Prevalence of Parental Alcohol Problems among a General Population Sample of 28,047 Norwegian Adults: Evidence for a Socioeconomic Gradient
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Measures
2.3. Statistical Analysis
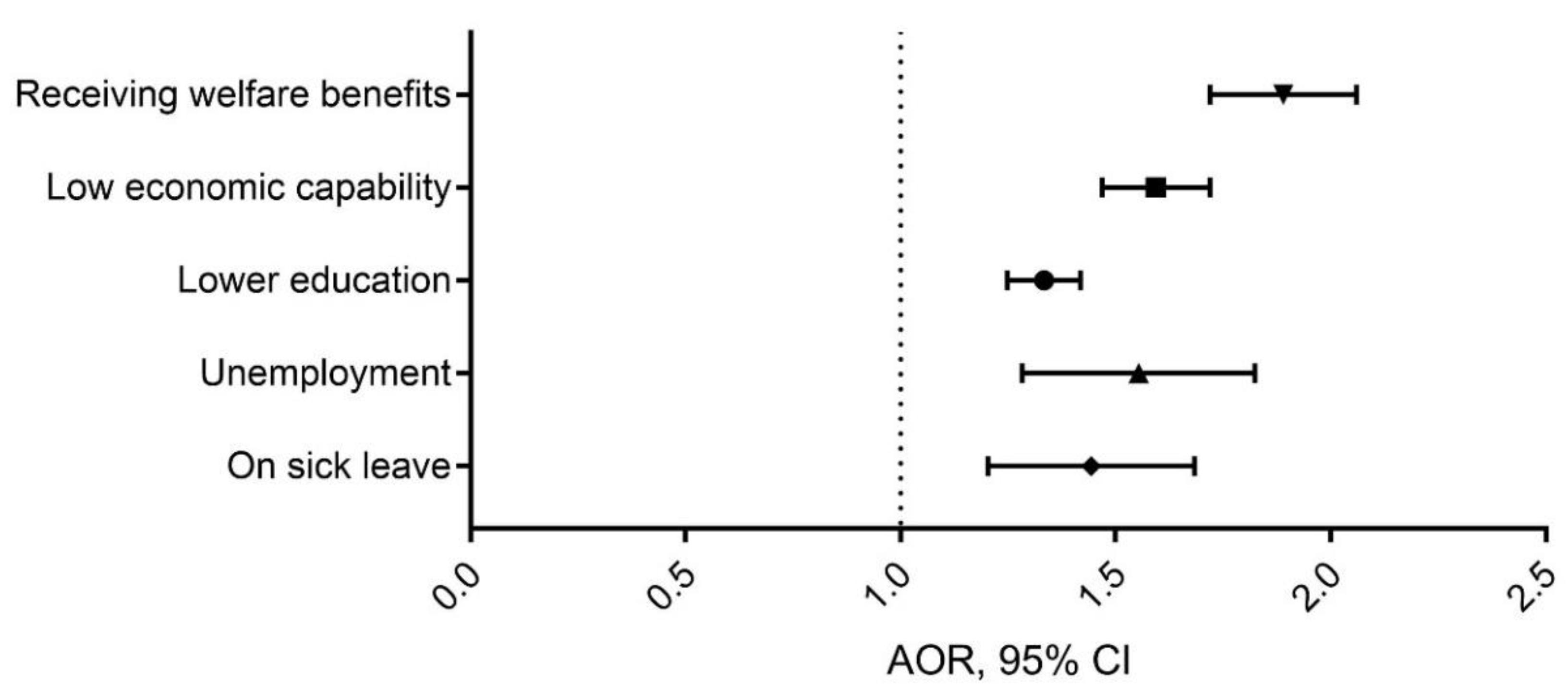
3. Results
4. Discussion
4.1. Study Strengths and Limitations
4.2. Implication for Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anda, R.F.; Whitfield, C.L.; Felitti, V.J.; Chapman, D.; Edwards, V.J.; Dube, S.R.; Williamson, D.F. Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatr. Serv. 2002, 53, 1001–1009. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.L.; Leff, M. Children of substance abusers: Overview of research findings. Pediatrics 1999, 103, 1085–1099. [Google Scholar] [PubMed]
- Lieberman, D.Z. Children of alcoholics: An update. Curr. Opin. Pediatr. 2000, 12, 336–340. [Google Scholar] [CrossRef] [PubMed]
- McGrath, C.E.; Watson, A.L.; Chassin, L. Academic achievement in adolescent children of alcoholics. J. Stud. Alcohol 1999, 60, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Berg, L.; Back, K.; Vinnerljung, B.; Hjern, A. Parental alcohol-related disorders and school performance in 16-year-olds-a Swedish national cohort study. Addiction 2016, 111, 1795–1803. [Google Scholar] [CrossRef]
- Rothman, E.F.; Edwards, E.M.; Heeren, T.; Hingson, R.W. Adverse childhood experiences predict earlier age of drinking onset: Results from a representative US sample of current or former drinkers. Pediatrics 2008, 122, e298–e304. [Google Scholar] [CrossRef]
- Kelley, M.L.; French, A.; Bountress, K.; Keefe, H.A.; Schroeder, V.; Steer, K.; Fals-Stewart, W.; Gumienny, L. Parentification and family responsibility in the family of origin of adult children of alcoholics. Addict. Behav. 2007, 32, 675–685. [Google Scholar] [CrossRef]
- Harter, S.L. Psychosocial adjustment of adult children of alcoholics: A review of the recent empirical literature. Clin. Psychol. Rev. 2000, 20, 311–337. [Google Scholar] [CrossRef]
- Cuijpers, P.; Steunenberg, B.; van Straten, A. When children of problem drinkers grow old: Does the increased risk of mental disorders persist? Addict. Behav. 2006, 31, 2284–2291. [Google Scholar] [CrossRef] [PubMed]
- Landberg, J.; Danielsson, A.-K.; Falkstedt, D.; Hemmingsson, T. Fathers’ alcohol consumption and long-term risk for mortality in offspring. Drugs 2018, 53, 753–759. [Google Scholar] [CrossRef]
- Hemmingsson, T.; Danielsson, A.-K.; Falkstedt, D. Fathers’ alcohol consumption and risk of alcohol-related hospitalization in offspring before 60 years of age. Drugs 2017, 24, 3–8. [Google Scholar] [CrossRef]
- Raninen, J.; Elgan, T.H.; Sundin, E.; Ramstedt, M. Prevalence of children whose parents have a substance use disorder: Findings from a Swedish general population survey. Scand. J. Public Health 2016, 44, 14–17. [Google Scholar] [CrossRef] [PubMed]
- Elgan, T.H.; Leifman, H. Prevalence of adolescents who perceive their parents to have alcohol problems: A Swedish national survey using a web panel. Scand. J. Public Health 2013, 41, 680–683. [Google Scholar] [CrossRef]
- Grant, B.F. Estimates of US children exposed to alcohol abuse and dependence in the family. Am. J. Public Health 2000, 90, 112–115. [Google Scholar] [CrossRef]
