Failure: An Integrative Review
Abstract
1. Introduction
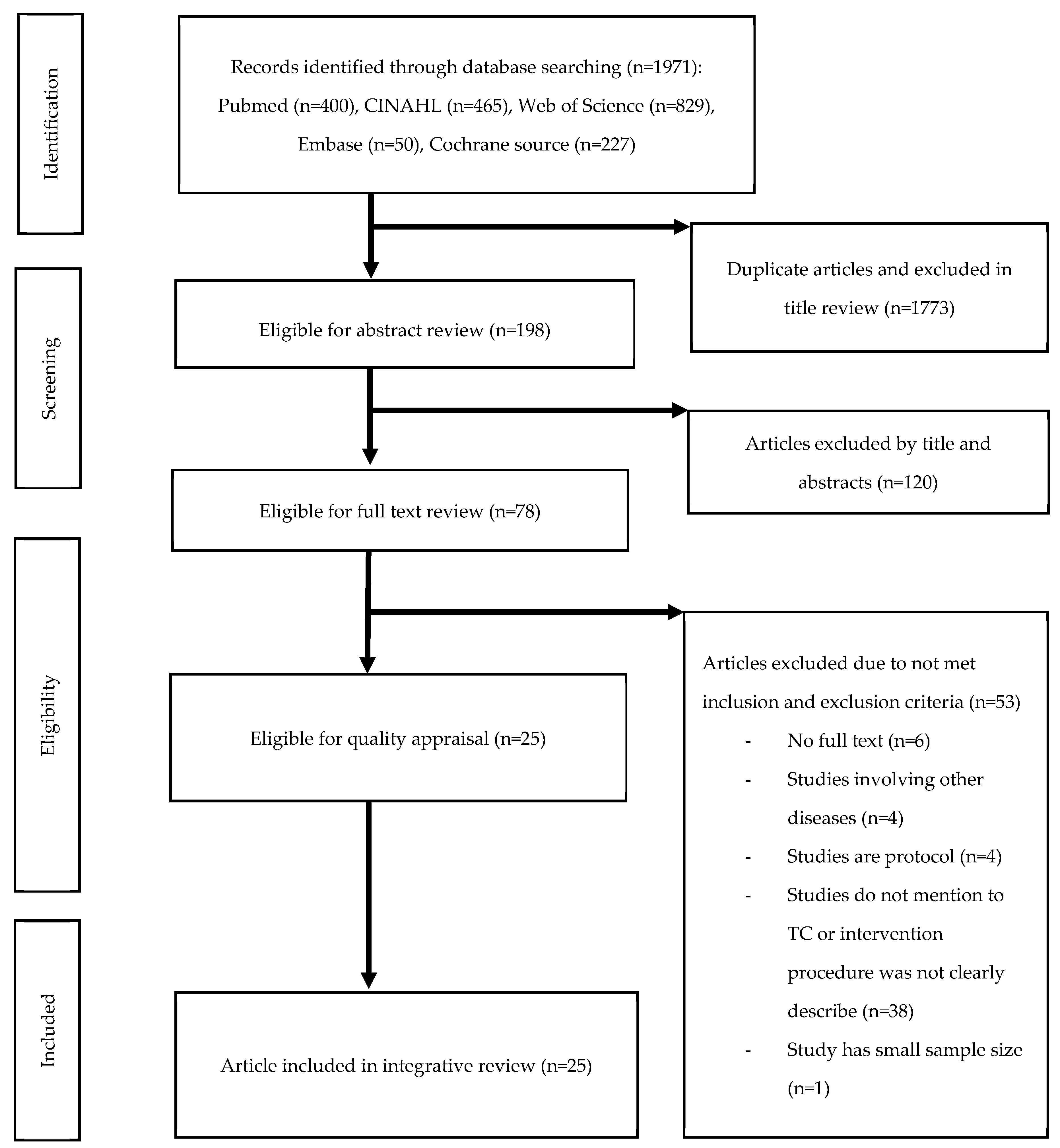
2. Materials and Methods
2.1. Study Design
2.2. Problem Identification
2.3. Literature Search
2.4. Data Evaluation
2.5. Data Analysis
3. Results
3.1. Characteristics of the Included Studies
3.2. Type and Severity of HF
3.3. Methodology of Transitional Care Interventions
3.4. Outcomes of Transitional Care Intervention
3.5. Effects of Transitional Care Intervention
3.6. Components of Transitional Care Interventions
3.6.1. Predischarge Interventions
3.6.2. Postdischarge Interventions
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dassanayaka, S.; Jones, S.P. Recent developments in heart failure. Circ. Res. 2015, 117, e58–e63. [Google Scholar] [CrossRef]
- von Lueder, T.G.; Agewall, S. The burden of heart failure in the general population: A clearer and more concerning picture. J. Thorac. Dis. 2018, 10, S1934–S1937. [Google Scholar] [CrossRef]
- Savarese, G.; Lund, L.H. Global public health burden of heart failure. Card. Fail. Rev. 2017, 3, 7–11. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Benjamin Emelia, J.; Go Alan, S.; Arnett Donna, K.; Blaha Michael, J.; Cushman, M.; Das Sandeep, R.; de Ferranti, S.; Després, J.-P.; Fullerton Heather, J.; et al. Heart disease and stroke statistics—2016 Update. Circulation 2016, 133, e38–e360. [Google Scholar] [CrossRef]
- Lee, J.H.; Lim, N.-K.; Cho, M.-C.; Park, H.-Y. Epidemiology of heart failure in Korea: Present and future. Korean Circ. J. 2016, 46, 658–664. [Google Scholar] [CrossRef] [PubMed]
- Nieminen, M.S.; Dickstein, K.; Fonseca, C.; Serrano, J.M.; Parissis, J.; Fedele, F.; Wikström, G.; Agostoni, P.; Atar, S.; Baholli, L.; et al. The patient perspective: Quality of life in advanced heart failure with frequent hospitalisations. Int. J. Cardiol. 2015, 191, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Lewis Eldrin, F.; Claggett Brian, L.; McMurray John, J.V.; Packer, M.; Lefkowitz Martin, P.; Rouleau Jean, L.; Liu, J.; Shi Victor, C.; Zile Michael, R.; Desai Akshay, S.; et al. Health-related quality of life outcomes in PARADIGM-HF. Circ. Heart Fail. 2017, 10, e003430. [Google Scholar] [CrossRef]
- Lee, H.; Oh, S.-H.; Cho, H.; Cho, H.-J.; Kang, H.-Y. Prevalence and socio-economic burden of heart failure in an aging society of South Korea. BMC Cardiovasc. Disord. 2016, 16, 215. [Google Scholar] [CrossRef] [PubMed]
- Van Spall, H.G.C.; Rahman, T.; Mytton, O.; Ramasundarahettige, C.; Ibrahim, Q.; Kabali, C.; Coppens, M.; Brian Haynes, R.; Connolly, S. Comparative effectiveness of transitional care services in patients discharged from the hospital with heart failure: A systematic review and network meta-analysis. Eur. J. Heart Fail. 2017, 19, 1427–1443. [Google Scholar] [CrossRef] [PubMed]
- Albert Nancy, M.; Barnason, S.; Deswal, A.; Hernandez, A.; Kociol, R.; Lee, E.; Paul, S.; Ryan Catherine, J.; White-Williams, C. Transitions of care in heart failure. Circ.: Heart Fail. 2015, 8, 384–409. [Google Scholar] [CrossRef]
- Naylor, M.; Sochalski, J. Scaling up: Bringing the transitional care model into the mainstream. Issue Brief (Commonw. Fund) 2010, 103, 1–12. [Google Scholar] [PubMed]
- Feltner, C.; Jones, C.D.; Cené, C.W.; Zheng, Z.-J.; Sueta, C.A.; Coker-Schwimmer, E.J.L.; Arvanitis, M.; Lohr, K.N.; Middleton, J.C.; Jonas, D.E. Transitional care interventions to prevent readmissions for persons with heart failure: A systematic review and meta-analysis. Ann. Intern. Med. 2014, 160, 774–784. [Google Scholar] [CrossRef] [PubMed]
