When Land Is Under Pressure Health Is Under Stress
Abstract
:1. Introduction
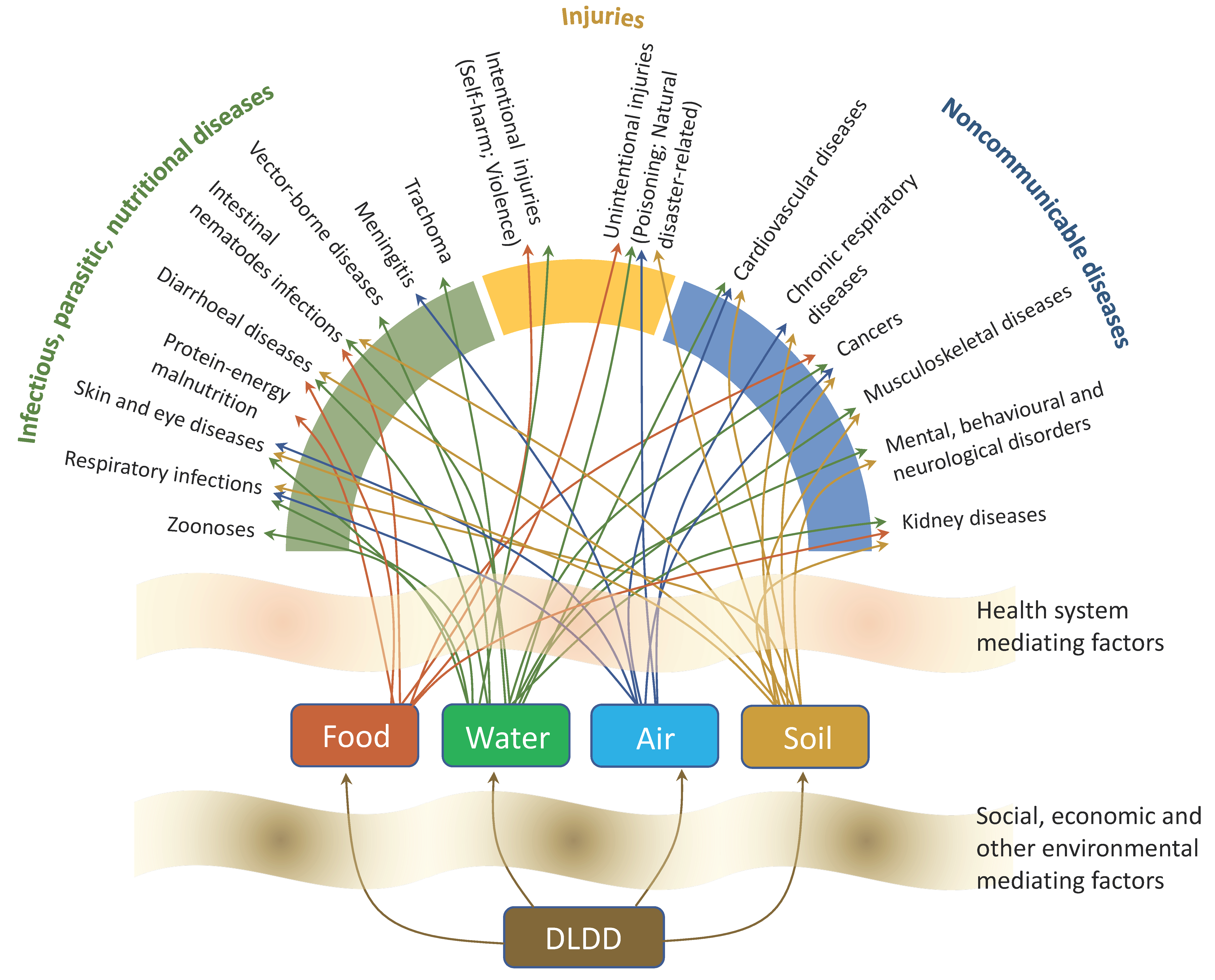
2. DLDD Pathways Affecting on Human Health
2.1. Environmental Mediating Factors
2.1.1. Water Security and Safety
2.1.2. Food Security and Safety
2.1.3. Air Quality
2.1.4. Soil Quality
2.2. Social, Economic and Health System Mediating Factors
3. Discussion: Challenges and Directions to Improve Human Livelihoods
3.1. Poverty
3.2. Forced Migration
3.3. Water Security
3.4. Food Security
3.5. Responding to the Challenges
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sanz, M.J.; de Vente, J.; Chotte, J.-L.; Bernoux, M.; Kust, G.; Ruiz, I.; Almagro, M.; Alloza, J.-A.; Vallejo, R.; Castillo, V.; et al. Sustainable Land Management contribution to successful land-based climate change adaptation and mitigation. In A Report of the Science-Policy Interface; United Nations Convention to Combat Desertification (UNCCD): Bonn, Germany, 2017; Available online: https://www.unccd.int/sites/default/files/documents/201709/UNCCD_Report_SLM.pdf (accessed on 25 December 2020).
- Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services (IPBES). Summary for Policymakers of the Global Assessment Report on Biodiversity and Ecosystem Services of the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services; Díaz, S., Settele, J., Brondízio, E.S., Ngo, H.T., Guèze, M., Agard, J., Arneth, A., Balvanera, P., Brauman, K.A., Butchart, S.H.M., et al., Eds.; IPBES Secretariat: Bonn, Germany, 2019; 56p, Available online: https://ipbes.net/global-assessment (accessed on 17 October 2020).
- World Health Organization (WHO). A Report of the Millennium Ecosystem Assessmen. In Ecosystems and Human Well-Being: Health Synthesis; World Health Organization: Geneva, Switzerland, 2005; Available online: https://apps.who.int/iris/bitstream/handle/10665/43354/9241563095.pdf?sequence=1&isAllowed=y (accessed on 17 October 2020).
- Whitmee, S.; Haines, A.; Beyrer, C.; Boltz, F.; Capon, A.; Souza Dias, B.F.; Ezeh, A.; Frumkin, H.; Gong, P.; Head, P.; et al. Safeguarding Human Health in the Anthropocene Epoch: Report of the Rockfeller Foundation-Lancet Commission on Planetary Health. Lancet 2015, 386, 1973–2028. Available online: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(15)60901-1/fulltext (accessed on 17 October 2020). [CrossRef]
- Food Security Information Network (FSIN). Global Report on Food Crisis. Joint Analysis for Better Decisions. Food Security Information Network. 2019. Available online: http://www.fsinplatform.org/sites/default/files/resources/files/GRFC_2019-Full_Report.pdf (accessed on 17 October 2020).
- Verner, D. Reducing Poverty, Protecting Livelihoods, and Building Assets in a Changing Climate: Social Implications of Climate Change for Latin America and the Caribbean. Directions in Development; Environment and Sustainable Development; The World Bank: Washington, DC, USA, 2010; Available online: https://openknowledge.worldbank.org/handle/10986/2473 (accessed on 25 December 2020).
- Intergovernmental Panel on Climate Change (IPCC). Climate Change 2014: Synthesis Report. Contribution of Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Core Writing Team; Pachauri, R.K., Meyer, L.A., Eds.; IPCC: Geneva, Switzerland, 2014; 151p, Available online: https://www.ipcc.ch/report/ar5/syr/ (accessed on 17 October 2020).
- Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services (IPBES). The IPBES assessment report on land degradation and restoration. In Secretariat of the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services; Montanarella, L., Scholes, R., Brainich, A., Eds.; IPBES Secretariat: Bonn, Germany, 2018; 744p, Available online: https://www.ipbes.net/assessment-reports/ldr (accessed on 25 December 2020).
- United Nations (UN). High-level Meeting on Addressing Desertification, Land Degradation and Drought in the Context of Sustainable Development and Poverty Eradication. United Nations General Assembly. A/65/861. June 2011. Available online: https://digitallibrary.un.org/record/706202?ln=en (accessed on 17 October 2020).
- United Nations General Assembly (UNGA). Intergovernmental Negotiating Committee for the Elaboration of an International Convention to Combat Desertification in Those Countries Experiencing Serious Drought and/or Desertification, Particularly in Africa. A/AC.241/27. 1994. Available online: https://www.unccd.int/sites/default/files/relevant-links/2017-01/English_0.pdf (accessed on 17 October 2020).
- Wilhite, D.A.; Glantz, M.H. Understanding the Drought Phenomenon: The Role of Definitions; Drought Mitigation Center Faculty Publications: Lincoln, NE, USA, 1985; Available online: https://digitalcommons.unl.edu/cgi/viewcontent.cgi?article=1019&context=droughtfacpub (accessed on 25 December 2020).
- National Drought Mitigation Center (NDMC). Types of Drought; University of Nebraska-Lincoln: Lincoln, NE, USA, n.d.; Available online: https://drought.unl.edu/Education/DroughtIn-depth/TypesofDrought.aspx (accessed on 25 December 2020).
