Bathing Water Quality Monitoring Practices in Europe and the United States
Abstract
:1. Introduction
1.1. Public Health Risks and Etiological Agents
1.2. Faecal Indicator Bacteria
1.3. Monitoring of FIB
1.4. Bathing Water Guidelines and Regulations
1.5. Differences between the Current European and U.S. Practices
- I.
- Enumeration Methods and Indicators
- a.
- Enterococci or Intestinal Enterococci
- b.
- Escherichia coli
- II.
- Epidemiological Studies
- III.
- Acceptable risk
- IV.
- Reporting metrics
- V.
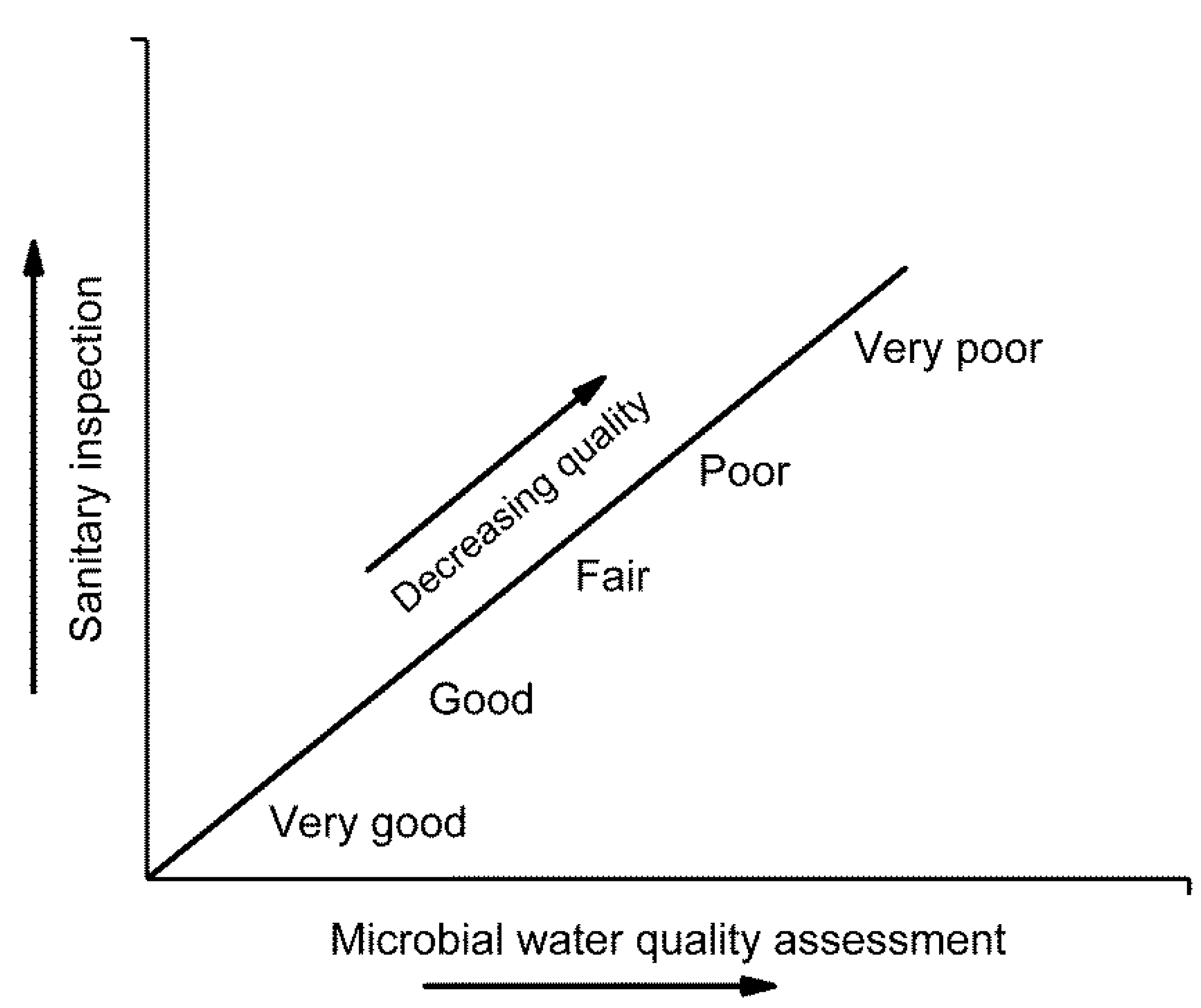
- Profiling and classification
2. Limitations of Current Approach and Future Directions
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tanaka, H. Swimming exercise: Impact of aquatic exercise on cardiovascular health. Sports Med. 2009, 39, 377–387. [Google Scholar] [CrossRef]
- United Nations. Factsheet: People and Oceans. In Proceedings of the Ocean Conference, New York, NY, USA, 5–9 June 2017; Available online: https://www.un.org/sustainabledevelopment/wp-content/uploads/2017/05/Ocean-fact-sheet-package.pdf (accessed on 23 April 2021).
- USEPA. Review of Zoonotic pathogens in Ambient Waters; USEPA Office of Water, Health and Ecological Criteria Division: Washington, DC, USA, 2009.