- Albert, N.M. A systematic review of transitional-care strategies to reduce rehospitalization in patients with heart failure. Heart Lung 2016, 45, 100–113. [Google Scholar] [CrossRef] [PubMed]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Hong, Q.N.; FÀBregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. 2018, 34, 1–7. [Google Scholar] [CrossRef]
- Yu, D.S.F.; Lee, D.T.F.; Stewart, S.; Thompson, D.R.; Choi, K.-C.; Yu, C.-M. Effect of nurse-implemented transitional care for Chinese individuals with chronic heart failure in Hong Kong: A randomized controlled trial. J. Am. Geriatr. Soc. 2015, 63, 1583–1593. [Google Scholar] [CrossRef]
- Whitaker-Brown, C.D.; Woods, S.J.; Cornelius, J.B.; Southard, E.; Gulati, S.K. Improving quality of life and decreasing readmissions in heart failure patients in a multidisciplinary transition-to-care clinic. Heart Lung 2017, 46, 79–84. [Google Scholar] [CrossRef]
- Plakogiannis, R.; Mola, A.; Sinha, S.; Stefanidis, A.; Oh, H.; Katz, S. Impact of pharmacy student–driven postdischarge telephone calls on heart failure hospital readmission rates: A pilot program. Hosp. Pharm. 2019, 54, 100–104. [Google Scholar] [CrossRef]
- Wood, M.; Sweeney, T.; Trayah, M.; Civalier, M.; McMillian, W. The impact of transitions of care pharmacist services and identification of risk predictors in heart failure readmission. J. Pharm. Pract. 2019. [Google Scholar] [CrossRef]
- O’Connor, M.; Asdornwised, U.; Dempsey, M.L.; Huffenberger, A.; Jost, S.; Flynn, D.; Norris, A. Using telehealth to reduce all-cause 30-day hospital readmissions among heart failure patients receiving skilled home health services. Appl. Clin. Inform. 2016, 7, 238–247. [Google Scholar] [CrossRef][Green Version]
- Harrison, M.B.; Browne, G.B.; Roberts, J.; Tugwell, P.; Gafni, A.; Graham, I.D. Quality of life of individuals with heart failure: A randomized trial of the effectiveness of two models of hospital-to-home transition. Med. Care 2002, 40, 271–282. [Google Scholar] [CrossRef] [PubMed]
- Naylor, M.D.; Brooten, D.A.; Campbell, R.L.; Maislin, G.; McCauley, K.M.; Schwartz, J.S. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. J. Am. Geriatr. Soc. 2004, 52, 675–684. [Google Scholar] [CrossRef] [PubMed]
- Williams, G.; Akroyd, K.; Burke, L. Evaluation of the transitional care model in chronic heart failure. Br. J. Nurs. 2010, 19, 1402–1407. [Google Scholar] [CrossRef] [PubMed]
- Barnason, S.; Zimmerman, L.; Hertzog, M.; Schulz, P. Pilot testing of a medication self-management transition intervention for heart failure patients. West J. Nurs. Res. 2010, 32, 849–870. [Google Scholar] [CrossRef] [PubMed]
- Stauffer, B.D.; Fullerton, C.; Fleming, N.; Ogola, G.; Herrin, J.; Stafford, P.M.; Ballard, D.J. Effectiveness and cost of a transitional care program for heart failure: A prospective study with concurrent controls. Arch. Intern. Med. 2011, 171, 1238–1243. [Google Scholar] [CrossRef]
- Simpson, M. A Quality Improvement plan to reduce 30-day readmissions of heart failure patients. J. Nurs. Care Qual. 2014, 29, 280–286. [Google Scholar] [CrossRef]
- Truong, J.T.; Backes, A.C. The impact of a continuum of care resident pharmacist on heart failure readmissions and discharge instructions at a community hospital. SAGE Open Med. 2015, 3. [Google Scholar] [CrossRef]
- Wong, F.K.Y.; Ng, A.Y.M.; Lee, P.H.; Lam, P.-T.; Ng, J.S.C.; Ng, N.H.Y.; Sham, M.M.K. Effects of a transitional palliative care model on patients with end-stage heart failure: A randomised controlled trial. Heart 2016, 102, 1100–1108. [Google Scholar] [CrossRef]
