Chewing Discomfort According to Dental Prosthesis Type in 12,802 Adults: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Survey Overview
2.2. Participants
2.3. Sociodemographic Status
2.4. General Health Status
2.5. Oral Health Status
2.6. Evaluation of Chewing Discomfort
2.7. Statistical Analysis
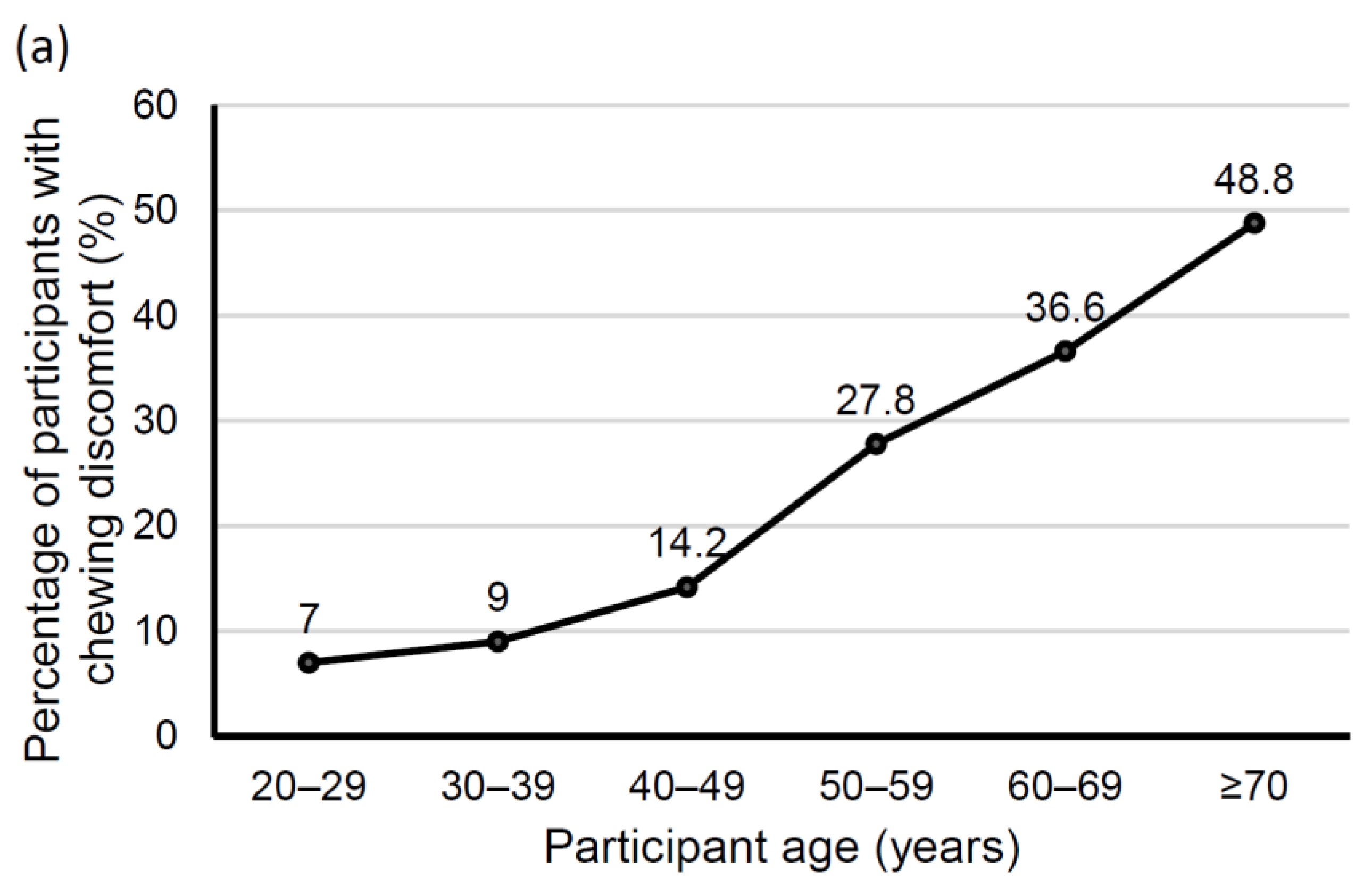
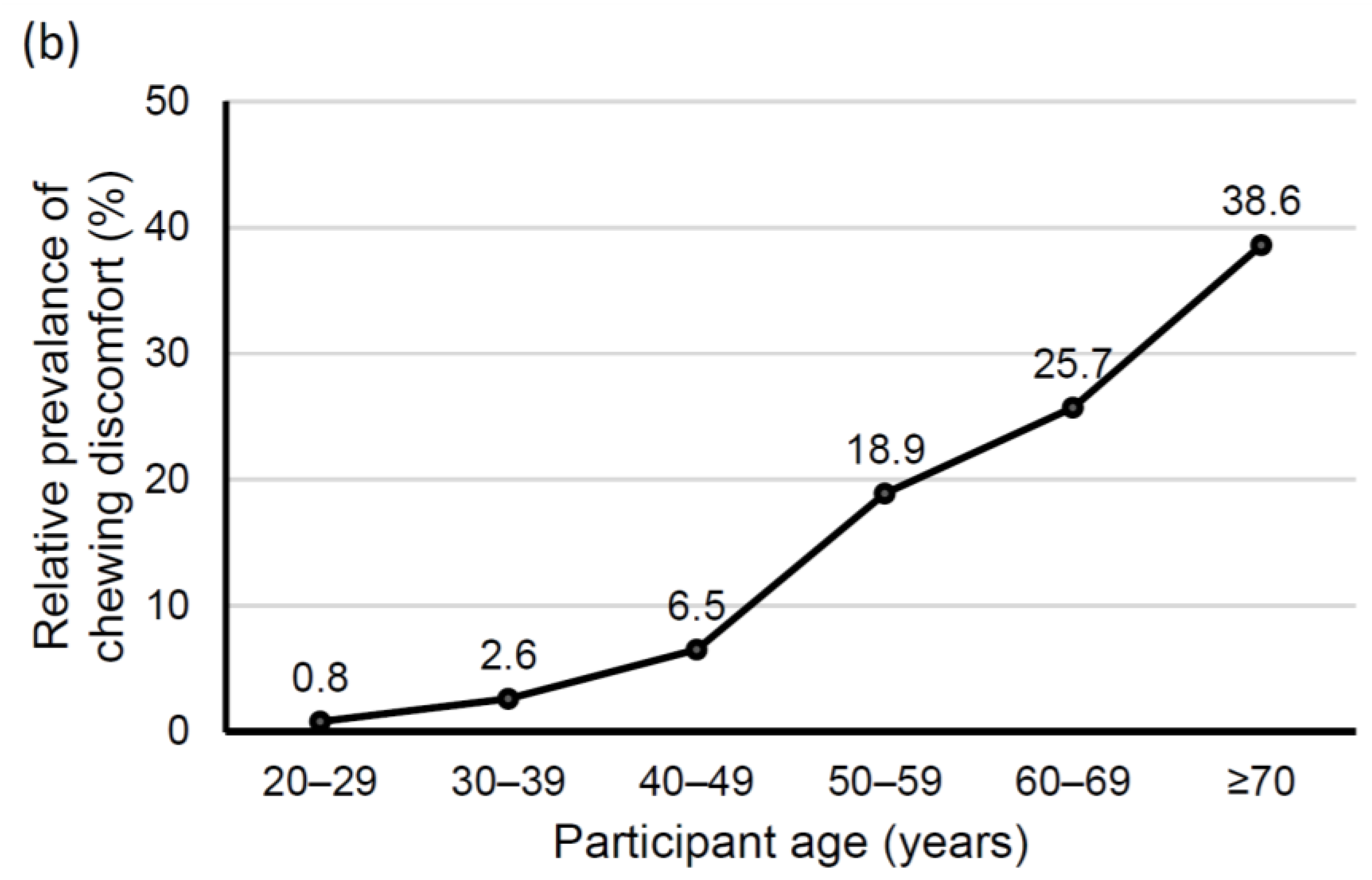
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- van der Bilt, A. Assessment of Mastication with Implications for Oral Rehabilitation: A Review. J. Oral Rehabil. 2011, 38, 754–780. [Google Scholar] [CrossRef] [PubMed]
- Feine, J.S.; Lund, J.P. Measuring Chewing Ability in Randomized Controlled Trials with Edentulous Populations Wearing Implant Prostheses. J. Oral Rehabil. 2006, 33, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Helkimo, E.; Carlsson, G.E.; Helkimo, M. Chewing Efficiency and State of Dentition. A Methodologic Study. Acta Odontol. Scand. 1978, 36, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.A.; Brennan, D.S. Chewing Disability in Older Adults Attributable to Tooth Loss and Other Oral Conditions. Gerodontology 2012, 29, 106–110. [Google Scholar] [CrossRef]
- Zhang, Q.; Witter, D.J.; Bronkhorst, E.M.; Creugers, N.H. Chewing Ability in an Urban and Rural Population Over 40 Years in Shandong Province, China. Clin. Oral Investig. 2013, 17, 1425–1435. [Google Scholar] [CrossRef][Green Version]
- Naka, O.; Anastassiadou, V.; Pissiotis, A. Association between Functional Tooth Units and Chewing Ability in Older Adults: A Systematic Review. Gerodontology 2014, 31, 166–177. [Google Scholar] [CrossRef]