- Fewtrell, L.; Kay, D. Recreational water and infection: A review of recent findings. Curr. Envir. Health Rep. 2015, 2, 85–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- EC, European Commission. Directive 2006/7/EC of the European Parliament and of the Council of 15 February 2006 concerning the management of bathing water quality and repealing Directive 76/160/EEC. Off. J. Eur. Union. 2006, 64, 37–51. [Google Scholar]
- EPA. Recreational Water Quality Criteria; U S Environmental Protection Agency: Washington, DC, USA, 2012.
- WHO. Volume 1, Coastal and fresh waters. Chapter 4: Faecal Pollution and Water Quality 51–101. In Guidelines for Safe Recreational Water Environments; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Wiedenmann, A.; Krüger, P.; Dietz, K.; López-Pila, J.M.; Szewzyk, R.; Botzenhart, K. A Randomized Controlled Trial Assessing Infectious Disease Risks from Bathing in Fresh Recreational Waters in Relation to the Concentration of Escherichia coli, Intestinal Enterococci, Clostridium perfringens, and Somatic Coliphages. Environ. Health Perspect. 2006, 114, 228–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colford, J.M.; Wade, T.J.; Schiff, K.C.; Wright, C.C.; Griffith, J.F.; Sandhu, S.K.; Burns, S.; Sobsey, M.; Lovelace, G.; Weisberg, S.B. Water Quality Indicators and the Risk of Illness at Beaches With Nonpoint Sources of Fecal Contamination. Epidemiology 2007, 18, 27–35. [Google Scholar] [CrossRef] [Green Version]
- Wade, T.J.; Calderon, R.L.; Brenner, K.P.; Sams, E.; Beach, M.; Haugland, R.; Wymer, L.; Dufour, A.P. High Sensitivity of Children to Swimming-Associated Gastrointestinal Illness. Epidemiology 2008, 19, 375–383. [Google Scholar] [CrossRef]
- Collier, S.A.; Wade, T.J.; Sams, E.A.; Hlavsa, M.C.; Dufour, A.P.; Beach, M.J. Swimming in the USA: Beachgoer characteristics and health outcomes at US marine and freshwater beaches. J. Water Health 2014, 13, 531–543. [Google Scholar] [CrossRef] [Green Version]
- Leonard, A.F.C.; Singer, A.; Ukoumunne, O.C.; Gaze, W.H.; Garside, R. Is it safe to go back into the water? A systematic review and meta-analysis of the risk of acquiring infections from recreational exposure to seawater. Int. J. Epidemiol. 2018, 47, 572–586. [Google Scholar] [CrossRef]
- Wade, T.J.; Calderon, R.L.; Sams, E.; Beach, M.; Brenner, K.P.; Williams, A.H.; Dufour, A.P. Rapidly Measured Indicators of Recreational Water Quality Are Predictive of Swimming-Associated Gastrointestinal Illness. Environ. Health Perspect. 2006, 114, 24–28. [Google Scholar] [CrossRef] [Green Version]
- Wade, T.J.; Sams, E.; Brenner, K.P.; Haugland, R.; Chern, E.; Beach, M.; Wymer, L.; Rankin, C.C.; Love, D.; Li, Q.; et al. Rapidly measured indicators of recreational water quality and swimming-associated illness at marine beaches: A prospective cohort study. Environ. Health 2010, 9, 66. [Google Scholar] [CrossRef] [Green Version]
- WHO. Volume 1, coastal and fresh waters: List of agreed updates. In Addendum to the Who Guidelines for Safe Recreational Water Environments; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Sinclair, R.; Jones, E.; Gerba, C. Viruses in recreational water-borne disease outbreaks: A review. J. Appl. Microbiol. 2009, 107, 1769–1780. [Google Scholar] [CrossRef]
- Hokajärvi, A.-M.; Pitkänen, T.; Siljanen, H.M.P.; Nakari, U.-M.; Torvinen, E.; Siitonen, A.; Miettinen, I.T. Occurrence of thermotolerant Campylobacter spp. and adenoviruses in Finnish bathing waters and purified sewage effluents. J. Water Health 2012, 11, 120–134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korajkic, A.; McMinn, B.R.; Harwood, V.J. Relationships between Microbial Indicators and Pathogens in Recreational Water Settings. Int. J. Environ. Res. Public Health 2018, 15, 2842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pond, K. Water recreation and disease. In Plausibility of Associated Infections: Acute Effects. Chapter 2: Hazard Identification and Factors Related to Infection and Disease; World Health Organization/IWA Publishing UK: London, UK, 2005; pp. 21–34. [Google Scholar]
- Hlavsa, M.C.; Roberts, V.A.; Kahler, A.M.; Hilborn, E.D.; Wade, T.J.; Backer, L.C.; Yoder, J.S. Recreational water-associated disease outbreaks—United States, 2009–2010. Morb. Mortal. Wkly. Rep. 2014, 63, 6–10. [Google Scholar]
- Harwood, V.J.; Staley, C.; Badgley, B.D.; Borges, K.; Korajkic, A. Microbial source tracking markers for detection of fecal contamination in environmental waters: Relationships between pathogens and human health outcomes. FEMS Microbiol. Rev. 2014, 38, 1–40. [Google Scholar] [CrossRef] [Green Version]
- Pitkänen, T. Review of Campylobacter spp. in drinking and environmental waters. J. Microbiol. Methods 2013, 95, 39–47. [Google Scholar] [CrossRef]
- Baker-Austin, C.; Trinanes, J.A.; Salmenlinna, S.; Lofdahl, M.; Siitonen, A.; Taylor, N.G.H.; Martinez-Urtaza, J. Heatwave-associated Vibriosis, Sweden and Finland, 2014. Emerg. Infect Dis. 2016, 22, 1216–1220. [Google Scholar] [CrossRef] [PubMed]
- Lutz, C.; Erken, M.; Noorian, P.; Sun, S.; McDougald, D. Environmental reservoirs and mechanisms of persistence of Vibrio cholerae. Front. Microbiol. 2013, 4, 375. [Google Scholar] [CrossRef] [Green Version]
- Field, K.G.; Samadpour, M. Fecal source tracking, the indicator paradigm, and managing water quality. Water Res. 2007, 41, 3517–3538. [Google Scholar] [CrossRef] [PubMed]
- Xue, J.; Lin, S.; Lamar, F.G.; LaMori, J.G.; Sherchan, S. Assessment of fecal pollution in Lake Pontchartrain, Louisiana. Mar. Pollut. Bull. 2018, 129, 655–663. [Google Scholar] [CrossRef]
- Markand, S.; Bachoon, D.; Gentit, L.; Sherchan, S.; Gates, K. Evaluation of fecal contamination in Harris Neck Estuarine Marshes along the Georgia Coast. Mar. Pollut. Bull. 2011, 62, 178–181. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Recommendations on Scientific, Analytical and Epidemiological Developments Relevant to the Parameters for Bathing Water Quality in the Bathing Water Directive (2006/7/EC); World Health Organization: Geneva, Switzerland, 2018.