- Ong, M.K.; Romano, P.S.; Edgington, S.; Aronow, H.U.; Auerbach, A.D.; Black, J.T.; De Marco, T.; Escarce, J.J.; Evangelista, L.S.; Hanna, B.; et al. Effectiveness of remote patient monitoring after discharge of hospitalized patients with heart failure: The better effectiveness after transition–heart failure (BEAT-HF) randomized clinical trial. JAMA Intern. Med. 2016, 176, 310–318. [Google Scholar] [CrossRef]
- Pacho, C.; Domingo, M.; Núñez, R.; Lupón, J.; Moliner, P.; de Antonio, M.; González, B.; Santesmases, J.; Vela, E.; Tor, J.; et al. Early postdischarge STOP-HF-Clinic reduces 30-day readmissions in old and frail patients with heart failure. Rev. Esp Cardiol. (Engl. Ed.) 2017, 70, 631–638. [Google Scholar] [CrossRef]
- Miller, A.; Edenfield, E.E.; Roberto, J.; Erb, J.K. Reduction in re-hospitalization rates utilizing physical therapists within a post–acute transitional care program for home care patients with heart failure. Home Health Care Manag. Pract. 2017, 29, 7–12. [Google Scholar] [CrossRef]
- Wong, F.K.Y.; So, C.; Ng, A.Y.M.; Lam, P.-T.; Ng, J.S.C.; Ng, N.H.Y.; Chau, J.; Sham, M.M.K. Cost-effectiveness of a transitional home-based palliative care program for patients with end-stage heart failure. J. Palliat. Med. 2017, 32, 476–484. [Google Scholar] [CrossRef]
- Rezapour-Nasrabad, R. Application of transitional care mode in patients with chronic heart disease: A case-controlled intervention study. Rev. Latinoam. Hiperte. 2018, 13, 285–290. [Google Scholar]
- Moye, P.M.; Chu, P.S.; Pounds, T.; Thurston, M.M. Impact of a pharmacy team–led intervention program on the readmission rate of elderly patients with heart failure. Am. J. Health Syst. Pharm. 2018, 75, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Garnier, A.; Rouiller, N.; Gachoud, D.; Nachar, C.; Voirol, P.; Griesser, A.-C.; Uhlmann, M.; Waeber, G.; Lamy, O. Effectiveness of a transition plan at discharge of patients hospitalized with heart failure: A before-and-after study. ESC Heart Fail. 2018, 5, 657–667. [Google Scholar] [CrossRef]
- Shekarriz-Foumani, R.; Laal, N.; Khosravi, S. The effect of educatoin and follow up after discharge (FAD) on reducing readmission of CHF patients: A randomized controlled trial. Int. J. Health Med. Cur. Res. 2018, 3, 736–743. [Google Scholar]
- Reese, R.L.; Clement, S.A.; Syeda, S.; Hawley, C.E.; Gosian, J.S.; Cai, S.; Jensen, L.L.; Kind, A.J.H.; Driver, J.A. Coordinated-transitional care for veterans with heart failure and chronic lung disease. J. Am. Geriatr. Soc. 2019, 67, 1502–1507. [Google Scholar] [CrossRef]
- Van Spall, H.G.C.; Lee, S.F.; Xie, F.; Oz, U.E.; Perez, R.; Mitoff, P.R.; Maingi, M.; Tjandrawidjaja, M.C.; Heffernan, M.; Zia, M.I.; et al. Effect of patient-centered transitional care services on clinical outcomes in patients hospitalized for heart failure: The PACT-HF randomized clinical trial. JAMA 2019, 321, 753–761. [Google Scholar] [CrossRef]
- Murphy, J.A.; Schroeder, M.N.; Rarus, R.E.; Yakubu, I.; McKee, S.O.P.; Martin, S.J. Implementation of a cardiac transitions of care pilot program: A prospective study of inpatient and outpatient clinical pharmacy services for patients with heart failure exacerbation or acute myocardial infarction. J. Pharm. Pract. 2019, 32, 68–76. [Google Scholar] [CrossRef]
- Neu, R.; Leonard, M.A.; Dehoorne, M.L.; Scalia, S.J.; Kale-Pradhan, P.B.; Giuliano, C.A. Impact of pharmacist involvement in heart failure transition of care. Ann. Pharmacother. 2020, 54, 239–246. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The task force for the diagnosis and treatment of acute and chronic heart failure of the European society of cardiology (ESC) developed with the special contribution of the heart failure association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef] [PubMed]