- Moriya, S.; Tei, K.; Murata, A.; Yamazaki, Y.; Hata, H.; Muramatsu, M.; Kitagawa, Y.; Inoue, N.; Miura, H. Associations between Self-Assessed Masticatory Ability and Higher Brain Function Among the Elderly. J. Oral Rehabil. 2011, 38, 746–753. [Google Scholar] [CrossRef]
- Lexomboon, D.; Trulsson, M.; Wårdh, I.; Parker, M.G. Chewing Ability and Tooth Loss: Association with Cognitive Impairment in an Elderly Population Study. J. Am. Geriatr. Soc. 2012, 60, 1951–1956. [Google Scholar] [CrossRef]
- Yamamoto, T.; Kondo, K.; Misawa, J.; Hirai, H.; Nakade, M.; Aida, J.; Kondo, N.; Kawachi, I.; Hirata, Y. Dental Status and Incident Falls Among Older Japanese: A Prospective Cohort Study. BMJ Open 2012, 2, e001262. [Google Scholar] [CrossRef]
- Klineberg, I.; Palla, S.; Trulsson, M. Contemporary Relevance of Occlusion and Mastication. Int. J. Prosthodont. 2014, 27, 411–412. [Google Scholar] [CrossRef]
- Brennan, D.S.; Spencer, A.J.; Roberts-Thomson, K.F. Tooth Loss, Chewing Ability and Quality of Life. Qual. Life Res. 2008, 17, 227–235. [Google Scholar] [CrossRef]
- Inukai, M.; John, M.T.; Igarashi, Y.; Baba, K. Association between Perceived Chewing Ability and Oral Health-Related Quality of Life in Partially Dentate Patients. Health Qual. Life Outcomes 2010, 8, 118. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.C.; Witter, D.J.; Bronkhorst, E.M.; Gerritsen, A.E.; Creugers, N.H. Chewing Ability and Dental Functional Status. Int. J. Prosthodont. 2011, 24, 428–436. [Google Scholar] [PubMed]