- Cabelli, V.J.; Dufour, A.P.; McCabe, L.J.; Levin, M.A. Swimming-Associated Gastroenteritis and Water Quality. Am. J. Epidemiol. 1982, 115, 606–616. [Google Scholar] [CrossRef] [PubMed]
- Wade, T.J.; Pai, N.; Eisenberg, J.N.; Colford, J.M. Do U.S. Environmental Protection Agency water quality guidelines for recreational waters prevent gastrointestinal illness? A systematic review and meta-analysis. Environ. Health Perspect. 2003, 111, 1102–1109. [Google Scholar] [CrossRef]
- Cordero, L.; Norat, J.; Mattei, H.; Nazario, C.M. Seasonal variations in the risk of gastrointestinal illness on a tropical recreational beach. J. Water Health 2012, 10, 579–593. [Google Scholar] [CrossRef] [Green Version]
- Sinton, L.W.; Hall, C.H.; Lynch, P.A.; Davies-Colley, R.J. Sunlight Inactivation of Fecal Indicator Bacteria and Bacteriophages from Waste Stabilization Pond Effluent in Fresh and Saline Waters. Appl. Environ. Microbiol. 2002, 68, 1122–1131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Savichtcheva, O.; Okabe, S. Alternative indicators of fecal pollution: Relations with pathogens and conventional indicators, current methodologies for direct pathogen monitoring and future application perspectives. Water Res. 2006, 40, 2463–2476. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, W.; Gyawali, P.; Sidhu, J.; Toze, S. Relative inactivation of faecal indicator bacteria and sewage markers in freshwater and seawater microcosms. Lett. Appl. Microbiol. 2014, 59, 348–354. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, W.; Zhang, Q.; Kozak, S.; Beale, D.; Gyawali, P.; Sadowsky, M.J.; Simpson, S. Comparative decay of sewage-associated marker genes in beach water and sediment in a subtropical region. Water Res. 2019, 149, 511–521. [Google Scholar] [CrossRef]
- Tiwari, A.; Kauppinen, A.; Pitkänen, T. Decay of Enterococcus faecalis, Vibrio cholerae and MS2 coliphage in a laboratory mesocosm under brackish beach conditions. Front. Public Health 2019, 7, 269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Byappanahalli, M.N.; Nevers, M.B.; Korajkic, A.; Staley, Z.R.; Harwood, V.J. Enterococci in the Environment. Microbiol. Mol. Biol. Rev. 2012, 76, 685–706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Griffith, J.F.; Weisberg, S.B.; Arnold, B.F.; Cao, Y.; Shiff, K.C.; Coldord, J.M. Epidemiologic evaluation of multiple alternate microbial water quality monitoring indicators at three California beaches. Water Res. 2016, 94, 371–381. [Google Scholar] [CrossRef]
- Kauppinen, A.; Al-Hello, H.; Zacheus, O.; Kilponen, J.; Maunula, L.; Huusko, S.; Lappalainen, M.; Miettinen, I.; Blomqvist, S.; Rimhanen-Finne, R. Increase in outbreaks of gastroenteritis linked to bathing water in Finland in summer 2014. Eurosurveillance 2017, 22, 1–8. [Google Scholar] [CrossRef]
- Whitman, R.L.; Harwood, V.J.; Edge, T.A.; Nevers, M.B.; Byappanahalli, M.N.; Vijayavel, K.; Brandão, J.; Sadowsky, M.J.; Alm, E.W.; Crowe, A.; et al. Microbes in beach sands: Integrating environment, ecology and public health. Rev. Environ. Sci. Bio/Technol. 2014, 13, 329–368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oliver, D.M.; Hanley, N.D.; Van Niekerk, M.; Kay, D.; Heathwaite, A.L.; Rabinovici, S.J.M.; Kinzelman, J.L.; Fleming, L.E.; Porter, J.; Shaikh, S.; et al. Molecular tools for bathing water assessment in Europe: Balancing social science research with a rapidly developing environmental science evidence-base. AMBIO 2015, 45, 52–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hodgson, C.J.; Oliver, D.M.; Fish, R.D.; Bulmer, N.M.; Heathwaite, A.L.; Winter, M.; Chadwick, D.R. Seasonal persistence of faecal indicator organisms in soil following dairy slurry application to land by surface broadcasting and shallow injection. J. Environ. Manag. 2016, 183, 325–332. [Google Scholar] [CrossRef]