- Yancy Clyde, W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey Donald, E.; Drazner Mark, H.; Fonarow Gregg, C.; Geraci Stephen, A.; Horwich, T.; Januzzi James, L.; et al. 2013 ACCF/AHA guideline for the management of heart failure: Executive summary. Circulation 2013, 128, 1810–1852. [Google Scholar] [CrossRef]
- Comín-Colet, J.; Enjuanes, C.; Lupón, J.; Cainzos-Achirica, M.; Badosa, N.; Verdú, J.M. Transitions of care between acute and chronic heart failure: Critical steps in the design of a multidisciplinary care model for the prevention of rehospitalization. Rev. Esp Cardiol. (Engl. Ed.) 2016, 69, 951–961. [Google Scholar] [CrossRef]
- Vedel, I.; Khanassov, V. Transitional care for patients with congestive heart failure: A systematic review and meta-analysis. Ann. Fam. Med. 2015, 13, 562–571. [Google Scholar] [CrossRef]
- Stamp, K.D.; Machado, M.A.; Allen, N.A. Transitional care programs improve outcomes for heart failure patients: An integrative review. J. Cardiovasc. Nurs. 2014, 29, 140–154. [Google Scholar] [CrossRef]
- Coleman, E.A.; Mahoney, E.; Parry, C. Assessing the quality of preparation for posthospital care from the patient’s perspective: The care transitions measure. Med. Care 2005, 43, 246–255. [Google Scholar] [CrossRef]
- Goldstein, J.N.; Hicks, L.S.; Kolm, P.; Weintraub, W.S.; Elliott, D.J. Is the care transitions measure associated with readmission risk? Analysis from a single academic center. J. Gen. Intern. Med. 2016, 31, 732–738. [Google Scholar] [CrossRef][Green Version]
- Zhang, P.; Xing, F.-M.; Li, C.-Z.; Wang, F.-L.; Zhang, X.-L. Effects of a nurse-led transitional care programme on readmission, self-efficacy to implement health-promoting behaviours, functional status and life quality among Chinese patients with coronary artery disease: A randomised controlled trial. J. Clin. Nurs. 2018, 27, 969–979. [Google Scholar] [CrossRef]
- Ziaeian, B.; Fonarow, G.C. Epidemiology and aetiology of heart failure. Nat. Rev. Cardiol. 2016, 13, 368–378. [Google Scholar] [CrossRef]
- Boisvert, S.; Proulx-Belhumeur, A.; Gonçalves, N.; Doré, M.; Francoeur, J.; Gallani, M.-C. An integrative literature review on nursing interventions aimed at increasing self-care among heart failure patients. Rev. Lat.-Am Enferm. 2015, 23, 753–768. [Google Scholar] [CrossRef]
| Author (Year) Country | Study Design | Sample (Number (Male %), Type of HF, Age, Racial Ethnicity, HF Severity) | Contents of Intervention (Intervention, Major Intervention Provider, Transition Time/Place, Intervention Duration) | Outcomes (Significance) | |
|---|---|---|---|---|---|
| Clinical Outcomes | Patient-Related Outcomes | ||||
| Harrison, et al. (2002) [21] Canada | RCT (Exp. vs. Con.) | N = 192 (55%) | Transitional care intervention | Hospital readmissions (−) | HRQoL (+++) |
| Congestive HF | Nurses | ||||
| 75 years | Hospital to home | All-cause emergency room visits (+) | QoL (−) | ||
| N/A | |||||
| NYHA III/IV 77% | Until 2 weeks after hospital discharge | ||||
| Naylor et al. (2004) [22] UnUSA | RCT (Exp. vs. Con.) | N = 239 (43%) | Transitional care intervention (APN-directed discharge planning and home follow-up) | First rehospitalization period or death at 52 weeks (+) | QoL (+) |
| HF | |||||
| 76 years | |||||
| APN | |||||
| African American 36% | Hospital to home | Satisfaction (+++) | |||
| LVEF (~45%–20%) ~69%–72% | 3 months | Cost (+) | |||
| Williams et al. (2010) [23] United Kingdom | Quasi-experiment (Exp. vs. Con.) | N = 97 (52%) | Transitional care service | Readmissions at 30 days (−) | Satisfaction (non-statistics, positive feedback) |
| CHF | |||||
| ~71–78 years | CNS | ||||
| N/A | Hospital to home | LOS (−) | |||