- Candel-Marti, E.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M.; Peñarrocha-Diago, M. Satisfaction and Quality of Life with Palatal Positioned Implants in Severely Atrophic Maxillae versus Conventional Implants Supporting Fixed Full-Arch Prostheses. Med. Oral Patol. Oral Cir. Bucal. 2015, 20, e751–e756. [Google Scholar] [CrossRef] [PubMed]
- Cosola, S.; Marconcini, S.; Giammarinaro, E.; Poli, G.L.; Covani, U.; Barone, A. Oral Health-Related Quality of Life and Clinical Outcomes of Immediately or Delayed Loaded Implants in the Rehabilitation of Edentulous Jaws: A Retrospective Comparative Study. Minerva Stomatol. 2018, 67, 189–195. [Google Scholar] [PubMed]
- Osterberg, T.; Carlsson, G.E.; Sundh, V.; Steen, B. Number of Teeth–A Predictor of Mortality in the Elderly? A Population Study in Three Nordic Localities. Acta Odontol. Scand. 2007, 65, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Osterberg, T.; Carlsson, G.E.; Sundh, V.; Mellström, D. Number of Teeth–A Predictor of Mortality in 70-Year-Old Subjects. Commun. Dent. Oral Epidemiol. 2008, 36, 258–268. [Google Scholar] [CrossRef]
- Schwahn, C.; Polzer, I.; Haring, R.; Döorr, M.; Wallaschofski, H.; Kocher, T. Missing, Unreplaced Teeth and Risk of All Cause and Cardiovascular Mortality. Int. J. Cardiol. 2013, 20, 1430–1437. [Google Scholar] [CrossRef]
- World Health Organization. Regional Office for the Western Pacific. In The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; Health Communications Australia: Sydney, Australia, 2000; pp. 17–18.