- Byappanahalli, M.N.; Sawdey, R.; Ishii, S.; Shively, D.A.; Ferguson, J.A.; Whitman, R.L.; Sadowsky, M.J. Seasonal stability of Cladophora-Associated Salmonella in Lake Michigan watersheds. Water Res. 2009, 43, 806–814. [Google Scholar] [CrossRef]
- Weiskerger, C.J.; Brandão, J.; Ahmed, W.; Aslan, A.; Avolio, L.; Badgley, B.D.; Boehm, A.B.; Edge, T.A.; Fleisher, J.M.; Heaney, C.D.; et al. Impacts of a changing earth on microbial dynamics and human health risks in the continuum between beach water and sand. Water Res. 2019, 162, 456–470. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, A.; Niemelä, S.I.; Vepsäläinen, A.; Rapala, J.; Kalso, S.; Pitkänen, T. Comparison of Colilert-18 with miniaturized most probable number method for monitoring of Escherichia coli in bathing water. J. Water Health 2016, 14, 121–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tiwari, A.; Hokajärvi, A.-M.; Domingo, J.W.S.; Kauppinen, A.; Elk, M.; Ryu, H.; Jayaprakash, B.; Pitkänen, T. Categorical performance characteristics of method ISO 7899-2 and indicator value of intestinal enterococci for bathing water quality monitoring. J. Water Health 2018, 16, 711–723. [Google Scholar] [CrossRef]
- Valente, M.S.; Pedro, P.; Alonso, M.C.; Borrego, J.J.; Dionísio, L. Are the defined substrate-based methods adequate to determine the microbiological quality of natural recreational waters? J. Water Health 2009, 8, 11–19. [Google Scholar] [CrossRef]
- Niemela, S.I.; Lee, J.V.; Fricker, C.R. A comparison of the international standards organization reference method for the detection of coliforms and Escherichia coli in water with a defined substrate procedure. J. Appl. Microbiol. 2003, 95, 1285–1292. [Google Scholar] [CrossRef] [PubMed]
- Pitkänen, T.; Paakkari, P.; Miettinen, I.T.; Heinonen-Tanski, H.; Paulin, L.; Hänninen, M.-L. Comparison of media for enumeration of coliform bacteria and Escherichia coli in non-disinfected water. J. Microbiol. Methods 2007, 68, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Pitkänen, T.; Ryu, H.; Elk, M.; Hokajärvi, A.-M.; Siponen, S.; Vepsäläinen, A.; Räsänen, P.; Santo, D.J.W. Detection of fecal bacteria and source tracking identifiers in environmental waters using rRNA-based RT-qPCR and rDNA-based qPCR assays. Environ. Sci. Technol. 2013, 47, 13611–13620. [Google Scholar] [CrossRef]
- ISO 7899-1:1998. Water Quality—Detection and Enumeration of Intestinal Enterococci—Part 1: Miniaturized Method (Most Probable Number) for Surface and Wastewater; International Organization for Standardization: Geneva, Switzerland, 1998. [Google Scholar]
- ISO 7899-2:2000. Water Quality-Detection and Enumeration of Intestinal Enterococci—Part 2: Membrane Filtration Method; International Organization for Standardization: Geneva, Switzerland, 2000. [Google Scholar]
- Stoeckel, D.M.; Harwood, V.J. Performance, design and analysis in microbial source tracking studies. Appl. Environ. Microbiol. 2007, 73, 2405–2415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Q.; Gallard, J.; Wu, B.; Harwood, V.J.; Sadowsky, M.J.; Hamilton, K.A.; Ahmed, W. Synergy between quantitative microbial source tracking (qMST) and quantitative microbial risk assessment (QMRA): A review and prospectus. Environ. Int. 2019, 130, 104703. [Google Scholar] [CrossRef]
- Soller, J.A.; Schoen, M.E.; Bartrand, T.; Ravenscroft, J.E.; Ashbolt, N. Estimated human health risks from exposure to recreational waters impacted by human and non-human sources of faecal contamination. Water Res. 2010, 44, 4674–4691. [Google Scholar] [CrossRef]
- Soller, J.A.; Eftim, S.; Wade, T.J.; Ichida, A.M.; Clancy, J.L.; Johnson, T.B.; Schwab, K.; Ramirez-Toro, G.; Nappier, S.; Ravenscroft, J.E. Use of quantitative microbial risk assessment to improve interpretation of a recreational water epidemiological study. Microb. Risk. Anal. 2016, 1, 2–11. [Google Scholar] [CrossRef]