- Laslett, A.-M.; Ferris, J.; Dietze, P.; Room, R. Social demography of alcohol-related harm to children in Australia. Addiction 2012, 107, 1082–1089. [Google Scholar] [CrossRef] [PubMed]
- Manning, V.; Best, D.W.; Faulkner, N.; Titherington, E. New estimates of the number of children living with substance misusing parents: Results from UK national household surveys. BMC Public Health 2009, 9, 377. [Google Scholar] [CrossRef]
- Christoffersen, M.N.; Soothill, K. The long-term consequences of parental alcohol abuse: A cohort study of children in Denmark. J. Subst. Abus. Treat. 2003, 25, 107–116. [Google Scholar] [CrossRef]
- Hodgins, D.C.; Maticka-Tyndale, E.; el-Guebaly, N.; West, M. The CAST-6: Development of a short-form of the Children of Alcoholics Screening Test. Addict. Behav 1993, 18, 337–345. [Google Scholar] [CrossRef]
- Pisinger, V.S.C.; Tolstrup, J.S. Are emotional symptoms and depression among young people with parental alcohol problems modified by socioeconomic position? Eur. Child. Adolesc. Psychiatry 2021. [Google Scholar] [CrossRef]
- Haugland, S.H.; Holmen, T.L.; Ravndal, E.; Bratberg, G.H. Parental alcohol misuse and hazardous drinking among offspring in a general teenage population: Gender-specific findings from the Young-HUNT 3 study. BMC Public Health 2013, 13, 1140. [Google Scholar] [CrossRef] [PubMed]
- Bowden, J.A.; Delfabbro, P.; Room, R.; Miller, C.; Wilson, C. Parental drinking in Australia: Does the age of children in the home matter? Drug Alcohol Rev. 2019, 38, 306–315. [Google Scholar] [CrossRef] [PubMed]
- Metzler, M.; Merrick, M.T.; Klevens, J.; Ports, K.A.; Ford, D.C. Adverse childhood experiences and life opportunities: Shifting the narrative. Child. Youth Serv. Rev. 2017, 72, 141–149. [Google Scholar] [CrossRef]
- Hodgins, D.C.; Shimp, L. Identifying adult children of alcoholics: Methodological review and a comparison of the CAST-6 with other methods. Addiction 1995, 90, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Elgán, T.H.; Berman, A.H.; Jayaram-Lindström, N.; Hammarberg, A.; Jalling, C.; Källmén, H. Psychometric properties of the short version of the children of alcoholics screening test (CAST-6) among Swedish adolescents. Nord. J. psychiatry 2020, 75, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Havey, J.M.; Dodd, D.K. Classifying COAs with three variations of the CAST: Classification rates, stability, and gender differences. Addict. Behav. 1995, 20, 501–507. [Google Scholar] [CrossRef]
- Hodgins, D.C.; Maticka-Tyndale, E.; el-Guebaly, N.; West, M. Alternative cut-point scores for the CAST-6. Addict. Behav. 1995, 20, 267–270. [Google Scholar] [CrossRef]
- Jones, J.W. The Children of Alcoholics Screening Test. and Test. Manual; Camelot Unlimited: Chicago, IL, USA, 1983. [Google Scholar]
- Hardt, J.; Rutter, M. Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. J. Child. Psychol. Psychiatry 2004, 45, 260–273. [Google Scholar] [CrossRef] [PubMed]
- Balsa, A.; Homer, J.; French, M. The health effects of parental problem drinking on adult children. J. Ment. Health Policy Econ. 2009, 12, 55–66. [Google Scholar] [PubMed]
- Præstiin, L.V.M. ALKOHOLSTATISTIKK I 150 ÅR. Store Svingninger-Klar Trend. (Alcohol Statistics over 150 Years): Statistics Norway. 2008. Available online: https://www.ssb.no/inntekt-og-forbruk/artikler-og-publikasjoner/store-svingninger-klar-trend (accessed on 9 April 2021).