- Intergovernmental Panel on Climate Change (IPCC). Managing the risks of extreme events and disasters to advance climate change adaptation. In A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change; Field, C.B., Barros, V., Stocker, T.F., Qin, D., Dokken, D.J., Ebi, K.L., Mastrandrea, M.D., Mach, K.J., Plattner, G.-K., Allen, S.K., et al., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2012; 582p, Available online: https://www.ipcc.ch/site/assets/uploads/2018/03/SREX_Full_Report-1.pdf (accessed on 17 October 2020).
- United Nations (UN). The future we want. In Proceedings of the Outcome Document of the United Nations Conference on Sustainable Development, Rio de Janeiro, Brazil, 20–22 June 2012; United Nations: New York, NY, USA, 2012. Available online: https://sustainabledevelopment.un.org/content/documents/733FutureWeWant.pdf (accessed on 25 December 2020).
- International Panel on Climate Change (IPCC). Climate change and land. In An IPCC Special Report on Climate Change, Desertification, Land Degradation, Sustainable Land Management, Food Security, and Greenhouse Gas Fluxes in Terrestrial Ecosystems; Summary for Policymakers—Approved Draft. International Panel on Climate Change; WMO and UNEP, 2019; Available online: https://www.ipcc.ch/site/assets/uploads/2019/08/4.-SPM_Approved_Microsite_FINAL.pdf (accessed on 25 December 2020).
- World Health Organization (WHO); World Meteorological Organizational (WMO). Atlas of Health and Climate; World Health Organization and World Meteorological Organizational: Geneva, Switzerland, 2012; Available online: https://www.who.int/globalchange/publications/atlas/report/en/ (accessed on 17 October 2020).
- Warner, K.; Ehrhart, C.; de Sherbinin, A.; Adamo, S.; Chai-Onn, T. In Search of Shelter: Mapping the Effects of Climate Change on Human Migration and Displacement. Bonn, Germany: United Nations University, CARE, and CIESIN-Columbia University and in Close Collaboration with the European Commission “Environmental Change and Forced Migration Scenarios Project”, the UNHCR, and the World Bank. 2009. Available online: https://ciesin.columbia.edu/documents/ClimMigr-rpt-june09.pdf (accessed on 17 October 2020).
- United Nations Convention to Combat Desertification (UNCCD). The Future Strategic Framework of the Convention. ICCD/COP(13)/L.18. 14 September 2017. Agenda Item 2 (b); 2030 Agenda for Sustainable Development: Implications for the United Nations Convention to Combat Desertification; UNCCD: Bonn, Germany, 2017; Available online: https://www.unccd.int/sites/default/files/inline-files/ICCD_COP%2813%29_L.18-1716078E_0.pdf (accessed on 25 December 2020).
- United Nations Convention to Combat Desertification (UNCCD). About the Convention; UNCCD: Bonn, Germany, n.d.; Available online: https://www.unccd.int/convention/about-convention (accessed on 25 December 2020).
- Patz, J.; Corvalan, C.; Horwitz, P.; Campbell-Lendrum, D. Our Planet, Our Health, Our Future: Human Health and the Rio Conventions: Biological Diversity, Climate Change and Desertification; World Health Organization: Geneva, Switzerland, 2012; Available online: https://www.who.int/globalchange/publications/reports/health_rioconventions.pdf?ua=1 (accessed on 17 October 2020).
- World Health Organization (WHO). Constitution of the World Health Organization; WHO: Geneva, Switzerland, 1948; Available online: http://apps.who.int/gb/bd/PDF/bd47/EN/constitution-en.pdf?ua=1 (accessed on 17 October 2020).
- Horton, R.; Beaglehole, R.; Bonita, R.; Raeburn, J.; McKee, M.; Wall, S. From public manifesto to planetary health: A manifesto. Lancet 2014, 383, 847. Available online: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(14)60409-8/fulltext (accessed on 17 October 2020). [CrossRef]
- Forouzanfar, M.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J.; et al. Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease. (GBD 2015 Risk Factors Collaborators). Lancet 2016, 388, 1659–1724. Available online: https://www.thelancet.com/action/showPdf?pii=S0140-6736%2816%2931679-8 (accessed on 17 October 2020).
- Landrigan, P.J.; Fuller, R.; Acosta, N.J.R.; Adeyi, O.; Arnold, R.; Basu, N.; Baldé, A.B.; Bertollini, R.; Bose-O’Reilly, S.; Boufford, J.I.; et al. The Lancet Commission on pollution and health. Lancet 2018, 391, 462–512. Available online: https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(17)32345-0.pdf?code=lancet-site (accessed on 17 October 2020). [CrossRef] [Green Version]
- Barbier, E.B. Poverty, development, and environment. In Environment and Development Economics; Cambridge University Press: Cambridge, UK, 2010; Volume 15, pp. 635–660. Available online: http://www.greengrowthknowledge.org/sites/default/files/Barbier,%20Edward%20-Poverty,%20development%20and%20environment%20(2010).pdf (accessed on 25 December 2020).
- World Health Organization (WHO). Operational Framework for Building Climate Resilient Health Systems; World Health Organization: Geneva, Switzerland, 2015; Available online: https://apps.who.int/iris/bitstream/handle/10665/189951/9789241565073_eng.pdf?sequence=1 (accessed on 17 October 2020).
- Barbier, E.B.; Hochard, J.P. Does Land Degradation Increase Poverty in Developing Countries? PLoS ONE 2016, 11, e0152973. Available online: https://journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0152973&type=printable (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- Berman, J.D.; Ebisu, K.; Peng, R.D.; Dominici, F.; Bell, M.L. Drought and the risk of hospital admissions and mortality in older adults in western USA from 2000 to 2013: A retrospective study. Lancet Planet. Health 2017, 1, e17–e25. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5646697/ (accessed on 17 October 2020). [CrossRef]
- Ebi, K.; Bowen, K. Extreme events as sources of health vulnerability: Drought as an example. Weather Clim. Extrem. 2016, 11, 95–102. Available online: https://www.sciencedirect.com/science/article/pii/S221209471530030X (accessed on 17 October 2020). [CrossRef] [Green Version]
- Beltrán, I.G.; Cuesta, J.G.; Trelles, M.; Jaweed, O.; Cherestal, S.; van Loenhout, J.A.F.; Guha-Sapir, D. Delays in arrival and treatment in emergency departments: Women, children and non-trauma consultations the most at risk in humanitarian settings. PLoS ONE 2019, 14, e0213362. Available online: https://doi.org/10.1371/journal.pone.0213362 (accessed on 17 October 2020).
- Sena, A. Land under pressure—Health under stress. In Global Land Outlook Working Paper; United Nations Convention to Combat Desertification (UNCCD): Bonn, Germany, 2019; Available online: https://knowledge.unccd.int/publication/land-under-pressure-health-under-stress (accessed on 25 December 2020).
- Intergovernmental Panel on Climate Change (IPCC). Climate change 2007: Impacts, adaptation and vulnerability. In Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change; Parry, M.L., Canziani, O.F., Palutikof, J.P., van der Linden, P.J., Hanson, C.E., Eds.; Cambridge University Press: Cambridge, UK, 2007; 976p, Available online: https://www.ipcc.ch/site/assets/uploads/2018/03/ar4_wg2_full_report.pdf (accessed on 17 October 2020).
- Smith, K.R.; Woodward, A.; Campbell-Lendrum, D.; Chadee, D.D.; Honda, Y.; Liu, Q.; Olwoch, J.M.; Revich, B.; Sauerborn, R. Human health: Impacts, adaptation, and co-benefits. In Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Field, B.C., Barros, V.R., Dokken, D.J., Mach, K.J., Mastrandrea, M.D., Bilir, T.E., Chatterjee, M., Ebi, K.L., Estrada, Y.O., Genova, R.C., et al., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2014; pp. 709–754. Available online: https://www.ipcc.ch/site/assets/uploads/2018/02/WGIIAR5-Chap11_FINAL.pdf (accessed on 17 October 2020).
- Haines, A.; Ebi, K. The Imperative for Climate Action to Protect Health. N. Engl. J. Med. 2019, 380, 263–273. Available online: https://www.nejm.org/doi/full/10.1056/NEJMra1807873 (accessed on 17 October 2020). [CrossRef]
- Haines, A. Addressing challenges to human health in the Anthropocene epoch—An overview of the findings of the Rockefeller/Lancet Commission on Planetary Health. Public Health Rev. 2016, 37, 14. Available online: https://publichealthreviews.biomedcentral.com/track/pdf/10.1186/s40985-016-0029-0 (accessed on 17 October 2020). [CrossRef] [Green Version]
- Lima-Camara, T.N. Emerging arboviruses and public health challenges in Brazil. Rev. Saude Publica 2016, 50, 36. Available online: http://www.scielo.br/pdf/rsp/v50/0034-8910-rsp-S1518-87872016050006791.pdf (accessed on 25 December 2020).