- Vierheilig, J.; Savio, D.; Ley, R.E.; Mach, R.L.; Farnleitner, A.H.; Reischer, G.H. Potential applications of next generation DNA sequencing of 16S rRNA gene amplicons in microbial water quality monitoring. Water Sci. Technol. 2015, 72, 1962–1972. [Google Scholar] [CrossRef] [Green Version]
- Okabe, S.; Shimazu, Y. Persistence of host-specific Bacteroides–Prevotella 16S rRNA genetic markers in environmental waters: Effects of temperature and salinity. Appl. Microbiol Biotechnol. 2007, 76, 935–944. [Google Scholar] [CrossRef]
- Boehm, A.B.; Van De Werfhorst, L.C.; Griffith, J.F.; Holden, P.A.; Jay, J.A.; Shanks, O.C.; Wang, D.; Weisberg, S.B. Performance of forty-one microbial source tracking methods: A twenty-seven lab evaluation study. Water Res. 2013, 47, 6812–6828. [Google Scholar] [CrossRef]
- Rytkönen, A.; Tiwari, A.; Hokajärvi, A.-M.; Uusheimo, S.; Vepsäläinen, A.; Tulonen, T.; Pitkänen, T. The use of ribosomal RNA as a microbial source tracking target highlights the assay host-specificity requirement in water quality assessments. Front. Microbiol. 2021, 12, 1137. [Google Scholar] [CrossRef]
- Haugland, R.A.; Varma, M.; Sivaganesan, M.; Kelty, C.; Peed, L.; Shanks, O.C. Evaluation of genetic markers from the 16S rRNA gene V2 region for use in quantitative detection of selected Bacteroidales species and human fecal waste by qPCR. Syst. Appl. Microbiol. 2010, 33, 348–357. [Google Scholar] [CrossRef]
- Haugland, R.A.; Siefring, S.C.; Wymer, L.J.; Brenner, K.P.; Dufour, A.P. Comparison of Enterococcus measurements in freshwater at two recreational beaches by quantitative polymerase chain reaction and membrane filter culture analysis. Water Res. 2005, 39, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Oliver, D.M.; Van Niekerk, M.; Kay, D.; Heathwaite, A.L.; Porter, J.; Fleming, L.E.; Kinzelman, J.L.; Connolly, E.; Cummins, A.; McPhail, C.; et al. Opportunities and limitations of molecular methods for quantifying microbial compliance parameters in EU bathing waters. Environ. Int. 2014, 64, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, A.; Kelty, C.A.; Sivaganesan, M.; Shanks, O.C.; Dorevitch, S. Fecal pollution source characterization at non-point source impacted beaches under dry and wet weather conditions. Water Res. 2020, 182, 116014. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Mortensen, M.S.; Schjørring, S.; Trivedi, U.; Vestergaard, G.; Stokholm, J.; Bisgaard, H.; Krogfelt, K.A.; Sørensen, S.J. Amplicon sequencing provides more accurate microbiome information in healthy children compared to culturing. Commun. Biol. 2019, 2, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- U.S. EPA. Report of the Expert Scientific Workshop on Critical Research Needs for the Development of New or Revised Recreational Water Quality Criteria (Airlie Workshop); EPA823-R-07-006; U.S. EPA: Washington, DC, USA, 2007.
- Fleisher, J.M.; Jones, F.; Kay, D.; Stanwell-Smith, R.; Wyer, M.; Morano, R. Water and Non-Water-Related Risk Factors for Gastroenteritis among Bathers Exposed to Sewage-Contaminated Marine Waters. Int. J. Epidemiol. 1993, 22, 698–708. [Google Scholar] [CrossRef] [PubMed]
- Fleisher, J.M.; Kay, D.; Salmon, R.L.; Jones, F.; Wyer, M.D.; Godfree, A.F. Marine waters contaminated with domestic sewage: Non-enteric illnesses associated with bather exposure in the United Kingdom. Am. J. Public Health 1996, 86, 1228–1234. [Google Scholar] [CrossRef] [Green Version]
- Kay, D.; Jones, F.; Wyer, M.D.; Fleisher, J.M.; Salmon, R.L.; Godfree, A.F.; Zelenauch-Jacquotte, A.; Shore, R. Predicting likelihood of gastroenteritis from sea bathing: Results from randomized exposer. Lancet 1994, 344, 905–909. [Google Scholar] [CrossRef]
- European Union. Combined Evaluation Roadmap/Inception Impact Assessment; Reference Ares; 1628779-04/03/2021; European Union: Brussels, Belgium, 2021.
- Dufour, A.P. Health Effects Criteria for Fresh Recreational Waters; EPA 600/1-84-004; Environmental Protection Agency: Cincinnati, OH, USA, 1984.