- Strand, B.H.; Steiro, A. [Alcohol consumption, income and education in Norway, 1993-2000] (In Norwegian). Tidsskr. Nor. Laegeforen. 2003, 123, 2849–2853. [Google Scholar]
- Probst, C.; Kilian, C.; Sanchez, S.; Lange, S.; Rehm, J. The role of alcohol use and drinking patterns in socioeconomic inequalities in mortality: A systematic review. Lancet Public Health 2020, 5, e324–e332. [Google Scholar] [CrossRef]
- Walsh, D.; McCartney, G.; Smith, M.; Armour, G. Relationship between childhood socioeconomic position and adverse childhood experiences (ACEs): A systematic review. J. Epidemiol. Community Health 2019, 73, 1087–1093. [Google Scholar] [CrossRef]
- Houtepen, L.C.; Heron, J.; Suderman, M.J.; Fraser, A.; Chittleborough, C.R.; Howe, L.D. Associations of adverse childhood experiences with educational attainment and adolescent health and the role of family and socioeconomic factors: A prospective cohort study in the UK. PLoS Med. 2020, 17, e1003031. [Google Scholar] [CrossRef]
- Shonkoff, J.P.; Garner, A.S.; Siegel, B.S.; Dobbins, M.I.; Earls, M.F.; McGuinn, L.; Pascoe, J.; Wood, D.L. Committee on Psychosocial Aspects of Child and Family Health, and Committee on Early Childhood, Adoption, and Dependent Care. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012, 129, e232–e246. [Google Scholar] [CrossRef] [PubMed]
- Kalmakis, K.A.; Chandler, G.E. Health consequences of adverse childhood experiences: A systematic review. J. Am. Assoc. Nurse Pract. 2015, 27, 457–465. [Google Scholar] [CrossRef]
- Hardt, J.; Vellaisamy, P.; Schoon, I. Sequelae of prospective versus retrospective reports of adverse childhood experiences. Psychol. Rep. 2010, 107, 425–440. [Google Scholar] [CrossRef] [PubMed]
- Rossow, I.; Felix, L.; Keating, P.; McCambridge, J. Parental drinking and adverse outcomes in children: A scoping review of cohort studies. Drug Alcohol Rev. 2015, 35, 397–405. [Google Scholar] [CrossRef] [PubMed]
- McGovern, R.; Gilvarry, E.; Addison, M.; Alderson, H.; Geijer-Simpson, E.; Lingam, R.; Smart, D.; Kaner, E. The association between adverse child health, psychological, educational and social outcomes, and nondependent parental substance: A rapid evidence assessment. Trauma Violence Abus. 2018, 21, 470–483. [Google Scholar] [CrossRef] [PubMed]
- Haugland, S.H.; Coombes, L.; Strandheim, A. Parental alcohol intoxication and adverse health outcomes among offspring. A 4-year follow up HUNT study among 2399 Norwegian adolescents. Prev. Med. Rep. 2020, 20, 101170. [Google Scholar] [CrossRef]
- Haugland, S.H.; Coombes, L.; Strandheim, A. Are sexually offensive or violent experiences more common among adolescents exposed to parental alcohol intoxication? Child. Abuse Review 2019, 28, 366–380. [Google Scholar] [CrossRef]
- Wannberg, H. Det funkar! Om Kommunernas stöd Till Barn Som Växer Upp Med Missbrukande Föräldrar; JUNIS: Stockholm, Sweden, 2020. (In Swedish) [Google Scholar]
- Elgán, T.H.; Källmén, H. Do professionals ask about children when establishing a collaborative individual plan for clients? A cross-sectional study. Nord. J. Psychiatry 2020, 74, 69–72. [Google Scholar] [CrossRef]