| N/A | 18 weeks | ||||
| Barnason et al. (2010) [24] USA | RCT (Exp. vs. Con.) | N = 38 (65%) | Hospital transition intervention | N/A | Medication adherence (+++) |
| HF | Research nurse | ||||
| 77 years | Hospital to home | Self-efficacy for HF self-care (+++) | |||
| N/A | |||||
| NYHA III 55% | 2~3 weeks | HRQoL (++) | |||
| Stauffer et al. (2011) [25] USA | Prospective study (Exp. vs. Con.) | N = 1025 (47%) | Transitional care program | 30 day all-cause readmission rate (+) | N/A |
| HF | APN | LOS (−) | |||
| ~79–81 years | |||||
| White ~78%–84% | Hospital to home | 60 day direct cost from admission (−) | |||
| BNP level > 200 ng/mL | 3 months | Budget impact analysis (non-statistics, reduced hospital financial) | |||
| Simpson (2014) [26] USA | Pre-and post-test (Exp. only) | N = 263 (N/A) | Nurse-implemented transitional care | 30 day readmission rate (non-statistics, decreased rate) | N/A |
| HF | NP | ||||
| N/A | |||||
| N/A | Hospital to home | ||||
| N/A | 5 months | ||||
| Yu et al. (2015) [16] China | RCT (Exp. vs. Con.) | N = 178 (45%) | Cardiac nurse-implemented transitional care | Event-free survival (−) | Self-care (maintenance, management, confidence, and knowledge) (+) HRQoL (++) |
| CHF | Cardiac nurse | ||||
| 79 years | Hospital to home | All-cause hospital readmission (+) | |||
| 9 months | |||||
| N/A | 9 month mortality (+) | ||||
| NYHA II/III ~97%–98% | LOS (+) | ||||
| Truong et al. (2015) [27] USA | Cohort study (Exp. vs. Con.) | N = 632 (~49%–61%) | Continuum of Care Network (CCN) program | 30 day all-cause hospital readmissions (++) | N/A |
| HF | Resident pharmacist | ||||
| ~68–82 years | |||||
| White ~59%–62% | Hospital to home | Compliance with HF-1 at a single community hospital (++) | |||
| N/A | From admission to home after discharge | ||||
| Wong et al. (2016) [28] China | RCT (Exp. vs. Con.) | N = 84 (52%) | Transitional Care Palliative (TCP)-ESHF program | Readmissions at 12 weeks (++) | Symptom intensity (+) |
| Functional status (+) | |||||
| QoL (+) | |||||
| ESHF | NCM | ||||
| Satisfaction with care (+++) | |||||
| 78 years | Hospital to home | ||||
| N/A | |||||
| NYHA III/IV 86%~93% | 12 weeks | ||||
| Ong et al. (2016) [29] USA | RCT (Exp. vs. Con.) | N = 1437 (54%) | Better Effectiveness After Transition–Heart | 180 day all-cause readmission (−) | QoL (+) |
| Decompensated HF | Failure (BEAT-HF) | ||||
| 73 year | Nurses | ||||
| White ~54%–55% | Hospital to home | 30 day all-cause readmission (−) | |||
| African American ~22%– | |||||
| 23% | 180 days | 180 day mortality (−) | |||
| NYHA III ~64%–66% | |||||
| O’Connor et al. (2016) [20] USA | Prospective study (Exp. only) | N = 818 (N/A) | Telehealth program using the Transitional Care Model | All-cause 30 day readmission rate (non-statistics, reduced readmission) | N/A |
| HF | RN and telehealth liaisons nurses | ||||
| N/A | |||||
| N/A | Hospital to home | ||||
| N/A | Mean 63~94 days | ||||
| Whitaker-Brown et al. (2017) [17] USA | Pre-and post-test (Exp. only) | N = 50 (42%) | 4-week pilot transition-to-care program | 30 day hospital readmission (non-statistics, two participants were readmitted) | HRQoL (+) |
| HF | Multidisciplinary team | ||||
| 70 years | Hospital to outpatient setting (Transition clinic) | ||||
| Caucasian 83% | |||||
| HFrEF (Severe <20%) | |||||
| HFrEF (Severe <20%) 11% /HFpEF (Mild 40%–55%) 19% | 4 weeks | ||||
| Pacho et al. (2017) [30] Spain | Prospective study (Exp. vs. Con.) | N = 518 (43%) | APN-directed discharge planning and home follow-up protocol | All-cause 30 day readmission (+++) | N/A |
| HF | |||||
| 82 years | APN | ||||