- Ferguson, D.; Moore, D.; Getrich, M.; Zhowandai, M. Enumeration and speciation of enterococci found in marine and intertidal sediments and coastal water in southern California. J. Appl. Microbiol. 2005, 99, 598–608. [Google Scholar] [CrossRef]
- Ferguson, D.M.; Griffith, J.F.; McGee, C.D.; Weisberg, S.B.; Hagedorn, C. Comparison of Enterococcus Species Diversity in Marine Water and Wastewater Using Enterolert and EPA Method 1600. J. Environ. Public Health 2013, 2013, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, D.; Zhowandai, M.; Ferguson, D.; McGee, C.; Mott, J.; Stewart, J. Comparison of 16S rRNA sequencing with conventional and commercial phenotypic techniques for identification of enterococci from the marine environment. J. Appl. Microbiol. 2006, 100, 1272–1281. [Google Scholar] [CrossRef] [PubMed]
- Layton, B.A.; Walters, S.P.; Lam, L.H.; Boehm, A.B. Enterococcus species distribution among human and animal hosts using multiplex PCR. J. Appl. Microbiol. 2010, 109, 539–547. [Google Scholar] [PubMed]
- ISO 9308-1:2000. Water Quality—Detection and Enumeration of Escherichia coli and Coliform bacteria—Part 1: Membrane Filtration Method; International Organization for standardization: Geneva, Switzerland, 2000. [Google Scholar]
- ISO 9308-3:1998. Water Quality—Detection and Enumeration of Escherichia coli and Coliform bacteria—Part 3: Miniaturized Method (Most Probable Number) for the Detection and Enumeration of E. coli in Surface and Wastewater; International Organization for standardization: Geneva, Switzerland, 1998. [Google Scholar]
- ISO 9308-1:2014. Water Quality—Enumeration of Escherichia coli and Coliform Bacteria—Part 1: Membrane Filtration Method for Waters with Low Bacterial Background Flora; International Organization for Standardization: Geneva, Switzerland, 2014. [Google Scholar]
- Jozić, S.; Lušić, D.V.; Ordulj, M.; Frlan, E.; Cenov, A.; Diković, S.; Kauzlarić, V.; Đurković, L.F.; Totić, J.S.; Ivšinović, D.; et al. Performance characteristics of the temperature-modified ISO 9308-1 method for the enumeration of Escherichia coli in marine and inland bathing waters. Mar. Pollut. Bull. 2018, 135, 150–158. [Google Scholar] [CrossRef]
- Le Baron, P.; Henry, A.; Lepeuple, A.-S.; Pena, G.; Servais, P. An operational method for the real-time monitoring of E. coli numbers in bathing waters. Mar. Pollut. Bull. 2005, 50, 652–659. [Google Scholar] [CrossRef] [PubMed]
- ISO 17994:2014. Water Quality—Requirements for the Comparison of the Relative Recovery of Microorganisms by Two Quantitative Methods; International Organization for standardization: Geneva, Switzerland, 2014. [Google Scholar]
- ISO 9308-2:2012. Water Quality—Enumeration of Escherichia coli and Coliform Bacteria—Part 2: Most Probable Number Method; International Organization for Standardization: Geneva, Switzerland, 2012. [Google Scholar]
- Quilliam, R.S.; Taylor, J.; Oliver, D.M. The disparity between regulatory measurements of E. coli in public bathing waters and the public expectation of bathing water quality. J. Environ. Manag. 2019, 232, 868–874. [Google Scholar] [CrossRef]
- Quilliam, R.S.; Kinzelman, J.; Brunner, J.; Oliver, D.M. Resolving conflicts in public health protection and ecosystem service provision at designated bathing waters. J. Environ. Manag. 2015, 161, 237–242. [Google Scholar] [CrossRef]
- Whitman, R.L.; Shively, D.A.; Pawlik, H.; Nevers, M.B.; Byappanahalli, M.N. Occurrence of Escherichia coli and Enterococci in Cladophora (Chlorophyta) in Nearshore Water and Beach Sand of Lake Michigan. Appl. Environ. Microbiol. 2003, 69, 4714–4719. [Google Scholar] [CrossRef] [Green Version]
- Abdelzaher, A.M.; Wright, M.E.; Ortega, C.; Solo-Gabriele, H.M.; Miller, G.; Elmir, S.; Newman, X.; Shih, P.; Bonilla, J.A.; Bonilla, T.D.; et al. Presence of Pathogens and Indicator Microbes at a Non-Point Source Subtropical Recreational Marine Beach. Appl. Environ. Microbiol. 2009, 76, 724–732. [Google Scholar] [CrossRef] [Green Version]
- Rodrigues, A.; Oliver, D.M.; McCarron, A.; Quilliam, R.S. Colonisation of plastic pellets (nurdles) by E. coli at public bathing beaches. Mar. Pollut. Bull. 2019, 139, 376–380. [Google Scholar] [CrossRef] [Green Version]
- Hlavsa, M.C.; Roberts, V.A.; Kahler, A.M.; Hilborn, E.D.; Mecher, T.R.; Beach, M.J.; Wade, T.J.; Yoder, J.S. Outbreaks of Illness Associated with Recreational Water—United States, 2011–2012. MMWR. Morb. Mortal. Wkly. Rep. 2015, 64, 668–672. [Google Scholar] [PubMed]
- Fujioka, R.S.; Solo-Gabriele, H.M.; Byappanahalli, M.N.; Kirs, M.U.S. Recreational Water Quality Criteria: A Vision for the Future. Int. J. Environ. Res. Public Health 2015, 12, 7752–7776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tiwari, A.; Hokajärvi, A.-M.; Santo, D.J.W.; Elk, M.; Jayaprakash, B.; Ryu, H.; Siponen, S.; Vepsäläinen, A.; Kauppinen, A.; Puurunen, O.; et al. Bacterial diversity and predicted enzymatic function in a multipurpose surface water system—From wastewater effluent discharges to drinking water production. Res. Sq. 2020. [Google Scholar] [CrossRef]
- Stidson, R.T.; Gray, C.A.; McPhail, C.D. Development and use of modelling techniques for real-time bathing water quality predictions. Water Environ. J. 2011, 26, 7–18. [Google Scholar] [CrossRef]