- Lee, J.H.; Han, J.S.; Han, K.; Lee, S.Y. Association between Diabetes and the Use of Removable Dental Prostheses among the Korean Population. J. Korean Med. Sci. 2019, 34, e262. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, S.Y.; Han, K.; Han, J.S. Relationship between Oral Health Behaviour and Handgrip Strength: A Cross-Sectional Study with 7589 Korean Adults. Acta Odontol. Scand. 2020, 78, 438–444. [Google Scholar] [CrossRef]
- Swelem, A.A.; Gurevich, K.G.; Fabrikant, E.G.; Hassan, M.H.; Aqou, S. Oral Health-Related Quality of Life in Partially Edentulous Patients Treated with Removable, Fixed, Fixed-Removable, and Implant-Supported Prostheses. Int. J. Prosthodont. 2014, 27, 338–347. [Google Scholar]
- Kimura, Y.; Ogawa, H.; Yoshihara, A.; Yamaga, T.; Takiguchi, T.; Wada, T.; Sakamoto, R.; Ishimoto, Y.; Fukutomi, E.; Chen, W.; et al. Evaluation of Chewing Ability and Its Relationship with Activities of Daily Living, Depression, Cognitive Status and Food Intake in the Community-Dwelling Elderly. Geriatr. Gerontol. Int. 2013, 13, 718–725. [Google Scholar] [CrossRef] [PubMed]
- Locker, D. Changes in Chewing Ability with Ageing: A 7-Year Study of Older Adults. J. Oral Rehabil. 2002, 29, 1021–1029. [Google Scholar] [CrossRef] [PubMed]
- Bagewitz, I.C.; Söderfeldt, B.; Palmqvist, S.; Nilner, K. Social Equality and Dental Conditions—A Study of an Adult Population in Southern Sweden. Swed. Dent. J. 2000, 24, 155–164. [Google Scholar] [PubMed]
- Petersen, P.E.; Kjøller, M.; Christensen, L.B.; Krustrup, U. Changing Dentate Status of Adults, Use of Dental Health Services, and Achievement of National Dental Health Goals in Denmark by the Year 2000. J. Public Health Dent. 2004, 64, 127–135. [Google Scholar] [CrossRef]
- Palmqvist, S.; Söderfeldt, B.; Vigild, M.; Kihl, J. Dental Conditions in Middle-Aged and Older People in Denmark and Sweden: A Comparative Study of the Influence of Socioeconomic and Attitudinal Factors. Acta Odontol. Scand. 2000, 58, 113–118. [Google Scholar] [CrossRef]
- Henriksen, B.M.; Axéll, T.; Laake, K. Geographic Differences in Tooth Loss and Denture-Wearing Among the Elderly in Norway. Commun. Dent. Oral Epidemiol. 2003, 31, 403–411. [Google Scholar] [CrossRef]
- Haraldson, T.; Karlsson, U.; Carlsson, G.E. Bite Force and Oral Function in Complete Denture Wearers. J. Oral Rehabil. 1979, 6, 41–48. [Google Scholar] [CrossRef]
- Roumanas, E.D.; Garrett, N.R.; Hamada, M.O.; Kapur, K.K. Comparisons of Chewing Difficulty of Consumed Foods with Mandibular Conventional Dentures and Implant-Supported Overdentures in Diabetic Denture Wearers. Int. J. Prosthodont. 2003, 16, 609–615. [Google Scholar]
- Savoca, M.R.; Arcury, T.A.; Leng, X.; Chen, H.; Bell, R.A.; Anderson, A.M.; Kohrman, T.; Frazier, R.J.; Gilbert, G.H.; Quandt, S.A. Severe Tooth Loss in Older Adults as a Key Indicator of Compromised Dietary Quality. Public Health Nutr. 2010, 13, 466–474. [Google Scholar] [CrossRef]