| N/A | Hospital to STOP-HE-clinic | HF-related 30 day readmission (+++) | |||
| N/A | 30 days | ||||
| Miller et al. (2017) [31] USA | Prospective study (Exp. vs. Con.) | N = 462 (49%) | Multidisciplinary post-acute transitional care (MDTC) program | All-cause readmission rates (+++) | N/A |
| HF | |||||
| 81 years | Multidisciplinary team | Visit number during the first 2 weeks (++) | |||
| Caucasian 79.5% | Hospital to home (connected by Hospital home care agency) | ||||
| N/A | 2 weeks | ||||
| Wong et al. (2017) [32] China | RCT (Exp. vs. Con.) | N = 84 (N/A) | Transitional Home-based Palliative End-stage Heart Failure (THPESHF) program | Readmission at 84 days (+++) | QoL (−) |
| ESHF | |||||
| 76 years | ER visit at 84 days (+) | QALY (non-statistics, 0.0012 at 28 days/0.0077 at 84 days) | |||
| N/A | NCM | Hospital stay at 84 days (+++) | |||
| Hospital to home | Cost (non-statistics, cost-effectiveness probability) | ||||
| N/A | 1 year | ||||
| Rezapour-Nasrabad (2018) [33] Iran | RCT (Exp. vs. Con.) | N = 168 (63%) | Transitional care intervention | N/A | HRQoL (+) |
| CHF | Liaison nurses | ||||
| >65 years (30%) | Hospital to home | ||||
| N/A | |||||
| N/A | 6 months | ||||
| Moye et al. (2018) [34] USA | Cohort study (Exp. vs. Con.) | N = 177 (35%) | Pharmacy team-led intervention program | The number of days that elapsed after discharge to the first readmission (+) | N/A |
| HF | Pharmacist | HF-related readmission (−) | |||
| 71 year | Hospital to home | ||||
| African American 92% | 15 months | ||||
| LVEF (<40%) ~41%–48% | |||||
| Garnier et al. (2018) [35] Switzerland | Cohort study (Exp. vs. Con.) | N = 1872 (~53%–54%) | Multimodal care transition plan | The fraction of days spent for readmissions (−) | N/A |
| HF | Multidisciplinary team | The rate of readmission (−) | |||
| ~76–78 years | Hospital to home | Decreasing the fraction of days spent for 30 day readmission compared to non-completers (++) | |||
| N/A | |||||
| N/A | 13 months | Decreasing PARE compared with non-completers (++) | |||
| The rate of PARE decreased ~8.7%–9.9%, reaching the adjusted expected range given by SQLape® (7.7%–9.1%) | |||||
| Shekarriz-Foumani et al. (2018) [36] Iran | RCT (Exp. vs. Con.) | N = 120 (~65%–73%) | Education and Follow-up after Discharge | Readmission rate (+) | Medication compliance (−) |
| HF | |||||
| ~65–66 years | (FAD) program | Outpatient visits to physician (−) | |||
| N/A | Multidisciplinary team | ||||
| NYHA III/IV ~42%–45% | Hospital to home | ||||
| 3 months | |||||
| Reese et al. (2019) [37] USA | Cohort study (Exp. vs. Con.) | N = 1092 (97%) | The Coordinated-Transitional Care (C-TraC) program | Readmission (+) | N/A |
| Congestive HF | 30 day ED or UC visits (−) | ||||
| ~74–75 years | RN-CM | Cost (non-statistics, TCI helps decrease total cost) | |||
| White ~90%–91% | Hospital to home | ||||
| N/A | 4 weeks | ||||
| Van Spall et al. (2019) [38] Canada | RCT (Exp. vs. Con.) | N = 2494 (50%) | Patient-Centered Care Transitions in HF (PACT-HF) service | All-cause readmission at 30 days (−), 3 months (−) | Discharge preparedness at 6 weeks (+++) |
| HF | |||||
| 78 years | |||||
| NCM | ED visit at 30 days (−), 3 months (−) | Quality of transition at 6 weeks (+) | |||
| N/A | Hospital to home | ||||
| N/A | 6 months | Death at 3 months (−) | QoL at discharge (+++), 6weeks (+), and 6 months (+) | ||
| QALY (−) | |||||
| Murphy et al. (2019) [39] USA | Prospective study (Exp. only) | N = 100 (58%) in HF | Cardiac Transitions of Care Pilot Program | 30 day readmission rates (−) | N/A |
| HF | Multidisciplinary team (physicians, pharmacists, nurse practitioners, dietitians) | 72 h ED visit rates (−) | |||