- Guterres, A.; Lemos, E.R.S. Hantaviruses and a neglected environmental determinant. One Health 2018, 5, 27–33. Available online: https://reader.elsevier.com/reader/sd/pii/S2352771417300526?token=C44F21B9A508E8D505878CEC4615F300FE4EF0670019CCA0ADC69254407645ACFCD65400D971949352EB2BC81655FBC4 (accessed on 17 October 2020). [CrossRef] [PubMed]
- Smith, L.T.; Aragão, L.E.; Sabel, C.E.; Nakaya, T. Drought impacts on children’s respiratory health in the Brazilian Amazon. Sci. Rep. 2014, 4, 3726. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3893650/ (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- Kriz, B.; Maly, M.; Benes, C.; Daniel, M. Epidemiology of tick-borne encephalitis in the Czech Republic 1970–2008. Vector Borne Zoonotic Dis. 2012, 12, 994–999. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3491623/ (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- Yun, S.I.; Lee, Y.M. Japanese encephalitis: The virus and vaccines. Hum. Vaccines Immunother. 2014, 10, 263–279. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4185882/ (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- Campbell, L.P.; Luther, C.; Moo-Llanes, D.; Ramsey, J.M.; Danis-Lozano, R.; Peterson, A.T. Climate change influences on global distributions of dengue and chikungunya virus vectors. Philos. Trans. R Soc. Lond. B Biol. Sci. 2015, 370, 20140135. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4342968/ (accessed on 17 October 2020). [CrossRef]
- Abiodun, G.J.; Maharaj, R.; Witbooi, P.; Okosun, K.O. Modelling the influence of temperature and rainfall on the population dynamics of Anopheles arabiensis. Malar. J. 2016, 15, 364. Available online: https://malariajournal.biomedcentral.com/track/pdf/10.1186/s12936-016-1411-6 (accessed on 17 October 2020). [CrossRef] [Green Version]
- Wahid, B.; Ali, A.; Rafique, S.; Idrees, M. Global expansion of chikungunya virus: Mapping the 64-year history. Int. J. Infect. Dis. 2017, 58, 69–76. Available online: https://www.ijidonline.com/article/S1201-9712(17)30089-9/pdf (accessed on 17 October 2020). [CrossRef] [Green Version]
- Beebe, N.; Cooper, R.; Mottram, P.; Sweeney, A. Australia’s dengue risk driven by human adaptation to climate change. PLoS Negl. Trop. Dis. 2009, 3, e429. Available online: https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0000429 (accessed on 17 October 2020). [CrossRef]
- Centers for Disease Control and Prevention (CDC); U.S. Environmental Protection Agency (EPA); National Oceanic and Atmospheric Agency (NOAA); American Water Works Association (AWWA). When every drop counts: Protecting public health during drought conditions—A guide for public health professionals. U.S. Department of Health and Human Services: Atlanta, GA, USA, 2010. Available online: https://www.cdc.gov/nceh/ehs/Docs/When_Every_Drop_Counts.pdf (accessed on 17 October 2020).
- Yusa, A.; Berry, P.; Cheng, J.; Ogden, N.; Bonsal, B.; Stewart, R.; Waldick, R. Climate change, drought and human health in Canada. Int. J. Environ. Res. Public Health 2015, 12, 8359–8412. Available online: https://www.mdpi.com/1660-4601/12/7/8359 (accessed on 17 October 2020). [CrossRef]
- World Health Organization (WHO). Climate-Resilient Water Safety Plans: Managing Health Risks Associated with Climate Variability and Change; World Health Organization: Geneva, Switzerland, 2017; Available online: https://apps.who.int/iris/bitstream/handle/10665/258722/9789241512794-eng.pdf;jsessionid=F4B5E121316C78D4BAB1C92FB4971F75?sequence=1 (accessed on 17 October 2020).
- Wilhite, D.; Sivakumar, M.; Pulwarty, R. Managing drought risk in a changing climate: The role of national drought policy. Weather Clim. Extrem. 2014, 3, 4–13. Available online: https://www.sciencedirect.com/science/article/pii/S2212094714000164 (accessed on 17 October 2020).
- Stanke, C.; Kerac, M.; Prudhomme, C.; Medlock, J.; Murray, V. Health Effects of Drought: A Systematic Review of the Evidence. PLoS Curr. Disasters 2013, 5, 5. Available online: http://currents.plos.org/disasters/index.html%3Fp=6221.html (accessed on 25 December 2020). [CrossRef] [PubMed] [Green Version]
- Sena, A.; Ebi, K.; Freitas, C.; Corvalan, C.; Barcellos, C. Indicators to measure risk of disaster associated with drought: Implications for the health sector. PLoS ONE 2017, 12, e0181394. Available online: https://journals.plos.org/plosone/article/comments?id=10.1371/journal.pone.0181394 (accessed on 17 October 2020). [CrossRef] [PubMed]
- World Water Assessment Programme (WWAP). The United Nations World Water Development Report 2016: Water and Jobs; United Nations World Water Assessment Programme; UNESCO: Paris, France, 2016; Available online: https://www.womenforwater.org/uploads/7/7/5/1/77516286/wwdr_2016_report_-_water_and_jobs.pdf (accessed on 17 October 2020).
- Jiménez Cisneros, B.E.; Oki, T.; Arnell, N.W.; Benito, G.; Cogley, J.G.; Döll, P.; Jiang, T.; Mwakalila, S.S. Freshwater resources. In Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Field, C.B., Barros, V.R., Dokken, D.J., Mach, K.J., Mastrandrea, M.D., Bilir, T.E., Chatterjee, M., Ebi, K.L., Estrada, Y.O., Genova, R.C., et al., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2014; pp. 229–269. Available online: https://www.ipcc.ch/site/assets/uploads/2018/02/WGIIAR5-Chap3_FINAL.pdf (accessed on 17 October 2020).
- McLeman, R. Migration and land Degradation: Recent experiences in future trends. In The Global Land Outlook Working Paper; United Nations Convention to Combat Desertification (UNCCD): Bonn, Germany, 2017; Available online: https://knowledge.unccd.int/sites/default/files/2018-06/8.%20Migration%2Band%2BLand%2BDegradation__R_McLeman.pdf (accessed on 25 December 2020).
- Berry, P.; Clarke, K.; Fleury, M.D.; Parker, S. Human health. In Canada in a Changing Climate: Sector Perspectives on Impacts and Adaptation; Warren, F.J., Lemmen, D.S., Eds.; Government of Canada: Ottawa, ON, Canada, 2014; pp. 191–232. Available online: https://www.nrcan.gc.ca/sites/www.nrcan.gc.ca/files/earthsciences/pdf/assess/2014/pdf/Chapter7-Human-Health_Eng.pdf (accessed on 17 October 2020).
- Hoy, W.; Giraldo, G.; Martinez, R.; Reveiz, L.; Ordunez, P. Setting the Context. In Epidemic of Chronic Kidney Disease in Agricultural Communities in Central America. Case definitions, methodological basis and approaches for public health surveillance; Hoy, W., Ordunez, P., Eds.; Pan American Health Organization (PAHO): Washington, DC, USA, 2017; Available online: http://iris.paho.org/xmlui/handle/123456789/34132 (accessed on 25 December 2020).