- Solbakken, B.H.; Lauritzen, G. Tilbud Til Barn av Foreldre Med Rusmiddelproblemer; Statens institutt for rusmiddelforskning: Oslo, Norway, 2006; Volume 1/2006. (In Norwegian) [Google Scholar]
- Elgán, T.H.; Leifman, H. Children of substance abusing parents: A national survey on policy and practice in Swedish schools. Health Policy 2011, 101, 29–36. [Google Scholar] [CrossRef]
- Maybery, D.; Reupert, A.; Bartholomew, C.; Cuff, R.; Duncan, Z.; Foster, K.; Matar, J.; Pettenuzzo, L. A web-based intervention for young adults whose parents have a mental illness or substance use concern: Protocol for a randomized controlled trial. JMIR Res. Protoc. 2020, 9, e15626. [Google Scholar] [CrossRef] [PubMed]
- Elgán, T.H.; Kartengren, N.; Strandberg, A.K.; Ingemarson, M.; Hansson, H.; Zetterlind, U.; Gripenberg, J. A web-based group course intervention for 15–25-year-olds whose parents have substance use problems or mental illness: Study protocol for a randomized controlled trial. BMC Public Health 2016, 16, 1011. [Google Scholar] [CrossRef] [PubMed]
- Elgán, T.H.; Hansson, H.; Zetterlind, U.; Kartengren, N.; Leifman, H. Design of a web-based individual coping and alcohol-intervention program (web-ICAIP) for children of parents with alcohol problems: Study protocol for a randomized controlled trial. BMC Public Health 2012, 12, 35. [Google Scholar] [CrossRef] [PubMed]
- Woolderink, M.; Smit, F.; van der Zanden, R.; Beecham, J.; Knapp, M.; Paulus, A.; Evers, S. Design of an internet-based health economic evaluation of a preventive group-intervention for children of parents with mental illness or substance use disorders. BMC Public Health 2010, 10, 470. [Google Scholar] [CrossRef]
- Hafting, M.; Gullbrå, F.; Anderssen, N.; Rørtveit, G.; Smith-Sivertsen, T.; van Doesum, K. Overcoming clinician and parent ambivalence: General practitioners’ support of children of parents with physical or mental illness and/or substance abuse. Front. Psychiatry 2019, 9, 724. [Google Scholar] [CrossRef] [PubMed]
| Variable | Questions | Response Options | Category Definitions |
|---|---|---|---|
| Problematic parental alcohol use | CAST-6 items | Yes/no | A sum score ≥3 on the CAST-6 was defined as parental alcohol problems vs. score <3; not a problem |
| |||
| |||
| |||
| |||
| |||
| |||
| Sex | Sex | Retrieved from registries | Male/female |
| Age | Age | Retrieved from registries | Age groups: 18–24, 25–44, 45–66, 67+ yearsIn multivariable analyses, age was employed as a continuous variable |
| Marital status | What is your marital status? |
| Partner vs. single |
| Education | What is your highest completed level of education? |
| 1 = low education 2 = intermediate education 3 and 4 = higher education |
| Financial capabilities | For one-person households, consider your total income. If you live with others, consider the total income of everyone in the household. How easy or difficult is it for you to make ends meet day to day with this income? |
| 1–3 = low economic capability vs. 4–7 = middle/high economic capability |
| Employment status | What is your current status concerning employment etc.?(Select as many as applicable.) |
| 1 = ≥ 32 h/week vs. not2 = < 32 h/week vs. not3 = Self-employed vs. not4 = On sick-leave vs. not6 and 7 = Receiving welfare benefits vs. not |