| 68 years | Hospital to home | 30 day mortality rate (−) | |||
| Caucasian 69% | |||||
| N/A | 5 weeks (Inpatient 1 week and outpatient 4 weeks) | ||||
| Plakogiannis et al. (2019) [18] USA | Retrospective cohort study (Exp. only) | N = 131 (57%) | Transdisciplinary HF care transition team (HFCTT) intervention with pharmacy student–driven postdischarge phone calls | Readmission: at 30 days (++) and 90 days (++) | N/A |
| HF | Pharmacy student (with Multidisciplinary team) | ||||
| 72 years | |||||
| White 71% | Hospital to home | ||||
| HFrEF 48% | Different duration by each patient ~14–60 days | ||||
| Wood et al. (2019) [19] USA | Retrospective cohort study (Exp. only) | N = 3462 (56%) | Transitions of Care (TOC) Pharmacist Services | 30 day all-cause readmission (−) | N/A |
| HF | |||||
| 72 years | Pharmacists and an HF nurse educator | ||||
| White 95% of n = 2347 | Hospital to home | ||||
| LVEF (≤40%) 26% | From admission to ~48–72 h after discharge | 30 day HF readmissions (−) | |||
| Neu et al. (2020) [40] USA | Quasi-experiment (Exp. vs. Con.) | N = 663 (52%) | Pharmacy-led HF transition of care (TOC) | HF 30 day hospital readmission rate (+) | N/A |
| HF | |||||
| ~66–69 years | Pharmacist | ||||
| White 40%, Black 57% | Hospital to home | ||||
| LVEF (≤40%) ~51%–54% | 30 days | ||||
| Author (Year) | Transitional Care Intervention Components | |
|---|---|---|
| Predischarge Intervention | Postdischarge Intervention | |
| Harrison et al. (2002) [21] | 1. Early assessment after hospital admission; 2. Medication reconciliation; 3. Discharge planning patient education | 1. Supportive care for self-management through education or home visit; 2. Links between hospital and home nurses and patients; 3. Balance of care between the patient and family and professional providers |
| Naylor et al. (2004) [22] | 1. Early assessment after hospital admission | 1. Telephone support; 2. Nurse home visits |
| Williams et al. (2010) [23] | 1. Discharge planning patient education | 1. Follow-up and home visit |
| Barnason et al. (2010) [24] | 1. Early follow-up after discharge; 2. Follow-up telephone call | |
| Stauffer et al. (2011) [25] | 1. Screening for eligibility within hospital admission; 2. Discharge planning | 1. Early follow-up after discharge; 2. Telephone support; 3. Nurse home visits |
| Simpson (2014) [26] | 1. Education | 1. Postdischarge telephone contact |
| Yu et al. (2015) [16] | 1. Appointment schedule before discharge; 2. Discharge planning | 1. Home visits; 2. Follow-up telephone call |
| Truong et al. (2015) [27] | 1. Admission medication review; 2. Daily monitoring; 3. Discharge medication review; 4. Discharge counseling | 1. Early follow-up after discharge |
| Wong et al. (2015) [28] | 1. Appointment schedule before discharge; 2. Discharge planning | 1. Home visit together; 2. Telephone follow-up |
| Ong et al. (2016) [29] | 1. Predischarge health education | 1. Follow-up telephone call |
| O’Connor et al. (2016) [20] | 1. Telemonitoring (personal goal setting, self-monitoring, management of symptoms, and reporting changes to their physician or care team) | |
| Whitaker-Brown et al. (2015) [17] | 1. Discharge planning | 1. Appointment for transition clinic visit (risk assessment, physical assessment, and evaluation); 2. Medication reconciliation; 3. Early follow-up telephone call; 4. Providing information related to rehabilitation, home care, hospice, and/or palliative care |
| Pacho et al. (2017) [30] | N/A | 1. Early postdischarge visit; 2. HF nurse education to patient and caregiver; 3. Treatment titration; 4. Intravenous medication; 5. Early follow-up via e-notification |