- Berry, H.; Bowen, K.; Kjellstrom, T. Climate change and mental health: A causal pathways framework. Int. J. Public Health 2010, 55, 123–132. Available online: https://link.springer.com/article/10.1007%2Fs00038-009-0112-0 (accessed on 17 October 2020). [CrossRef] [PubMed]
- Hanigan, I.C.; Butler, C.D.; Kokic, P.N.; Hutchinson, M.F. Suicide and drought in New South Wales, Australia, 1970–2007. Proc. Natl. Acad. Sci. USA 2012, 109, 13950–13955. Available online: https://www.pnas.org/content/pnas/109/35/13950.full.pdf (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- Obrien, L.V.; Berry, H.L.; Coleman, C.; Hanigan, I.C. Drought as a mental health exposure. Environ. Res. 2014, 131, 181–187. Available online: https://www.sciencedirect.com/science/article/pii/S0013935114000607?via%3Dihub (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- Vins, H.; Bell, J.; Saha, S.; Hess, J.J. The Mental Health Outcomes of Drought: A Systematic Review and Causal Process Diagram. Int. J. Environ. Res. Public Health 2015, 12, 13251–13275. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4627029/pdf/ijerph-12-13251.pdf (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- Sena, A.; Barcellos, C.; Freitas, C.; Corvalan, C. Managing the Health Impacts of Drought in Brazil. Int. J. Environ. Res. Public Health 2014, 11, 10737–10751. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4211003/pdf/ijerph-11-10737.pdf (accessed on 17 October 2020). [CrossRef] [Green Version]
- Alpino, T.A.; Sena, A.; Freitas, C. Disasters related to drought and public health—A review of the scientific literature. Ciência Saúde Coletiva 2016, 21, 809–820. Available online: http://www.scielo.br/pdf/csc/v21n3/en_1413-8123-csc-21-03-0809.pdf (accessed on 17 October 2020). [CrossRef] [Green Version]
- Sena, A.; Freitas, C.; Feitosa, S.P.; Carneiro, F.; Alpino, T.A.; Pedroso, M.; Corvalan, C.; Barcellos, C. Drought in the Semiarid Region of Brazil: Exposure, Vulnerabilities and Health Impacts from the Perspectives of Local Actors. PLoS Curr. Disasters 2018, 10. Available online: http://currents.plos.org/disasters/index.html%3Fp=40402.html (accessed on 25 December 2020). [CrossRef]
- McMichael, A.J. Drought, drying and mental health: Lessons from recent experiences for future risk-lessening policies. Aust. J. Rural Health 2011, 19, 227–228. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/j.1440-1584.2011.01217.x (accessed on 17 October 2020). [CrossRef]
- Edwards, B.; Gray, M.; Hunter, B. The impact of drought on mental health in rural and regional Australia. Soc. Indic. Res. 2015, 121, 177–194. Available online: https://link.springer.com/article/10.1007%2Fs11205-014-0638-2 (accessed on 17 October 2020). [CrossRef]
- Austin, E.K.; Handley, T.; Kiem, A.S.; Rich, J.L.; Lewin, T.J.; Askland, H.H.; Askarimarnani, S.S.; Perkins, D.A.; Kelly, B.J. Drought-related stress among farmers: Findings from the Australian Rural Mental Health Study. Med. J. Aust. 2018, 209, 159–165. Available online: https://www.mja.com.au/journal/2018/209/4/drought-related-stress-among-farmers-findings-australian-rural-mental-health (accessed on 17 October 2020). [CrossRef] [PubMed]
- Geere, J.-A.L.; Hunter, P.R.; Jagals, P. Domestic water carrying and its implications for health: A review and mixed methods pilot study in Limpopo Province, South Africa. Environ. Health 2010, 9, 52. Available online: https://ehjournal.biomedcentral.com/track/pdf/10.1186/1476-069X-9-52 (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- Zhang, J.; Mauzerall, D.L.; Zhu, T.; Liang, S.; Ezzati, M.; Remais, J.V. Environmental health in China: Progress towards clean air and safe water. Lancet 2010, 375, 1110–1119. Available online: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2810%2960062-1/fulltext (accessed on 17 October 2020). [CrossRef] [Green Version]
- Bartram, J.; Cairncross, S. Hygiene, Sanitation, and Water: Forgotten Foundations of Health. PLoS Med. 2010, 7, e1000367. Available online: https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1000367 (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- Lim, S.S.; Vox, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Anderson, H.R.; Andrews, K.G.; Aryee, M.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 15, 2224–2260. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4156511/ (accessed on 17 October 2020). [CrossRef] [Green Version]
- Stocks, M.E.; Ogden, S.; Haddad, D.; Addiss, D.G.; McGuire, C.; Freeman, M.C. Effect of water, sanitation, and hygiene on the prevention of trachoma: A systematic review and meta-analysis. PLoS Med. 2014, 11, e1001605. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3934994/pdf/pmed.1001605.pdf (accessed on 17 October 2020). [CrossRef] [Green Version]
- McMichael, A.J. Extreme weather events and infectious disease outbreaks. J. Virulence 2015, 6, 543–547. Available online: https://www.tandfonline.com/doi/full/10.4161/21505594.2014.975022 (accessed on 17 October 2020). [CrossRef] [Green Version]
- World Health Organization (WHO); United Nations Children’s Fund (UNICEF); United States Agency International Development (USAID). Improving Nutrition Outcomes with Better Water, Sanitation and Hygiene: Practical Solutions for Policies and Programmes; World Health Organization: Geneva, Switzerland, 2015; Available online: https://apps.who.int/iris/bitstream/handle/10665/193991/9789241565103_eng.pdf?sequence=1 (accessed on 17 October 2020).
- Prüss-Üstün, A.; Wolf, J.; Corvalan, C.; Bos, R.; Neira, M.P. Preventing Disease Through Healthy Environments: A Global Assessment of the Burden of Disease from Environmental Risks; World Health Organization: Geneva, Switzerland, 2016; Available online: https://apps.who.int/iris/handle/10665/204585 (accessed on 25 December 2020).
- United Nations Environment Programme (UNEP). Measuring Water Use in a Green Economy: A Report of the Working Group on Water Efficiency to the International Resource Panel; McGlade, J., Werner, B., Young, M., Matlock, M., Jefferies, D., Sonnemann, G., Aldaya, M., Pfister, S., Berger, M., Farell, C., et al., Eds.; United Nations Environment Programme (UNEP): Nairobi, Kenya, 2012; Available online: https://waterfootprint.org/media/downloads/UNEP-2012-MeasuringWaterUse_1.pdf (accessed on 17 October 2020).
- World Health Organization (WHO); United Nations Children’s Fund (UNICEF). Progress on Drinking Water, Sanitation and Hygiene: 2017 Update and SDG Baselines; World Health Organization (WHO); United Nations Children’s Fund (UNICEF): Geneva, Switzerland, 2017; Available online: https://www.who.int/mediacentre/news/releases/2017/launch-version-report-jmp-water-sanitation-hygiene.pdf (accessed on 17 October 2020).
- World Health Organization (WHO). Mortality and Burden of Disease from Water and Sanitation; Global Health Observatory Data; World Health Organization: Geneva, Switzerland, 2016; Available online: https://www.who.int/gho/phe/water_sanitation/burden_text/en/ (accessed on 17 October 2020).
- World Health Organization (WHO). Diarrhoeal Diseases; Key Factors; World Health Organization: Geneva, Switzerland, 2017; Available online: https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease (accessed on 17 October 2020).
- Food and Agriculture Organization of the United Nations (FAO). The State of Food and Agriculture 2018. Migration, Agriculture and Rural Development; Food and Agriculture Organization of the United Nations: Rome, Italy, 2018; Available online: http://www.fao.org/3/I9549EN/i9549en.pdf (accessed on 25 December 2020).
- Food and Agriculture Organization of the United Nations (FAO). The Future of Food and Agriculture—Trends and Challenges; Food and Agriculture Organization of the United Nations: Rome, Italy, 2017; Available online: http://www.fao.org/3/a-i6583e.pdf (accessed on 17 October 2020).
- Food and Agriculture Organization of the United Nations (FAO). The Impact of Natural Hazards and Disasters on Agriculture and Food Security and Nutrition: A Call for Action to Build Resilient Livelihoods; Food and Agriculture Organization of the United Nations: Rome, Italy, 2015; p. 16. Available online: http://www.fao.org/3/a-i4434e.pdf (accessed on 17 October 2020).
- Compton, J.; Wiggins, S.; Keats, S. Impact of the Global Food Crisis on the Poor: What is the Evidence? Overseas Development Institute; UK Department for International Development: London, UK, 2010. Available online: https://www.odi.org/sites/odi.org.uk/files/odi-assets/publications-opinion-files/6371.pdf (accessed on 17 October 2020).
- Green, R.; Cornelsen, L.; Dangour, A.D.; Turner, R.; Shankar, B.; Mazzocchi, M.; Smith, R.D. The effect of rising food prices on food consumption: Systematic review with meta-regression. BMJ 2013, 346, f3703. Available online: https://www.bmj.com/content/346/bmj.f3703 (accessed on 17 October 2020). [CrossRef] [Green Version]
- Food and Agriculture Organization of the United Nations (FAO); International Fund for Agricultural Development (IFAD); United Nations Children’s Fund (UNICEF); World Fund Programme (WFP); World Health Organization (WHO). The State of Food Security and Nutrition in the World 2018; Building Climate Resilience for Food Security and Nutrition; FAO: Rome, Italy, 2018; Available online: http://www.fao.org/3/i9553en/i9553en.pdf (accessed on 17 October 2020).
- United Nations (UN). Water Security & the Global Water Agenda: A UN-Water Analytical Brief; United Nations University: Hamilton, ON, Canada, 2013; Available online: https://www.unwater.org/publications/water-security-global-water-agenda/ (accessed on 25 December 2020).