- Sheiham, A.; Steele, J.G.; Marcenes, W.; Lowe, C.; Finch, S.; Bates, C.J.; Prentice, A.; Walls, A.W. The Relationship among Dental Status, Nutrient Intake, and Nutritional Status in Older People. J. Dent. Res. 2001, 80, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Oates, T.W.; Huynh-Ba, G.; Vargas, A.; Alexander, P.; Feine, J. A Critical Review of Diabetes, Glycemic Control, and Dental Implant Therapy. Clin. Oral Implant Res. 2013, 24, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, S.H.; Yoon, H.I.; Yeo, I.L.; Han, J.S. Implant-Assisted Removable Prosthetic Rehabilitation after Distraction Osteogenesis in a Patient with Ameloblastoma Recurrence: A Case Report. Medicine 2019, 98, e18290. [Google Scholar] [CrossRef] [PubMed]

| Variable | Chewing Discomfort | p-Value | ||
|---|---|---|---|---|
| No | Yes | |||
| Unweighted (n) | 12802 | 9825 | 2977 | |
| Total (%) | 100 | 76.75 | 23.25 | |
| Age (years) | 42.89 ± 0.23 | 55.41 ± 0.38 | <0.0001 | |
| Gender | Male | 50.05 (0.5) | 49.81 (1.02) | 0.8413 |
| Female | 49.95 (0.5) | 50.19 (1.02) | ||
| Income | Lowest quartile | 10.86 (0.51) | 26.21 (1.06) | <0.0001 |
| Lower middle quartile | 24.01 (0.79) | 27.44 (1.08) | ||
| Upper middle quartile | 31.39 (0.85) | 24.41 (1.02) | ||
| Highest quartile | 33.74 (1.03) | 21.94 (1.14) | ||
| Education | Elementary: ≤6 y | 10.43 (0.41) | 34.61 (1.2) | <0.0001 |
| Middle: 7–9 y | 7.47 (0.31) | 14.79 (0.83) | ||
| High: 10–12 y | 40.68 (0.7) | 31.11 (1.19) | ||
| University: ≥ 13 y | 41.42 (0.79) | 19.49 (1.04) | ||
| Place of residence | Rural | 15.49 (1.47) | 21.37 (1.92) | <0.0001 |
| Body mass index (BMI, kg/m2) | 23.67 ± 0.04 | 24.04 ± 0.08 | <0.0001 | |
| Obesity | BMI ≥ 25 | 31.37 (0.54) | 35.81 (1.08) | <0.0001 |
| Smoking | current smoker | 21.28 (0.55) | 26.5 (1.09) | <0.0001 |
| Drinking | heavy drinker | 16.5 (0.48) | 18.81 (0.9) | 0.0169 |
| Stress | Yes | 24.67 (0.55) | 31.57 (1) | <0.0001 |
| Diabetes | Yes | 7.21 (0.29) | 16.68 (0.82) | <0.0001 |
| Hypertension | Yes | 20.72 (0.49) | 37.11 (1.12) | <0.0001 |
| Dental pain | Yes | 33.55 (0.75) | 57.57 (1.18) | <0.0001 |
| Prosthesis need | Yes | 4.12 (0.23) | 20.97 (0.88) | <0.0001 |
| Dental clinic visit (last year) | Yes | 30.44 (0.63) | 28.95 (1.06) | 0.1945 |
| Remaining teeth (n) | 25.95 ± 0.05 | 21.25 ± 0.18 | <0.0001 | |
| Tooth brushing frequency | ≤1 | 8.89 (0.34) | 16.9 (0.88) | <0.0001 |
| 2 | 35.68 (0.54) | 42.16 (1.12) | ||
| ≥3 | 55.43 (0.59) | 40.94 (1.14) | ||
| Without Prosthesis | Fixed Prosthesis | Partial Denture | Complete Denture | p-Value | ||
|---|---|---|---|---|---|---|
| Unweighted (n) | 12802 | 7441 | 3812 | 914 | 635 | |
| Total (%) | 100 | 58.12 | 29.78 | 7.14 | 4.96 | |
| Age (years) | 39.36 ± 0.21 | 53.27 ± 0.3 | 66.05 ± 0.46 | 69.34 ± 0.55 | <0.0001 | |
| Gender | Male | 50.59 (0.58) | 48.91 (0.84) | 44.68 (1.83) | 54.81 (2.14) | 0.002 |
| Female | 49.41 (0.58) | 51.09 (0.84) | 55.32 (1.83) | 45.19 (2.14) | ||
| Income | Lowest quartile | 9.42 (0.53) | 15.86 (0.76) | 38.91 (1.91) | 48.3 (2.6) | <0.0001 |
| Lower middle quartile | 24.55 (0.87) | 23.87 (0.93) | 28.73 (1.9) | 27.7 (2.27) | ||
| Upper middle quartile | 32.26 (0.91) | 28.42 (1.06) | 19.63 (1.57) | 14.39 (1.8) | ||