| Miller et al. (2017) [31] | N/A | 1. Education and consulting; 2. Early home visit |
| Wong et al. (2017) [32] | 1. Hospital visit before discharge to introduce the program | 1. Nurse home visit; 2. Nurse telephone call; 3. Volunteer social visit |
| Rezapour-Nasrabad (2018) [33] | 1. Nursing care support | 1. Follow-up telephone call |
| Moye et al. (2018) [34] | 1. Medication prescript and manage; 2. Standard-of-care HF education program; 3. Medication reconciliation; 4. Discharge planning | 1. Postdischarge appointment; 2. Follow-up phone calls by pharmacy team |
| Garnier et al. (2018) [35] | 1. Targeted therapeutic education; 2. Caregiver therapeutic education; 3. Medication reconciliation at admission and discharge; 4. Set up of an appointment with the GP; 5. Notification of the GP; 6. Community nurse notification; 7. Patient-centered discharge instructions | 1. Follow-up telephone call; 2. Telephone support |
| Shekarriz-Foumani et al. (2018) [36] | 1. Screening for eligibility within hospital admission; 2. Collecting demographic and disease information; 3. Explaining questions to be interviewed on telephone calls | 1. Educating the patients and their guardians immediately after discharge; 2. Follow-up telephone call |
| Reese et al. (2019) [37] | 1. Discharge planning patient education | 1. Telephone follow-up |
| Van Spall et al. (2019) [38] | 1. Nurse-led self-care education; 2. A structured hospital discharge summary | 1. Family physician follow-up; 2. Postdischarge nurse-led home visits and heart function clinic care (includes telephone assessment) |
| Murphy et al. (2019) [39] | 1. Admission medication review. 2. Daily monitoring 3. Discharge medication review | 1. Discharge counseling by telephone; 2. Postdischarge follow-up |
| Plakogiannis et al. (2019) [18] | 1. Early assessment after hospital admission | 1. The social worker provided the patient and the caregiver with the necessary support for a smooth transition into the community; 2. Telephone call by pharmacy student (reviewed the medications, HF symptoms, and performed a detailed medication reconciliation and counseling) |
| Wood et al. (2019) [19] | 1. Inpatient medication reconciliation; 2. Medication history review | 1. A follow-up phone call |
| Neu et al. (2020) [40] | 1. Admission medication reconciliation; 2. Discharge medication reconciliation; 3. Patient or caregiver counseling with a focus on HF medications through verbal and written education materials | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mai Ba, H.; Son, Y.-J.; Lee, K.; Kim, B.-H. Transitional Care Interventions for Patients with Heart Failure: An Integrative Review. Int. J. Environ. Res. Public Health 2020, 17, 2925. https://doi.org/10.3390/ijerph17082925
Mai Ba H, Son Y-J, Lee K, Kim B-H. Transitional Care Interventions for Patients with Heart Failure: An Integrative Review. International Journal of Environmental Research and Public Health. 2020; 17(8):2925. https://doi.org/10.3390/ijerph17082925
Chicago/Turabian StyleMai Ba, Hai, Youn-Jung Son, Kyounghoon Lee, and Bo-Hwan Kim. 2020. "Transitional Care Interventions for Patients with Heart Failure: An Integrative Review" International Journal of Environmental Research and Public Health 17, no. 8: 2925. https://doi.org/10.3390/ijerph17082925
APA StyleMai Ba, H., Son, Y.-J., Lee, K., & Kim, B.-H. (2020). Transitional Care Interventions for Patients with Heart Failure: An Integrative Review. International Journal of Environmental Research and Public Health, 17(8), 2925. https://doi.org/10.3390/ijerph17082925