- Alexander, K.A.; Carzolio, M.; Goodin, D.; Vance, E. Climate change is likely to worsen the public health threat of diarrheal disease in Botswana. Int. J. Environ. Res. Public Health 2013, 10, 1202–1230. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709313/ (accessed on 17 October 2020). [CrossRef]
- Horn, L.M.; Hajat, A.; Sheppard, L.; Quinn, C.; Colborn, J.; Zermoglio, M.F.; Gudo, E.S.; Marrufo, T.; Ebi, K. Association between Precipitation and Diarrheal Disease in Mozambique. Int. J. Environ. Res. Public Health 2018, 15, 709. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5923751/ (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- United Nations Environment Programme (UNEP). Towards a Pollution-Free Planet Background Report; United Nations Environment Programme: Nairobi, Kenya, 2017; Available online: http://wedocs.unep.org/bitstream/handle/20.500.11822/21800/UNEA_towardspollution_long%20version_Web.pdf?sequence=1&isAllowed=y (accessed on 17 October 2020).
- Obrador, G.T.; Schultheiss, U.T.; Kretzler, M.; Langham, R.G.; Nangaku, M.; Pecoits-Filho, R.; Pollock, C.; Rossert, J.; Correa-Rotter, R.; Stenvinkel, P.; et al. Genetic and environmental risk factors for chronic kidney disease. Kidney Int. Suppl. 2017, 7, 88–106. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6341015/ (accessed on 17 October 2020). [CrossRef] [PubMed]
- Bernard, A. Cadmium and its adverse effects on human health. Ind. J. Med. Res. 2008, 128, 557–564. Available online: https://www.ncbi.nlm.nih.gov/pubmed/19106447 (accessed on 17 October 2020).
- Lam, H.M.; Remais, J.; Fung, M.C.; Xu, L.; Sun, S.S. Food supply and food safety issues in China. Lancet 2013, 381, 2044–2053. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3888022/ (accessed on 17 October 2020). [CrossRef] [Green Version]
- World Health Organization (WHO). Lead Poisoning and Health; World Health Organization: Geneva, Switzerland, 2019; Available online: https://www.who.int/news-room/fact-sheets/detail/lead-poisoning-and-health (accessed on 17 October 2020).
- Porter, J.R.; Xie, L.; Challinor, A.J.; Cochrane, K.; Howden, S.M.; Iqbal, M.M.; Lobell, D.B.; Travasso, M.I. Food security and food production systems. In Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Field, B.C., Barros, V.R., Dokken, D.J., Mach, K.J., Mastrandrea, M.D., Bilir, T.E., Chatterjee, M., Ebi, K.L., Estrada, Y.O., Genova, R.C., et al., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2014; pp. 485–533. Available online: https://www.ipcc.ch/site/assets/uploads/2018/02/WGIIAR5-Chap7_FINAL.pdf (accessed on 17 October 2020).
- World Health Organization (WHO). Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death, 2030 and 2050s; World Health Organization: Geneva, Switzerland, 2014; Available online: https://apps.who.int/iris/bitstream/handle/10665/134014/9789241507691_eng.pdf?sequence=1 (accessed on 17 October 2020).
- Jones, K.D.; Thitiri, J.; Ngari, M.; Berkley, J.A. Childhood malnutrition: Toward an understanding of infections, inflammation, and antimicrobials. Food Nutr. Bull. 2014, 35 (Suppl. S2), S64–S70. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4257992/ (accessed on 17 October 2020). [CrossRef] [Green Version]
- United Nations Children’s Fund (UNICEF); World Health Organization (WHO); International Bank for Reconstruction and Development/The World Bank (WB). Levels and Trends in Child Malnutrition: Key Findings of the 2020 Edition of the Joint Child Malnutrition Estimates; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications-detail/jme-2020-edition (accessed on 17 October 2020).
- Black, R.E.; Victora, C.G.; Walker, S.P.; Zulfiqar, A.B.; Christian, P.; deOnis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorelli, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 3, 427–451. Available online: https://www.ncbi.nlm.nih.gov/pubmed/23746772 (accessed on 17 October 2020). [CrossRef]
- Campbell, O.M.; Benova, L.; Gon, G.; Afsana, K.; Cumming, O. Getting the basic rights—The role of water, sanitation and hygiene in maternal and reproductive health: A conceptual framework. Trop. Med. Int. Health 2015, 20, 252–267. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4681319/pdf/tmi0020-0252.pdf (accessed on 17 October 2020). [CrossRef] [Green Version]
- Malley, C.S.; Kuylenstierna, J.C.I.; Vallack, H.W.; Henze, D.K.; Blencowe, H.; Ashmore, M.R. Preterm birth associated with maternal fine particulate matter exposure: A global, regional and national assessment. Environ. Int. 2017, 101, 173–182. Available online: https://www.sciencedirect.com/science/article/pii/S0160412016305992?via%3Dihub (accessed on 17 October 2020). [CrossRef]
- United Nations Children’s Fund (UNICEF); World Health Organization (WHO); International Bank for Reconstruction and Development/The World Bank (WB). Levels and Trends in Child Malnutrition: Key Findings of the 2019 Edition of the Joint Child Malnutrition Estimates; World Health Organization: Geneva, Switzerland, 2019; Available online: https://www.who.int/nutgrowthdb/jme-2019-key-findings.pdf?ua=1 (accessed on 17 October 2020).
- Chapman, E.; Haby, M.M.; Illanes, E.; Sanchez-Viamonte, J.; Elias, V.; Reveiz, L. Risk factors for chronic kidney disease of non-traditional causes: A systematic review. Rev. Panam. Salud Publica 2019, 43, e35. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6461065/ (accessed on 17 October 2020). [CrossRef] [Green Version]
- Goudie, A.S. Desert dust and human health disorders. Environ. Int. 2014, 63, 101–113. Available online: https://doi.org/10.1016/j.envint.2013.10.011 (accessed on 17 October 2020). [CrossRef]
- United Nations Environment Programme (UNEP); World Meteorological Organization (WMO); The United Nations Convention to Combat Desertification (UNCCD). Global Assessment of Sand and Dust Storms; The United Nations Convention to Combat Desertification: Nairobi, Kenya, 2016; Available online: http://catalogue.unccd.int/765_Global_assessment_sand_dust_storms_2016.pdf (accessed on 17 October 2020).
- Millennium Ecosystem Assessment. Ecosystems and Human Well-being: Synthesis; Island Press: Washington, DC, USA, 2005; Available online: https://www.millenniumassessment.org/documents/document.356.aspx.pdf (accessed on 17 October 2020).
- Nourmoradi, H.; Moradnejadi, K.; Moghadam, F.M.; Khosravi, B.; Lida Hemati, L.; Ramin Khoshniyat, R.; Kazembeigi, F. The Effect of Dust Storm on the Microbial Quality of Ambient Air in Sanandaj: A City Located in the West of Iran. Glob. J. Health Sci. 2015, 7, 114–119. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4803936/ (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- Beggs, P.J. Adaptation to impacts of climate change on aeroallergens and allergic respiratory diseases. Int. J. Environ. Res. Public Health 2010, 7, 3006–3021. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2954564/pdf/ijerph-07-03006.pdf (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- Intergovernmental Panel on Climate Change (IPCC). Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Stocker, T.F., Qin, D., Plattner, G.-K., Tignor, M., Allen, S.K., Boschung, J., Nauels, A., Xia, Y., Bex, V., Midgley, P.M., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2013; 1535p, Available online: http://www.climatechange2013.org/report/full-report/ (accessed on 17 October 2020).
- Xu, R.; Yu, P.; Abramson, M.J.; Johnston, F.H.; Samet, J.M.; Bell, M.L.; Haines, A.; Ebi, K.; Li, S.; Guo, Y. Wildfires, Global Climate Change, and Human Health. N. Engl. J. Med. 2020. Available online: https://www.nejm.org/doi/full/10.1056/NEJMsr2028985 (accessed on 17 October 2020).
- Finlay, S.E.; Moffat, A.; Gazzard, R.; Baker, D.; Murray, V. Health Impacts of Wildfires. PLoS Curr. Disasters 2012, 4, e4f959951cce2c. Available online: https://currents.plos.org/disasters/index.html%3Fp=1881.html (accessed on 25 December 2020). [CrossRef] [PubMed]
- Handmer, J.; Honda, Y.; Kundzewicz, Z.W.; Arnell, N.; Benito, G.; Hatfield, J.; Mohamed, I.F.; Peduzzi, P.; Wu, S.; Sherstyukov, B.; et al. Changes in impacts of climate extremes: Human systems and ecosystems. In Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation; A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change, (IPCC); Field, C.B., Barros, V., Stocker, T.F., Qin, D., Dokken, D.J., Ebi, K.L., Mastrandrea, M.D., Mach, K.J., Plattner, G.-K., Allen, S.K., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2012; pp. 231–290. Available online: https://www.ipcc.ch/site/assets/uploads/2018/03/SREX-Chap4_FINAL-1.pdf (accessed on 17 October 2020).