| Highest quartile | 33.78 (1.08) | 31.85 (1.23) | 12.73 (1.4) | 9.61 (1.59) | ||
| Education | Elementary: ≤6 y | 7.17 (0.35) | 21.79 (0.88) | 53.35 (2.07) | 63.28 (2.46) | <0.0001 |
| Middle: 7–9 y | 6.3 (0.33) | 13.27 (0.63) | 16.24 (1.47) | 14.74 (1.85) | ||
| High:10–12 y | 42.25 (0.76) | 36.22 (0.98) | 22.06 (1.94) | 16.53 (1.8) | ||
| University: ≥13 y | 44.29 (0.86) | 28.73 (1.02) | 8.34 (1.17) | 5.45 (1.16) | ||
| Place of residence | Rural | 14.04 (1.43) | 19.15 (1.73) | 27.89 (2.7) | 31.13 (3.39) | <0.0001 |
| Body mass index (BMI, kg/m2) | 23.58 ± 0.05 | 24.04 ± 0.06 | 24.35 ± 0.13 | 23.78 ± 0.17 | <0.0001 | |
| Obesity | BMI ≥ 25 | 30.5 (0.6) | 35 (0.93) | 40.04 (1.99) | 33.25 (2.38) | <0.0001 |
| Smoking | Current smoker | 23.36 (0.63) | 20.02 (0.78) | 18.93 (1.72) | 24.58 (2.15) | 0.0006 |
| Drinking | Heavy drinker | 17.29 (0.56) | 17.15 (0.75) | 13.06 (1.36) | 14.58 (1.69) | 0.0447 |
| Stress | Yes | 27.51 (0.65) | 24.29 (0.87) | 17.91 (1.48) | 22.63 (1.98) | <0.0001 |
| Diabetes | Yes | 5.8 (0.28) | 12.42 (0.65) | 22.45 (1.71) | 26.66 (2.2) | <0.0001 |
| Hypertension | Yes | 16.48 (0.54) | 33.36 (0.87) | 53.64 (1.98) | 51.67 (2.58) | <0.0001 |
| Dental pain | Yes | 36.66 (0.83) | 43.47 (0.97) | 42.9 (2.12) | 22.14 (2.17) | <0.0001 |
| Dental clinic visit (last year) | Yes | 28.85 (0.7) | 37.49 (1.01) | 21.3 (1.75) | 10.94 (1.43) | <0.0001 |
| Remaining teeth (n) | 27.29 ± 0.02 | 23.96 ± 0.07 | 15.32 ± 0.22 | 3.7 ± 0.19 | <0.0001 | |
| Tooth brushing frequency | ≤1 | 8.84 (0.4) | 9.66 (0.61) | 19.99 (1.7) | 34.3 (2.32) | <0.0001 |
| 2 | 36.03 (0.64) | 38.09 (0.93) | 41.27 (1.81) | 39.68 (2.38) | ||
| ≥3 | 55.13 (0.67) | 52.25 (1) | 38.74 (2.04) | 26.02 (2.01) | ||
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Without prosthesis | 1 (ref.) | 1 (ref.) | 1 (ref.) | 1 (ref.) |
| Fixed prosthesis | 1.392 (1.244,1.557) | 1.379 (1.232,1.543) | 1.373 (1.223,1.541) | 1.363 (1.213,1.532) |
| Partial denture | 2.655 (2.208,3.193) | 2.547 (2.114,3.069) | 2.263 (1.873,2.734) | 2.275 (1.879,2.753) |
| Complete denture | 3.142 (2.452,4.026) | 2.95 (2.298,3.788) | 2.502 (1.946,3.217) | 2.483 (1.929,3.197) |
| p for trend | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-H.; Kim, D.H.; Park, Y.-G.; Lee, S.Y. Chewing Discomfort According to Dental Prosthesis Type in 12,802 Adults: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 71. https://doi.org/10.3390/ijerph18010071
Lee J-H, Kim DH, Park Y-G, Lee SY. Chewing Discomfort According to Dental Prosthesis Type in 12,802 Adults: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(1):71. https://doi.org/10.3390/ijerph18010071
Chicago/Turabian StyleLee, Jae-Hyun, Da Hye Kim, Yong-Gyu Park, and Su Young Lee. 2021. "Chewing Discomfort According to Dental Prosthesis Type in 12,802 Adults: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 1: 71. https://doi.org/10.3390/ijerph18010071
APA StyleLee, J.-H., Kim, D. H., Park, Y.-G., & Lee, S. Y. (2021). Chewing Discomfort According to Dental Prosthesis Type in 12,802 Adults: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(1), 71. https://doi.org/10.3390/ijerph18010071