- Oliver, D.M.; Porter, K.D.H.; Pachepsky, Y.; Muirhead, R.W.; Reaney, S.M.; Coffey, R.; Kay, D.; Milledge, D.G.; Hong, E.; Anthony, S.G.; et al. Predicting microbial water quality with models: Over-arching questions for managing risk in agricultural catchments. Sci. Total. Environ. 2016, 544, 39–47. [Google Scholar] [CrossRef] [Green Version]
- Herrig, I.; Seis, W.; Fischer, H.; Regnery, J.; Manz, W.; Reifferscheid, G.; Böer, S. Prediction of fecal indicator organism concentrations in rivers: The shifting role of environmental factors under varying flow conditions. Environ. Sci. Eur. 2019, 31, 1–16. [Google Scholar] [CrossRef]
- Wyer, M.D.; Kay, D.; Morgan, H.; Naylor, S.; Clark, S.; Watkins, J.; Davies, C.M.; Francis, C.; Osborn, H.; Bennett, S. Within-day variability in microbial concentrations at a UK designated bathing water: Implications for regulatory monitoring and the application of predictive modelling based on historical compliance data. Water Res. X 1 2018, 1, 100006. [Google Scholar] [CrossRef]
- Tedetti, M.; Longhitano, R.; Garcia, N.; Guigue, C.; Ferretto, N.; Goutx, M. Fluorescence properties of dissolved organic matter in coastal Mediterranean waters influenced by a municipal sewage effluent (Bay of Marseilles, France). Environ. Chem. 2012, 9, 438–449. [Google Scholar] [CrossRef] [Green Version]
- Madonia, A.; Caruso, G.; Piazzolla, D.; Bonamano, S.; Piermattei, V.; Zappalà, G.; Marcelli, M. Chromophoric Dissolved Organic Matter as a Tracer of Fecal Contamination for Bathing Water Quality Monitoring in the Northern Tyrrhenian Sea (Latium, Italy). J. Mar. Sci. Eng. 2020, 8, 430. [Google Scholar] [CrossRef]
- Bonamano, S.; Madonia, A.; Caruso, G.; Zappalà, G.; Marcelli, M. Development of a New Predictive index (Bathing Water Quality Index, BWQI) Based on Escherichia coli Physiological States for Bathing Waters Monitoring. J. Mar. Sci. Eng. 2021, 9, 120. [Google Scholar] [CrossRef]
- Benjamin-Chung, J.; Arnold, B.F.; Wade, T.J.; Schiff, K.; Griffith, J.F.; Dufour, A.P.; Weisberg, S.B.; Colford, J.M. Coliphages and Gastrointestinal Illness in Recreational Waters. Epidemiology 2017, 28, 644–652. [Google Scholar] [CrossRef] [PubMed]
Short Biography of Authors
 | Doctor Ananda Tiwari, PhD, is a water health microbiologist. Currently, he is working as a postdoctoral researcher in the Expert Microbiology Research Unit of the Finnish Institute for Health and Welfare, Kuopio Finland. He did his doctoral study in monitoring microbial quality of bathing water. His research interest includes indicator bacteria (Escherichia coli and intestinal enterococci), microbial source tracking, virus indicators, beach monitoring, Vibrio cholera, Cyanobacteria, microbial ecology, antibiotic-resistant bacteria/genes, wastewater-based epidemiology, drinking water distribution system, and biofilm production. |
 | Associate Professor David Oliver, PhD, is an Associate Professor of Catchment Science based at the University of Stirling UK, where he has worked for the last 10 years. He completed his BSc and PhD at the University of Sheffield, UK. His broad research interests cover the connections between land, water and people, in particular the impact of the environment on people’s health. Current research focus includes fate and transfer dynamics of diffuse pollutants, managing competing demands on soil and water resources in catchments to benefit public health, healthy and resilient bathing water environments and the co-design of decision support systems to visualise risks to water quality across multiple scales. |
 | Doctor Aaron Bivins, PhD, is a post-doctoral research associate in the Department of Civil and Environmental Engineering and Earth Sciences at the University of Notre, Notre Dame, Indiana, USA. He is a public health engineer interested in the transmission of human pathogens via environmental and engineered systems. His work includes the use of environmental microbiology techniques to detect and quantify rare pathogens, quantitative microbial risk assessment to estimate risks to human health, and BioRender to create compelling scientific illustrations. |
 | Assistant Professor Samendra P. Sherchan, PhD, is currently an assistant professor in the department of environmental health sciences at Tulane University. He received his PhD from the University of Arizona under Drs. Charles Gerba, Ian Pepper and Shane Snyder. He began studying environmental virology in graduate school where he worked on virus treatment for water reuse. He has been working primarily at better understanding the survival, fate and transport of emerging viruses in natural and engineered water systems. His research interests include environmental virology, one health, diarrheal diseases, water reuse, water quality, sanitation, and hygiene in developing counties. He currently serves as an associate editor for the Journal ofWater and Health and BMC Infectious Diseases. He is also on the editorial boards of ACS Water and Science of the Total Environment. |