- Johnston, F.H.; Henderson, S.B.; Chen, Y.; Randerson, J.T.; Marlier, M.; DeFries, R.S.; Kinney, P.; Bowman, D.M.J.S.; Brauer, M. Estimated Global Mortality Attributable to Smoke from Landscape Fires. Environ. Health Perspect. 2012, 120, 695–701. Available online: https://ehp.niehs.nih.gov/doi/pdf/10.1289/ehp.1104422 (accessed on 25 December 2020). [CrossRef] [PubMed] [Green Version]
- Portier, C.J.; Thigpen, T.K.; Carter, S.R.; Dilworth, C.H.; Grambsch, A.E.; Gohlke, J.; Hess, J.; Howard, S.N.; Luber, G.; Lutz, J.T.; et al. A Human Health Perspective on Climate Change: A Report Outlining the Research Needs on the Human Health Effects of Climate Change; Environmental Health Perspectives/National Institute of Environmental Health Sciences: Research Triangle Park, NC, USA, 2010. Available online: www.niehs.nih.gov/climatereport (accessed on 17 October 2020).
- Tóth, G.; Hermann, T.; Da Silva, M.; Montanarella, L. Heavy metals in agricultural soils of the European Union with implications for food safety. Environ. Int. 2016, 88, 299–309. Available online: https://www.sciencedirect.com/science/article/pii/S0160412015301203 (accessed on 17 October 2020). [CrossRef] [PubMed]
- Molesworth, A.M.; Cuevas, L.E.; Connor, S.J.; Morse, A.P.; Thomson, M.C. Environmental Risk and Meningitis Epidemics in Africa. Emerg. Infect. Dis. 2003, 9, 1287–1293. Available online: https://dx.doi.org/10.3201/eid0910.030182 (accessed on 17 October 2020). [CrossRef] [PubMed]
- World Health Organization (WHO). Meningitis outbreak response in sub-Saharan Africa. In WHO Guideline; World Health Organization: Geneva, Switzerland, 2014. Available online: https://www.ncbi.nlm.nih.gov/books/NBK274197/ (accessed on 17 October 2020).
- Grineski, S.E.; Staniswalis, J.G.; Bulathsinhala, P.; Peng, Y.; Gill, T.E. Hospital admissions for asthma and acute bronchitis in El Paso, Texas: Do age, sex, and insurance status modify the effects of dust and low wind events? Environ. Res. 2011, 111, 1148–1155. Available online: https://www.ncbi.nlm.nih.gov/pubmed/21782162 (accessed on 17 October 2020). [CrossRef] [Green Version]
- Sajani, S.Z.; Miglio, R.; Bonasoni, P.; Cristofanelli, P.; Marinoni, A.; Sartini, C.; Goldoni, C.A.; De Girolamo, G.; Lauriola, P. Saharan dust and daily mortality in Emilia-Romagna (Italy). Occup. Environ. Med. 2011, 68, 446–451. Available online: https://oem.bmj.com/content/oemed/68/6/446.full.pdf (accessed on 17 October 2020). [CrossRef] [Green Version]
- Jiménez, E.; Linares, C.; Martinéz, D.; Díaz, J. Role of Saharan dust in the relationship between particulate matter and short-term daily mortality among the elderly in Madrid (Spain). Sci. Total Environ. 2010, 408, 5729–5736. Available online: https://www.sciencedirect.com/science/article/pii/S0048969710009101?via%3Dihub (accessed on 17 October 2020). [CrossRef]
- Food and Agriculture Organization of the United Nations (FAO). Voluntary Guidelines for Sustainable Soil Management; Food and Agriculture Organization of the United Nations: Rome, Italy, 2017; Available online: http://www.fao.org/3/a-bl813e.pdf (accessed on 17 October 2020).
- Food and Agriculture Organization of the United Nations (FAO). Global Soil Partnership, 2018, Polluting Our Soils Is Polluting Our Future; Food and Agriculture Organization of the United Nations: Rome, Italy, 2018; Edited on 7 May 2018; Available online: http://www.fao.org/global-soil-partnership/resources/highlights/detail/en/c/1127952/ (accessed on 25 December 2020).
- United Nations Convention to Combat Desertification (UNCCD). The Global Land Outlook, 1st ed.; United Nations Convention to Combat Desertification: Bonn, Germany, 2017; Available online: https://knowledge.unccd.int/sites/default/files/2018-06/GLO%20English_Full_Report_rev1.pdf (accessed on 17 October 2020).
- United Nations Convention to Combat Desertification (UNCCD). Threats to Soils: Global Trends and Perspectives. A contribution from the Intergovernmental Technical Panel on Soils, Global Soil Partnership Food and Agriculture Organization of the United Nations. In Global Land Outlook Working Paper; Pierzynski, G., Brajendra, Eds.; United Nations Convention to Combat Desertification: Bonn, Germany, 2017; Available online: https://knowledge.unccd.int/sites/default/files/2018-06/17.%20Threats%2Bto%2BSoils__Pierzynski_Brajendra.pdf (accessed on 25 December 2020).
- Rodríguez-Eugenio, N.; McLaughlin, M.; Pennock, D. Soil Pollution: A Hidden Reality; FAO: Rome, Italy, 2018; 142p, Available online: http://www.fao.org/3/I9183EN/i9183en.pdf (accessed on 17 October 2020).
- Dooyema, C.A.; Neri, A.; Lo, Y.C.; Durant, J.; Dargan, P.I.; Swarthout, T.; Biya, O.; Gidado, S.O.; Haladu, S.; Sani-Gwarzo, N.; et al. Outbreak of fatal childhood lead poisoning related to artisanal gold mining in northwestern Nigeria, 2010. Environ. Health Perspect. 2012, 120, 601–607. Available online: https://www.ncbi.nlm.nih.gov/pubmed/22186192 (accessed on 17 October 2020). [CrossRef] [Green Version]
- Oviatt, K.; Brett, J. The intrinsic link of vulnerability to sustainable development. In Social Vulnerability to Disasters; Phillips, B., Thomas, D., Fothergill, A., Blinn-Pike, L., Eds.; CRC Press: Boca Raton, FL, USA, 2010. [Google Scholar]
- Cardona, O.-D.; van Aalst, M.K.; Birkmann, J.; Fordham, M.; McGregor, G.; Perez, R.; Pulwarty, R.S.; Schipper, E.L.F.; Sinh, B.T. Determinants of risk: Exposure and vulnerability. In Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation; A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change; Field, C.B., Barros, V., Stocker, T., Dahe, Q., Dokken, D., Ebi, K., Mastrandrea, M.D., Mach, K.J., Plattner, G.-K., Allen, S.K., et al., Eds.; Intergovernmental Panel on Climate Change: Cambridge, UK; New York, NY, USA, 2012; pp. 65–108. Available online: https://www.ipcc.ch/site/assets/uploads/2018/03/SREX-Chap2_FINAL-1.pdf (accessed on 17 October 2020).
- Hallegate, S.; Fay, M.; Barbier, E.B. Poverty and climate change: Introduction. Environ. Dev. Econ. 2018, 23, 217–233. Available online: https://www.cambridge.org/core/journals/environment-and-development-economics/article/poverty-and-climate-change-introduction/EAE3DA276184ED0DAEE6062E5DB0DB17 (accessed on 17 October 2020). [CrossRef] [Green Version]
- Peters, D.H.; Garg, A.; Bloom, G.; Walker, D.G.; Brieger, W.R.; Hafizur, R.M. Poverty and access to health care in developing countries. Ann. N. Y. Acad. Sci. 2008, 25, 161–171. Available online: https://nyaspubs.onlinelibrary.wiley.com/doi/epdf/10.1196/annals.1425.011 (accessed on 17 October 2020). [CrossRef] [PubMed]
- United Nations secretariat of the International Strategy for Disaster Reduction (UNISDR). Drought Risk Reduction Framework and Practices: Contributing to the Implementation of the Hyogo Framework for Action; United Nations secretariat of the International Strategy for Disaster Reduction: Geneva, Switzerland, 2009; 2013p, Available online: http://www.unisdr.org/files/11541_DroughtRiskReduction2009library.pdf (accessed on 17 October 2020).