| Characteristics | n | % |
|---|---|---|
| Sex | ||
| Female | 14,925 | 53.2 |
| Male | 13,122 | 46.8 |
| Age group, y | ||
| 18–24 | 3169 | 11.3 |
| 25–44 | 9180 | 32.7 |
| 45–66 | 12,026 | 42.9 |
| 67+ | 3672 | 13.1 |
| Education level | ||
| Low | 3333 | 11.9 |
| Intermediate | 11,088 | 39.7 |
| High | 13,502 | 48.4 |
| Employment status * | ||
| Difficult financial situation | 5547 | 20.8 |
| Easy financial situation | 21,140 | 79.2 |
| Employed full-time | 14,278 | 50.9 |
| Employed part-time | 3840 | 13.7 |
| Self-employed | 1470 | 5.2 |
| Unemployed | 815 | 2.9 |
| On sick leave | 849 | 2.9 |
| On welfare benefits | 3208 | 11.4 |
| Characteristics | Parental Alcohol Problems (CAST-6 Sum Score ≥ 3) | |||
|---|---|---|---|---|
| N (%) | χ2 (a) | df | p | |
| Female | 2597 (17.5) | 88.13 | 1 | <0.001 |
| Male | 1759 (13.4) | |||
| Age 18–24 y | 406 (12.9) | 123.19 | 3 | <0.001 |
| Age 25–44 y | 1587 (17.4) | |||
| Age 45–66 y | 1983 (16.6) | |||
| Age 67+ y | 370 (10.2) | |||
| Married/registered partner | 2107 (14.1) | 66.84 | 3 | <0.001 |
| Cohabitee | 871 (18.8) | |||
| Have a girlfriend/boyfriend | 371 (16.7) | |||
| Single | 989 (16.4) | |||
| Low education | 660 (20.0) | 87.49 | 2 | <0.001 |
| Intermediate education | 1814 (16.4) | |||
| High education | 1856 (13.8) | |||
| Low economic capability | 1176 (21.1) | 162.09 | 1 | <0.001 |
| High economic capability | 2999 (14.2) | |||
| Employed full-time | 2107 (15.4) | 1.05 | 1 | 0.305 |
| vs. not employed full-time | 2239 (15.8) | |||
| Employed part-time | 640 (16.7) | 4.60 | 1 | 0.032 |
| vs. not employed part-time | 3706 (15.4) | |||
| Self-employed | 194 (13.2) | 6.62 | 1 | 0.010 |
| vs. not self-employed | 4152 (15.7) | |||
| Unemployed | 176 (21.6) | 23.30 | 1 | <0.001 |
| vs. not unemployed | 4170 (15.4) | |||
| On sick leave | 181 (21.4) | 22.63 | 1 | <0.001 |
| vs. not on sick leave | 4165 (15.4) | |||
| Welfare benefits | 782 (24.5) | 218.19 | 1 | <0.001 |
| vs. no welfare benefits | 3564 (14.4) | |||
| Total | 4346 (15.6) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haugland, S.H.; Elgán, T.H. Prevalence of Parental Alcohol Problems among a General Population Sample of 28,047 Norwegian Adults: Evidence for a Socioeconomic Gradient. Int. J. Environ. Res. Public Health 2021, 18, 5412. https://doi.org/10.3390/ijerph18105412
Haugland SH, Elgán TH. Prevalence of Parental Alcohol Problems among a General Population Sample of 28,047 Norwegian Adults: Evidence for a Socioeconomic Gradient. International Journal of Environmental Research and Public Health. 2021; 18(10):5412. https://doi.org/10.3390/ijerph18105412
Chicago/Turabian StyleHaugland, Siri H., and Tobias H. Elgán. 2021. "Prevalence of Parental Alcohol Problems among a General Population Sample of 28,047 Norwegian Adults: Evidence for a Socioeconomic Gradient" International Journal of Environmental Research and Public Health 18, no. 10: 5412. https://doi.org/10.3390/ijerph18105412
APA StyleHaugland, S. H., & Elgán, T. H. (2021). Prevalence of Parental Alcohol Problems among a General Population Sample of 28,047 Norwegian Adults: Evidence for a Socioeconomic Gradient. International Journal of Environmental Research and Public Health, 18(10), 5412. https://doi.org/10.3390/ijerph18105412