 | Associate Professor Tarja Pitkänen, PhD , has a broad expertise on detection methods and infection risk assessment of microbes in water. She works as a Chief Specialist at the Water Microbiology Laboratory, Finnish Institute for Health and Welfare, Finland. Since 1.10.2020, she has co-affiliation as Associate Professor in the field of Environmental Health at the University of Helsinki as a part of HOH Helsinki One Health Network. Tarja Pitkänen conducts research and expertise tasks related to waterborne outbreak preparedness for fecal contamination and microbial water safety research with her team members and PhD students. She is adjunct Professor in Molecular water microbiology at the University of Eastern Finland, where she gained a PhD on Environmental microbiology in 2010. In 2012-2013, she was a researcher at the National Risk Management Research Laboratory of the United States Environmental Protection Agency, USA where she focused her research on molecular detection, next-generation sequencing tools and the characterization of active bacterial communities in water. Currently she is involved in several research projects and international expert duties related to the water microbiology. |
| Agent | Illness | Probable Source | Transmission Pathway |
|---|---|---|---|
| Campylobacter spp. | Gastroenteritis, fever | Human and animals | Ingestion |
| Enteropathogenic E. coli | Bloody diarrhea, abdominal cramp | Human and animals | Ingestion |
| Helicobacter pylori | Gastritis, abdominal pain | Human and animals | Ingestion |
| Legionella spp. | Pneumonia, gastroenteritis | Natural | Inhalation |
| Leptospira spp. | Fever, headache, vomiting, jaundice | Natural and animals | Ingestion |
| Salmonella spp. | Gastroenteritis, fever, pain | Human and animals | Ingestion |
| Mycobacterium avium | Respiratory disease | Natural | Inhalation/contact |
| Vibrio vulnificus | Infection in pre-existed open wound | Natural | Wound infection |
| Shigella spp. | Bacillary dysentery, abdominal pain | Human | Ingestion |
| Adenovirus | Gastroenteritis, respiratory disease | Human | Ingestion, inhalation |
| Noroviruses | Gastroenteritis | Human | Ingestion |
| Rotaviruses | Gastroenteritis | Human | Ingestion |
| Coxsackievirus | Mild febrile illness to myocarditis | Human | Ingestion |
| Enteroviruses | Central nervous system, ocular and respiratory infections | Human | Ingestion |
| Echovirus | Diarrhea, secretions from the eyes or throat | Human | Ingestion |
| Hepatitis A virus | Liver disease | Human | Ingestion |
| Hepatitis E virus | Liver disease | Human and animals | Ingestion |
| Cryptosporidium | Diarrhea, abdominal pain, fever | Human and animals | Ingestion |
| Giardia | Diarrhea, abdominal cramp | Human and animals | Ingestion |
| Microsporidia | GI illness, diarrhea | Human and animals | Ingestion |
| Naegeria fowleri | Meningoencephalitis | Natural | Contact |
| Schistosoma spp. | GI illness, haematuria | Human | Ingestion, Contact |
| Entamoeba histolytica | Amoebic dysentery | Human | Ingestion |
| Regulation or Guideline | Indicator | Water Type | FIB Value (CFU or MPN/100 mL) | Reporting Metric | Illness Rate for Swimmers | Symptoms | Sampling Frequency |
|---|---|---|---|---|---|---|---|
| [7] | Ent | Fresh/Marine | 500 | 95 per | 10% GI illness risk | AFRI, GI illness | ~20/per bathing season |
| [5] | INT Ent | Fresh | 200 * (Excellent), 400 * (Good), 330 ** (Sufficient) | * 95 per, ** 90 per | AFRI: Excellent 1%, Good 2.5%, GI: Excellent 3%, Good 5% | AFRI, GI illness | >4/per bathing season |
| [5] | INT Ent | Marine | 100 * (Excellent), 200 * (Good), 185 ** (Sufficient) | * 95 per, ** 90 per | AFRI: Excellent 1%, Good 2.5%, GI: Excellent 3%, Good 5% | AFRI, GI illness | >4/per bathing season |
| [5] | E. coli | Fresh | 500 * (Excellent), 1000 * (Good), 900 ** (Sufficient) | * 95 per, ** 90 per | AFRI: Excellent 1%, Good 2.5%, GI: Excellent 3%, Good 5% | AFRI, GI illness | >4/per bathing season |
| [5] | E. coli | Marine | 250 * (Excellent), 500 * (Good), 500 ** (Sufficient) | * 95 per, ** 90 per | AFRI: Excellent 1%, Good 2.5%, GI: Excellent 3%, Good 5% | AFRI, GI illness | >4/per bathing season |
| [6] | ENT | Fresh | 30/110 STV | GM/STV | 32/1000 | GI illness | ~5/30 days in bathing season |
| [6] | E. coli | Fresh | 100/320 | GM/STV | 32/1000 | GI illness | ~5/30 days in bathing season |
| [6] | ENT | Marine | 35/130 STV | GM/STV | 36/1000 | GI illness | ~5/30 days in bathing season |
| [6] | ENT qPCR (GC) | Fresh/Marine | 470 CCE/2000 CCE | GM/STV | GI illness | ~5/30 days in bathing season | |
| [6] | ENT qPCR (GC) | Fresh/Marine | 1000 CCE | 75 per | GI illness | ~5/30 days in bathing season |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tiwari, A.; Oliver, D.M.; Bivins, A.; Sherchan, S.P.; Pitkänen, T. Bathing Water Quality Monitoring Practices in Europe and the United States. Int. J. Environ. Res. Public Health 2021, 18, 5513. https://doi.org/10.3390/ijerph18115513
Tiwari A, Oliver DM, Bivins A, Sherchan SP, Pitkänen T. Bathing Water Quality Monitoring Practices in Europe and the United States. International Journal of Environmental Research and Public Health. 2021; 18(11):5513. https://doi.org/10.3390/ijerph18115513
Chicago/Turabian StyleTiwari, Ananda, David M. Oliver, Aaron Bivins, Samendra P. Sherchan, and Tarja Pitkänen. 2021. "Bathing Water Quality Monitoring Practices in Europe and the United States" International Journal of Environmental Research and Public Health 18, no. 11: 5513. https://doi.org/10.3390/ijerph18115513