- Bultó, P.L.; Rodríguez, A.P.; Valencia, A.R.; Vega, N.L.; Gonzalez, M.D.; Carrera, A.P. Assessment of human health vulnerability to climate variability and change in Cuba. Environ. Health Perspect. 2006, 114, 1942–1949. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1764156/ (accessed on 17 October 2020). [CrossRef] [PubMed]
- Scandlyn, J.; Simon, C.N.; Thomas, D.S.K.; Brett, J. Theorical framing of worldviews, values, and structural dimensions of disasters. In Social Vulnerability to Disasters; Phillips, B., Thomas, D., Fothergill, A., Blinn-Pike, L., Eds.; CRC Press: Boca Raton, FL, USA, 2010; pp. 27–49. [Google Scholar]
- Freitas, C.; Carvalho, M.L.; Ximenes, E.F.; Arraes, E.F.; Gomes, J.O. Vulnerabilidade socioambiental, redução de riscos de desastres e construção da resiliência: Lições do terremoto no Haiti e das chuvas fortes na Região Serrana, Brasil. Ciênc Saúde Coletiva 2012, 17, 1577–1586. Available online: http://www.scielo.br/pdf/csc/v17n6/v17n6a21.pdf (accessed on 17 October 2020). [CrossRef] [PubMed] [Green Version]
- Ford, J.D. Indigenous health and climate change. Am. J. Public Health 2012, 102, 1260–1266. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3477984/pdf/AJPH.2012.300752.pdf (accessed on 17 October 2020). [CrossRef] [PubMed]
- Corrarino, J.E. Health Literacy and Women’s Health: Challenges and Opportunities. J. Midwifery Women’s Health 2013, 58, 257–264. Available online: https://www.ncbi.nlm.nih.gov/pubmed/23631442 (accessed on 17 October 2020). [CrossRef] [PubMed]
- World Health Organization (WHO). Gender, Climate Change and Health; World Health Organization: Geneva, Switzerland, 2014; Available online: https://www.who.int/globalchange/GenderClimateChangeHealthfinal.pdf (accessed on 17 October 2020).
- United Nations (UN). The World’s Women 2015: Trends and Statistics; Sales No. E.15.XVII.8; United Nations, Department of Economic and Social Affairs, Statistics Division: New York, NY, USA, 2015; Available online: https://unstats.un.org/unsd/gender/downloads/worldswomen2015_report.pdf (accessed on 17 October 2020).
- Stain, H.J.; Kelly, B.; Carr, V.J.; Lewin, T.J.; Fitzgerald, M.; Fragar, L. The psychological impact of chronic environmental adversity: Responding to prolonged drought. Soc. Sci. Med. 2011, 73, 1593–1599. Available online: https://www.ncbi.nlm.nih.gov/pubmed/22005316 (accessed on 17 October 2020). [CrossRef]
- Sena, A.; Freitas, C.; Eliane, L.S.; Corvalan, C. Atuação do setor saúde frente a situações de seca. In Il. (Série Desenvolvimento Sustentável e Saúde, 3); Organização Pan-Americana de Saúde/Organização Mundial de Saúde (OPAS-Brasil); Ministério da Saúde (MS-Brasil): Brasília, Brazil, 2015; 52p, Available online: https://iris.paho.org/handle/10665.2/18468 (accessed on 17 October 2020).
- Neumann, K.; Sietz, D.; Hilderink, H.; Janssen, P.; Kok, M.; van Dijk, H. Environmental drivers of human migration in drylands—A spatial picture. Appl. Geogr. 2015, 56, 116–126. Available online: http://agris.fao.org/agris-search/search.do?recordID=US201900060291 (accessed on 17 October 2020). [CrossRef]
- United Nations Office for Disaster Risk Reduction (UNISDR). Sendai Framework for Disaster Risk Reduction 2015–2030; United Nations Office for Disaster Risk Reduction: Geneva, Switzerland, 2015; Available online: https://www.preventionweb.net/files/43291_sendaiframeworkfordrren.pdf (accessed on 17 October 2020).
- International Organization for Migration (IOM). World Migration Report 2018; International Organization for Migration/ The UN Migration Agency: Geneva, Switzerland, 2018; Available online: https://www.iom.int/sites/default/files/country/docs/china/r5_world_migration_report_2018_en.pdf (accessed on 25 December 2020).
- United Nations Convention to Combat Desertification (UNCCD). The Land in Numbers: Livelihoods at a Tipping Point; Secretariat of the United Nations Convention to Combat Desertification: Bonn, Germany, 2014; Available online: https://www.unccd.int/sites/default/files/documents/Land_In_Numbers_web.pdf (accessed on 17 October 2020).
- Lavell, A.; Oppenheimer, M.; Diop, C.; Hess, J.; Lempert, R.; Li, J.; Muir-Wood, R.; Myeong, S. Climate change: New dimensions in disaster risk, exposure, vulnerability, and resilience. In Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation; A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change; Field, C.B., Barros, V., Stocker, T., Qin, D., Dokken, D., Ebi, K., Mastrandrea, M.D., Mach, K.J., Plattner, G.-K., Allen, S.K., et al., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2012; pp. 25–64. Available online: https://www.ipcc.ch/site/assets/uploads/2018/03/SREX-Chap1_FINAL-1.pdf (accessed on 17 October 2020).
- Kjellstrom, T.; McMichael, A.J. Climate change threats to population health and well-being: The imperative of protective solutions that will last. Glob. Health Action 2013, 6, 20816, Correction in Glob. Health Action 2014, 7, 25010. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3617647/pdf/GHA-6-20816.pdf (accessed on 17 October 2020). [CrossRef]
- Zezza, A.; Carletto, C.; Davis, B.; Winters, P. Assessing the impact of migration on food and nutrition security. Food Policy 2011, 36, 1–6. Available online: https://openknowledge.worldbank.org/handle/10986/5037 (accessed on 17 October 2020). [CrossRef]
- United Nations Convention to Combat Desertification (UNCCD). Land-Based Adaptation and Resilience: Powered by Nature; Secretariat of the United Nations Convention to Combat Desertification: Bonn, Germany, 2014; Available online: http://catalogue.unccd.int/856_Land_Based_Adaptation_ENG.pdf (accessed on 25 December 2020).
- Kravitz, J.D. Drought: A global environmental concern. Lancet/Planet. Health 2017, 1, e130–e131. Available online: https://doi.org/10.1016/S2542-5196(17)30043-8 (accessed on 25 December 2020). [CrossRef]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. Available online: https://www.thelancet.com/action/showPdf?pii=S0140-6736%2818%2931788-4 (accessed on 17 October 2020). [CrossRef]
- United Nations, Department of Economic and Social Affairs, Population Division (2019). World Population Prospects 2019: Highlights (ST/ESA/SER.A/423); United Nations: New York, NY, USA, 2019; Available online: https://population.un.org/wpp/Publications/Files/WPP2019_Highlights.pdf (accessed on 25 December 2020).
- United Nations, Department of Economic and Social Affairs, Population Division (2019). Department of Economic and Social Affairs/Population Division. World Population Prospects 2019; United Nations: New York, NY, USA, 2019; Available online: https://population.un.org/wpp/Download/Probabilistic/Population/ (accessed on 25 December 2020).
- Food and Agriculture Organization of the United Nations (FAO). The State of the World’s Land and Water Resources for Food and Agriculture (SOLAW)—Managing Systems at Risk; Food and Agriculture Organization of the United Nations: Rome, Italy; Earthscan: London, UK, 2011; Available online: http://www.fao.org/3/i1688e/i1688e.pdf? (accessed on 17 October 2020).
- Chiabai, A.; Quiroga, S.; Martinez-Juarez, P.; Higgins, S.; Taylor, T. The nexus between climate change, ecosystem services and human health: Towards a conceptual framework. Sci. Total Environ. 2018, 635, 1191–1204. Available online: https://doi.org/10.1016/j.scitotenv.2018.03.323 (accessed on 17 October 2020). [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Preparing for the Health Effects of Drought: A Resource Guide for Public Health Professionals; Centers for Disease Control and Prevention, U.S. National Center for Environmental Health: Atlanta, GA, USA, 2018. Available online: https://www.cdc.gov/nceh/hsb/cwh/docs/CDC_Drought_Resource_Guide-508.pdf (accessed on 17 October 2020).
- World Health Organization Regional Office for the Western Pacific (WHO/WPRO). Western Pacific Regional Framework for Action on Health and Environment on a Changing Planet; World Health Organization Regional Office for the Western Pacific: Manila, Philippines, 2017; Available online: https://iris.wpro.who.int/bitstream/handle/10665.1/13653/9789290618164-eng.pdf (accessed on 17 October 2020).
- World Health Organization (WHO). Health in All Policies: Helsinki Statement; Framework for Country Action; World Health Organization: Geneva, Switzerland, 2014; Available online: https://apps.who.int/iris/bitstream/handle/10665/112636/9789241506908_eng.pdf?sequence=1 (accessed on 17 October 2020).
- Shiferaw, B.; Tesfaye, K.; Kassie, M.; Abate, T.; Prasanna, B.M.; Menkir, A. Managing vulnerability to drought and enhancing livelihood resilience in sub-Saharan Africa: Technological, institutional and policy options. Weather Clim. Extrem. 2014, 3, 67–79. Available online: https://www.sciencedirect.com/science/article/pii/S2212094714000280 (accessed on 17 October 2020). [CrossRef] [Green Version]
- Alston, M. Synthesis paper on socioeconomic factors relating to agriculture and community development. Crop Pasture Sci. 2012, 63, 232–239. Available online: http://www.publish.csiro.au/cp/pdf/CP11173 (accessed on 17 October 2020). [CrossRef] [Green Version]
- World Health Organization (WHO). Protecting Health from Climate Change: Vulnerability and Adaptation Assessment; World Health Organization: Geneva, Switzerland, 2013; Available online: http://www.who.int/iris/handle/10665/104200 (accessed on 17 October 2020).
- Slater, R.; Holmes, R.; Mathers, N. Food and Nutrition (in-)Security and Social Protection; OECD Development Co-operation Working Papers; No. 15; OECD: Paris, France, 2014; Available online: http://www.indiaenvironmentportal.org.in/files/file/Food%20and%20Nutrition%20(in-)Security%20and%20Social%20Protection.pdf (accessed on 25 December 2020).
- Crossman, N.D. Drought Resilience, Adaptation and Management Policy (DRAMP) Framework; UNCCD: Bonn, Germany, 2018; Available online: https://www.unccd.int/sites/default/files/relevant-links/2018-08/DRAMP_Policy_Framework.pdf (accessed on 25 December 2020).
- United Nations Educational, Scientific and Cultural Organization (UNESCO). Leaving no one behind: How far on the way to universal primary and secondary education? Institute for Statistics (UIS) and the Global Education Monitoring (GEM) Report. Policy paper 27/Fact Sheet 37; UNESCO: Paris, France, 2016; Available online: http://uis.unesco.org/sites/default/files/documents/fs37-leaving-no-one-behind-how-far-on-the-way-to-universal-primary-and-secondary-education-2016-en.pdf (accessed on 25 December 2020).
- Grigoletto, J.C.; Cabral, A.R.; Bonfim, C.V.; Rohlfs, D.B.; Silva, E.L.; DeQueiroz, F.B.; Francischetti, J.; Daniel, M.H.B.; Resende, R.M.S.; Andrade, R.C.; et al. Management of health sector actions in drought situations. Ciência Saúde Coletiva 2016, 21, 709–718. Available online: http://www.scielo.br/pdf/csc/v21n3/en_1413-8123-csc-21-03-0709.pdf (accessed on 17 October 2020). [CrossRef]
- Gibbs, H.K.; Salmon, J.M. Mapping the world’s degraded lands. Appl. Geogr. 2015, 57, 12–21. Available online: https://www.sciencedirect.com/science/article/pii/S0143622814002793?via%3Dihub (accessed on 17 October 2020). [CrossRef]
| DLDD Drivers | Environmental and Social Pathways | Human Health Impacts (Morbidity and Mortality) |
|---|---|---|
| Water Security and Safety | Water shortage Consequences of water quality (non-potable water, saline water) Contamination of water by various means, such as toxic algal blooms, bacteria, fungi, virus, toxins, chemical pollutants Damages to health services functioning, with consequences to the provision of some sanitary procedures Consequences on the water supply and distribution system (for piped water, water trucks, cisterns, artesian wells, dams and other alternative sources) Household water collection and storage, which may compromise water quality Water collection and transport (which may cause physical injuries) Change in vectors, hosts and reservoir cycles Effect on irrigation for agricultural production and in livestock and fishing increasing the possibility of food shortages Impaired hygiene (personal, household, food, health service equipment) due to lack of water Consequences of sanitation services, urban cleaning, health services and other basic services | Gastrointestinal infectious diseases (diarrhea, hepatitis A, typhoid fever, and other infections) Parasitic infections (intestinal nematodes infections) Dermatological infectious diseases (scabies) Diseases transmitted by vectors and zoonoses (e.g., dengue, Zika, chikungunya, malaria, leishmaniasis, leptospirosis) Infectious diseases transmitted by viruses, bacteria, fungi (flu, pneumonia, conjunctivitis, trachoma, scabies, and other diseases) Cardiovascular diseases (e.g., hypertension) Kidney diseases Cancers (esophageal cancer) Dehydration Undernutrition Unintentional injuries (poisoning by toxins) Musculoskeletal disorders (bone damage, back and muscle pain) Mental and behavioral disorders (stress, anxiety, depression) |
| Food Security and Safety | Deficiency in agricultural, livestock and fishery production causing food shortages Difficulty in the sustainability of family agriculture, livestock and fishery Food contamination (microbiological and chemical) Rising food prices Decreased access to food, especially to healthy food | Nutritional deficiencies (anemia, night blindness, scurvy) Malnutrition and its complications (low physical and cognitive development, deficiency of the immune system, overweight) Fetal growth restriction, neonatal and child deaths Infections from food contaminated by viruses, bacteria, fungi, parasites (diarrhea, cholera, hepatitis A, worms, other infections) Chronic diseases (hypertension, obesity, cancers, diabetes) Renal and kidney damages Mental, behavioral and neurological disorders (stress, anxiety, depression, suicide) Unintentional injuries (poisoning) |
| Air Quality | Low humidity Increased temperature (heat, warmer conditions) Dust storms, dust particles Air contamination by particles from fires (wildfires, agricultural practices) and toxins accumulated in air, soil and water Accidents caused by reduced visibility Release of airborne allergens (fungal spores and plant pollen) | Acute respiratory diseases (flu, sinusitis, rhinitis, bronchitis, pneumonia) Chronic respiratory diseases (asthma, allergic rhinitis, chronic obstructive pulmonary disease) Cardiovascular diseases (stroke, ischemic heart disease, hypertensive heart disease) Cancer (lung, bronchus, trachea, liver, kidney) Neurodegenerative disorders Skin irritations (dermatitis) and eye infection (conjunctivitis) Meningococcal meningitis Diseases caused by fungi, viruses, algae, bacteria, allergens Valley fever Premature births and low birth weight Unintentional injuries by road accidents |
| Soil Quality | Loss of productive soil leads to lower food production, from decreasing agricultural yields and livestock, causing food shortages Soil contamination from chemical products Soil contamination from animal and human excreta Air contamination through contaminated dust | Infections from food contaminated by viruses, bacteria, fungi, parasites (diarrhea, cholera, hepatitis A, worms, other infections) Non-communicable diseases (types of cancers, neurological damage, lung and kidney diseases, skeletal and bone diseases, sterility and reproductive disorders, immune suppression) Respiratory infections (e.g., pneumonia) Skin and eye irritation and allergies or infections Nutritional deficiencies Unintentional injuries (poisonings) |
| Mediating Factors | Environmental and Social Pathways | Human Health Impacts (Morbidity and Mortality) |
|---|---|---|
| Social and Economic Factors | Loss and damage of livestock and subsistence plantations due to difficulty in accessing water Loss or lack of employment, or low income Social impacts from the need to collect water (gender differences, opportunity loss) Lack of access to drinking-water leading to inadequate water storage, and use of contaminated water Lack of hygiene conditions and practices Lack of access to food and the ability of sustenance Rising water prices due to scarcity and high purchase demand Migration of populations due to conflict or seeking improvement in their quality of life (resulting in other social and cultural changes and changes in the epidemiological profile of migrants and of the receiving areas) Family separation (displacement of a family member to other areas in search of employment to supply family needs) causing disruption and changes in the family structure and dynamics Loss of social identity; uncertainty and concerns for the future; lower levels of hopefulness and of social support | Psychological disorders (anxiety, stress, behavioral change generating other problems such as violence, alcoholism, depression) Suicide Increasing chronic non-communicable diseases (cardiovascular diseases, back and arms pain) Increasing infectious and parasitic diseases (gastrointestinal diseases, worms, water and vector-borne diseases) Increasing demand for health services and other social problems in the places where people migrate to |
| Health System Factors | Risks of interruption of health care procedures due to lack of water Increased demands for care and supply of health services Risk of impacts in energy supply, impairing the use of health equipment, refrigeration of medicines and vaccines and other medical supplies, and the health care of some facilities services | Increasing communicable and non-communicable diseases Lack of, or reduction of, health care due to lack of working conditions that may worsen the health conditions of the population |
| Adaptation/Coordination |
|
| Strengthening Capacity-Building and Resilience |
|
| Emergency Preparedness and Response to Disasters |
|
| Monitoring and Surveillance |
|
| Assessment |
|
| Education and Communication |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sena, A.; Ebi, K. When Land Is Under Pressure Health Is Under Stress. Int. J. Environ. Res. Public Health 2021, 18, 136. https://doi.org/10.3390/ijerph18010136
Sena A, Ebi K. When Land Is Under Pressure Health Is Under Stress. International Journal of Environmental Research and Public Health. 2021; 18(1):136. https://doi.org/10.3390/ijerph18010136
Chicago/Turabian StyleSena, Aderita, and Kristie Ebi. 2021. "When Land Is Under Pressure Health Is Under Stress" International Journal of Environmental Research and Public Health 18, no. 1: 136. https://doi.org/10.3390/ijerph18010136
APA StyleSena, A., & Ebi, K. (2021). When Land Is Under Pressure Health Is Under Stress. International Journal of Environmental Research and Public Health, 18(1), 136. https://doi.org/10.3390/ijerph18010136






